Abstract
Objective
We investigate whether differences in sleep duration help explain ethnic disparities in body mass index (BMI) among U.S. adolescents. We also evaluate the functional form of the association between sleep duration and BMI, and investigate whether this association varies by sex and ethnicity.
Participants and Methods
We analyzed restricted-use data from the first 2 waves of the National Longitudinal Study of Adolescent Health (n=30 133) to evaluate linear and quadratic associations between sleep duration and BMI. Through a series of models that incorporated interaction terms between sex, ethnicity and sleep duration, we also assessed whether (1) sleep duration mediates associations between ethnicity and BMI, and (2) associations between sleep duration and BMI differ for girls and boys from different ethnic groups.
Results
A linear association between sleep duration and BMI best fits the data in this large sample of U.S. adolescents. We find no evidence that sleep duration contributes substantially to ethnic disparities in BMI. However, we detect significant differences in the association between sleep duration and BMI by sex and ethnicity. Sleep duration is negatively associated with BMI among white, Hispanic and Asian boys, positively associated with BMI among black girls, and not related to BMI among black boys or girls from white, Hispanic or Asian ethnic groups.
Conclusion
Despite significant associations between sleep duration and BMI for certain groups of adolescents, we find no evidence that ethnic differences in sleep duration exacerbate ethnic disparities in BMI. Future research should explore mechanisms that underlie ethnic differences in the association between sleep and BMI.
Keywords: Adolescent Health, Body Mass Index-BMI, Ethnicity, Health Disparities, Sleep
INTRODUCTION
In the past few decades, obesity has become ubiquitous in the U.S., affecting persons from all socioeconomic and demographic groups.1-3 Recent birth cohorts have been especially susceptible to excess weight gain,4, 5 as shown by the tripling of obesity rates among U.S. adolescents between 1980 and 2000.6 Perhaps less well known is the fact that children and adolescents in the U.S. do not get enough sleep.7-10 Although 9 hours of sleep is considered optimal for children aged 10-17,11 data show that sleep duration is insufficient and declines during adolescence, from an average of around 8.1 hours at ages 12-13 to an average of only 7.0 hours at ages 16-17.12
The concomitant timing of unhealthful sleep and obesity patterns in the U.S. population gives the appearance that these trends may be related – a notion supported by epidemiological and experimental data indicating that short sleep promotes weight gain and obesity.13, 14 However, the large body of literature on associations between sleep and obesity among children and adolescents has produced inconsistent findings.15-22 We attempt to resolve discrepancies in prior research and address new issues through a systematic examination of two waves of data from the National Longitudinal Study of Adolescent Health (Add Health) – a large, nationally representative, and diverse sample of U.S. adolescents.
Three aims guide our investigation: First, we examine the functional form of the relation between sleep and body mass. Although several studies of children have found negative linear associations between sleep duration and body mass,14-16, 19 others have detected U-shaped associations,18 or no association at all.23 We test linear and non-linear specifications to examine the functional form that best describes the association in our large, nationally representative sample.
Second, we examine whether differences in sleep duration account for a portion of ethnic disparities in obesity. There are considerable differences in the prevalence of obesity among ethnic groups,3 which tend to widen considerably in young adulthood.24, 25 There are also persistent ethnic disparities in sleep.26-30 Among adults, non-Hispanic blacks and Hispanics are more likely than non-Hispanic whites to report sleeping 6 or fewer hours each night.31, 32 Black children also receive less nighttime sleep than white children,27, 30, 33 and are at higher risk for sleep-disordered breathing.34, 35 The odds of going to bed at 11 p.m. or later are 4.8 times higher among minority schoolchildren than nonminority schoolchildren.26 In early childhood, minority children have later bedtimes than non-Hispanic white children, and also have lower odds of having regular bedtimes and bedtime routines.36
Third, we investigate whether the relation between sleep and body mass varies by sex and ethnicity. Some studies have failed to detect sex differences in the association between sleep duration and body mass,21 or have detected associations only among females,37 but most have reported stronger effects for males than females,15, 16, 19 including a recent analysis of a subsample of Add Health data.15 To date, most studies have not considered the influence of demographic variables such as ethnicity in their assessment of the association between sleep and body mass,23 and those that do tend to treat such variables as potential confounders. While it is true that ethnicity could confound the association between sleep and body mass, it is also possible that this association varies across ethnic groups.38 To our knowledge, our study is the first to assess this possibility in a large, nationally representative data source that contains sufficient data across four major ethnic subgroups.
METHODS
Data
After receiving approval for our research from relevant institutional review boards, we obtained restricted-use data from the National Longitudinal Study of Adolescent Health (Add Health). Unlike public releases of Add Health, which protect confidentiality by removing certain variables as well as a random subset of half the participants, restricted-use data include complete information from all participants. Our rationale for utilizing restricted-use data was its considerable statistical power—a vital feature of our study, as discussed below.
For over a decade, Add Health has gathered health information from a large, nationally representative sample of adolescents.39 In the initial data collection effort, over 90 000 students in grades 7-12 from 132 schools were administered a brief in-school questionnaire. Within each school, about 17 students were randomly selected from strata arranged by grade and sex to participate in home-based interviews. Between the core sample and various subsamples, 20 746 adolescents participated in the Wave 1 in-home interviews, which were conducted in 1995. In 1996 (Wave 2), Add Health investigators re-interviewed 14 738 adolescents who were still in middle or high school. Although Add Health now offers additional waves of data, participants in them have aged into adulthood and beyond our target population.
Because we examined associations between sleep duration and BMI by sex among a diverse set of ethnic groups, we sought to maximize statistical power in our analyses by pooling observations from the Wave 1 and Wave 2 in-home interviews into a single cross-section of data. Although pooling two waves of data does not fully exploit the longitudinal features of Add Health, it is most appropriate for our research questions for two reasons: First, in general, considerable statistical power is required to detect statistical interactions (here, differences in sleep-BMI associations among ethnic subsamples). The sample size for the pooled data is more than twice as large as longitudinal analyses of Waves 1 and 2, thereby preserving our ability to detect ethnic differences—a key aim of our analyses. Second, only one year elapses between Waves 1 and 2, providing a limited timespan for BMI to change substantially in response to sleep duration patterns. Separate analyses (not shown) found broadly similar results when predicting Wave 2 BMI with Wave 1 sleep duration, but much larger standard errors due to the reduced sample size. The large sample provided by pooling Waves 1 and 2, the population-based sampling frame, and the oversample of minority ethnic groups in Add Health supported our research aims.
Measures
The outcome of interest in our study is body mass index (BMI = kg/m2). Studies of children and adolescents in the U.S. typically make use of BMI charts that are standardized by age and sex.40 We explored that approach, but opted instead to model BMI values rather than standardized scores because (1) we control for variables (age and sex) that influence BMI percentiles, and (2) results are broadly similar.
Wave 2 included both self-reports and direct measures of height and weight, which made the calculation of measured BMI straightforward. Correlations between reported and measured BMI ranged between 0.89 to 0.93 (p < 0.0001) for each sex/ethnicity group in our sample, permitting us to create simple regression equations that correct for small biases in reported BMI (mean differences between reported and measured BMI are < |0.5| for each sex/ethnicity group), as described elsewhere.5 After deriving correction equations from Wave 2, we applied them to Wave 1 data, which only provided self-reports of height and weight.
Main Predictors
The main predictor in our study is self-reported sleep duration, measured as the number of hours of sleep during a typical weeknight. The majority of U.S. adolescents sleep between 4 and 12 hours per night. Over 99% of Add Health participants reported sleep durations in this range, and 87% reported sleeping between 6 and 9 hours.
Because we focus on differential effects of sleep on BMI by sex and ethnicity, these variables are also important predictors in our analyses. We created two- and three-way interaction terms by sleep duration, sex, and ethnicity. In our study, sex is a dichotomous variable, and we divided ethnicity into four groups: non-Hispanic white (white), non-Hispanic black (black), Hispanic, and non-Hispanic Asian (Asian).
Covariates
Physical development affects both BMI and sleep requirements among adolescents. Therefore, we included measures of age and pubertal status. We treated age as a continuous variable, and pubertal status as a simple dichotomous variable (onset of menses for girls and voice changes for boys).
Sample Inclusion Criteria and Missing Data
Inclusion in our final sample was conditional on ethnicity and pregnancy status. Because adolescents from “other” ethnic groups were relatively few in number (n=616) in the pooled data, we excluded them from our analyses. We also excluded girls who have ever been pregnant (n=1305) as this can alter BMI and sleep patterns. This yielded a sample of 30 133 observations for our analyses.
A small number of outliers for BMI (BMI z-score > |5|) and usual sleep duration (less than 4 or more than 12 hours) were treated as missing data. When combined with item nonresponse, 669 adolescents had missing data on BMI and 230 had missing data on sleep duration. In addition, 444 lacked data on pubertal status and 8 had no information on age. The total number of adolescents with missing data on one or more of these variables was 1227, constituting 4.1% of our sample.
Analyses
Despite the small amount of missing data, we conducted multiple imputation analyses in SAS using the fully conditional specification (FCS) option to preserve our sample size. Multiple imputation methods assume that data are missing at random (MAR), conditional on observed variables, a weaker (i.e., more plausible) assumption than is made by listwise deletion.41 The plausibility of the MAR assumption improves with the inclusion of variables in the imputation model that are (1) seldom missing, and (2) correlated with other variables in the analysis; thus, we incorporated a global measure of self-rated health into our imputation models. To account for non-independence of observations in the pooled data, we clustered on individual identifiers in each set of analyses. We also accounted for Add Health's complex survey design through the SURVEYMEANS and SURVEYREG procedures in SAS (see Chantala for details).42
Our analyses proceeded in four steps: First, we evaluated the functional form of the association between sleep duration and BMI by evaluating linear and quadratic terms for sleep. Second, we estimated baseline models that include physical development, sex and ethnicity. Third, we introduced sleep to evaluate the extent to which it mediates associations between ethnicity and BMI. Fourth, we examined two- and three-way interaction terms to determine whether the effect of sleep varies for girls and boys from different ethnic groups. Changes in model fit were evaluated through partial F-tests.43
RESULTS
Sample characteristics are presented in Table 1. A large number of boys and girls are in each ethnic subgroup, facilitating our study aims. Consistent with previous research, ethnic disparities in BMI, overweight and obesity are more pronounced among girls than boys. For instance, over 17% of black girls are obese, compared to just 2.9% of Asian girls. Disparities in sleep duration are somewhat less pronounced, with whites and Hispanics generally reporting longer sleep than blacks and Asians. More than 3 out of every 4 adolescents report less than the recommended 9 hours of sleep per night. Mean age differences are small but significant across groups; relative to boys, a substantially higher percentage of girls achieved puberty in each ethnic group.
Table 1.
Descriptive Statistics for a Pooled Sample of Participants in Waves 1-2 of the National Longitudinal Study of Adolescent Health
| Girls |
Boys |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| White | Black | Hispanic | Asian | p † | White | Black | Hispanic | Asian | p ‡ | Overall | |
| sample size (n) | 8,188 | 3,132 | 2,481 | 962 | 8,336 | 3,159 | 2,714 | 1,161 | 30,133 | ||
| Body Mass | |||||||||||
| Mean BMI | 22.2 | 24.2 | 23.1 | 20.7 | <.0001 | 22.7 | 23.1 | 23.3 | 22.0 | .0011 | 22.7 |
| Overweight | 21.5% | 37.4% | 30.4% | 13.1% | <.0001 | 26.8% | 25.8% | 30.2% | 21.6% | .0419 | 25.8% |
| Obese | 8.3% | 17.3% | 12.0% | 2.9% | <.0001 | 12.9% | 12.7% | 13.4% | 8.7% | .2098 | 11.4% |
| Sleep Duration | |||||||||||
| Mean hours per night | 7.8 | 7.5 | 7.8 | 7.4 | <.0001 | 7.9 | 7.6 | 7.8 | 7.5 | <.0001 | 7.8 |
| Very short (<7 hours) | 15.1% | 25.4% | 15.5% | 23.5% | <.0001 | 13.0% | 21.4% | 16.1% | 18.8% | <.0001 | 15.9% |
| Short (7-8 hours) | 61.5% | 55.0% | 58.7% | 57.3% | .0002 | 59.6% | 58.4% | 58.3% | 63.8% | .3652 | 59.7% |
| Physical Development | |||||||||||
| Mean age | 15.9 | 16.1 | 16.0 | 16.3 | <.0001 | 16.2 | 16.5 | 16.4 | 16.3 | <.0001 | 16.1 |
| Pubescent | 91.8% | 91.0% | 89.3% | 85.7% | .0008 | 57.4% | 37.6% | 43.7% | 40.7% | <.0001 | 70.6% |
p-values derived from TEST statement in PROC MIANALYZE for global differences by ethnicity, separately for girls.
p-values derived from TEST statement in PROC MIANALYZE for global differences by ethnicity, separately for boys.
Regression models of BMI do not show quadratic effects of age, or interactions between age and sex – as might be expected from standardized growth charts.40 Consequently, these terms are omitted from Model 1, which presents our baseline analysis (Table 2). Older adolescents and those who have achieved puberty are significantly heavier, on average, than younger and prepubescent adolescents. Boys also have significantly higher BMI than girls. More substantial BMI differences are found across ethnic groups; black and Hispanic adolescents are approximately 1.1 and 0.7 BMI units heavier than white adolescents, on average (p < 0.001 for both groups). Conversely, Asian adolescents are about 1.1 BMI units lighter than whites (p < 0.001).
Table 2.
Effects of Sex, Ethnicity and Sleep Duration on Body Mass Index for Participants in the National Longitudinal Study of Adolescent Health
| MODEL 1 | MODEL 2 | MODEL 3 | |
|---|---|---|---|
| Intercept | 15.57*** (0.50) | 16.73*** (0.60) | 15.89*** (0.70) |
| Age | 0.40*** (0.03) | 0.38*** (0.03) | 0.38*** (0.03) |
| Puberty | |||
| Yes [referent category is prepubescence] | 0.45*** (0.11) | 0.43*** (0.11) | 0.37*** (0.11) |
| Sex | |||
| Male [referent category is female] | 0.32** (0.11) | 0.33** (0.11) | 2.50*** (0.52) |
| Ethnicity | |||
| Black | 1.11*** (0.14) | 1.08*** (0.14) | 0.33 (0.70) |
| Hispanic | 0.74*** (0.17) | 0.74*** (0.17) | 1.42 (0.76) |
| Asian [referent category is White] | −1.06*** (0.19) | −1.09*** (0.19) | −1.45 (1.06) |
| Sleep Duration | −0.10** (0.03) | −0.01 (0.05) | |
| 2-Way Interactions | |||
| Sex by Ethnicity | |||
| Male*Black | −1.67*** (0.28) | ||
| Male*Hispanic | −0.37 (0.34) | ||
| Male*Asian | 0.87* (0.38) | ||
| Sex by Sleep Duration | |||
| Male*Sleep | −0.25*** (0.07) | ||
| Ethnicity by Sleep Duration | |||
| Black*Sleep | 0.21* (0.09) | ||
| Hispanic*Sleep | −0.06 (0.10) | ||
| Asian*Sleep | −0.02 (0.13) | ||
p<0.05
p<0.01
p<0.001
standard errors in parentheses
Our analyses affirm a linear association between sleep and body mass (study aim 1); the quadratic term for sleep duration was not statistically significant in any of our models (results not shown). Models with categorical measures of short (7-8 hours) and very short (<7 hours) sleep are consistent with this finding. Therefore, in Model 2 we estimate only the linear association between sleep duration and BMI (Table 2). This model shows that BMI is 0.1 units lower, on average, with each additional hour of sleep (p < 0.01). However, the significant impact of sleep duration does not attenuate coefficients for ethnicity, indicating that sleep disparities do not mediate ethnic disparities in BMI (study aim 2).
We estimate a series of two- and three-way interaction effects between sex, ethnicity, and sleep duration to evaluate our third study aim (Table 2). Model 3 shows at least one statistically significant coefficient in each two-way cluster of interaction terms, demonstrating that the effects of sleep vary significantly by both sex and ethnicity. Moreover, partial F-tests confirm that the removal of any set of interaction terms (e.g., ethnicity by sleep duration) causes significant deterioration in model fit (results not shown). However, F-tests fail to show that model fit improves with the inclusion of 3-way interaction terms. Therefore, we regard Model 3 as the best fitting model in our analysis.
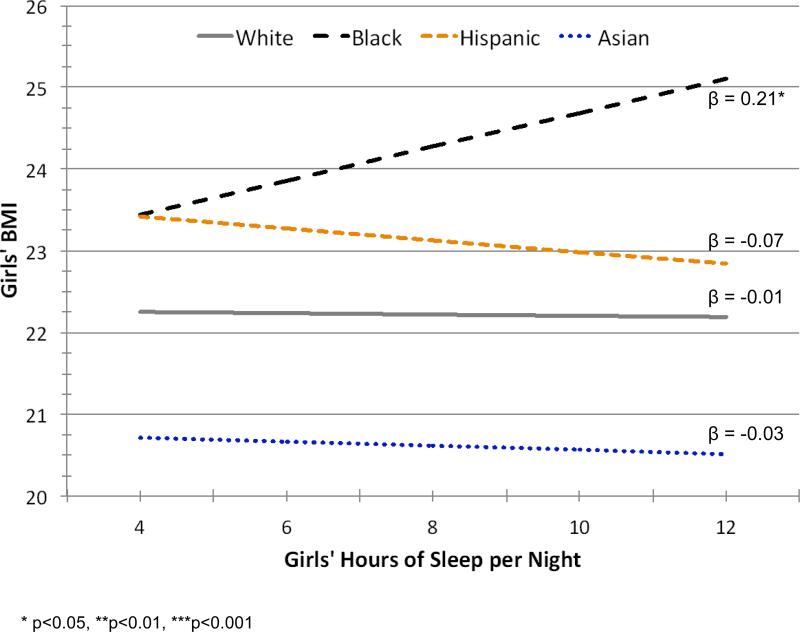
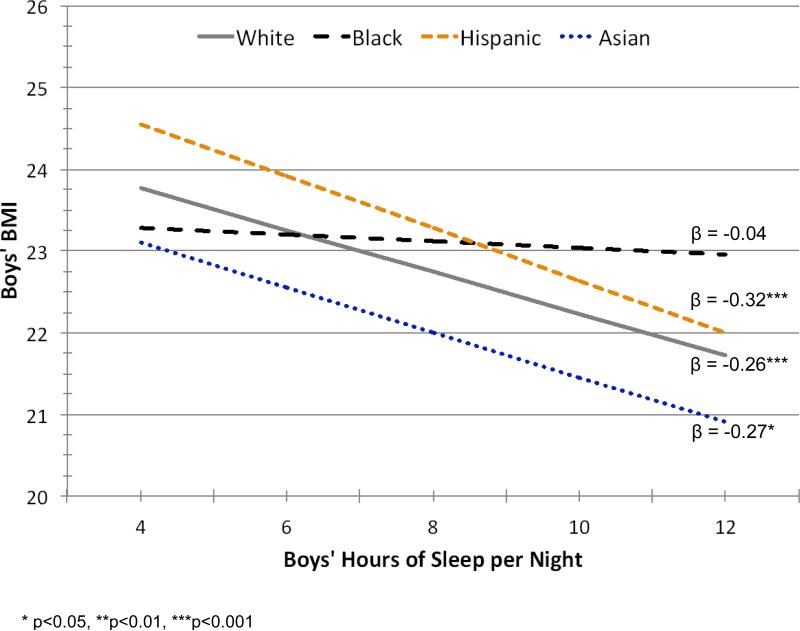
We graph the expected values from Model 3 separately for girls (Figure 1) and boys (Figure 2), where age is fixed at 16 years and puberty is presumed to have occurred. Among girls, only Hispanics and, to a lesser extent, Asians show any indication of lower BMI with more sleep – but these slopes are not statistically significant (p > 0.05). There is essentially no association among white girls and, curiously, a significant positive association between sleep and BMI among black girls (β=0.21; p < 0.05). Among boys, longer sleep duration is associated with sharp and statistically significant declines in BMI for whites, Hispanics and Asians. A negative association is also evident for black boys, but it is much weaker than the association found among boys in other ethnic groups, and it is not statistically significant (p > 0.05).
Figure 1.
Associations between Sleep Duration and Body Mass Index for Girls in the National Longitudinal Study of Adolescent Health
Figure 2.
Associations between Sleep Duration and Body Mass Index for Boys in the National Longitudinal Study of Adolescent Health
DISCUSSION
This study advances prior research on the relation between sleep duration and body mass by using a large, nationally representative sample of U.S. adolescents and focusing on ethnic and sex differences in that association.
Our investigation affirms a negative linear association between sleep duration and body mass in the general U.S adolescent population (study aim 1). This finding is consistent with other studies that have documented negative linear associations between sleep duration and body mass.14-16, 19 Although some researchers have found U-shaped associations18 or null associations,23 we do not find support for a substantial nonlinear relation between sleep duration and body mass in this large sample of adolescents. However, as we discuss below, the slope of the linear association between sleep duration and body mass varies by sex and ethnicity.
Our study also shows that sleep duration does not mediate ethnic differences in body mass (study aim 2). Although there are considerable ethnic disparities in both body mass24, 25 and sleep duration and sleep hygiene26, 27, 33, 44-46 among children and adolescents, we find no evidence that variation in sleep duration across groups accounts for disparities in body mass.
This result may be driven in part by differences in the association between sleep duration and body mass for boys and girls from different ethnic groups (study aim 3). Ethnic disparities in obesity are wider among girls than boys – as confirmed by our descriptive analyses. However, we find that the association between sleep duration and body mass is weak for most girls in the U.S. population, and is positive for black girls. This finding corroborates detection of a significant positive association between sleep duration and adiposity among girls in cross-sectional analyses of a small (n=1171) but population-based urban cohort of adolescents aged 17.47 Contrary to our expectation, this suggests that the higher prevalence of short sleep among non-Hispanic blacks could actually limit the extent of ethnic disparities in body mass. Although the underlying cause of the positive association among black girls is unclear, it is plausible that stress, obesity and related conditions (e.g., depression) are associated with psychiatric hypersomnia and excessive daytime sleepiness (EDS), leading to more total reported sleep time.48, 49
Our study is among the first to evaluate ethnic differences in the association between sleep and body mass – and the first to evaluate such differences in a well-powered analysis of four major ethnic groups in the U.S. population. Differences detected in our study are consistent with a substantial body of research indicating that social categories like ethnicity can modify the effect of risk factors on health outcomes, even where there are clear biological mechanisms at work (e.g., the effect of smoking on mortality).50-52 One possible explanation for this is the Blaxter hypothesis,51, 53 which posits that the wide constellation of disadvantages experienced by ethnic minorities leads to worse health outcomes among those groups, thereby overwhelming the effect of more proximate risk factors. This hypothesis is consistent with our finding that sleep duration is less protective among non-Hispanic blacks than non-Hispanic whites. Our findings are also consistent with research among adults showing that short sleep duration (often defined as <6 hours, as adults require less sleep than adolescents) is more weakly associated with other adverse outcomes, including mortality, among blacks than among whites and Hispanics.51
Despite significant variability in the association between sleep duration and BMI for boys and girls from different ethnic groups, our study broadly affirms prior research showing that sufficient sleep reduces body mass for boys but not girls.15, 16, 19 Researchers documenting sex differences in this association have posited that biological mechanisms may underlie weaker ties between sleep duration and body mass among girls.15, 16, 19 An alternative view is that girls who sleep for short durations may behave differently than their male counterparts. For example, in recent decades, career aspirations, school involvement and academic achievement have increased substantially among girls relative to boys in the U.S. population.54, 55 Research also shows that girls tend to spend more time doing homework and less time playing video games.56 We speculate that systematic differences between boys and girls in health-related behaviors have implications for BMI and weight gain; for instance, short-sleeping girls may be more likely than short-sleeping boys to use additional wake hours to engage in physical activities.
We have noted several strengths of our study, which include a nationally representative sample, excellent statistical power, the inclusion of four major ethnic groups, and a nested-model approach that permits formal comparison of model fit. Further, supplemental analyses (available upon request) found that adjusting for physical activity, a potentially important confounder, does not change the results. There are, however, two important limitations. First, our analyses rely on self-reported sleep duration data. Although some research shows that self-reported sleep duration correlates imperfectly with sleep diaries57 and actigraphy data,58, 59 Wolfson et al. find that self-reported sleep duration among adolescents does not differ significantly from actigraphy or sleep diaries.60 Nevertheless, it would be useful to compare and contrast our findings to analyses based on direct measures of sleep in comparable population-based data sources, but such data sources are not currently available. Second, our ability to detect differences across ethnic groups – a key strength of our study – necessitated that we treat successive waves of Add Health as one cross-section of data. Thus, our analyses do not provide the stronger evidence for causality that a longitudinal design would permit. Although prior research (observational and experimental) provides evidence that favors the viewpoint that a causal relation exists between short sleep and elevated body mass,13, 14 two longitudinal studies suggest that it may not apply to the adolescent population.61
Future research should continue to investigate the association between sleep duration and body mass using longitudinal data,14 with specific interest in identifying whether these associations vary by sex and ethnicity as found in this investigation. Studies could also explore mechanisms that underlie sex and ethnic differences in the association between sleep and body mass. As noted, researchers have surmised that biological factors drive differences between boys and girls; we speculatively add that behavioral factors (e.g., food consumption and patterns of physical activity) are likely important as well. Furthermore, behavioral patterns and structural factors (e.g., peer networks and household characteristics) associated with sleep duration among adolescents62, 63 could account for ethnic differences in sleep-BMI associations. However, additional research is needed to elucidate these mechanisms.
Conclusion
Our study suggests that reducing ethnic disparities in short sleep duration will not attenuate ethnic disparities in body mass. Nevertheless, current evidence suggests that sufficient sleep could help boys from most ethnic groups manage body weight. Indeed, an average reduction in BMI of approximately 0.3 units with each additional hour of sleep is comparable to the effect of organized physical activity (BMI is 0.47 lower with each additional sport/activity) and substantially stronger than the effect of dietary composition among U.S. adolescents.64
Although the latency period between increased sleep and improvements in body mass is presently unclear, adequate sleep is associated with healthy body mass among several groups of adolescents, and it offers a wide range of additional health benefits. For instance, adequate sleep is vital for optimal physical development, immune function, emotional wellbeing and cognitive performance.65-67 Therefore, there is every incentive from a public health perspective to reduce sleep deficits that prevail among a large majority of U.S. adolescents. Even among black girls, where BMI is higher among girls who receive sufficient sleep (at least 9 hours per night) than among girls with sleep deficiencies, risks associated with increased BMI need to be balanced against the health benefits of adequate sleep duration. Pediatricians, parents, and other stakeholders in the health of children and adolescents are now widely aware of the challenges and health risks posed by obesity. It is equally important for us to become attuned to widespread sleep deficiencies and attendant health risks in the U.S. adolescent population, so that we can take proactive measures to ensure that young Americans receive enough sleep to maximize their wellbeing and human potential.
Acknowledgments
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (award number R21DK089414). The authors also gratefully acknowledge the Eunice Kennedy Shriver National Institute of Child Health and Human Development funded University of Colorado Population Center (award number R24 HD066613) for administrative support and the provision of meeting space. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health.
Funding Source: This project was supported by Award Number R21DK089414 from the National Institute of Diabetes and Digestive and Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health.
Footnotes
Conflict of Interest: The authors declare no conflict of interest.
REFERENCES CITED
- 1.McLaren L. Socioeconomic status and obesity. Epidemiol Rev. 2007;29:29–48. doi: 10.1093/epirev/mxm001. [DOI] [PubMed] [Google Scholar]
- 2.Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001;286(10):1195–200. doi: 10.1001/jama.286.10.1195. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295(13):1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 4.Komlos J, Breitfelder A, Sunder M. The transition to post-industrial BMI values among US children. Am J Hum Biol. 2009;21(2):151–60. doi: 10.1002/ajhb.20806. [DOI] [PubMed] [Google Scholar]
- 5.Reither EN, Hauser RM, Yang Y. Do birth cohorts matter? Age-period-cohort analyses of the obesity epidemic in the United States. Soc Sci Med. 2009;69(10):1439–48. doi: 10.1016/j.socscimed.2009.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999-2000. JAMA. 2002;288(14):1728–32. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 7.Liu X, Liu L, Owens JA, Kaplan DL. Sleep patterns and sleep problems among schoolchildren in the United States and China. Pediatrics. 2005;115(1 Suppl):241–9. doi: 10.1542/peds.2004-0815F. [DOI] [PubMed] [Google Scholar]
- 8.Mercer PW, Merritt SL, Cowell JM. Differences in reported sleep need among adolescents. J Adolesc Health. 1998;23(5):259–63. doi: 10.1016/s1054-139x(98)00037-8. [DOI] [PubMed] [Google Scholar]
- 9.Smaldone A, Honig JC, Byrne MW. Sleepless in America: inadequate sleep and relationships to health and well-being of our nation's children. Pediatrics. 2007;119(Suppl 1):S29–37. doi: 10.1542/peds.2006-2089F. [DOI] [PubMed] [Google Scholar]
- 10.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998;69(4):875–87. [PubMed] [Google Scholar]
- 11.Van Cauter E, Knutson KL. Sleep and the epidemic of obesity in children and adults. Eur J Endocrinol. 2008;1591(Suppl):S59–66. doi: 10.1530/EJE-08-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Science Foundation . 2006 Sleep in America Poll. National Sleep Foundation; Washington, DC: 2006. [Google Scholar]
- 13.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring) 2008;16(3):643–53. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Magee L, Hale L. Longitudinal associations between sleep duration and subsequent weight gain: A systematic review. Sleep Med Rev. 2011 doi: 10.1016/j.smrv.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Knutson KL. Sex differences in the association between sleep and body mass index in adolescents. J Pediatr. 2005;147(6):830–4. doi: 10.1016/j.jpeds.2005.07.019. [DOI] [PubMed] [Google Scholar]
- 16.Lytle LA, Pasch KE, Farbakhsh K. The Relationship Between Sleep and Weight in a Sample of Adolescents. Obesity. 2011;19(2):324–331. doi: 10.1038/oby.2010.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kong AP, Wing Y-K, Choi KC, Li AM, Ko GTC, Ma RC, et al. Associations of sleep duration with obesity and serum lipid profile in children and adolescents. Sleep Medicine. 2011;12(7):659–665. doi: 10.1016/j.sleep.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 18.Danielsen YS, Pallesen S, Stormark KM, Nordhus IH, Bjorvatn B. The relationship between school day sleep duration and body mass index in Norwegian children (aged 10–12). International Journal of Pediatric Obesity. 2010;5(3):214–220. doi: 10.3109/17477160903473739. [DOI] [PubMed] [Google Scholar]
- 19.Eisenmann JC, Ekkekakis P, Holmes M. Sleep duration and overweight among Australian children and adolescents. Acta Pædiatrica. 2006;95(8):956–963. doi: 10.1080/08035250600731965. [DOI] [PubMed] [Google Scholar]
- 20.Hitze B, Bosy-Westphal A, Bielfeldt F, Settler U, Plachta-Danielzik S, Pfeuffer M, et al. Determinants and impact of sleep duration in children and adolescents: data of the Kiel Obesity Prevention Study. Eur J Clin Nutr. 2008;63(6):739–746. doi: 10.1038/ejcn.2008.41. [DOI] [PubMed] [Google Scholar]
- 21.Drescher AA, Goodwin JL, Silva GE, Quan SF. Caffeine and screen time in adolescence: associations with short sleep and obesity. Journal Of Clinical Sleep Medicine: JCSM: Official Publication Of The American Academy Of Sleep Medicine. 2011;7(4):337–342. doi: 10.5664/JCSM.1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Silva GE, Goodwin JL, Parthasarathy S, Sherrill DL, Vana KD, Drescher AA, et al. Longitudinal association between short sleep, body weight, and emotional and learning problems in Hispanic and Caucasian children. Sleep. 2011;34(9):1197–205. doi: 10.5665/SLEEP.1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hassan F, Davis MM, Chervin RD. No independent association between insufficient sleep and childhood obesity in the National Survey of Children's Health. Journal Of Clinical Sleep Medicine: JCSM: Official Publication Of The American Academy Of Sleep Medicine. 2011;7(2):153–157. [PMC free article] [PubMed] [Google Scholar]
- 24.Gordon-Larsen P, Adair LS, Nelson MC, Popkin BM. Five-year obesity incidence in the transition period between adolescence and adulthood: the National Longitudinal Study of Adolescent Health. Am J Clin Nutr. 2004;80(3):569–75. doi: 10.1093/ajcn/80.3.569. [DOI] [PubMed] [Google Scholar]
- 25.Scharoun-Lee M, Adair LS, Kaufman JS, Gordon-Larsen P. Obesity, race/ethnicity and the multiple dimensions of socioeconomic status during the transition to adulthood: a factor analysis approach. Soc Sci Med. 2009;68(4):708–16. doi: 10.1016/j.socscimed.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spilsbury JC, Storfer-Isser A, Drotar D, Rosen CL, Kirchner LH, Benham H, et al. Sleep behavior in an urban US sample of school-aged children. Arch Pediatr Adolesc Med. 2004;158(10):988–94. doi: 10.1001/archpedi.158.10.988. [DOI] [PubMed] [Google Scholar]
- 27.Crosby B, LeBourgeois MK, Harsh J. Racial differences in reported napping and nocturnal sleep in 2- to 8-year-old children. Pediatrics. 2005;115(1 Suppl):225–32. doi: 10.1542/peds.2004-0815D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Milan S, Snow S, Belay S. The context of preschool children's sleep: racial/ethnic differences in sleep locations, routines, and concerns. J Fam Psychol. 2007;21(1):20–8. doi: 10.1037/0893-3200.21.1.20. [DOI] [PubMed] [Google Scholar]
- 29.Jenni OG, O'Connor BB. Children's sleep: an interplay between culture and biology. Pediatrics. 2005;115(1 Suppl):204–16. doi: 10.1542/peds.2004-0815B. [DOI] [PubMed] [Google Scholar]
- 30.McLaughlin Crabtree V, Beal Korhonen J, Montgomery-Downs HE, Faye Jones V, O'Brien LM, Gozal D. Cultural influences on the bedtime behaviors of young children. Sleep Med. 2005;6(4):319–24. doi: 10.1016/j.sleep.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 31.Krueger PM, Friedman EM. Sleep duration in the United States: a cross-sectional population-based study. Am J Epidemiol. 2009;169(9):1052–63. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30(9):1096–103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lavigne JV, Arend R, Rosenbaum D, Smith A, Weissbluth M, Binns HJ, et al. Sleep and behavior problems among preschoolers. J Dev Behav Pediatr. 1999;20(3):164–9. doi: 10.1097/00004703-199906000-00005. [DOI] [PubMed] [Google Scholar]
- 34.Redline S, Tishler PV, Schluchter M, Aylor J, Clark K, Graham G. Risk factors for sleep-disordered breathing in children. Associations with obesity, race, and respiratory problems. Am J Respir Crit Care Med. 1999;159(5 Pt 1):1527–32. doi: 10.1164/ajrccm.159.5.9809079. [DOI] [PubMed] [Google Scholar]
- 35.Spilsbury JC, Storfer-Isser A, Kirchner HL, Nelson L, Rosen CL, Drotar D, et al. Neighborhood disadvantage as a risk factor for pediatric obstructive sleep apnea. J Pediatr. 2006;149(3):342–7. doi: 10.1016/j.jpeds.2006.04.061. [DOI] [PubMed] [Google Scholar]
- 36.Hale L, Berger LM, LeBourgeois MK, Brooks-Gunn J. Social and Demographic Predictors of Preschoolers' Bedtime Routines. Journal of Developmental & Behavioral Pediatrics. 2009;30(5):394–402. doi: 10.1097/DBP.0b013e3181ba0e64. 10.1097/DBP.0b013e3181ba0e64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sun Y, Sekine M, Kagamimori S. Lifestyle and Overweight Among Japanese Adolescents: The Toyama Birth Cohort Study. Journal of Epidemiology. 2009;19(6):303–310. doi: 10.2188/jea.JE20080095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Knutson KL. Association between sleep duration and body size differs among three Hispanic groups. Am J Hum Biol. 2011;23(1):138–41. doi: 10.1002/ajhb.21108. [DOI] [PubMed] [Google Scholar]
- 39.Boonstra H. The ‘Add Health’ Survey: Origins, Purposes and Design. The Guttmacher Report on Public Policy. 2001;4(3):10–12. [Google Scholar]
- 40.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. CDC Growth Charts for the United States: methods and development. Vital Health Stat. 2000;2002;11(246):1–190. [PubMed] [Google Scholar]
- 41.Rubin DB. Multiple Imputation for Nonresponse in Surveys. Wiley; New York: 1987. [Google Scholar]
- 42.Chantala K. Guidelines for Analyzing Add Health Data. University of North Carolina at Chapel Hill; 2006. [Google Scholar]
- 43.Kleinbaum DG, Kupper LL, Nizam A, Muller KE, editors. Applied Regression Analysis and Other Multivariable Methods. Duxbury; Belmont: 1998. [Google Scholar]
- 44.Knutson KL, Lauderdale DS. Sociodemographic and behavioral predictors of bed time and wake time among US adolescents aged 15 to 17 years. J Pediatr. 2009;154(3):426–30. 430, e1. doi: 10.1016/j.jpeds.2008.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Adam EK, Snell EK, Pendry P. Sleep timing and quantity in ecological and family context: a nationally representative time-diary study. J Fam Psychol. 2007;21(1):4–19. doi: 10.1037/0893-3200.21.1.4. [DOI] [PubMed] [Google Scholar]
- 46.Moore M, Kirchner HL, Drotar D, Johnson N, Rosen C, Redline S. Correlates of adolescent sleep time and variability in sleep time: the role of individual and health related characteristics. Sleep Med. 2011;12(3):239–45. doi: 10.1016/j.sleep.2010.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Araujo J, Severo M, Ramos E. Sleep duration and adiposity during adolescence. Pediatrics. 2012;130(5):e1146–54. doi: 10.1542/peds.2011-1116. [DOI] [PubMed] [Google Scholar]
- 48.Vgontzas AN, Bixler EO, Kales A, Criley C, Vela-Bueno A. Differences in nocturnal and daytime sleep between primary and psychiatric hypersomnia: diagnostic and treatment implications. Psychosom Med. 2000;62(2):220–6. doi: 10.1097/00006842-200003000-00013. [DOI] [PubMed] [Google Scholar]
- 49.Vgontzas AN, Bixler EO, Chrousos GP. Obesity-related sleepiness and fatigue: the role of the stress system and cytokines. Annals of the New York Academy of Sciences. 2006;1083:329–44. doi: 10.1196/annals.1367.023. [DOI] [PubMed] [Google Scholar]
- 50.Jackson JS, Knight KM, Refferty JA. Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. American Journal of Public Health. 2010;100(5):933–939. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Krueger PM, Saint Onge JM, Chang VW. Race/ethnic differences in adult mortality: the role of perceived stress and health behaviors. Social Science & Medicine. 2011;73:1312–1322. doi: 10.1016/j.socscimed.2011.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pampel FC, Rogers RG. Socioeconomic status, smoking, and health: a test of competing theories of cumulative advantage. J Health Soc Behav. 2004;45:306–321. doi: 10.1177/002214650404500305. [DOI] [PubMed] [Google Scholar]
- 53.Blaxter M. Health and lifestyles. Tavistock; London: 1990. [Google Scholar]
- 54.Patten E, Parker K. A Gender Reversal On Career Aspirations: Young Women Now Top Young Men in Valuing a High-Paying Career. Pew Research Center; 2012. [Google Scholar]
- 55.Matthews JS, Ponitz CC, Morrison FJ. Early gender differences in self-regulation and academic achievement. Journal of Educational Psychology. 2009;101(3):689–704. [Google Scholar]
- 56.Wight VR, Price J, Bianchi SM, Hunt BR. The time use of teenagers. Soc Sci Res. 2009;38(4):792–809. [Google Scholar]
- 57.Knutson KL, Lauderdale DS. Sleep duration and overweight in adolescents: self-reported sleep hours versus time diaries. Pediatrics. 2007;119(5):e1056–62. doi: 10.1542/peds.2006-2597. [DOI] [PubMed] [Google Scholar]
- 58.Sadeh A, Sharkey KM, Carskadon MA. Activity-based sleep-wake identification: an empirical test of methodological issues. Sleep. 1994;17(3):201–7. doi: 10.1093/sleep/17.3.201. [DOI] [PubMed] [Google Scholar]
- 59.Chambers MJ. Actigraphy and insomnia: a closer look. Part 1. Sleep. 1994;17(5):405–8. discussion 408-10. [PubMed] [Google Scholar]
- 60.Wolfson AR, Carskadon MA, Acebo C, Seifer R, Fallone G, Labyak SE, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26(2):213–6. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- 61.Guidolin M, Gradisar M. Is shortened sleep duration a risk factor for overweight and obesity during adolescence? A review of the empirical literature. Sleep Medicine. 2012;(0) doi: 10.1016/j.sleep.2012.03.016. [DOI] [PubMed] [Google Scholar]
- 62.Mednick SC, Christakis NA, Fowler JH. The Spread of Sleep Loss Influences Drug Use in Adolescent Social Networks. Plos One. 2010;5(3) doi: 10.1371/journal.pone.0009775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Marco CA, Wolfson AR, Sparling M, Azuaje A. Family Socioeconomic Status and Sleep Patterns of Young Adolescents. Behav Sleep Med. 2011;10(1):70–80. doi: 10.1080/15402002.2012.636298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Storey ML, Forshee RA, Weaver AR, Sansalone WR. Demographic and lifestyle factors associated with body mass index among children and adolescents. Int J Food Sci Nutr. 2003;54(6):491–503. doi: 10.1080/09637480310001622350. [DOI] [PubMed] [Google Scholar]
- 65.Dahl RE, Lewin DS. Pathways to adolescent health sleep regulation and behavior. Journal of Adolescent Health. 2002;31(6, Supplement):175–184. doi: 10.1016/s1054-139x(02)00506-2. [DOI] [PubMed] [Google Scholar]
- 66.Ganz FD. Sleep and Immune Function. Critical Care Nurse. 2012;32(2):e19–e25. doi: 10.4037/ccn2012689. [DOI] [PubMed] [Google Scholar]
- 67.Carskadon MA. Sleep difficulties in young people. Arch Pediatr Adolesc Med. 2004;158(6):597–8. doi: 10.1001/archpedi.158.6.597. [DOI] [PubMed] [Google Scholar]