Abstract
Purpose
Decision making regarding cardiopulmonary resuscitation (CPR) is challenging. This study examined the effect of a video decision support tool on CPR preferences among patients with advanced cancer.
Patients and Methods
We performed a randomized controlled trial of 150 patients with advanced cancer from four oncology centers. Participants in the control arm (n = 80) listened to a verbal narrative describing CPR and the likelihood of successful resuscitation. Participants in the intervention arm (n = 70) listened to the identical narrative and viewed a 3-minute video depicting a patient on a ventilator and CPR being performed on a simulated patient. The primary outcome was participants' preference for or against CPR measured immediately after exposure to either modality. Secondary outcomes were participants' knowledge of CPR (score range of 0 to 4, with higher score indicating more knowledge) and comfort with video.
Results
The mean age of participants was 62 years (standard deviation, 11 years); 49% were women, 44% were African American or Latino, and 47% had lung or colon cancer. After the verbal narrative, in the control arm, 38 participants (48%) wanted CPR, 41 (51%) wanted no CPR, and one (1%) was uncertain. In contrast, in the intervention arm, 14 participants (20%) wanted CPR, 55 (79%) wanted no CPR, and 1 (1%) was uncertain (unadjusted odds ratio, 3.5; 95% CI, 1.7 to 7.2; P < .001). Mean knowledge scores were higher in the intervention arm than in the control arm (3.3 ± 1.0 v 2.6 ± 1.3, respectively; P < .001), and 65 participants (93%) in the intervention arm were comfortable watching the video.
Conclusion
Participants with advanced cancer who viewed a video of CPR were less likely to opt for CPR than those who listened to a verbal narrative.
INTRODUCTION
Informing patients about their choices at the end of life is an essential component of high-quality medical care.1–4 However, end-of-life decision making can be challenging and emotionally charged. Physicians often do not effectively inform terminally ill patients about available medical procedures, including cardiopulmonary resuscitation (CPR). Patient comprehension may be hampered by common barriers to decision making, including the inability to realistically envision CPR, variability in the quality of physician counseling, distortions portrayed in the lay media, anxiety about advance care planning, and low health literacy.5–9
Over the last two decades, various decision support tools, including videos, have been created to complement patient-clinician discussions and ensure that patients remain active participants in shared decision making.10–12 These tools help patients make better decisions by providing standardized information regarding treatment options and clarifying benefits and risks of each choice.10,13,14 Videos have the potential to further enhance verbal discussions by providing realistic visual images of treatment options and outcomes.13–15
Our group, the Video Images of Disease for Ethical Outcomes (VIDEO) Consortium, has developed and conducted evaluations of advance care planning video decision support tools for several conditions.16,17 One study involved a single-site, randomized trial of 50 patients with advanced brain cancer.17 We found that patients assigned the video were less likely to opt for CPR and were more informed about their decisions than those given verbal descriptions alone. This pilot work supports the potential efficacy of video support tools for advance care planning. However, to justify widespread implementation, further research is necessary to test their efficacy in a larger, more diverse sample of terminally ill patients with cancer from multiple institutions.
We conducted a randomized controlled trial to evaluate the effectiveness of a CPR video decision support tool among patients with different forms of advanced cancer being treated at oncology centers in different cities. We hypothesized that those viewing the video would be more likely to opt against attempted CPR compared with participants assigned to listen to only a verbal description of CPR. Secondary hypotheses were that participants who viewed the video would have greater knowledge of CPR, that their choices would endure over time, and that random assignment to the video and higher health literacy would be associated with a preference to forgo CPR.
PATIENTS AND METHODS
Setting
The study was performed at the following four outpatient oncology clinics: Boston Medical Center and Massachusetts General Hospital in Boston, Queens Hospital Cancer Center in New York City, and Vanderbilt-Ingram Cancer Center in Nashville. The institutional review board of each center approved the protocol, and all participants provided informed consent.
Study Sample
Consecutive participants were enrolled from April 16, 2009, to January 17, 2012. Eligible patients had to be English-speaking, return patients (ie, not a new consult), and patients with advanced cancer who were aware that the prognosis was less than 1 year as per the oncologist18 (Table 1). Potential participants were identified by the oncologist and research assistant (RA) by reviewing the medical charts of patients with clinic appointments. The RA was either a nurse or physician who underwent standardized training and used structured scripts to administer questionnaires and the verbal narrative of CPR.
Table 1.
Advanced Cancer Eligibility Criteria
| Eligibility Criteria |
|---|
| All patients with the following: |
| Brain cancer |
| Inoperable hepatocellular/bile duct/gallbladder cancer |
| Incurable non–small-cell lung carcinoma |
| Extensive-stage small-cell lung cancer |
| Inoperable mesothelioma |
| Inoperable pancreatic cancer |
| Metastatic gastric cancer |
| Metastatic esophageal cancer |
| Metastatic melanoma |
| Patients with the following if first-line therapy has failed and limited response is expected to second-line therapy |
| Breast cancer |
| Colorectal cancer |
| Head and neck cancer |
| Leukemia |
| Ovarian cancer |
| Prostate cancer |
| Renal cancer |
| Sarcoma |
| Lung cancer |
| Myeloma |
| Lymphoma |
On arrival in the clinic, potential participants were provided with a flier describing the study. During the patients' appointments, their oncologists asked whether they wished to consider participation in the study. The RA met with interested patients after their appointment in a private room to verify eligibility and obtain informed consent. The RA then administered the baseline questionnaire, delivered the verbal narrative describing CPR, and randomly assigned participants to the control or intervention group. Participants in the intervention group were shown the video with the RA present, and all participants completed a postintervention questionnaire. Anyone accompanying the patient was invited to view the video, and the RA and oncologist were available to assess any adverse events.
Random assignments based on a computer-generated scheme were concealed in numbered envelopes and opened by the interviewer after participants heard the verbal description of CPR. Because of the nature of the study, the RA conducting all the in-person procedures at the clinic assessment could not be blinded to participant allocation. Another RA, who was blinded to the random assignment scheme, telephoned participants 6 to 8 weeks after the clinic assessment to reassess CPR preferences.
Verbal Narrative
The verbal narrative describing CPR was read to each patient regardless of random assignment. A panel of clinicians with expertise in oncology (n = 15), critical care (n = 2), palliative care (n = 2), medical ethics (n = 2), health literacy (n = 1), and decision making (n = 1) drafted and edited the narrative in an iterative process. The description was based on a review of the literature and was written with language below an eighth grade reading level.19 The narrative states that “CPR attempts to get your heart to beat again if it stops” and outlines the process, risks, and likelihood of successful resuscitation in patients with advanced cancer (Appendix, online only).
Video Decision Support Tool
The 3-minute video included the same narrative as the verbal description that each participant heard. The development of the video followed a similar iterative process as that of the narrative and involved the same panel of experts. The video includes images of simulated chest compressions and intubation on a mannequin, as well as images of an actual ventilated patient receiving intravenous medicines. The visual scenes were filmed without the use of prompts or stage directions to convey a candid realism in the style known as cinéma vérité.20,21 All filming and editing were performed by the research team (A.E.V., M.K.P.-O., A.D.D., and E.D.A.) following previously published filming criteria.22,23 All patients (or their proxies) included in the video gave informed consent to be filmed, and no actors or special effects were used.
Data Collection and Outcomes
The primary outcome was participants' CPR preferences if their heart should stop beating while hospitalized as determined immediately after exposure to either the verbal narrative alone or the verbal narrative followed by the video. Responses were categorized as “Yes, attempt CPR,” “No, do not attempt CPR,” or “Not sure” (Appendix). CPR preferences were also ascertained during the baseline questionnaire at the initial clinical visit and at 6 to 8 weeks.
Additional baseline data included age, race, sex, educational status, marital status, having an advance directive (health care proxy or living will), and health status (excellent, very good, good, fair, or poor). Cancer type was determined from the participant's chart.
Knowledge about CPR was a secondary outcome and was assessed using three true or false questions and one multiple-choice question, each worth one point (Cronbach's α coefficient = 0.68). Knowledge scores ranged from 0 to 4; higher scores reflect greater knowledge. All questions were used in previous studies (Appendix).17 Knowledge scores were ascertained from the baseline and post–random assignment questionnaires at the clinic assessment.
Health literacy was measured after random assignment using the Rapid Estimate of Adult Literacy in Medicine tool.24 This 2- to 3-minute assessment of medically relevant vocabulary has been validated and correlates well with other measures of literacy. Participants were categorized as ≤ sixth grade, seventh to eighth grade, or ≥ ninth grade.25,26
Participants in the intervention arm were asked about their perceptions of the video (very, somewhat, a little, or not helpful), their comfort watching the images (very, somewhat, or not comfortable or don't know), and whether they would recommend the tool to other patients (definitely, probably, probably not, or definitely not recommend).
Statistical Analysis
Participant characteristics and outcomes were described using proportions for categorical variables and means and standard deviations (SDs) for continuous variables. The primary outcome was participants' CPR preferences as ascertained at the postintervention questionnaire. Preferences were compared between the participants in the intervention arm and participants in the control arm using Pearson's χ2 test with exact P values.
Secondary outcomes included knowledge about CPR and CPR preferences 6 to 8 weeks after the clinic visit (control v intervention). Cochran-Mantel-Haenszel tests were used to compare participants' knowledge scores and change in knowledge scores from baseline to postintervention questionnaires between the two groups.
Bivariate analyses were conducted to determine the association between individual participant characteristics (age, sex, race, education, marital status, advance directive, health status, health literacy, and random assignment group) and preference against CPR using the Pearson exact tests. Factors associated with this outcome at P < .10 in the bivariate analyses were entered into multivariable logistic regression models to identify factors independently associated with preferences against CPR. Participants uncertain about their preferences were combined with those who preferred to have CPR in this analysis, because both groups would generally get CPR. Odds ratios (ORs) and 95% CIs were derived from these analyses.
All reported P values are two-sided; P < .05 was considered statistically significant. The study was designed to detect a 31% relative difference in the proportion of participants choosing to forgo CPR between the two groups assuming the rate was 59% in the verbal group and 84% in the video group. With a target of 150 total patients, the power of the study was estimated to be 90%. Data were analyzed using SAS software, version 9.3 (SAS Institute, Cary, NC).
RESULTS
Participant Flow and Baseline Characteristics
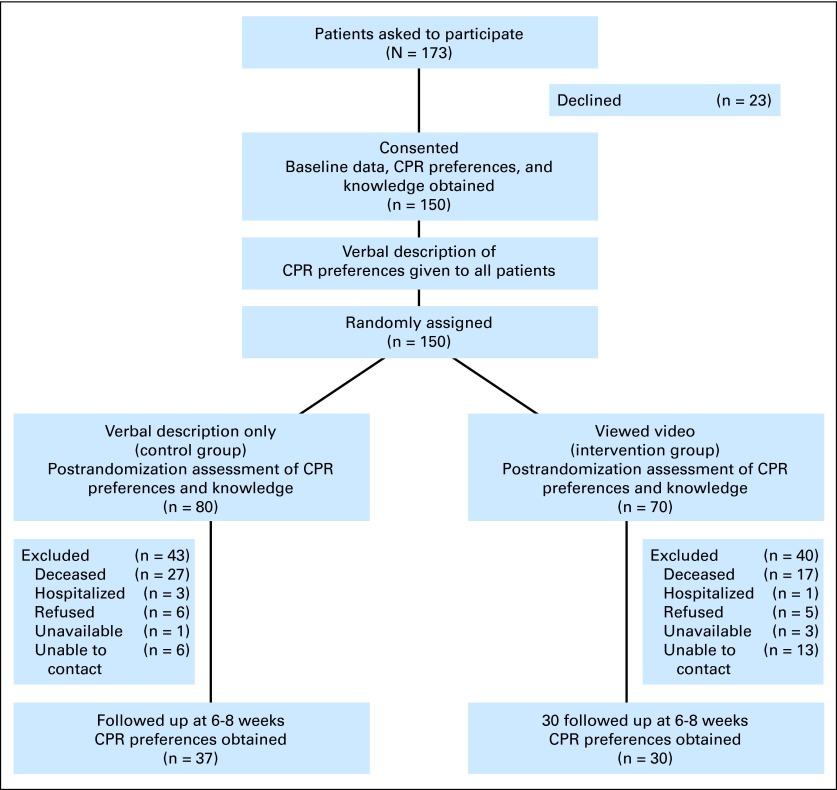
A total of 173 eligible patients were approached to participate, and 150 (87%) were enrolled (Fig 1). Of the 150 enrolled participants, 80 were randomly assigned to the verbal control group and 70 were assigned to the video intervention group. Table 2 lists the demographic and clinical characteristics of the two groups.
Fig 1.
Study flow diagram. CPR, cardiopulmonary resuscitation.
Table 2.
Demographics and Clinical Characteristics of Participants Randomly Assigned to the Verbal and Video Groups
| Characteristic | Verbal Group (n = 80) |
Video Group (n = 70) |
||
|---|---|---|---|---|
| No. of Patients | % | No. of Patients | % | |
| Age, years | ||||
| Mean | 62 | 63 | ||
| Standard deviation | 10 | 13 | ||
| Women | 40 | 50 | 34 | 49 |
| Race | ||||
| American Indian/Native American | 2 | 3 | 0 | 0 |
| Asian | 6 | 8 | 3 | 4 |
| Black or African American | 24 | 30 | 27 | 39 |
| Hispanic or Latino | 6 | 8 | 9 | 13 |
| Other | 0 | 0 | 2 | 3 |
| White (non-Latino) | 42 | 53 | 29 | 41 |
| Education | ||||
| Elementary | 8 | 10 | 6 | 9 |
| Some high school | 15 | 19 | 8 | 11 |
| High school graduate | 21 | 26 | 25 | 36 |
| Some college | 15 | 19 | 17 | 24 |
| College graduate | 13 | 16 | 7 | 10 |
| Postgraduate or professional | 8 | 10 | 7 | 10 |
| Marital status | ||||
| Married or with partner | 42 | 53 | 36 | 51 |
| Widowed | 10 | 13 | 7 | 10 |
| Divorced | 15 | 19 | 11 | 16 |
| Single | 13 | 16 | 16 | 23 |
| Self-reported health status | ||||
| Excellent | 5 | 6 | 4 | 6 |
| Very good | 12 | 15 | 11 | 16 |
| Good | 28 | 35 | 25 | 36 |
| Fair | 29 | 36 | 23 | 33 |
| Poor | 6 | 8 | 7 | 10 |
| Type of cancer* | ||||
| Breast | 11 | 14 | 6 | 9 |
| Colon | 18 | 23 | 17 | 24 |
| Lung | 21 | 26 | 14 | 20 |
| Liver | 6 | 8 | 4 | 6 |
| Prostate | 3 | 4 | 5 | 7 |
| Head and neck | 4 | 5 | 2 | 3 |
| Other | 17 | 20 | 20 | 29 |
| Have an advance directive† | 44 | 55 | 33 | 47 |
Data are missing for two participants in video group.
Participants were asked if they had an advance directive, either a living will or health care proxy. One participant in the video group did not answer the question.
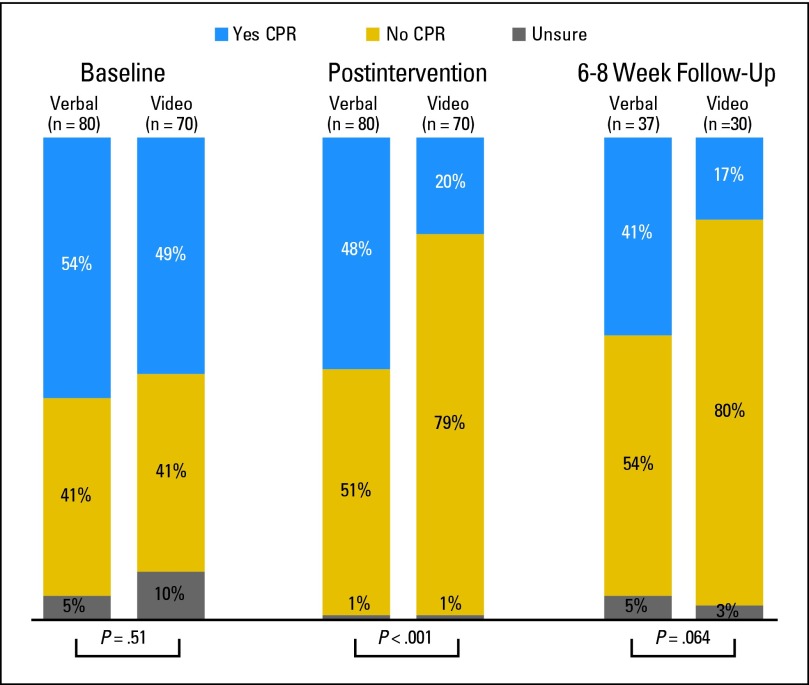
Preferences for CPR
Figure 2 shows baseline CPR preferences between the two groups before random assignment. In the postintervention questionnaire, CPR preferences differed significantly between the two groups. Of the 80 control participants, 38 (48%) preferred to have CPR attempted, 41 (51%) desired not to have CPR attempted, and one (1%) was uncertain. Of the 70 intervention participants, 14 (20%) preferred to have CPR attempted, 55 (79%) desired not to have CPR attempted, and one (1%) was uncertain (P < .001; unadjusted OR, 3.5; 95% CI, 1.7 to 7.2; P < .001).
Fig 2.
Cardiopulmonary resuscitation (CPR) preferences at baseline, after intervention, and at 6 to 8 weeks of follow-up. Exact P values were calculated using Pearson's χ2 tests.
A total of 37 control participants (46%) and 30 intervention participants (43%) were reached for the follow-up telephone interview. Death was the most common reason for the inability to complete the follow-up interview in both groups (Fig 1). Among participants contacted in the control group, 15 (41%) wanted CPR attempted, 20 (54%) opted to forgo CPR, and two (5%) were uncertain. Among participants contacted in the intervention group, five (17%) wanted CPR attempted, 24 (80%) did not want CPR, and one (3%) was uncertain (Fig 2; P = .06).
Knowledge
There were no statistically significant differences in baseline knowledge scores (range, 0 to 4) between the control and intervention groups before random assignment (mean score, 2.1 ± 1.2 v 2.0 ± 1.3, respectively; median score, 2 v 2, respectively; P = .9). However, postintervention knowledge scores differed significantly (control group: mean score, 2.6 ± 1.3; median score, 3; intervention group: mean score, 3.3 ± 1.0; median score, 4; P < .001). The mean increase in postintervention knowledge scores was 0.6 (95% CI, 0.3 to 0.8) for the control group and 1.3 (95% CI, 1.0 to 1.6) for the intervention group.
Predictors of CPR Preferences
In the bivariate analyses, participant characteristics associated with a greater likelihood to forgo CPR at the P < .10 level, as ascertained in the postintervention questionnaire, were female sex (OR, 0.5; 95% CI, 0.3 to 1.02), white race (OR, 2.2; 95% CI, 1.09 to 4.3), random assignment to the intervention arm (OR, 3.5; 95% CI, 1.7 to 7.2), and higher health literacy (seventh to eighth grade v ≤ sixth grade: OR, 3.4; 95% CI, 1.2 to 10.2; ≥ ninth grade v ≤ sixth grade: OR, 4.2; 95% CI, 1.9 to 9.4; Table 3).
Table 3.
Predictors of Postintervention Preferences Against CPR
| Characteristic | Participants Choosing Against CPR |
Unadjusted P* | OR |
||||
|---|---|---|---|---|---|---|---|
| No. | % | Unadjusted OR | 95% CI | Adjusted OR† | 95% CI | ||
| Age, years | |||||||
| < 60 | 36 | 59 | Reference | ||||
| ≥ 60 | 60 | 67 | .30 | 1.4 | 0.7 to 2.8 | ||
| Sex | |||||||
| Female | 53 | 72 | Reference | Reference | |||
| Male | 43 | 57 | .063 | 0.5 | 0.3 to 1.02 | 2.0 | 0.9 to 4.3 |
| Race | |||||||
| Nonwhite | 44 | 56 | Reference | Reference | |||
| White (non-Latino) | 52 | 73 | .028 | 2.2 | 1.09 to 4.3 | 1.5 | 0.6 to 4.0 |
| Education | |||||||
| < College graduate | 70 | 61 | Reference | ||||
| ≥ College graduate | 26 | 74 | .16 | 1.9 | 0.8 to 4.3 | ||
| Marital status | |||||||
| Not married or with partner | 45 | 63 | Reference | ||||
| Married or with partner | 51 | 65 | .74 | 1.1 | 0.6 to 2.2 | ||
| Health status‡ | |||||||
| Fair or poor | 45 | 69 | Reference | ||||
| Good or better | 51 | 60 | .30 | 0.7 | 0.3 to 1.3 | ||
| Advance directive | |||||||
| None | 43 | 60 | Reference | ||||
| Living will/health care proxy | 53 | 69 | .30 | 1.5 | 0.8 to 2.9 | ||
| Intervention | |||||||
| Verbal | 41 | 51 | Reference | Reference | |||
| Video | 55 | 79 | < .001 | 3.5 | 1.7 to 7.2 | 4.7 | 2.1 to 10.7 |
| Health literacy (REALM)§ | |||||||
| ≤ Sixth grade (0-45) | 16 | 40 | Reference | Reference | |||
| Seventh to eighth grades (46-60) | 16 | 70 | .036 | 3.4 | 1.2 to 10.2 | 3.6 | 1.1 to 12.0 |
| ≥ Ninth grade (61-66) | 62 | 74 | < .001 | 4.2 | 1.9 to 9.4 | 3.8 | 1.3 to 10.8 |
Abbreviations: CPR, cardiopulmonary resuscitation; OR, odds ratio; REALM, Rapid Estimate of Adult Literacy in Medicine.
All reported P values are two-sided, with P < .05 considered as statistically significant.
For the multivariable analysis, characteristics were excluded if they were not related to the outcome (P ≥ .10), choosing against CPR.
Health status was one of the following: excellent, very good, good, fair, or poor.
Health literacy was assessed with REALM. Three participants had missing data.
After including these variables in a multivariable logistic regression model, random assignment to the intervention group (adjusted OR [aOR], 4.7; 95% CI, 2.1 to 10.7) and higher health literacy level (seventh to eighth grade v ≤ sixth grade: aOR, 3.6; 95% CI, 1.1 to 12.0; ≥ ninth grade v ≤ sixth grade: aOR, 3.8; 95% CI, 1.3 to 10.8) remained independently associated with a preference to forgo CPR.
Experience With Video
Among the 70 participants in the intervention arm, 51 (73%) found the video to be “very helpful” and 12 (17%) found the video to be “somewhat helpful.” Similarly, 51 participants (73%) were “very comfortable” watching the video and 14 (20%) were “somewhat comfortable.” When asked whether they would recommend the video to other patients, 54 participants (77%) would “definitely recommend,” 14 (20%) would “probably recommend,” and no one would “not recommend” the video. There were no adverse events (eg, emotional distress) in either arm of the study.
DISCUSSION
This study presents an innovative video approach to decision making for patients with advanced cancer. Patients assigned to view a video were less likely to wish for attempted CPR compared with patients who only heard a verbal description of the intervention. Patients who viewed the video also had more accurate knowledge about CPR, and the vast majority were comfortable viewing the visual images. The effect of the video was largely unchanged after controlling for a variety of relevant patient features. In addition, we found that higher health literacy was independently associated with opting against CPR. Videos supplementing verbal discussions may play a significant role in helping patients make more informed treatment decisions at the end of life.
To the best of our knowledge, this study represents the only multisite randomized trial of a video decision support tool for end-of-life decision making among patients with advanced cancer conducted to date. Our prior study conducted in a small group of patients with advanced brain cancer showed similar findings, but the patients were from one site and had a single, relatively rare cancer. The current study extends and builds on this work by demonstrating the efficacy of the video in a randomized controlled trial among patients with diverse cancers from multiple centers.
An essential ingredient of end-of-life decision making is the patient's ability to comprehend and realistically imagine options for medical interventions along with the accompanying risks and benefits. Viewing a video may provide patients with details and information that are not necessarily communicated in verbal descriptions. With the proliferation of visual media, patients are increasingly accustomed to obtaining vital information for decision making from visual images.27,28 The fact that many patients had higher knowledge scores after the video and were comfortable viewing the video bolsters the acceptance of multimedia tools to empower patients and enhance decision making.
An additional finding of our study is the role of health literacy in complex decision making. Our findings suggest that patients with low health literacy may particularly benefit from the use of appropriately designed decision tools to explain medical procedures, which is consistent with prior work,29–31 including in the advance care planning context.16
Our study has limitations that warrant comment. First, the RAs collecting the primary outcome data were not blinded to the random assignment, which is difficult to achieve with a video intervention. Previous randomized trials of advance care planning were also not blinded for similar reasons.5–7 Consequently, to minimize any potential bias, we used scripted interviews and standardized training developed in our prior work. We did, however, measure health literacy after the intervention; some people feel shame as a result of measurement of health literacy, and we did not want this to influence people's experience of the intervention.32
Second, our study included questions regarding patients' knowledge that were not tested for reliability and validation, and we did not explore other aspects of decision quality such as decisional conflict, regret, and anxiety regarding decision making. Whether or not the video impacted the overall quality of patients' decisions is an important area for future study.
Third, hearing the verbal description of CPR again in the video narration may have reinforced preferences and knowledge in the video group. However, if the support tool is adopted into practice, its intent would be to reinforce, not supplant, a verbal discussion with a clinician. Fourth, visual images can be manipulated to steer patients toward a particular decision. To avoid favoring a particular perspective, we extensively previewed the video images with experts and used published filming criteria. Fifth, many patients in both groups died before the 6- to 8-week follow-up interview, which may have limited our ability to detect a statistically significant difference at this time point, but also underscored the severity of their illness. Finally, we surveyed participants' treatment choices in the context of a research study and did not confirm actual care delivery.
Videos supplementing verbal discussions can improve understanding of medical interventions that are difficult to imagine using words. More work needs to be done to standardize and implement these tools across a range of diseases.13,33 As society adapts to the informational power of visual images, clinicians and health care systems can also harness these tools to educate and empower patients. This trial suggests that videos are an important tool to enhance patients' decision making by making sure patients understand CPR and are able to express their preferences at the end of life.
Supplementary Material
Acknowledgment
We thank Daniel E. Singer for his contribution to the project.
Appendix
Verbal Description of Cardiopulmonary Resuscitation
One important decision you will need to make while in the hospital is whether you would want doctors to attempt CPR. CPR tries to get your heart to beat again if it stops. This means pressing on your chest and using an electric shock to attempt to restart your heart. Most of the time in patients with advanced cancer, CPR does not work.
If you want CPR attempted, you would also agree to have a ventilator or breathing machine if you need it to keep breathing. This involves putting a tube down your throat into your lungs and connecting you to a machine that pushes air into your lungs. You cannot eat or talk while on this machine. If you are on a ventilator, you will likely need very strong medicines. These are usually given in the intensive care unit or ICU. CPR will not cure your cancer and in most patients with advanced cancer, CPR does not return you to your previous state of health.
CPR Preference Question
If you were to get so sick that your heart stopped beating, would you want doctors to shock your heart and do chest compressions as part of CPR to try to make your heart start again?
Possible responses:
–No, do not attempt CPR
–Yes, attempt CPR
–Not sure
Knowledge Questions
1. Cardiopulmonary resuscitation or CPR is a medical procedure that is done on patients whose heart stops beating in an attempt to restart their heart.
2. Most patients with advanced cancer that get CPR in the hospital survive and get to leave the hospital.
3. Most patients with advanced cancer who survive CPR and having been placed on a breathing machine have very few complications from these procedures.
Possible responses for questions 1 to 3:
–True
–False
–Not sure
4. How many patients with advanced cancer that get CPR in the hospital survive and get to leave the hospital?
Possible responses:
–Almost all (more than 90%)
–About half (more than 50%)
–Few (less than 10%)
–Not sure
Footnotes
Listen to the podcast by Dr Smith at www.jco.org/podcasts
Written on behalf of the Video Images of Disease for Ethical Outcomes (VIDEO) Consortium.
Supported by Grant No. K08HS018780 from the Agency for Healthcare Research and Quality (A.E.V.) and by a grant from the Informed Medical Decisions Foundation (Research Grant No. 0177-1).
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality or the Informed Medical Decisions Foundation.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
Clinical trial information: NCT01241929.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Although all authors completed the disclosure declaration, the following author(s) indicated a financial or other interest that is relevant to the subject matter under consideration in this article. Certain relationships marked with a “U” are those for which no compensation was received; those relationships marked with a “C” were compensated. For a detailed description of the disclosure categories, or for more information about ASCO's conflict of interest policy, please refer to the Author Disclosure Declaration and the Disclosures of Potential Conflicts of Interest section in Information for Contributors.
Employment or Leadership Position: Michael J. Barry, Informed Medical Decisions Foundation (C) Consultant or Advisory Role: None Stock Ownership: None Honoraria: None Research Funding: None Expert Testimony: None Other Remuneration: None
AUTHOR CONTRIBUTIONS
Conception and design: Angelo E. Volandes, Michael K. Paasche-Orlow, Susan L. Mitchell, Areej El-Jawahri, Aretha Delight Davis, Michael J. Barry, Lenny López, Elmer D. Abbo, April F. Eichler, Andrew S. Epstein, Ariela Noy, Tomer T. Levin, Jennifer S. Temel
Financial support: Angelo E. Volandes
Administrative support: Angelo E. Volandes, Michael K. Paasche-Orlow
Provision of study materials or patients: Angelo E. Volandes, Kevan L. Hartshorn, Matt Peachey
Collection and assembly of data: Areej El-Jawahri, Kevan L. Hartshorn, Elizabeth S. Walker-Corkery, Margaret Kemeny, Linda Bulone, Eileen Mann, Sumi Misra, Matt Peachey, April F. Eichler, Tomer T. Levin
Data analysis and interpretation: Michael K. Paasche-Orlow, Areej El-Jawahri, Vicki Ann Jackson, Muriel R. Gillick, Yuchiao Chang, Lenny López, Elmer D. Abbo, April F. Eichler, Andrew S. Epstein, Tomer T. Levin, Jennifer S. Temel
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
- 1.Council on Scientific Affairs,; American Medical Association. Good care of the dying patient: JAMA. 1996;275:474–478. [PubMed] [Google Scholar]
- 2.Institute of Medicine: Washington, DC: National Academy Press; 2003. Crossing the quality chasm, in Richard and Hinda Rosenthal Lectures 2001. [Google Scholar]
- 3.Lynn J. Measuring quality of care at the end of life: A statement of principles. J Am Geriatr Soc. 1997;45:526–527. doi: 10.1111/j.1532-5415.1997.tb05184.x. [DOI] [PubMed] [Google Scholar]
- 4.Lo B, Snyder L. Care at the end of life: Guiding practice where there are no easy answers. Ann Intern Med. 1999;130:772–774. [PubMed] [Google Scholar]
- 5.A controlled trial to improve care for seriously ill hospitalized patients: The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT)—The SUPPORT Principal Investigators. JAMA. 1995;274:1591–1598. [PubMed] [Google Scholar]
- 6.Hofmann JC, Wenger NS, Davis RB, et al. Patient preferences for communication with physicians about end-of-life decisions: SUPPORT Investigators—Study to Understand Prognoses and Preference for Outcomes and Risks of Treatment. Ann Intern Med. 1997;127:1–12. doi: 10.7326/0003-4819-127-1-199707010-00001. [DOI] [PubMed] [Google Scholar]
- 7.Covinsky KE, Fuller JD, Yaffe K, et al. Communication and decision-making in seriously ill patients: Findings of the SUPPORT project—The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Am Geriatr Soc. 2000;48(suppl):S187–S193. doi: 10.1111/j.1532-5415.2000.tb03131.x. [DOI] [PubMed] [Google Scholar]
- 8.Tulsky JA, Fischer GS, Rose MR, et al. Opening the black box: How do physicians communicate about advance directives? Ann Intern Med. 1998;129:441–449. doi: 10.7326/0003-4819-129-6-199809150-00003. [DOI] [PubMed] [Google Scholar]
- 9.Diem SJ, Lantos JD, Tulsky JA. Cardiopulmonary resuscitation on television: Miracles and misinformation. N Engl J Med. 1996;334:1578–1582. doi: 10.1056/NEJM199606133342406. [DOI] [PubMed] [Google Scholar]
- 10.Barry MJ. Health decision aids to facilitate shared decision making in office practice. Ann Intern Med. 2002;136:127–135. doi: 10.7326/0003-4819-136-2-200201150-00010. [DOI] [PubMed] [Google Scholar]
- 11.Stacey D, Bennett CL, Barry MJ, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2011;10:CD001431. doi: 10.1002/14651858.CD001431.pub3. [DOI] [PubMed] [Google Scholar]
- 12.Stacey D, Samant R, Bennett C. Decision making in oncology: A review of patient decision aids to support patient participation. CA Cancer J Clin. 2008;58:293–304. doi: 10.3322/CA.2008.0006. [DOI] [PubMed] [Google Scholar]
- 13.Elwyn G, Frosch D, Volandes AE, et al. Investing in deliberation: A definition and classification of decision support interventions for people facing difficult health decisions. Med Decis Making. 2010;30:701–711. doi: 10.1177/0272989X10386231. [DOI] [PubMed] [Google Scholar]
- 14.Frosch DL, Kaplan RM. Shared decision making in clinical medicine: Past research and future directions. Am J Prev Med. 1999;17:285–294. doi: 10.1016/s0749-3797(99)00097-5. [DOI] [PubMed] [Google Scholar]
- 15.Elwyn G, O'Connor AM, Bennett C, et al. Assessing the quality of decision support technologies using the International Patient Decision Aid Standards instrument (IPDASi) PLoS One. 2009;4:e4705. doi: 10.1371/journal.pone.0004705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Volandes AE, Paasche-Orlow MK, Barry MJ, et al. Video decision support tool for advance care planning in dementia: Randomised controlled trial. BMJ. 2009;338:b2159. doi: 10.1136/bmj.b2159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.El-Jawahri A, Podgurski LM, Eichler AF, et al. Use of video to facilitate end-of-life discussions with patients with cancer: A randomized controlled trial. J Clin Oncol. 2010;28:305–310. doi: 10.1200/JCO.2009.24.7502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Glare P, Christakis NA. New York, NY: Oxford University Press; 2008. Prognosis in Advanced Cancer. [Google Scholar]
- 19.Kincaid J, Fishburne R, Rogers R, et al. Memphis, TN: Memphis Naval Air Station; 1975. Derivation of New Readability Formulas (Automated Readability Index, Fog Count, and Flesch Reading Ease Formula) for Navy Enlisted Personnel. [Google Scholar]
- 20.Volandes AE, Barry MJ, Wood F, et al. Audio-video decision support for patients: The documentary genre as a basis for decision aids. Health Expect. doi: 10.1111/j.1369-7625.2011.00727.x. 10.1111/j.1369-7625.2011.00727.x [epub ahead of print on October 28, 2011] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grant BK, Sloniowski J. Detroit, MI: Wayne State University Press; 1998. Documenting the Documentary: Close Readings of Documentary Film and Video. [Google Scholar]
- 22.Volandes A, El-Jawahri A. Hauppauge, NY: Nova Science Publishers; 2012. Improving CPR decision-making for patients and families with video decision aids, in Doyle L, Saltsman R (eds): Cardiopulmonary Resuscitation: Procedures and Challenges. [Google Scholar]
- 23.Gillick MR, Volandes AE. New York, NY: Nova Science Publishers; 2007. The psychology of using and creating video decision aids for advance care planning, in Lynch TE (ed): Psychology of Decision Making in Medicine and Health Care; pp. 193–206. [Google Scholar]
- 24.Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: A shortened screening instrument. Fam Med. 1993;25:391–395. [PubMed] [Google Scholar]
- 25.Paasche-Orlow MK, Parker RM, Gazmararian JA, et al. The prevalence of limited health literacy. J Gen Intern Med. 2005;20:175–184. doi: 10.1111/j.1525-1497.2005.40245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davis TC, Wolf MS, Bass PF, 3rd, et al. Literacy and misunderstanding prescription drug labels. Ann Intern Med. 2006;145:887–894. doi: 10.7326/0003-4819-145-12-200612190-00144. [DOI] [PubMed] [Google Scholar]
- 27.Mayer RE. ed 2. New York, NY: Cambridge University Press; 2009. Multimedia Learning. [Google Scholar]
- 28.Mayer RE. Cambridge, United Kingdom: Cambridge University Press; 2005. The Cambridge Handbook of Multimedia Learning. [Google Scholar]
- 29.Smith SK, Trevena L, Simpson JM, et al. A decision aid to support informed choices about bowel cancer screening among adults with low education: Randomised controlled trial. BMJ. 2010;341:c5370. doi: 10.1136/bmj.c5370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Holmes-Rovner M, Stableford S, Fagerlin A, et al. Evidence-based patient choice: A prostate cancer decision aid in plain language. BMC Med Inform Decis Mak. 2005;5:16. doi: 10.1186/1472-6947-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miller DP, Jr, Spangler JG, Case LD, et al. Effectiveness of a web-based colorectal cancer screening patient decision aid: A randomized controlled trial in a mixed-literacy population. Am J Prev Med. 2011;40:608–615. doi: 10.1016/j.amepre.2011.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paasche-Orlow M. Caring for patients with limited health literacy: A 76-year-old man with multiple medical problems. JAMA. 2011;306:1122–1129. doi: 10.1001/jama.2011.1203. [DOI] [PubMed] [Google Scholar]
- 33.Elwyn G, O'Connor A, Stacey D, et al. Developing a quality criteria framework for patient decision aids: Online international Delphi consensus process. BMJ. 2006;333:417. doi: 10.1136/bmj.38926.629329.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.