Abstract
Different approaches are necessary when Community Based Participatory Research (CBPR) of environmental illness is initiated after an environmental disaster within a community. Often such events are viewed as golden scientific opportunities to do epidemiological studies. However, we believe that in such circumstances, community engagement and empowerment needs to be integrated into the public health service efforts in order for both those and any science to be successful, with special care being taken to address the immediate health needs of the community first rather than the pressing needs to answer important scientific questions. We will demonstrate how we have simultaneously provided valuable public health service, embedded generalizable scientific knowledge, and built a successful foundation for supplemental CBPR through our on-going recovery work after the chlorine gas disaster in Graniteville, South Carolina.
Keywords: disaster, epidemiology, environment, chlorine, community based participatory research, ethics, public health, Graniteville
Introduction
Chemical exposure events resulting in environmental health disasters within communities are not unprecedented, nor are community based approaches to recover from them. If well studied, such events can provide scientifically robust information on the human health effects of that specific chemical1. However, performing a scientific study in the wake of a disaster can have additional limitations2.
Though they have not been thoroughly discussed in the context of Community Based Participatory Research (CBPR), the Hiroshima and Nagasaki survivor studies actually were some of the first CBPR studies ever performed3-12. Many epidemiologists may have forgotten, also, that the research on these cohorts did not actually begin until after years of public health service, capacity building, community engagement/co-operation, and community empowerment7, 13, 14. United States scientists co-operated with Japanese scientists equitably, and engaged many city and national groups in the design, implementation, and performance of the public health services and later research with the explicit goal of helping the casualties to recover through methods that were sensitive to the Japanese culture13. The temporal lag between the events and eventual initiation of research allowed the communities to begin to recover. Also, during the period prior to being studied the affected communities were provided many public health and relief services which built their trust in the United States and their researchers who eventually were able to engage those communities in both the longest and largest prospective cohort study ever performed following a single environmental exposure event. The communities were engaged in how the studies would be performed, local scientists and clinicians performed the clinical assessments and services required for the communities, and all correspondence with the participants was orchestrated through local partners. The Hiroshima and Nagasaki studies were ahead of their time, and served as ideal models to guide our team in our recovery and epidemiology efforts following a much smaller environmental health disaster.
Other disasters since Hiroshima and Nagasaki, too, have used CBPR related principals embedded within both the public health services provided and any resulting research that was pursued. The most recent example is the recovery efforts following the World Trade Center Collapse15. But the most complete work currently in the literature is from the recovery of the Mt. St. Helens volcanic eruption16-29. In both the 9/11 and Mt. St. Helens disasters human subjects research studies were initiated only in response to the desire for the local communities to have a better understanding of the uncertainties of their health after their exposures during the disaster. In contrast, other epidemiologic studies have been imposed rapidly following other recent disasters without any community engagement and have been plagued with poor participation rates and differential external control groups 30-32. Also, as hinted by Dominici, et al.1, in their statement “as perverse as it might sound, epidemiologists must view disasters as important opportunities to learn about the etiology of disease”, there are some rather difficult ethical considerations when studying a population that has recently experienced disaster.
Because of the values, responsibilities, and obligations unique to the practice of our profession, it is inevitable that public health professionals will face ethical trade-offs which require that we relinquish one good in order to achieve another we judge of greater value. Defining what is the common good and determining how that shared value should be weighted versus individual goods or rights in the calculus of ethical decisions are among the most critical challenges facing public health ethics. In the context of a community impacted by disaster, this plays out as the issue of when and how to study the impacted population.
In the context of a community study, ethical considerations go beyond the individual and must incorporate the studied community as an independent entity, also33. We believe this is even more important with communities recovering from disaster. Such communities should be considered as a vulnerable population34. Well designed and implemented community based participatory research (CBPR) methods nested within public health service activities can adequately address these complex ethical issues33. Epidemiologists and environmental health scientists are not just scientists, but public health practitioners, also. As public health practitioners we are obligated to come to the aid of communities in crisis35-37, not just study them. Counting the casualties is one of our duties; but our ultimate goal is to limit the toll of the disaster on the life and health of the affected community by providing timely public health assistance 38. In summary, we believe that a community impacted by disaster should not be asked to participate in research unless the research is secondary to public health recovery assistance, and then ideally instituted through CBPR.
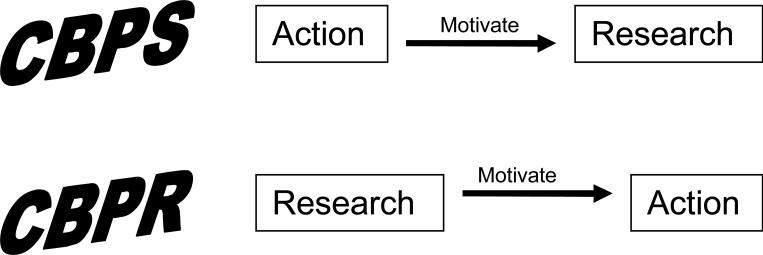
Akin to the CBPR design, it is possible to provide effective and efficient public health service (Community-Based Participatory Service, CBPS) using similar methods of engagement, empowerment, and academic/public health/community collaboration. CBPS is focused on public health action (service) itself, which could motivate research, rather than research to motivate action. This is the fundamental difference between CBPS and CBPR; it is the purpose of the activity that differentiates the two (Figure 1). Scientific knowledge about disease can be learned observationally, without structured human subjects research. Therefore, we believe that by performing ethically conscientious CBPS in response to a technology disaster within a community it is possible to mitigate the toll of the event on the health of the community while concurrently providing generalizable science comparable to that potentially produced by conventional human subjects research methods, such as in CBPR. To accomplish such work unique partnerships of academia and public health with local community organizations are required. We will demonstrate this type of unique partnership within the first several months of the GRACE (Graniteville Recovery And Chlorine Epidemiology) project as a case-study, which has produced both successful CBPS and science, and is positioned to eventually generate supplemental CBPR in response to the chlorine gas disaster in the town of Graniteville, South Carolina.
Figure 1.
Diagram Contrasting Community-based Participatory Service (CBPS) with Community-based Participatory Research (CBPR)
Methods
At 2:48 on the morning of January 6, 2005, a freight train traveling over 77 km/h was inadvertently switched onto an industrial spur and immediately collided with a parked train outside of a textile mill in downtown Graniteville, an unincorporated cotton mill-town in Western South Carolina. The train immediately derailed and one of the derailed cars was punctured and leaked an estimated 54,422 kg of liquid chlorine which quickly boiled and produced a thick cloud of chlorine gas. The weather was calm and the winds were still down in the valley, allowing the plume to spread throughout the community silently while it slept. Chlorine is a strong irritant gas and a weapon of mass destruction first used during World War I39 and has been used by insurgents in the Iraq war. As a result of the chlorine spill, 9 people died, 72 were hospitalized, and more than 840 people sought medical attention at area hospitals and physicians’ offices. At least 220 others experienced symptoms but did not receive medical treatment. The epidemiological response to this event is described in greater detail elsewhere40-43.
The Department of Health and Environmental Control (DHEC) quickly began to assist the community with their recovery. The environmental side of DHEC was the first group within DHEC to start work on the recovery by helping approximately 875 homes and businesses receive air monitoring and safety inspections before people were allowed to reenter evacuated buildings. But the Graniteville community itself played the key role in guiding the public health recovery work.
DHEC staff was contacted by a Graniteville community leader who asked DHEC to address some of the environmental and health concerns that other leaders and other people had within their community. These voluntary local leaders decided they would form into a group called the Graniteville Community Coalition (GCC) to assist with addressing their community's disaster recovery concerns, which DHEC helped them to establish. The GCC compiled health and environmental questions and concerns from the community into a joint list which was provided to DHEC. DHEC staff took those questions, answered them and developed a fact sheet listing the answers. The GCC determined that they would hold a series of community meetings where citizens could come to have their questions answered. Staffs from both the health and environmental sides of DHEC were asked to be there to answer questions. These meetings were held in Graniteville over a one-week period during March 2005. A community partnership was formed. DHEC, also, had questions that needed to be answered. These included “Did we count all of the casualties?”, “Did everyone who needed medical care receive it?”, “Have all of the surviving casualties recovered from their injuries and illnesses?”. The answer to each was “No.” A few weeks following those initial community meetings, the GCC planned the next steps for DHEC and the GCC: 1) perform additional environmental sampling and monitoring to ensure that the environment was safe; and, 2) establish a community health tracking program. DHEC conducted additional environmental monitoring and sampling and found that the air, water, and soil were all indeed safe. The health side of DHEC designed a comprehensive long-term community health tracking program intended to provide routine medical testing and care for members of the Graniteville community. The proposed design resulted from careful research of the approaches taken to recover from similar environmental disasters in other communities44-84, 15, 85-93,14, 94, 95, 16-27, 96-97. As a part of that research consultants within the federal and state government, academia, a private research institute, and international experts on previous disasters49, 55, 57, 70-73, 75-79, 98-100 were queried about their experiences in disaster recovery and their knowledge of persistent health effects of chlorine gas poisoning. A multidisciplinary academic advisory team was later developed which included some of these consultants and additional scientists from the most proximate schools of public health and medicine. Though early efforts to fund the long-term community health tracking program through the responsible railroad eventually failed, these plans were later modified and incorporated into the DHEC and University of South Carolina (USC) supported health registry and screening projects.
Funds were leveraged within DHEC and through the partnership with USC to begin the health registry and screening projects during the summer of 2005. The goal of these health services was to prevent an epidemic of persistent illness associated with acute exposure to chlorine gas and associated traumatic stress. We believed that by identifying people who were likely experiencing persistent health problems associated with the exposure event we could refer them for local medical care and minimize or stop the progression of their persistent disease and control the epidemic of persistent disease.
We first needed to identify people who were at risk of having yet untreated persistent health problems. Therefore, DHEC developed a completely voluntary health registry open to all persons who lived in, worked in, traveled through, or responded to the Graniteville community on January 6, 2005. Partnering with the GCC, local schools, local businesses, local university (University of South Carolina Aiken), and many local churches, the registry was marketed door-to-door within the communities up to two miles from the accident site, since the closest shelter and decontamination site was located just beyond that distance. In addition, all casualties identified during the response phase of the event were notified by mail about the registry and the health screening to follow. To register people simply called into a local phone number and answered a brief enrollment survey. Most registry telephone operators were raised in the local area and one lost a relative during the event. Additional operators were hired who were fluent in Spanish to allow non-English speaking registrants to enroll. Both within our marketing and upon completion of the enrollment survey, we disclosed that registrants may be eligible for a free health screening and that it was our hope to eventually be able to provide a screening to every registrant. Though the registry opened in July 2005, the primary marketing of the registry began at the community healing picnic, when registry staff from our contractor University of South Carolina Aiken were available on-site to meet with people and enroll them. The registry remains open but was transitioned to the 2-1-1 system after the call volume decreased significantly. The 2-1-1 system, which is staffed continuously by local volunteers and funded by the county, has allowed us to keep the registry open continuously.
To address the issue that many individuals were experiencing problems coping with the traumatic stress that they experienced, the GCC partnered with DHEC and a non-profit, faith-based organization in the community to coordinate a community healing picnic immediately before the start of the 2005-2006 academic year. This event was, also, a springboard for both the health registry and health screenings to follow. At this picnic, USC, DHEC, and Department of Mental Health (DMH) social workers were able to talk with residents about their experiences. It also gave trained DHEC and DMH staff an immediate opportunity to offer follow-up to those in need in a safe and comfortable environment. This picnic was full of activities that provided a fun, family atmosphere and was a huge success with more than 850 people attending. The partnership and collaboration on this event began to collectively heal the emotional wounds of this community and to dispel some myths about the town and its future.
Three weeks later in late August 2005 we began 10 weeks of health screenings within the Graniteville community. These health screenings were designed to identify people who likely had medical problems associated with exposure to chlorine or traumatic stress which warranted additional care, not to diagnose and treat them101, 102. The content of the health screenings was determined in consultation with our academic advisory team and the GCC. The health screenings were staffed by local volunteers and contractors and were performed at two area churches (one predominantly black, one predominantly white) and one local medical clinic on a rotating schedule. In brief, the public health screenings included vital signs assessment, medical and exposure histories103, a focused physical examination, psycho-social health questionnaires104-107 and consultation with a licensed counselor, lung function and reactivity tests108, and measurement of an airway inflammation indicator109-111. At the close of each screening the results were reviewed by a physician and recommendations were made for follow-up care, when appropriate. A list of available health and social assistance resources within the community and their contact information was provided to all registrants at the close of each screening so that everyone was empowered to pursue the resolution of their most urgent individual health concerns. At the time, all registrants who were exposed within 1 mile from the event were offered a health screening. This public health intervention did not meet the definition of “Human Subjects Research” as defined by 45 CFR 46.102(d) and determined by the DHEC and USC institutional review boards (IRBs). All registrants voluntarily agreed to participate in the public health screenings. Each screened registrant first provided their informed consent, or in the case of children, parents provided informed consent in proxy. All volunteers/contractors complied with DHEC's Confidentiality Agreement and were either HIPAA certified or trained. Lung function testing is very safe and performed routinely, though has some risk. A crash cart and physician were available on-site at all times for any unexpected complications. Lung reactivity testing was provided only to those who demonstrated a potential clinical benefit from it and was performed during a follow-up evaluation at a local hospital due to the increased risks with that test.
Results
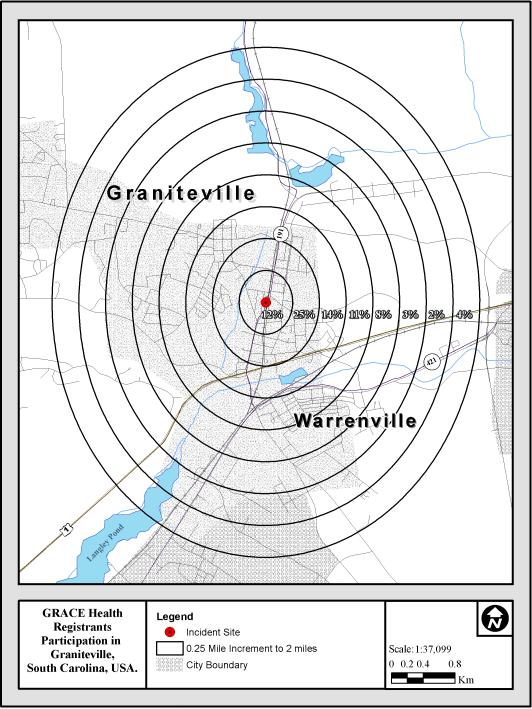
The Graniteville Health Registry represents the greater Graniteville community. The registry is 50% female, 69% white/Caucasian, 26% black/African-American, 0.7% Native American, and 1.7% Hispanic/Latino. These figures are almost identical to the resident population of Graniteville according to Census 2000 data (Table 1). Compared to Census 2000 data, the registrants were slightly older with slightly fewer children and more seniors. Screened registrants were also older, though comparable to the parent population in most all other demographics. The peak level of education within adults over 25 years who were enrolled in the registry was nearly identical to the Census 2000 data for both the high and low education levels. A higher percentage of registrants were high school graduates, but fewer had some post-high school education. Participation rates were stable across the community and exhibited a randomly scattered spatial distribution across the Graniteville area (Figure 2).
Table 1.
Demographic Comparison of the Graniteville Population
| Graniteville* | Registry | Screened | |
|---|---|---|---|
| Population size | 7,009 | 958 | 259 |
| Age under 5 yrs., % | 8.4 | 4.4 | 3.5 |
| Age under 18 yrs., % | 29.8 | 20.5 | 17.0 |
| Age 65 yrs. and over, % | 12.0 | 15.7 | 20.5 |
| Female , % | 52.0 | 51.0 | 55.6 |
| Race, White , % | 69.6 | 68.9 | 63.6 |
| Race, Black or African American , % | 26.9 | 25.6 | 31.8 |
| Race, American Indian and Alaska Native , % | 0.6 | 0.7 | 0.8 |
| Race, Asian , % | 0.3 | 0.0 | 0.0 |
| Race, reporting some other race, % | 1.5 | 1.5 | 0.8 |
| Race, reporting two or more races, % | 1.2 | 0.5 | 0.4 |
| Race, Hispanic or Latino, % | 2.1 | 1.7 | 3.1 |
| Speak Spanish | 2.8 | 1.1 | 1.9 |
| Less than 9th grade, % of age 25+ | 9.6 | 9.9 | 10.3 |
| 9th to 12th grade, no diploma, % of age 25+ | 19.1 | 20.5 | 20.1 |
| High school graduates, % of age 25+ | 34.8 | 41.1 | 39.7 |
| Some college, no degree, % of age 25+ | 20.9 | ||
| Associate Degree, % of age 25+ | 7.5 | ||
| Some college/Associates degree, % of age 25+ | 18.5 | 22.1 | |
| Bachelor's degree, % of age 25+ | 5.3 | 7.0 | 5.4 |
| Graduate or Professonal degree, % of age 25+ | 2.8 | 2.9 | 2.5 |
Census 2000, US Census Bureau
Figure 2.
Map of the Spatial Distribution of the Addresses of GRACE Registrants
Our participatory public health services have enabled us to gather a more accurate count of the casualties from this disaster, to identify casualties likely to require additional medical care and refer them for that care, and to promote health and prevent the progression of persistent disease within community members. Through the health registry we have identified 197 previously unreported casualties who sought medical care for injuries and/or illnesses which occurred or were worsened during the disaster. Between the casualties identified during the response and recovery phases, we currently are aware of 1,384 casualties from this event. Of those, 958 have enrolled in the health registry. There were 259 registrants who received a health screening at 8-10 months post-event. As a result of the initial health screening, we identified 142 casualties (55%) who likely needed additional care, provided them with their medical records from the health screening to support that determination, and referred them for additional medical treatment. The remaining 117 screened registrants were relieved that there were no current medical concerns observed during their screening that warranted immediate additional follow-up care. During the initial screening, 19% of the registrants screened were recommended for additional pulmonary care based on their pulmonary function, inflammation, and reactivity testing results (Table 2). Prior to the health screenings the medical concerns of some registrants were underappreciated by local physicians due to their skepticism of the validity of reported symptoms due to the litigious environment following the disaster. The objective medical testing results from the health screening empowered community members to rebut concerns about the validity of their health problems and promoted their ability to regain control of their health and to prevent their continued morbidity.
Table 2.
| n | % | |
|---|---|---|
| Total | 142 | 54.8 |
| Pulmonology | 48 | 18.5 |
| Psychiatry/Psychology | 47 | 18.2 |
| Ophthamology | 19 | 7.3 |
| Dermatology | 14 | 5.4 |
| Otolaryncology | 7 | 2.7 |
| Cardiology | 6 | 2.3 |
| Neurology | 3 | 1.2 |
| Other | 86 | 33.2 |
By employing a conscientious CBPS strategy without complex population sampling methods or obligation, we have enrolled a population within our health registry that is representative of the population we sought to serve. The registrants were randomly distributed within the community, indicating that chlorine and traumatic stress exposure were, also, randomly distributed within the community. Furthermore, because we did not limit registry enrollment geographically a priori, registrants who were located on the outer fringe of the community at the time of the event and likely were not significantly exposed could serve as internal controls for any supplemental epidemiologic study. Since such potential internal controls were selected with the same criteria as the exposed persons, there is little likelihood of selection bias112. Furthermore, using an internal control group within a follow-up epidemiologic study could disentangle the effects of chlorine from the effects of traumatic stress within the disaster because both the internal control group and the chlorine exposed group would have been exposed to the traumatic stress of the event while an external control group would not. This population based sample could serve as a study population in supplemental CBPR if the community should choose to do so.
Discussion
The GRACE project has demonstrated the successful application of CBPS following a technology disaster within a community. In addition to our project goals of assisting with the recovery of the affected community, we have developed a population based registry, which could eventually serve as a study cohort. Because the registry so well represents the parent population and registrant locations during the disaster were scattered randomly across the community, we further conclude that the registry is comparable to a random sample from the parent population. Essentially, the GRACE project has demonstrated that by performing thoughtful CBPS with the primary goal being to serve the population affected by disaster, it is simultaneously possible to generate similar science that is sought from a traditional investigator-initiated “natural experiment design” disaster epidemiology study, but without actually performing any human subjects research.
However, our CBPS approach has some limitations. Because enrollment in our registry was voluntary, many people who we identified in the response phase have not registered. Some of them were lost to follow-up. Because 62% of the known victims who chose not to register had received medical care within a hospital immediately following the event, we believe that many of those who have not enrolled in the registry chose not to because they did not believe that it would help them since they were already well aware of their current health and were receiving sufficient medical care. This means that our estimates of disease prevalence from the registrants alone are likely to underestimate the real prevalence of persistent disease within the Graniteville community. The health screening was primarily targeted to help the casualties of the event who were unaware of or dissatisfied with their current health status, and the registry was used as a conduit to identify that target population. The registry was never intended to include every casualty from the event. As a consequence, we are still unable to accurately estimate the true prevalence of disease within this community through the data collected from the health screening alone. Further public health surveillance is needed to better estimate the true prevalence of persistent disease within the Graniteville community.
We would have liked to have done more active surveillance of persistent disease within the Graniteville community but we were limited by our resource capacity, both human and financial. DHEC had no prior funding dedicated to assist with the recovery and surveillance of communities impacted by technology disasters. It is important to note that the responsible railroad has been supportive of our public service activities, though they did not chose to fund them. We believe, however, that financial support by the responsible railroad could have undermined the trust of the community in the CBPS. Furthermore, any medical knowledge which could have been gained from those efforts could have potentially exhibited a conflict of interest, and been distrusted or even discounted by treating physicians. In addition, the knowledge that the railroad was financially supporting the public health activities might have elicited further distrust in the activity within the community, reduced participation rates and found our GRACE team guilty by association.
We believe that there is a general gap in the understanding of the profound differences between bioethics and public health ethics among most IRBs and epidemiological researchers. Within public health, the ethical value of respect for persons is expanded to respect for communities33. This implies a respect for the community's will and self-determination, though discerning the will of the community and determining who speaks for the communities are not easily ascertained. The individual ethical value of respect for dignity also carries the broader sense of respect for cultures and communities so that public health actions are sensitive to groups, especially vulnerable populations. The respect for dignity within a vulnerable population is dramatically illustrated in communities impacted by disaster. We believe that by incorporating CBPR types of strategies into public health disaster recovery activities it is possible to address these very complicated ethical issues while still fostering valuable services and science while potentially serving as a foundation for later research.
Conclusions
The scientific heritage of Hiroshima and Nagasaki demonstrated effective implementation of CBPS which later led to copiously productive CBPR. The GRACE project has followed that example, and demonstrated how thoughtful CBPS can both assist the community affected by disaster and advance scientific understanding of the health effects of such an event on the impacted community all without initially performing any human subjects research. Such work could serve as a foundation for supplemental CBPR.
Acknowledgements
We would like to acknowledge all of the assistance provided to us from residents of Graniteville and surrounding communities in performing this work and the many local institutions and organizations who assisted in myriad ways to help our collective CBPS be successful. David Reed helped make the map figure.
Literature Cited
- 1.Dominici F, Levy JI, Louis TA. Methodological challenges and contributions in disaster epidemiology. Epidemiol Rev. 2005;27:9–12. doi: 10.1093/epirev/mxi009. [DOI] [PubMed] [Google Scholar]
- 2.Melius SBJ. Industrial Disasters. In: Gregg MB, editor. The Public Health Consequences of Disasters 1989. US Department of Health and Human Services; Atlanta, Georgia: 1989. pp. 97–102. [Google Scholar]
- 3.Radiation Effects Research Foundation: A Cooperative Japan-US Research Organization-Greetings and Welcome Radiation Effects Research Foundation. 2007 (Accessed 8/1/2007, at http://www.rerf.or.jp/intro/index_e.html.)
- 4.Yamada M, Kasagi F, Sasaki H, Masunari N, Mimori Y, Suzuki G. Association between dementia and midlife risk factors: the Radiation Effects Research Foundation Adult Health Study. J Am Geriatr Soc. 2003;51:410–4. doi: 10.1046/j.1532-5415.2003.51117.x. [DOI] [PubMed] [Google Scholar]
- 5.Nakashima E, Fujiwara S, Funamoto S. Effect of radiation dose on the height of atomic bomb survivors: a longitudinal study. Radiat Res. 2002;158:346–51. doi: 10.1667/0033-7587(2002)158[0346:eordot]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 6.Ron E, Ikeda T, Preston DL, Tokuoka S. Male breast cancer incidence among atomic bomb survivors. J Natl Cancer Inst. 2005;97:603–5. doi: 10.1093/jnci/dji097. [DOI] [PubMed] [Google Scholar]
- 7.Kodama K, Mabuchi K, Shigematsu I. A long-term cohort study of the atomic-bomb survivors. J Epidemiol. 1996;6:S95–105. doi: 10.2188/jea.6.3sup_95. [DOI] [PubMed] [Google Scholar]
- 8.Pierce DA, Shimizu Y, Preston DL, Vaeth M, Mabuchi K. Studies of the mortality of atomic bomb survivors. Report 12, Part I. Cancer: 1950-1990. Radiat Res. 1996;146:1–27. [PubMed] [Google Scholar]
- 9.Goodman MT, Moriwaki H, Vaeth M, Akiba S, Hayabuchi H, Mabuchi K. Prospective cohort study of risk factors for primary liver cancer in Hiroshima and Nagasaki, Japan. Epidemiology. 1995;6:36–41. doi: 10.1097/00001648-199501000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Preston DL, Kusumi S, Tomonaga M, et al. Cancer incidence in atomic bomb survivors. Part III. Leukemia, lymphoma and multiple myeloma, 1950-1987. Radiat Res. 1994;137:S68–97. [PubMed] [Google Scholar]
- 11.Wong FL, Yamada M, Sasaki H, et al. Noncancer disease incidence in the atomic bomb survivors: 1958-1986. Radiat Res. 1993;135:418–30. [PubMed] [Google Scholar]
- 12.Shimizu Y, Kato H, Schull WJ, Hoel DG. Studies of the mortality of A-bomb survivors. 9. Mortality, 1950-1985: Part 3. Noncancer mortality based on the revised doses (DS86) Radiat Res. 1992;130:249–66. [PubMed] [Google Scholar]
- 13.Neel JV. Unprecedented Challenge Faced in Early Year. RERF Update. 1990;1:7–8. [Google Scholar]
- 14.Day B, Waitzkin H. The medical profession and nuclear war. A social history. Jama. 1985;254:644–51. [PubMed] [Google Scholar]
- 15.Reibman J, Lin S, Hwang SA, et al. The World Trade Center residents' respiratory health study: new-onset respiratory symptoms and pulmonary function. Environ Health Perspect. 2005;113:406–11. doi: 10.1289/ehp.7375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shore JH, Tatum EL, Vollmer WM. Evaluation of mental effects of disaster, Mount St. Helens eruption. Am J Public Health. 1986;76:76–83. doi: 10.2105/ajph.76.suppl.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baxter PJ, Bernstein RS, Buist AS. Preventive health measures in volcanic eruptions. Am J Public Health. 1986;76:84–90. doi: 10.2105/ajph.76.suppl.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buist AS, Bernstein RS, Johnson LR, Vollmer WM. Evaluation of physical health effects due to volcanic hazards: human studies. Am J Public Health. 1986;76:66–75. doi: 10.2105/ajph.76.suppl.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buist AS, Martin TR, Shore JH, Butler J, Lybarger JA. The development of a multidisciplinary plan for evaluation of the long-term health effects of the Mount St. Helens eruptions. Am J Public Health. 1986;76:39–44. doi: 10.2105/ajph.76.suppl.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bernstein RS, Baxter PJ, Falk H, Ing R, Foster L, Frost F. Immediate public health concerns and actions in volcanic eruptions: lessons from the Mount St. Helens eruptions, May 18-October 18, 1980. Am J Public Health. 1986;76:25–37. doi: 10.2105/ajph.76.suppl.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Newhall CG, Fruchter JS. Volcanic activity: a review for health professionals. Am J Public Health. 1986;76:10–24. doi: 10.2105/ajph.76.suppl.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Health effects of volcanoes: an approach to evaluating the health effects of an environmental hazard. Am J Public Health. 1986;76:1–90. [PubMed] [Google Scholar]
- 23.Buist AS, Bernstein RS. Health effects of volcanoes: an approach to evaluating the health effects of an environmental hazard. Am J Public Health. 1986;76:1–2. [PMC free article] [PubMed] [Google Scholar]
- 24.Merchant JA. Preparing for disaster. Am J Public Health. 1986;76:233–5. doi: 10.2105/ajph.76.3.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bernstein RS, Baxter PJ, Buist AS. Introduction to the epidemiological aspects of explosive volcanism. Am J Public Health. 1986;76:3–9. doi: 10.2105/ajph.76.suppl.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martin TR, Wehner AP, Butler J. Evaluation of physical health effects due to volcanic hazards: the use of experimental systems to estimate the pulmonary toxicity of volcanic ash. Am J Public Health. 1986;76:59–65. doi: 10.2105/ajph.76.suppl.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dollberg DD, Bolyard ML, Smith DL. Evaluation of physical health effects due to volcanic hazards: crystalline silica in Mount St. Helens volcanic ash. Am J Public Health. 1986;76:53–8. doi: 10.2105/ajph.76.suppl.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baxter PJ, Ing R, Falk H, et al. Mount St Helens eruptions, May 18 to June 12, 1980. An overview of the acute health impact. Jama. 1981;246:2585–9. [PubMed] [Google Scholar]
- 29.Merchant JA, Baxter P, Bernstein R, et al. Health implications of the Mount St. Helen's eruption: epidemiological considerations. Ann Occup Hyg. 1982;26:911–9. [PubMed] [Google Scholar]
- 30.Lang T, Schwoebel V, Diene E, et al. Assessing post-disaster consequences for health at the population level: experience from the AZF factory explosion in Toulouse. J Epidemiol Community Health. 2007;61:103–7. doi: 10.1136/jech.2005.043331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.van Kamp I, van der Velden PG, Stellato RK, et al. Physical and mental health shortly after a disaster: first results from the Enschede firework disaster study. Eur J Public Health. 2006;16:253–9. doi: 10.1093/eurpub/cki188. [DOI] [PubMed] [Google Scholar]
- 32.Mills MA, Edmondson D, Park CL. Trauma and stress response among Hurricane Katrina evacuees. Am J Public Health. 2007;97(Suppl 1):S116–23. doi: 10.2105/AJPH.2006.086678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Flicker S, Travers R, Guta A, McDonald S, Meagher A. Ethical dilemmas in community-based participatory research: recommendations for institutional review boards. J Urban Health. 2007;84:478–93. doi: 10.1007/s11524-007-9165-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McKeown RE, Weed DL. Ethics in epidemiology and public health II. Applied terms. J Epidemiol Community Health. 2002;56:739–41. doi: 10.1136/jech.56.10.739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weed DL, McKeown RE. Science, ethics, and professional public health practice. J Epidemiol Community Health. 2003;57:4–5. doi: 10.1136/jech.57.1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weed DL, McKeown RE. Science and social responsibility in public health. Environ Health Perspect. 2003;111:1804–8. doi: 10.1289/ehp.6198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McKeown RE, Weed DL, Kahn JP, Stoto MA. American College of Epidemiology Ethics Guidelines: foundations and dissemination. Sci Eng Ethics. 2003;9:207–14. doi: 10.1007/s11948-003-0008-y. [DOI] [PubMed] [Google Scholar]
- 38.Foxman B, Camargo CA, Jr., Lilienfeld D, et al. Looking back at hurricane Katrina: lessons for 2006 and beyond. Ann Epidemiol. 2006;16:652–3. doi: 10.1016/j.annepidem.2005.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Spanjaard OKH, editor. Chemical Weapons. Oxford University Press; Oxford, England: 2003. [Google Scholar]
- 40.Public health consequences from hazardous substances acutely released during rail transit--South Carolina, 2005; selected States, 1999-2004. MMWR Morb Mortal Wkly Rep. 2005;54:64–7. [PubMed] [Google Scholar]
- 41.Miller GW, Richardson JR. Toxicology. In: Frumkin H, editor. Environmental Health: From Global to Local. Jossey-Bass; San Francisco, California: 2005. pp. 29–30. [Google Scholar]
- 42.Van Sickle D, Wenck MA, Belflower A, et al. Acute health effects after exposure to chlorine gas released after a train derailment. American Journal of Emergency Medicine. 2009;27:1–7. doi: 10.1016/j.ajem.2007.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wenck MA, Van Sickle D, Drociuk D, et al. Rapid assessment of exposure to chlorine released from a train derailment and resulting health impact. Public Health Rep. 2007;122:784–92. doi: 10.1177/003335490712200610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kilburn KH. Effects of chlorine and its cresylate byproducts on brain and lung performance. Arch Environ Health. 2003;58:746–55. doi: 10.3200/AEOH.58.12.746-755. [DOI] [PubMed] [Google Scholar]
- 45.Kilburn KH. Brain but not lung functions impaired after a chlorine incident. Ind Health. 2003;41:299–305. doi: 10.2486/indhealth.41.299. [DOI] [PubMed] [Google Scholar]
- 46.Lippin TM, McQuiston TH, Bradley-Bull K, et al. Chemical plants remain vulnerable to terrorists: a call to action. Environ Health Perspect. 2006;114:1307–11. doi: 10.1289/ehp.8762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Weill H. Disaster at Bhopal: the accident, early findings and respiratory health outlook in those injured. Bull Eur Physiopathol Respir. 1987;23:587–90. [PubMed] [Google Scholar]
- 48.Vijayan VK, Sankaran K. Relationship between lung inflammation, changes in lung function and severity of exposure in victims of the Bhopal tragedy. Eur Respir J. 1996;9:1977–82. doi: 10.1183/09031936.96.09101977. [DOI] [PubMed] [Google Scholar]
- 49.Dhara VR. What ails the Bhopal disaster investigations? (And is there a cure?). Int J Occup Environ Health. 2002;8:371–9. doi: 10.1179/107735202800338605. [DOI] [PubMed] [Google Scholar]
- 50.Srivastava RC, Gupta BN, Athar M, et al. Effect of exposure to toxic gas on the population of Bhopal: Part III--Assessment of toxic manifestations in humans--haematological and biochemical studies. Indian J Exp Biol. 1988;26:165–72. [PubMed] [Google Scholar]
- 51.Srinivasa Murthy R. Has the world forgotten Bhopal? Lancet. 2001;357:810. doi: 10.1016/s0140-6736(05)71245-9. [DOI] [PubMed] [Google Scholar]
- 52.Koplan JP, Falk H, Green G. Public health lessons from the Bhopal chemical disaster. Jama. 1990;264:2795–6. [PubMed] [Google Scholar]
- 53.Saxena AK, Singh KP, Nagle SL, et al. Effect of exposure to toxic gas on the population of Bhopal: Part IV--Immunological and chromosomal studies. Indian J Exp Biol. 1988;26:173–6. [PubMed] [Google Scholar]
- 54.Rastogi SK, Gupta BN, Husain T, Kumar A, Chandra S, Ray PK. Effect of exposure to toxic gas on the population of Bhopal: Part II--Respiratory impairment. Indian J Exp Biol. 1988;26:161–4. [PubMed] [Google Scholar]
- 55.Dhara VR, Dhara R, Acquilla SD, Cullinan P. Personal exposure and long-term health effects in survivors of the union carbide disaster at bhopal. Environ Health Perspect. 2002;110:487–500. doi: 10.1289/ehp.02110487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gupta BN, Rastogi SK, Chandra H, et al. Effect of exposure to toxic gas on the population of Bhopal: Part I--Epidemiological, clinical, radiological & behavioral studies. Indian J Exp Biol. 1988;26:149–60. [PubMed] [Google Scholar]
- 57.Dhara VR, Dhara R. The Union Carbide disaster in Bhopal: a review of health effects. Arch Environ Health. 2002;57:391–404. doi: 10.1080/00039890209601427. [DOI] [PubMed] [Google Scholar]
- 58.Percival R. Has the world forgotten Bhopal? Lancet. 2001;357:810. doi: 10.1016/S0140-6736(05)71246-0. [DOI] [PubMed] [Google Scholar]
- 59.Nemery B. Late consequences of accidental exposure to inhaled irritants: RADS and the Bhopal disaster. Eur Respir J. 1996;9:1973–6. doi: 10.1183/09031936.96.09101973. [DOI] [PubMed] [Google Scholar]
- 60.Naik SR, Acharya VN, Bhalerao RA, et al. Medical survey of methyl isocyanate gas affected population of Bhopal. Part II. Pulmonary effects in Bhopal victims as seen 15 weeks after M.I.C. exposure. J Postgrad Med. 1986;32:185–91. [PubMed] [Google Scholar]
- 61.Naik SR, Acharya VN, Bhalerao RA, et al. Medical survey of methyl isocyanate gas affected population of Bhopal. Part I. General medical observations 15 weeks following exposure. J Postgrad Med. 1986;32:175–84. [PubMed] [Google Scholar]
- 62.Misra UK, Nag D, Nath P, Khan WA, Gupta BN, Ray PK. A clinical study of toxic gas poisoning in Bhopal, India. Indian J Exp Biol. 1988;26:201–4. [PubMed] [Google Scholar]
- 63.Lorin HG, Kulling PE. The Bhopal tragedy--what has Swedish disaster medicine planning learned from it? J Emerg Med. 1986;4:311–6. doi: 10.1016/0736-4679(86)90008-9. [DOI] [PubMed] [Google Scholar]
- 64.Broughton E. The Bhopal disaster and its aftermath: a review. Environ Health. 2005;4:6. doi: 10.1186/1476-069X-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kapoor R. Fetal loss and contraceptive acceptance among the Bhopal gas victims. Soc Biol. 1991;38:242–8. doi: 10.1080/19485565.1991.9988791. [DOI] [PubMed] [Google Scholar]
- 66.Jaising I, Sathyamala C. Legal rights and wrongs: internationalising Bhopal. Dev Dialogue. 1992:103–15. [PubMed] [Google Scholar]
- 67.Irani SF, Mahashur AA. A survey of Bhopal children affected by methyl isocyanate gas. J Postgrad Med. 1986;32:195–8. [PubMed] [Google Scholar]
- 68.Cordero JF. The epidemiology of disasters and adverse reproductive outcomes: lessons learned. Environ Health Perspect. 1993;101(Suppl 2):131–6. doi: 10.1289/ehp.93101s2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Goswami HK. Cytogenetic effects of methyl isocyanate exposure in Bhopal. Hum Genet. 1986;74:81–4. doi: 10.1007/BF00278790. [DOI] [PubMed] [Google Scholar]
- 70.Dhara VR, Gassert TH. The Bhopal syndrome: persistent questions about acute toxicity and management of gas victims. Int J Occup Environ Health. 2002;8:380–6. doi: 10.1179/107735202800338731. [DOI] [PubMed] [Google Scholar]
- 71.Dhara R, Dhara VR. Bhopal-A Case Study of International Disaster. Int J Occup Environ Health. 1995;1:58–69. doi: 10.1179/oeh.1995.1.1.58. [DOI] [PubMed] [Google Scholar]
- 72.Dhara VR, Kriebel D. The Bhopal gas disaster: it's not too late for sound epidemiology. Arch Environ Health. 1993;48:436–7. doi: 10.1080/00039896.1993.10545966. [DOI] [PubMed] [Google Scholar]
- 73.Dhara VR, Cullinan P. Bhopal priorities. Int J Occup Environ Health. 2004;10:107. doi: 10.1179/oeh.2004.10.1.107. [DOI] [PubMed] [Google Scholar]
- 74.Dhara VR. Assessing exposure to toxic gases in Bhopal. JAMA. 2004;291:422. doi: 10.1001/jama.291.4.422-a. [DOI] [PubMed] [Google Scholar]
- 75.Dhara VR. On the bioavailability of methyl isocyanate in the Bhopal gas leak. Arch Environ Health. 1992;47:385–6. doi: 10.1080/00039896.1992.9938379. [DOI] [PubMed] [Google Scholar]
- 76.Dhara R, Acquilla S, Cullinan P. Has the world forgotten Bhopal? Lancet. 2001;357:809–10. doi: 10.1016/s0140-6736(05)71244-7. [DOI] [PubMed] [Google Scholar]
- 77.Dhara R. Health effects of the Bhopal gas leak: a review. Epidemiol Prev. 1992;14:22–31. [PubMed] [Google Scholar]
- 78.Cullinan P, Acquilla SD, Dhara VR. Long term morbidity in survivors of the 1984 Bhopal gas leak. Natl Med J India. 1996;9:5–10. [PubMed] [Google Scholar]
- 79.Cullinan P, Acquilla S, Dhara VR. Respiratory morbidity 10 years after the Union Carbide gas leak at Bhopal: a cross sectional survey. The International Medical Commission on Bhopal. Bmj. 1997;314:338–42. doi: 10.1136/bmj.314.7077.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Crabb C. Revisiting the Bhopal tragedy. Science. 2004;306:1670–1. doi: 10.1126/science.306.5702.1670. [DOI] [PubMed] [Google Scholar]
- 81.Bajaj JS, Misra A, Rajalakshmi M, Madan R. Environmental release of chemicals and reproductive ecology. Environ Health Perspect. 1993;101(Suppl 2):125–30. doi: 10.1289/ehp.93101s2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Andersson N, Kerr Muir M, Mehra V, Salmon AG. Exposure and response to methyl isocyanate: results of a community based survey in Bhopal. Br J Ind Med. 1988;45:469–75. doi: 10.1136/oem.45.7.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Has the world forgotten Bhopal? Lancet. 2000;356:1863. [PubMed] [Google Scholar]
- 84.Bhopal gas disaster: clinical & experimental studies. Indian J Exp Biol. 1988;26:149–204. [PubMed] [Google Scholar]
- 85.Lin S, Reibman J, Bowers JA, et al. Upper respiratory symptoms and other health effects among residents living near the World Trade Center site after September 11, 2001. Am J Epidemiol. 2005;162:499–507. doi: 10.1093/aje/kwi233. [DOI] [PubMed] [Google Scholar]
- 86.Samet JM, Geyh AS, Utell MJ. The legacy of World Trade Center dust. N Engl J Med. 2007;356:2233–6. doi: 10.1056/NEJMp068287. [DOI] [PubMed] [Google Scholar]
- 87.Herbstman JB, Frank R, Schwab M, et al. Respiratory effects of inhalation exposure among workers during the clean-up effort at the World Trade Center disaster site. Environ Res. 2005;99:85–92. doi: 10.1016/j.envres.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 88.Izbicki G, Chavko R, Banauch GI, et al. World Trade Center “sarcoid-like” granulomatous pulmonary disease in New York City Fire Department rescue workers. Chest. 2007;131:1414–23. doi: 10.1378/chest.06-2114. [DOI] [PubMed] [Google Scholar]
- 89.Banauch GI, Dhala A, Prezant DJ. Pulmonary disease in rescue workers at the World Trade Center site. Curr Opin Pulm Med. 2005;11:160–8. doi: 10.1097/01.mcp.0000151716.96241.0a. [DOI] [PubMed] [Google Scholar]
- 90.Banauch GI, Dhala A, Alleyne D, et al. Bronchial hyperreactivity and other inhalation lung injuries in rescue/recovery workers after the World Trade Center collapse. Crit Care Med. 2005;33:S102–6. doi: 10.1097/01.ccm.0000151138.10586.3a. [DOI] [PubMed] [Google Scholar]
- 91.Community needs assessment of lower Manhattan residents following the World Trade Center attacks--Manhattan, New York City, 2001. MMWR Morb Mortal Wkly Rep. 2002;51 Spec No:10-3. [PubMed] [Google Scholar]
- 92.Raphael KG, Natelson BH, Janal MN, Nayak S. A community-based survey of fibromyalgia-like pain complaints following the World Trade Center terrorist attacks. Pain. 2002;100:131–9. doi: 10.1016/s0304-3959(02)00273-7. [DOI] [PubMed] [Google Scholar]
- 93.Tapp LC, Baron S, Bernard B, Driscoll R, Mueller C, Wallingford K. Physical and mental health symptoms among NYC transit workers seven and one-half months after the WTC attacks. Am J Ind Med. 2005;47:475–83. doi: 10.1002/ajim.20177. [DOI] [PubMed] [Google Scholar]
- 94.Sadamori N, Shibata S, Mine M, et al. Incidence of intracranial meningiomas in Nagasaki atomic-bomb survivors. Int J Cancer. 1996;67:318–22. doi: 10.1002/(SICI)1097-0215(19960729)67:3<318::AID-IJC2>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 95.Ishimaru T, Cihak RW, Land CE, Steer A, Yamada A. Lung cancer at autopsy in A-bomd survivors and controls, Hiroshima and Nagasaki, 1961-1970. II. Smoking, occupation, and A-bomb exposure. Cancer. 1975;36:1723–8. doi: 10.1002/1097-0142(197511)36:5<1723::aid-cncr2820360527>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 96.Olsen KB, Fruchter JS. Identification of the physical and chemical characteristics of volcanic hazards. Am J Public Health. 1986;76:45–52. doi: 10.2105/ajph.76.suppl.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Radon K, Rosenberger A, Ehrenstein V, et al. Geographical distribution of acute symptoms after a train collision involving epichlorohydrin exposure. Environ Res. 2006;102:46–51. doi: 10.1016/j.envres.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 98.Radon K, Rosenberger A, Ehrenstein V, et al. Geographical distribution of acute symptoms after a train collision involving epichlorohydrin exposure. Environ Res. 2006;102:46. doi: 10.1016/j.envres.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 99.Ramana Dhara V, Dhara R, Acquilla SD, Cullinan P. Personal exposure and long-term health effects in survivors of the Union CarbIde disaster at Bhopal. Environmental Health Perspectives. 2002;110:487. doi: 10.1289/ehp.02110487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Dhara VR. Assessing exposure to toxic gases in Bhopal. Jama. 2004;291:422. doi: 10.1001/jama.291.4.422-a. author reply -3. [DOI] [PubMed] [Google Scholar]
- 101.Weiss NS, Koepsell TD. Epidemiologic Methods: Studying the Occurrence of Illness. Oxford University Press; Oxford, England: 2003. [Google Scholar]
- 102.Teutsch SM, Truman BI. Screening in the Community. In: Petitti DB, Brownson RC, editors. Applied Epidemiology: Theory to Practice. Oxford University Press; Oxford, England: 1998. p. 213. [Google Scholar]
- 103.Ferris BG. Epidemiology Standardization Project (American Thoracic Society). Am Rev Respir Dis. 1978;118:1–120. [PubMed] [Google Scholar]
- 104.Marshall GN. Posttraumatic Stress Disorder Symptom Checklist: factor structure and English-Spanish measurement invariance. J Trauma Stress. 2004;17:223–30. doi: 10.1023/B:JOTS.0000029265.56982.86. [DOI] [PubMed] [Google Scholar]
- 105.Ruggiero KJ, Del Ben K, Scotti JR, Rabalais AE. Psychometric properties of the PTSD Checklist-Civilian Version. J Trauma Stress. 2003;16:495–502. doi: 10.1023/A:1025714729117. [DOI] [PubMed] [Google Scholar]
- 106.Holden RR. Faking and its detection on the Holden Psychological Screening Inventory. Psychol Rep. 1995;76:1235–40. doi: 10.2466/pr0.1995.76.3c.1235. [DOI] [PubMed] [Google Scholar]
- 107.Holden RR, Mendonca JD, Mazmanian D, Reddon JR. Clinical construct validity of the Holden Psychological Screening Inventory (HPSI). J Clin Psychol. 1992;48:627–33. doi: 10.1002/1097-4679(199209)48:5<627::aid-jclp2270480508>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 108.ATS Standardization of Spirometry, 1994 Update. American Thoracic Society. Am J Respir Crit Care Med. 1995;152:1107–36. doi: 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- 109.Hunt J. Exhaled breath condensate pH: reflecting acidification of the airway at all levels. Am J Respir Crit Care Med. 2006;173:366–7. doi: 10.1164/rccm.2512001. [DOI] [PubMed] [Google Scholar]
- 110.Hunt J. Exhaled breath condensate: an evolving tool for noninvasive evaluation of lung disease. J Allergy Clin Immunol. 2002;110:28–34. doi: 10.1067/mai.2002.124966. [DOI] [PubMed] [Google Scholar]
- 111.Vaughan J, Ngamtrakulpanit L, Pajewski TN, et al. Exhaled breath condensate pH is a robust and reproducible assay of airway acidity. Eur Respir J. 2003;22:889–94. doi: 10.1183/09031936.03.00038803. [DOI] [PubMed] [Google Scholar]
- 112.Duncan RC, Aldrich TE, Griffith J. Epidemiologic Research Methods. In: Griffith J, Aldrich TE, editors. Enviornmental Epidemiology and Risk Assessment. John Wiley & Sons; Hoboken, New Jersey: 2002. p. 44. [Google Scholar]