Abstract
Objectives
To examine compliance with the Baby-Friendly Hospital Initiative (BFHI) as well as evaluate the BFHI and its components on breastfeeding initiation and duration overall and according to maternal education level.
Design
Quasi-experimental study using data from the Pregnancy Risk Assessment Monitoring System (PRAMS) from 2004 to 2008.
Setting
Birth facilities in Maine.
Participants
915 mothers who gave birth in four hospitals that were BFHI-accredited or became accredited and 1099 mothers from six matched non-BFHI facilities. Mothers reported on seven (of 10) BFHI practices (breastfeeding practice score 0–7) and receipt of a gift pack with formula (yes/no).
Main outcome measures
Self-report of breastfeeding initiation, any breast feeding for ≥4 weeks, exclusive breast feeding for ≥4 weeks.
Results
34.6% of mothers from BFHI-accredited facilities reported experiencing all seven BFHI breastfeeding practices, while 28.4% reported being given a gift pack with formula. Among mothers with lower education, the BFHI increased breastfeeding initiation by 8.6 percentage points (adjusted coefficient, 0.086 [95% CI, 0.01 to 0.16]) and, independently, each additional breastfeeding practice was associated with an average increase in breastfeeding initiation of 16.2 percentage points (adjusted coefficient, 0.162 [95% CI, 0.15 to 0.18]). Among all mothers and mothers with higher education, there was no effect of the BFHI on breastfeeding rates.
Conclusions
Compliance with BFHI practices among BFHI-accredited facilities is not optimal and needs to be monitored, as greater compliance may have an even larger impact on breastfeeding rates and potentially reduce socio-economic disparities in breast feeding.
Introduction
Hospital policies and clinical practices remain significant barriers for many women to start breast feeding and continue after discharge.1–3 In 2009, 77% of US mothers initiated breast feeding and only 36% were exclusively breast feeding at 3 months postpartum.4 The 2011 US Surgeon General's Call to Action to Support Breastfeeding identified the Baby-Friendly Hospital Initiative (BFHI) as a critical strategy for increasing high-quality maternity care.3 The WHO and Unicef established the BFHI in 1991 and the Ten Steps to Successful Breastfeeding outlines evidence-based practices to promote, protect and support breast feeding within the birth facility and after (figure 1).5,6
Figure 1.
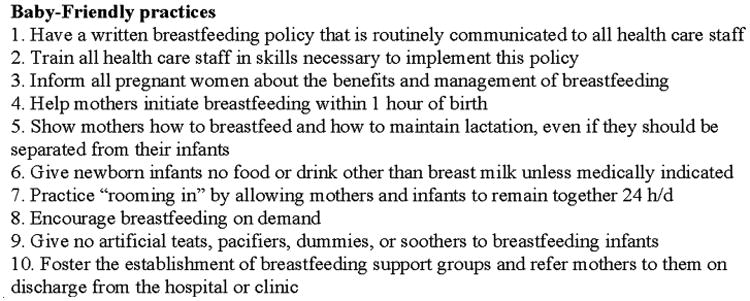
The Baby-Friendly Hospital Initiative's Ten Steps to Successful Breastfeeding.5,6
As of 2012, only 6.2% of live births in the USA occurred in BFHI facilities, ranging from 0% of births in 16 states to 27.7% of births in Maine.4 The 2011 CDC National Survey of Maternity Practices in Infant Nutrition and Care (mPINC) produced a score for each state indicating the extent to which their birth facilities supported breast feeding.7 The national mPINC score was 70 out of 100, with a mean of 65 in the 16 states without any BFHI facilities and 83 in Maine.7 Although the majority of birth facilities in the USA do not have BFHI accreditation, relatively high scores even in the absence of BFHI facilities indicate that many have nonetheless implemented some maternity practices to promote breast feeding.
In a natural experiment using data from 5 states, we have previously shown that among mothers with lower education the BFHI increased breastfeeding initiation by an estimated 3.8 percentage points (adjusted coefficient, 0.038 [95% CI, −0.00 to 0.08]; p=0.05) and exclusive breast feeding for at least 4 weeks by 4.5 percentage points (adjusted coefficient, 0.045 [95% CI, 0.01 to 0.08]; p=0.02).8 However, several questions remained including the distribution of breastfeeding-promoting maternity practices across facilities and whether it was the BFHI itself or its accompanying practices that increased breast feeding. Maine, from the prior study, also collected mothers' reports of seven (of 10) BFHI components. In this paper our aims were to examine compliance with the BFHI as well as evaluate the BFHI and its components on breastfeeding initiation and duration overall and according to maternal education level.
Methods
Since 1987, Maine has participated in the Pregnancy Risk Assessment Monitoring System (PRAMS), a collaborative surveillance project between the CDC and the Maine Department of Health and Human Services.9 Each month the PRAMS survey is mailed to a sample of approximately 125 mothers from state birth certificate files.9,10 Questionnaires are sent 2 to 6 months after delivery and if there is no response to repeated mailings, then women are interviewed by phone. Data collection methodology and the core questionnaire are standardised across states.
Maine PRAMS data with information on infant feeding practices were available for years 2004 through 2008. We used the same exclusion and matching criteria described in our previous paper.8 The final sample included 915 mothers who gave birth in four hospitals that became BFHI accredited before or during the study period and 1099 mothers from six matched non-BFHI birth facilities.
Breastfeeding initiation and duration
On the PRAMS questionnaires, mothers were asked if they ever breastfed or pumped breast milk to feed their baby after delivery and, if so, the number of weeks or months.
We defined breastfeeding initiation as yes if mothers reported their infant received any breast milk. We also categorised whether mothers reported any breast feeding for 4 weeks or more (yes/no) and exclusive breast feeding if mothers reported the baby consumed only breast milk for 4 weeks or more (yes/no).
BFHI accreditation and hospital practices
Baby-Friendly USA, the accrediting body for the BFHI in the USA, provided information on the month and year of BFHI accreditation for all birth facilities.6 We identified 4 BFHI birth facilities in Maine and coded mothers as giving birth before or after accreditation based on the month/year of birth.
From 2004 through 2008, the Maine PRAMS questionnaire asked mothers 9 statements about hospital practices related to infant feeding (yes/no). Seven of these statements correspond to the BFHI Ten Steps #3-#9 (figure 1).5,6 We calculated a breastfeeding practice score for each mother by summing all ‘yes’ responses to the 7 BFHI statements (statement on pacifier use was reverse-coded to be consistent with the BFHI practice) (range 0–7). We also created a categorical breastfeeding practice score: 0–2, 3–5, 6, 7. The remaining 2 statements (yes/no) asked whether mothers received a discharge gift pack with formula and, separately, were provided a telephone number for breastfeeding support.
Sociodemographic characteristics
The PRAMS survey data are linked with information on maternal race/ethnicity and years of education from infants' birth certificates. We dichotomised maternal education into ≤12 years (0–11 years, 12 years) indicating a high school education or less and ≥13 years (13–15 years, 16+ years) indicating at least some college.
Statistical analysis
For each Baby-Friendly hospital we identified two matched birth facilities using the ‘neighbor’ program in Stata,11 which finds the ‘nearest neighbors’ by computing the Euclidian distance between the standardised values of pairs of observations. The ‘nearest neighbors’ were identified using three variables: the number of births as a proxy for the size of the birth facility, percentage of white mothers and percentage of mothers with high education. A non-BFHI birth facility could be matched with more than one BFHI hospital.
We first examined differences in the proportion of mothers who agreed with each BFHI-related statement across three groups: non-BFHI facilities, BFHI facilities preaccreditation and BFHI facilities postaccreditation. We then used differences-in-differences models to assess the impact of the BFHI on breastfeeding initiation and duration overall and according to maternal education level. We compared breastfeeding rates before and after BFHI accreditation among mothers who gave birth in hospitals that became accredited with mothers who gave birth in non-BFHI facilities. Based on our knowledge of disparities in breast feeding,3, 12 we stratified the analyses into lower and higher education groups. Models subsequently included mothers' breastfeeding practice score (0-7) and whether mothers reported being given a gift pack with formula (yes/no) to determine the independent effect of the BFHI on breastfeeding rates.
For all analyses we estimated ordinary least squares (OLS) regression models with year and hospital fixed effects to control for time trends in breast feeding13 and time-invariant hospital characteristics. We included a variable indicating whether mothers gave birth after BFHI accreditation and an interaction between year and whether a birth facility ever received accreditation to account for potentially differing time trends. The coefficients on OLS models with a dichotomous outcome are interpreted as the percentage point increase in the outcome. We ran separate models for 3 breastfeeding outcomes: breastfeeding initiation, any breast feeding for ≥4 weeks, exclusive breast feeding for ≥4 weeks. Analyses were conducted using Stata statistical software, V.12.1SE, with robust SEs.
Results
Table 1 illustrates that the racial/ethnic and educational composition of mothers in Maine was comparable across birth facilities. The proportion of mothers who started breast feeding ranged from 76% to 85% across birth facilities, with similar variability among mothers with lower education.
Table 1. Characteristics of participating BFHI hospitals, matched birth facilities and women who participated in the Pregnancy Risk Assessment Monitoring System, 2004–2008 (N=2014).
| Date accredited* | Annual birth* | No of babies born before/after BFHI accreditation | % Race/ethnicity | % Education | % Breastfeed | % Breastfeed initiation | |||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| White | Black | Hispanic | ≤ 12 years | All mothers | ≤ 12 years of education | ||||
| Hospital A | 07/97 | 203 | 0/79 | 96 | 1 | 1 | 48 | 85 | 68 |
| Hospital B | 05/06 | 821 | 122/169 | 93 | 3 | 0.7 | 46 | 76 | 70 |
| Hospital C | 04/07 | 1162 | 271/158 | 97 | 0.2 | 0.7 | 50 | 80 | 73 |
| Hospital D | 02/08 | 402 | 94/22 | 96 | 0 | 4 | 29 | 82 | 65 |
| 6 matched facilities | 1099 | 96 | 0.8 | 2 | 38 | 79 | 64 | ||
Information from Baby-Friendly USA.6.
BFHI, Baby-Friendly Hospital Initiative.
We found that 34.6% of mothers from BFHI facilities reported experiencing seven BFHI practices compared to 27.1% of mothers from non-BFHI facilities (table 2). Although a higher proportion of mothers from BFHI facilities postaccreditation reported being given information about breast feeding than preaccreditation (Step 3, 96.0% vs 90.6%), compliance with the remaining practices was not optimal. For Steps 4 to 9, compliance for BFHI facilities postaccreditation ranged from 57% to 87%. The largest difference across facility type was seen for the non-BFHI practice on giving mothers gift packs with formula. Mothers who gave birth in non-BFHI facilities were twice as likely to report they were given a gift pack with formula than mothers who gave birth in BFHI facilities preaccreditation or postaccreditation (67% vs 35% vs 28%), respectively.
Table 2. The BFHI's Ten Steps to Successful Breastfeeding and percentage of mothers who reported hospital practices according to BFHI accreditation, Pregnancy Risk Assessment Monitoring System (N=1935)*.
| Non-BFHI % (N=1099) | Pre-BFHI accreditation % (N=487) | Post-BFHI accreditation % (N=349) | p Value | |
|---|---|---|---|---|
| Statements from PRAMS questionnaire (yes/no) as numbered in BFHI Ten Steps | ||||
| 3. Hospital staff gave me information about breast feeding | 91.9 | 90.6 | 96.0† | 0.01 |
| 4. I breastfed in the first hour after my baby was born | 56.8 | 57.5 | 57.2 | 1.0 |
| 5. Hospital staff helped me learn how to breastfeed | 69.0 | 68.8 | 72.2 | 0.5 |
| 6. My baby was fed only breast milk at the hospital | 51.8 | 61.1 | 58.8 | 0.001 |
| 7. My baby stayed in the same room with me at the hospital | 90.5 | 89.1 | 86.5 | 0.1 |
| 8. Hospital staff told me to breastfeed whenever my baby wanted | 72.8 | 71.8 | 73.0 | 0.9 |
| 9. My baby (did not) use a pacifier in the hospital‡ | 61.0 | 74.3 | 71.4 | <0.001 |
| BFHI practices summarised | ||||
| Mean number of practices (SD) (range 0–7)‡ | 4.9 (2.0) | 5.1 (2.0) | 5.3 (1.9) | |
| 0–2 practices | 18.1 | 16.6 | 12.1 | 0.001 |
| 3–5 practices | 32.4 | 25.2 | 32.3 | |
| 6 practices | 22.4 | 23.3 | 21.0 | |
| 7 practices | 27.1 | 34.9 | 34.6 | |
| Other practices to support breast feeding | ||||
| The hospital gave me a gift pack with formula | 69.0 | 34.6 | 28.4§ | <0.001 |
| The hospital gave me a telephone number to call for help with breast feeding | 76.6 | 79.4 | 79.4 | 0.4 |
Excludes mothers from BFHI Hospital A with no ‘before’ data available.
p<0.05 comparison of BFHI facilities before and after accreditation.
Pacifier use was reverse-coded to indicate ‘did not use a pacifier in the hospital’.
p=0.06 comparison of BFHI facilities before and after accreditation.
BFHI, Baby-Friendly Hospital Initiative; PRAMS, Pregnancy Risk Assessment Monitoring System.
We did not find an effect of the BFHI on breastfeeding initiation or duration either overall or stratified by maternal education (table 3). We subsequently included mothers' breastfeeding practice scores and whether they reported being given a gift pack with formula. After controlling for these measures, we found that breastfeeding initiation increased by 8.6 percentage points after BFHI accreditation (adjusted coefficient, 0.086 [95% CI, 0.01 to 0.16]) among mothers with lower education. In contrast, we did not find an effect of the BFHI on breastfeeding initiation overall or among mothers with higher education and we did not observe an additional effect of the BFHI on either measure of breastfeeding duration.
Table 3. Fixed effects models evaluating the impact of the BFHI and additional breastfeeding practices on breastfeeding outcomes, Pregnancy Risk Assessment Monitoring System (N=1975)*.
| All mothers | Mothers with ≤12 years of education | Mothers with ≥13 years of education | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Total N | Coefficient† (95% CI) | p Value | n | Coefficient† (95% CI) | p Value | n | Coefficient† (95% CI) | p Value | |
| Breastfeeding initiation | |||||||||
| BFHI | 1975 | 0.070 (−0.04 to 0.18) | 0.2 | 821 | 0.093 (−0.06 to 0.24) | 0.2 | 1153 | 0.048 (−0.07 to 0.17) | 0.4 |
| Additional breastfeeding practices | 1975 | 821 | 1153 | ||||||
| BFHI | 0.032 (−0.02 to 0.08) | 0.2 | 0.086 (0.01 to 0.16) | 0.03 | −0.002 (−0.08 to 0.07) | 0.9 | |||
| Mother's breastfeeding practice score | 0.146 (0.13 to 0.16) | <0.001 | 0.162 (0.15 to 0.18) | <0.001 | 0.127 (0.11 to 0.15) | <0.001 | |||
| Given gift pack with formula | −0.113 (−0.15 to -0.08) | <0.001 | −0.129 (−0.17 to −0.09) | <0.001 | −0.098 (−0.15 to −0.04) | 0.003 | |||
| Any breastfeeding for ≥4 weeks | |||||||||
| BFHI | 1938 | 0.068 (−0.02 to 0.16) | 0.1 | 807 | 0.099 (−0.11 to 0.30) | 0.3 | 1130 | 0.013 (−0.10 to 0.12) | 0.8 |
| Additional breastfeeding practices | 1938 | 807 | 1130 | ||||||
| BFHI | 0.030 (−0.11 to 0.17) | 0.6 | 0.094 (−0.18 to 0.37) | 0.5 | −0.037 (−0.12 to 0.05) | 0.3 | |||
| Mother's breastfeeding practice score | 0.138 (0.12 to 0.16) | <0.001 | 0.144 (0.13 to 0.16) | <0.001 | 0.121 (0.10 to 0.15) | <0.001 | |||
| Given gift pack with formula | −0.159 (−0.19 to −0.13) | <0.001 | −0.129 (−0.18 to −0.08) | <0.001 | −0.156 (−0.21 to −0.10) | <0.001 | |||
| Exclusive breastfeeding for ≥4 weeks | |||||||||
| BFHI | 1951 | 0.025 (−0.07 to 0.12) | 0.6 | 812 | 0.054 (−0.09 to 0.20) | 0.4 | 1138 | −0.019 (−0.20 to 0.16) | 0.8 |
| Additional breastfeeding practices | 1951 | 812 | 1138 | ||||||
| BFHI | −0.010 (−0.05 to 0.03) | 0.6 | 0.045 (−0.09 to 0.18) | 0.5 | −0.066 (−0.20 to 0.06) | 0.3 | |||
| Mother's breastfeeding practice score | 0.124 (0.11 to 0.14) | <0.001 | 0.121 (0.10 to 0.14) | <0.001 | 0.121 (0.10 to 0.14) | <0.001 | |||
| Given gift pack with formula | −0.173 (−0.20 to −0.15) | <0.001 | −0.133 (−0.21 to −0.05) | 0.005 | −0.179 (−0.22 to −0.14) | <0.001 | |||
Excludes 39 mothers with missing information on breastfeeding practice score or being given a gift pack with formula.
All models include a birth facility fixed effect and an interaction between year and whether a birth facility ever received BFHI accreditation.
BFHI, Baby-Friendly Hospital Initiative.
Mothers' breastfeeding practice scores and their report of being given a gift pack with formula had independent relationships with women's probability of breastfeeding initiation. Overall, each additional breastfeeding practice was associated with an average increase in breastfeeding initiation of 14.6 percentage points (adjusted coefficient, 0.146 [95% CI, 0.13 to 0.16]), but being given a gift pack with formula was associated with an average decrease in breastfeeding initiation of 11.3 percentage points (adjusted coefficient, −0.113 [95% CI, −0.15 to −0.08]). Similar patterns were seen for breastfeeding duration. We repeated analyses using the categorical breastfeeding practice score and the results were consistent (not shown).
Discussion
We showed that at least half of the mothers from Maine reported experiencing 6–7 breastfeeding practices consistent with the BFHI, regardless of the birth facility's BFHI status. However, BFHI-accredited hospitals' compliance with the BFHI components was not optimal, ranging from 57% to 96%, and over a quarter of mothers reported being given a gift pack with formula. Nevertheless, we showed that among mothers with lower education, breastfeeding initiation increased by an estimated 8.6 percentage points after BFHI accreditation and that, on average, each additional breastfeeding practice was associated with an average increase in breastfeeding initiation of 16.2 percentage points. Among all mothers and mothers with higher education, we did not find an additional effect of the BFHI on breastfeeding rates after controlling for the number of breastfeeding practices mothers experienced. Taken together, these findings suggest that greater compliance with the BFHI components may have resulted in a larger effect of the BFHI on breastfeeding initiation.
These findings build on our prior evaluation of the BFHI using PRAMS data from five states. Although previously we did not find an overall impact of the BFHI on breastfeeding initiation rates, an effect was observed among mothers with lower education. The detailed data on maternity practices in Maine provided insight into seven (of 10) BFHI practices experienced by mothers across all types of birth facilities. Even though hospitals may have been implementing some breastfeeding practices as they were working towards BFHI accreditation, we showed that maternal report of practices was similar across facilities preaccreditation and postaccreditation. In addition, nearly one-third of mothers who gave birth in non-BFHI facilities reported experiencing seven BFHI practices. This suggests that mothers in the control group were also ‘treated’ with some breastfeeding practices; had we been able to compare similar birth facilities with no/very few breastfeeding practices with facilities that complied with all 10 BFHI practices, the effect sizes estimated would almost certainly have been larger.
After controlling for mothers' breastfeeding practice score, we did not find an additional effect of the BFHI on breastfeeding initiation overall or among mothers with higher education. The attenuation of the coefficients due to confounding suggests that it may be the number of hospital practices supporting breast feeding rather than BFHI accreditation itself that increases breast feeding. In contrast, among mothers with lower education, we found that the coefficient was largely unchanged, but the CI narrowed, indicating that BFHI accreditation increased breastfeeding initiation after controlling for mothers' breastfeeding practice score. Giving birth in a BFHI hospital had an additional effect on breastfeeding initiation for these mothers, a group less likely to start breast feeding.3,13 Although we can only speculate as to the reasons for this finding, it may be related to the remaining BFHI-mandated practices on which we do not have data that may have particularly benefitted these mothers, or the whole suite of practices required for accreditation may have provided the additional support that at-risk mothers needed to start breast feeding. Further research is needed to test these differences.
Research in the USA on the BFHI and its components has been limited. Cross-sectional studies have shown that a higher number of hospital practices are associated with higher rates of breast feeding,14–19 but cannot identify the direction of causality. Consistent with before–after studies of Boston Medical Center, an inner-city hospital accredited in 1999 serving a predominantly low-income population, we found a positive effect of the BFHI on breastfeeding initiation among mothers with lower education.20,21 Although their rate of breast feeding at 6 months was consistent with national levels, it was lower than would be expected given their high rates of breastfeeding initiation.22 We did not find evidence for an effect of the BFHI on either measure of breastfeeding duration. In our previous evaluation, we found that the BFHI increased exclusive breast feeding for at least 4 weeks among mothers with lower education.8 Although the effect sizes were similar between studies, the coefficients in the present analysis were not statistically significant.
The only randomised controlled trial (RCT) of the BFHI has been conducted outside the USA, in Belarus.23 While the Belarussian RCT found that babies born in BFHI facilities were more likely to be exclusively breastfed at 3 and 6 months than babies from control hospitals, Kramer and colleagues created postnatal breastfeeding support through the intervention polyclinics.23 The aim of Step 10 is to develop breastfeeding support groups after discharge.5,6 In Maine, about three-quarters of mothers reported they were given a telephone number to call for help with breast feeding, but no other information was available on postpartum support. This may leave substantial room for variability between birth facilities and, thus, its impact on breastfeeding duration.
Maine has the highest proportion of births in BFHI facilities, suggesting that results may not generalise fully to other states. The large sample of births in BFHI facilities and detailed data on maternity practices provided us with an opportunity to build on the limited evidence of the BFHI in the USA. Although social desirability may have inflated reported breastfeeding rates or breastfeeding practices experienced, the PRAMS survey was not designed to assess BFHI compliance and we have no reason to believe that giving birth in a Baby-Friendly hospital would systematically bias maternal report. PRAMS does not contain any objective measures of the Ten Steps and we have shown that compliance, as measured by self-report, was low for some BFHI components even in BFHI-accredited hospitals. Mothers may have been less likely to report having experienced a particular practice because they chose not to breastfeed or maternity care staff were less likely to offer a particular practice because mothers chose not to breastfeed. Understanding these distinctions is essential to inform better implementation of the BFHI and, ultimately, improve breastfeeding rates.
We also found that over a quarter of mothers in Maine who gave birth in BFHI facilities reported receiving a gift pack with formula, a practice not allowed by the BFHI because of its negative influence on breastfeeding rates.6,24,25 BFHI-accredited facilities are required to follow the Ten Steps and the International Code of Breast-Milk Substitutes.26 Interestingly, Feldman-Winter and colleagues found that one-third of mothers who received a ‘diaper discharge bag’ without formula reported receiving formula at 10 weeks postpartum.27 Further research is needed to assess compliance with the Ten Steps and International Code using both objective measures of hospital practices and maternal report.
Although we demonstrated that most birth facilities had some maternity practices supporting breast feeding regardless of their Baby-Friendly status, compliance with the BFHI components was not optimal among BFHI-accredited hospitals. We also showed that BFHI accreditation increased breastfeeding initiation among mothers with lower education, independent of the number of breastfeeding-promoting maternity practices mothers experienced, but did not impact breastfeeding duration. Currently, 94% of mothers in the USA give birth in non-BFHI accredited facilities.4 Our results suggest that compliance with the BFHI needs to be monitored, as greater compliance may have an even larger impact on breastfeeding rates and potentially reduce socio-economic disparities in breast feeding.
What is already known.
Hospital policies and clinical practices are significant barriers for successful breast feeding.
The Baby-Friendly Hospital Initiative (BFHI) has been shown to increase breastfeeding rates.
What this study adds.
Only one-third of mothers from Baby-Friendly Hospital Initiative (BFHI)-accredited facilities reported experiencing all 7 BFHI breastfeeding practices.
Over a quarter of mothers from BFHI-accredited facilities reported receiving a gift pack with formula.
The BFHI is effective at increasing breastfeeding initiation among mothers with lower education.
BFHI-accredited hospitals compliance with the BFHI is not optimal, as greater compliance may have a larger impact on breastfeeding rates and socio-economic disparities in breast feeding.
Acknowledgments
The authors would like to thank Tom Patenaude and the PRAMS working group in Maine for the data and their assistance throughout this project as well as the Centers for Disease Control and Prevention PRAMS Team, Applied Sciences Branch, Division of Reproductive Health.
Funding: This study was funded by grants from NIH—NICHD R00HD068506 to Dr Hawkins and T32-AG000186 to the National Bureau of Economic Research and the NSF-IGERT program, ‘Multidisciplinary Program in Inequality & Social Policy’ at Harvard University (Grant No. 0333403) for Ms Stern. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Contributors: SSH conceptualised and designed the study, participated in data collection, analysis and interpretation and drafted the initial manuscript. ADS participated in data analysis and interpretation, critically reviewed and revised the manuscript. CFB participated in data analysis and interpretation, reviewed and revised the manuscript. MWG participated in data interpretation, critically reviewed and revised the manuscript. All authors approved the final manuscript as submitted. SSH had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Competing interests: None.
Ethics approval: The Harvard School of Public Health Institutional Review Board reviewed this study and considered it exempt. The Maine Office of Data, Research and Vital Statistics also reviewed and approved the protocol.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- U.S. Department of Health and Human Services. Healthy People 2020 Objective Topic Areas and Page Numbers. [accessed 25 Oct 2012]; http://healthypeople.gov/2020/topicsobjectives2020/pdfs/HP2020objectives.pdf.
- 2.American Academy of Pediatrics Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics. 2012;129:e827–41. doi: 10.1542/peds.2011-3552. [DOI] [PubMed] [Google Scholar]
- 3.U.S. Department of Health & Human Services. The Surgeon General's Call to Action to Support Breastfeeding. Washington, DC: U.S. Department of Health & Human Services; 2011. [Google Scholar]
- 4.Centers for Disease Control and Prevention. Breastfeeding Report Card—United States. [accessed 20 Nov 2012];2012 http://www.cdc.gov/breastfeeding/pdf/2012BreastfeedingReportCard.pdf.
- 5.World Health Organization, United Nations Children's Fund. Promoting and Supporting Breastfeeding: the Special Role of Maternity Services. Geneva: World Health Organization; 1989. [Google Scholar]
- 6. [accessed 15 Mar 2013];Baby-Friendly USA. http://www.babyfriendlyusa.org.
- 7.Centers for Disease Control and Prevention. mPINC results. [accessed 18 Jul 2012]; http://www.cdc.gov/breastfeeding/data/mpinc/results.htm.
- 8.Hawkins SS, Stern AD, Baum CF, et al. Effect of Baby-Friendly Hospital Initiative on breastfeeding rates in the US: a multi-state analysis. under review. [Google Scholar]
- 9.Maine Department of Health and Human Services. Pregnancy Risk Assessment Monitoring System (PRAMS) [accessed 1 Nov 2013]; http://www.maine.gov/dhhs/mecdc/public-health-systems/data-research/prams/
- 10.Data, Research and Vital Statistics, Maine Centers for Disease Control and Prevention. Maine PRAMS Surveillance Report 2004-2008. Augusta: Maine Department of Health and Human Services; 2011. [Google Scholar]
- 11.Baum CF. An Introduction to Stata Programming, 2009. College Station, TX: Stata Press; 2009. Chapter 14.7. Locating nearest neighbors with Mata; pp. 327–31. [Google Scholar]
- 12.Centers for Disease Control and Prevention. Racial and ethnic differences in breastfeeding initiation and duration, by state—National Immunization Survey, United States, 2004-2008. MMWR Morb Mortal Wkly Rep. 2010;59:327–34. [PubMed] [Google Scholar]
- 13.Grummer-Strawn LM, Shealy KR. Progress in protecting, promoting, and supporting breastfeeding: 1984-2009. Breastfeed Med. 2009;4:S31–9. doi: 10.1089/bfm.2009.0049. [DOI] [PubMed] [Google Scholar]
- 14.DiGirolamo AM, Grummer-Strawn LM, Fein SB. Effect of maternity-care practices on breastfeeding. Pediatrics. 2008;122:S43–9. doi: 10.1542/peds.2008-1315e. [DOI] [PubMed] [Google Scholar]
- 15.Merewood A, Mehta SD, Chamberlain LB, et al. Breastfeeding rates in US Baby-Friendly hospitals: results of a national survey. Pediatrics. 2005;116:628–34. doi: 10.1542/peds.2004-1636. [DOI] [PubMed] [Google Scholar]
- 16.Rosenberg KD, Stull JD, Adler MR, et al. Impact of hospital policies on breastfeeding outcomes. Breastfeed Med. 2008;3:110–16. doi: 10.1089/bfm.2007.0039. [DOI] [PubMed] [Google Scholar]
- 17.Murray EK, Ricketts S, Dellaport J. Hospital practices that increase breastfeeding duration: results from a population-based study. Birth. 2007;34:202–11. doi: 10.1111/j.1523-536X.2007.00172.x. [DOI] [PubMed] [Google Scholar]
- 18.Perrine CG, Scanlon KS, Li R, et al. Baby-Friendly hospital practices and meeting exclusive breastfeeding intention. Pediatrics. 2012;130:54–60. doi: 10.1542/peds.2011-3633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Declercq E, Labbok MH, Sakala C, et al. Hospital practices and women's likelihood of fulfilling their intention to exclusively breastfeed. Am J Public Health. 2009;99:929–35. doi: 10.2105/AJPH.2008.135236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Philipp BL, Malone KL, Cimo S, et al. Sustained breastfeeding rates at a US Baby-Friendly hospital. Pediatrics. 2003;112:e234–6. doi: 10.1542/peds.112.3.e234. [DOI] [PubMed] [Google Scholar]
- 21.Philipp BL, Merewood A, Miller LW, et al. Baby-friendly hospital initiative improves breastfeeding initiation rates in a US hospital setting. Pediatrics. 2001;108:677–81. doi: 10.1542/peds.108.3.677. [DOI] [PubMed] [Google Scholar]
- 22.Merewood A, Patel B, Newton KN, et al. Breastfeeding duration rates and factors affecting continued breastfeeding among infants born at an inner-city US Baby-Friendly hospital. J Hum Lact. 2007;23:157–64. doi: 10.1177/0890334407300573. [DOI] [PubMed] [Google Scholar]
- 23.Kramer MS, Chalmers B, Hodnett ED, et al. Promotion of Breastfeeding Intervention Trial (PROBIT): a randomized trial in the Republic of Belarus. JAMA. 2001;285:413–20. doi: 10.1001/jama.285.4.413. [DOI] [PubMed] [Google Scholar]
- 24.Bergevin Y, Dougherty C, Kramer MS. Do infant formula samples shorten the duration of breast-feeding? Lancet. 1983;1:1148–51. doi: 10.1016/s0140-6736(83)92878-7. [DOI] [PubMed] [Google Scholar]
- 25.Rosenberg KD, Eastham CA, Kasehagen LJ, et al. Marketing infant formula through hospitals: the impact of commercial hospital discharge packs on breastfeeding. Am J Public Health. 2008;98:290–5. doi: 10.2105/AJPH.2006.103218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization. International Code of Marketing Breast-milk Substitutes. Geneva: World Health Organization; 1981. [Google Scholar]
- 27.Feldman-Winter L, Grossman X, Palaniappan A, et al. Removal of industry-sponsored formula sample packs from the hospital: does it make a difference? J Hum Lact. 2012;28:380–8. doi: 10.1177/0890334412444350. [DOI] [PubMed] [Google Scholar]


