Abstract
Objectives: To compare the value of transvaginal ultrasonographic measurement of the cervical length versus the Bishop score, prior to induction of labour, in predicting the mode of delivery within four days.
Materials and Methods: This longitudinal study included 110 women (at term, singleton, vertex presentation) in whom induction of labour was performed at 37-42 weeks of gestation. Cervical length on transvaginal ultrasound and the Bishop score were assessed prior to induction according to standard protocol. Medical records were reviewed for relevant demographic and clinical data.
Primary outcome criterion was successful vaginal delivery within 96 h. Univariate analyses and receiver operating characteristic (ROC) curves were used to examine differences between variables possibly predicting outcome.
Results: Of the 110 women 66 were nulliparous and 44 multiparous. Vaginal delivery within 96 h was successful in 48 (73%) nulliparous and in 40 (91%) multiparous women ( i.e. in 80% of the total population). The overall rate of caesarean delivery was 17%.
There was a significant difference between nulliparous and multiparous women in age, cervical length (mean in mm in nulliparous women: 29.31, range: 5.00-56.00; in multiparous women: 37.04, range: 12.00-56.00), Bishop score and successful induction, but no significant difference between these subgroups in neonatal outcomes.
Only the Bishop score in nulliparous women showed a significant relationship between this variable and predicting successful labour induction (area under the ROC curve 0.679; standard error 0.73; p < 0.05; 95% CI: 0.536-0.823).
The best cut-off value for the Bishop score was 3, with a sensitivity of 56.3% and a specificity of 72.2%.
Conclusion: In this study group significant independent prediction of vaginal delivery within 96 h is provided by the Bishop score but only in nulliparous women. Transvaginal ultrasonographic measurement of cervical length is not a significant independent predictor of vaginal delivery within 96 h.
Keywords: Bishop score, cervical length, induction of labour, term pregnancy, transvaginal ultrasonography, vaginal delivery
Introduction
Induction of labour is performed in about 20% of all pregnancies and successful induction is reported to be related to cervical characteristics, or ‘ripeness’ (Pandis et al., 2001; Laencina et al., 2007; Vrouenraets et al.,2005).
Although cervical ripeness can be established with the Bishop score, this frequently used method shows a high inter-and intra-observer variability (Laencina et al., 2007; Vrouenraets et al., 2005; Bishop, 1964). Alternatively, transvaginal ultrasonographic measurement of cervical length may be a more objective method for assessing cervical status (Pandis et al., 2001; Rozenberg, 1999; Roman et al., 2004).
In women undergoing total hysterectomy Jackson et al. measured cervical length preoperatively both digitally and by transvaginal ultrasound. After surgery, for comparison purposes, cervical length was measured with a ruler; it appeared that digital examination significantly underestimated cervical length by an average of 13.6 mm compared with the ruler measurement ( Jackson et al., 1992).
Birth by caesarean delivery is generally more hazardous than a normal vaginal delivery (Yeast et al., 1999), or at least poses more risks for subsequent pregnancies (Kwee et al.,2007). Therefore, we hypothesized that prediction of the success rate of induction of labour might lead to a reduction in caesarean delivery and thereby its complications.
Results of studies comparing the usefulness of the Bishop score versus transvaginal cervical ultrasonography in predicting the success of labour induction are conflicting (Pandis et al., 2001; Tan et al., 2007; Strobel et al., 2006; Rozenberg et al., 2005; Rane et al., 2003).
Moreover, most of these studies used different induction strategies (mostly a 24-hour period) and various definitions of ‘success’ were used.
The present longitudinal study explores the use of transvaginal ultrasonographic measurement of cervical length versus the Bishop score, prior to induction, to predict the mode of delivery within 4 days (96 hours).
Materials and Methods
Preinduction cervical assessment was undertaken in 110 women who were included in this study from March 2007 through December 2007. Inclusion criteria were: singleton pregnancy, live fetus in cephalic presentation, and undergoing induction of labour at 37 to 42 weeks of gestation (gestational age determined by ultrasound fetometry) for a variety of indications; PROM > 48 h, HELLP syndrome or pre-eclampsia, diabetes maternal or gravity related, prolonged pregnancy, restricted intra-uterine fetal growth, amniotic fluid problems, elective inductions and gestational cholestasis.
Exclusion criteria were: any reason for priming and/or contra-indication for induction of labour: suspicion of fetal distress at admission, previous history of uterine surgery or contra-indications for prostaglandins or vaginal delivery.
The attending obstetrician performed a digital examination of the cervix and noted the Bishop score on a dedicated study form. To calculate ripeness of the cervix, Bishop scores were scored separately for nulliparous and multiparous women, according to the guidelines of the Dutch Society of Obstetrics and Gynaecology (Table I).
Table I. Bishop scores for nulliparous women (N-score) versus multiparous women (M-score).
| N- score | |||
|---|---|---|---|
| Components | Score | ||
| 0 | 1 | 2 | |
| Consistency | firm | medium | soft |
| Cervical position | posterior | mid | anterior |
| Effacement of cervix | 0% | 0%-100% | 100% |
| Degree of dilatation | < 1 cm | 1-2 cm | > 2 cm |
| Station of presenting part | < Hodge 2 | Hodge 2-3 | > Hodge 3 |
| M-score | |||
| Components | Score | ||
| 0 | 1 | 2 | |
| Degree of dilatation | < 1 cm | 1-2 cm | > 2 cm |
| Station of presenting part | < Hodge 1 | Hodge 1-2 | > Hodge 2 |
The score used for nulliparous women has the components: consistency, cervical position, effacement of the cervix, degree of dilatation, and station of the presenting part (range 0-10); for multiparous women the score components are: degree of dilatation, and station of the presenting part (range 0-4).
Cervical length was then measured by a transvaginal ultrasound scanner (Hitachi EUB-5500, Japan) with a 10 MHz V53W R10 probe . All ultrasound measurements were carried out according to standard protocol: i.e. women are examined in a dorsal lithotomy position with an empty urinary bladder. Once the cervical canal is identified the probe is withdrawn slightly so there is no pressure of the tip of the probe on the cervix. A sagittal plane through the cervix is identified where the external cervical os, the cervical canal and the internal cervical os is visible. The length of the cervix is measured from the outer to the inner cervical os as a straight line. It is important to include only that part of the cervical canal that is bordered by the endocervical mucosa.
Induction of labour was also carried out according to standard protocol. The agents used for induction were dinoprostone gel on the first 2 days and, if necessary, misoprostol tablets intravaginal on the third or fourth day. Digital examination was made 5 h after the first intravaginal administration; if necessary, a second dose of dinoprostone was then administered. The maximum dose of dinoprostone in 24 h was 3 mg given in two doses. On the third and fourth day a maximum of 75 µg misoprostol in 24 h could be applied intravaginally in three doses at intervals of 4 h.
External cardiotocography was regularly performed to monitor the condition of the fetus.
Onset of labour was defined as the time when cervical dilatation reached at least 3 cm with completed cervical effacement. Continuous (internal) cardiotocography was used in all cases. If necessary, amniotomy was performed. Intravenous oxytocin administration was started when there was an arrest of dilatation, according to the hospital protocol. For analgesia, intramuscular pethidine and/or epidural anaesthesia was offered.
In the present study, successful outcome was defined as induction resulting in vaginal delivery within 96 h. The need for caesarean delivery for presumed fetal distress (e.g. abnormal fetal heart rate with fetal acidosis pH < 7.20), or for a durable arrest of dilatation for at least 2 h, or no descent of the fetal head for at least 1 h despite adequate uterine contractions, was decided by the attending physician.
Medical records were reviewed for data on age, ethnicity, parity, gestational age, indication for labour induction, agent used for induction, augmentation of oxytocine, use of analgesia, time period between induction and delivery, Apgar score at 1 and 5 min, umbilical artery pH at birth, fetal weight at birth, and mode of delivery.
Data were entered into the statistical software package SPSS version 15. Separate analyses were made for nulliparous and multiparous women. Univariate analysis was used to test several variables (age, weight at birth, indications for induction of labour, Bishop score, cervical length) predicting the successful outcome. Receiver operating characteristic (ROC) curves were used to assess the efficacy of the Bishop score and cervical length in predicting the outcome. Sensitivity, specificity, likelihood ratios, and positive and negative predictive values were calculated.
Results
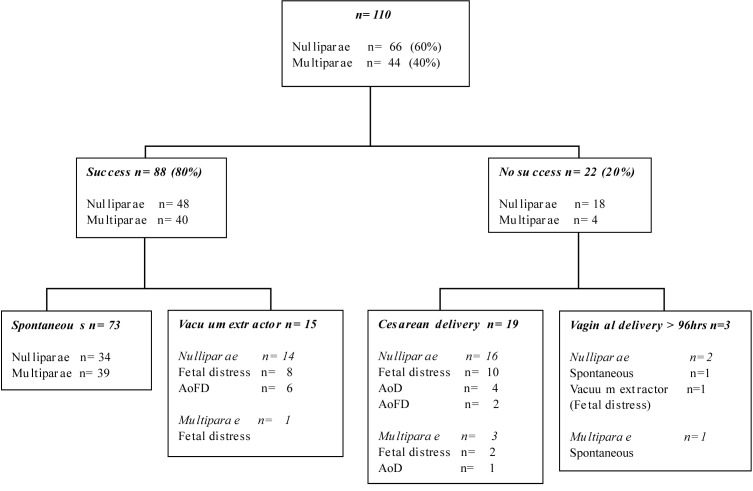
The study population included 110 at term women of whom 66 were nulliparous and 44 multiparous. Vaginal delivery within 96 h was achieved in 48 (73%) nulliparous and in 40 (91%) multiparous women; i.e. in 80% of the total group. The overall rate of caesarean delivery was 17% (Fig. 1 ).
1. Flowchart of the success rate in the present study.
There was a significant difference in age, cervical length, Bishop score and successful induction between nulliparous and multiparous women (Table II).
Table II. Characteristics and indications of the study population (n = 110) at start of induction of labour.
| Nulliparous women n = 66 (60%) | Multiparous women n = 44 (40%) | |||
|---|---|---|---|---|
| Age in years: mean (range)* | 28.61 (18-43) | 32.93 (26-41) | ||
| Ethnicity n (%) | ||||
| Dutch | 28 (42.42) | 21 (47.73) | ||
| Non-Dutch | 38 (57.58) | 23 (52.27) | ||
| Mediterranean | 23 (34.85) | 16 (36.36) | ||
| Negroid | 11 (16.67 | 4 (9.09) | ||
| Asiatic | 1 (1.52) | 0 (0.00) | ||
| Hindustani | 1 (1.52) | 3 (6.82) | ||
| East-European | 2 (3.03) | 0 | ||
| Indication for induction n (%) | ||||
| PROM > 48 hours | 14 (21.21) | 7 (15.91) | ||
| HELLP syndrome or pre-eclampsia | 9 (13.64) | 6 (13.64) | ||
| Diabetes maternal or gravity related | 4 (6.06) | 17 (38.64) | ||
| Prolonged pregnancy | 28 (42.42) | 7 (15.91) | ||
| Restricted intrauterine growth Amniotic fluid problems** | 5 (7.58) | 0 | ||
| Elective induction | 4 (6.06) | 3 (6.82) | ||
| Gestational cholestasis | 1 (1.52) | 3 (6.82) | ||
| 1 (1.52) | 1 (2.27) | |||
| Gestational age at induction in days: mean (range) * | 282.92 (259-294) | 274.61 (259- 294) | ||
| Length of the cervix at induction in mm: mean (range) * | 29.31 (5.0-56.0) | 37.04 (12.0-56.0) | ||
| Bishop score at induction: mean (range) * | 2.38 (0-6) | 0.70 (0-2) | ||
* p-value < 0.05 one-way ANOVA
** oligohydramnion, polyhydramnion, stained amniotic fluid
PROM (Prelabour rupture of membranes)
HELLP (Haemolysis elevated liver enzymes and low platelets)
Significantly more nulliparous women needed more oxytocin augmentation and analgesia. The success rate was significantly higher in multiparous women. There was no significant difference in neonatal outcomes between the subgroups (Table III).
Table III. Characteristics and outcome after induction of labour (n = 110).
| Nulliparous women n = 66 (60%) | Multiparous women n = 44 (40%) | |
|---|---|---|
| Dinoprostone gel mg (range) | 2.94 (1-7) | 3.22 (2-6) |
| Misoprostol tablets of 25 µg (range) | 0.17 (0-4) | 0.24 (0-6) |
| Oxytocin augmentation n (%)* | 37 (56.06) | 14 (31.8) |
| Analgesic n (%)* | 51 (77.27) | 20 (45.45) |
| None | 15 (22.73) | 24 (54.55) |
| Pethidine | 28 (42.42) | 17 (38.64) |
| Epidural anaesthesia | 10 (15.15) | 1 ( 2.27) |
| Combination | 13 (19.70) | 2 ( 4.55) |
| Interval between induction and delivery in hours: mean (range) | 28.95 (7.0-92.0) | 23.66 (4.5- 95.5) |
| Apgar score at 1 min: mean (range) | 8.21 (1-9) | 8.55 (1-10) |
| Apgar score at 5 min: mean (range) | 9.42 (5-10) | 9.73 (7-10) |
| Umbilical artery pH: mean (range) | 7.203 (7.01-7.34) | 7.204 (7.01-7.37) |
| Fetal weight in g: mean (range) | 3389 (1830-4585) | 3415 (2310-4440) |
| Vaginal delivery n (%)* | 50 (75.76) | 41 (93.18) |
| < 96 h (success) * | 48 (72.73) | 40 (90.91) |
| Spontaneous | 34 (51.52) | 39 (88.64) |
| Vacuum | 14 (21.21) | 1 (2.27) |
| Fetal distress | 8 (12.12) | 1 (2.27) |
| Arrest of fetal descent | 6 (9.09) | 0 |
| > 96 h | 2 (3.03) | 1 (2.27) |
| Spontaneous | 1 (1.52) | 1 (2.27) |
| Vacuum | 1 (1.52) | 0 |
| Fetal distress | 1 (1.52) | 0 |
| Arrest of fetal descent | 0 | 0 |
| Caesarean section n (%) | 16 (24.24) | 3 (6.82) |
| Fetal distress | 10 (15.15) | 2 (4.55) |
| Arrest of dilatation | 4 (6.06) | 1 (2.27) |
| Arrest of fetal descent | 2 (3.03) | 0 |
* p-value < 0.05 one-way ANOVA
Univariate analyses were performed for nulliparous and multiparous women to determine the significance of the following items possibly involved in predicting successful induction of labour: age, weight at birth, indications for induction of labour, Bishop score and cervical length. Univariate analysis of the possible predictors of success showed that only the Bishop score in nulliparous women was significant for predicting the outcome of success. ROC curves were computed for the Bishop score and cervical length in nulliparous and multiparous women. Only the Bishop score in nulliparous women showed a significant relationship between this variable and success of induction (area under the curve 0.679; SE 0.730; p < 0.05; 95% CI: 0.536-0.823) (Table IV). The best cut-off value for the Bishop was 3, with a sensitivity of 56.3 % and a specificity of 72.2% (Table V).
Table IV. Areas under the ROC curve and 95% CI for the Bishop score and cervical length in nulliparous and multiparous women.
| Area | SE | Significance | 95% confidence interval | ||
|---|---|---|---|---|---|
| Lower Boundary | Upper Boundary | ||||
| Bishop score nulliparae | 0.679 | 0.730 | 0.026* | 0.536 | 0.823 |
| Bishop score multiparae | 0.712 | 0.100 | 0.165 | 0.516 | 0.909 |
| Cervical length nulliparae | 0.430 | 0.081 | 0.384 | 0.272 | 0.588 |
| Cervical length multiparae | 0.719 | 0.080 | 0.153 | 0.562 | 0.876 |
* p-value > 0.05, SE = standard error
Table V. Data on diagnostic value of varying the cut-off point of the Bishop score in nulliparous women to predict the success of induction of labour.
| Parameter | Sensitivity % | Specificity % | LR+ | LR- | PPV | NPV |
|---|---|---|---|---|---|---|
| Bishop score | ||||||
| 6 | 2.1 | 100 | ∞ | 0.98 | 1.00 | 0.28 |
| 5 | 16.7 | 44.0 | 2.98 | 0.88 | 0.89 | 0.17 |
| 4 | 37.5 | 83.3 | 2.25 | 0.75 | 0.86 | 0.33 |
| 3 | 56.3 | 72.2 | 2.03 | 0.61 | 0.84 | 0.38 |
| 2 | 75.0 | 55.6 | 1.69 | 0.45 | 0.82 | 0.46 |
| 1 | 81.3 | 38.9 | 1.33 | 0.48 | 0.78 | 0.44 |
LR+ = positive likelihood ratio; L- = negative likelihood ratio; PPV = positive predictive value; NPP = negative predictive value
Discussion
The results show that only the Bishop score in nulliparous women was a predictor of success of induction. The overall chance of vaginal delivery within 96 h in nulliparous women is 72.7 % (pre-test probability). A Bishop score of 3 corresponded with a positive likelihood ratio of 2.03, resulting in a post-test probability of 84%. Cervical length was not a predictor of success in either nulliparous or multiparous women.
Results of studies comparing cervical length with cervical palpation were not conclusive (Pandis et al., 2001; Tan et al., 2007; Strobel et al., 2006; Rozenberg et al., 2005; Rane et al., 2003).
In a study by Laencina et al. (2007), cervical length and Bishop score proved to be predictors of successful labour; however, their outcome of success was defined as vaginal delivery within 12 h and 60 h respectively. In addition, women in their study with an unfavourable Bishop score (< 6) received 1 or 2 doses of prostaglandin gel. If labour was not triggered within 24 h and the Bishop score continued to be < 6 , the Bishop score and ultrasonographic scores were recorded and a second dose of prostaglandine gel was given. In that case cervical characteristics would probably have been changed by the gel and may have lost their predictive value. If labour was not triggered after 24 h, the Bishop score and ultrasonographic scores were recorded and oxytocin induction was started. Moreover, Laencina et al. (2007) showed that some women received oxytocin even when the Bishop score was less than six.
In contrast, in the present study ultrasonographic cervical measurement was performed just before intravaginal prostaglandin was applied. These methodological differences may explain the different results found compared with the present study (Laencina et al., 2007).
Rane et al. found that cervical length measured by ultrasound was an independent predictor of vaginal delivery within 24 h. However, the only indication for induction was prolonged pregnancy (at 41+3/7 and 42+1/7 weeks of gestation) in nulliparous women (Roman et al., 2004).
In our study population, the multiple indications for induction of labour might explain the differences between these two studies.
Gonen et al. (1998) also found that the transvaginal ultrasonographic evaluation of the cervix before induction of labour does not improve the prediction of cervical inducibility obtained by the Bishop score. Their study, as in ours, included multiple indications for induction of labour.
In addition, compared with the study of Laencina et al. (2007), we chose a longer interval (96h) between start of induction and vaginal delivery in order to avoid caesarean delivery as much as possible. Our caesarean delivery rate was 17.3% compared with 35.6% in their study.
Although cervical length measured by ultrasonography appears to be a more objective and precise measure, other cervical variables might be involved in predicting ripeness of the cervix; if this is so, then the Bishop score is certainly more valuable than the cervical length measured by ultrasound.
Rane et al. (2003) suggested that a combination of cervical length, posterior cervical angle and occipital position may be of more value in the prediction of induction of labour. In their study, the sonographic parameters were superior to the Bishop score in predicting the outcome of induction; however, the odds ratios were moderate.
A limitation of our study is the small numbers involved in the indications for induction of labour. A future study with larger numbers of women is required in order to make subgroup analyses for different indications. It is encouraging, however, that in their study on 240 women, Pandis et al. (2001) found the same optimal cut-off point for the Bishop score (i.e. 3) as we found in our study.
In conclusion, the present study indicates that the Bishop score is a predictor of successful vaginal delivery in nulliparous women, and that ultrasound measurement of cervical length does not contribute to the prediction of successful vaginal delivery. Over a period of 96 h (with cardiotocography monitoring), it appears to be a safe procedure to start induction of labour with prostaglandins and, if necessary, followed by administration of oxytocin. In our study population this resulted in a success rate of 80% vaginal delivery and a low caesarean delivery rate of 17%.
Vaginal examination is necessary to evaluate the progress of induction of labour, and in our experience the art of manual assessment still exists in clinical practice.
Acknowledgments
We are grateful to the women who participated in the study, the hospital staff and nurses of the Maasstad hospital who supported the study.
References
- Bishop EH. Pelvic scoring for elective induction. Obstet Gynecol. 1964;24:266–268. [PubMed] [Google Scholar]
- Gonen R, Degani S, Ron A. Prediction of successful induction of labor: comparison of transvaginal ultrasonography and the Bishop score. European Journal of Ultrasound. 1998;7:183–187. doi: 10.1016/s0929-8266(98)00042-1. [DOI] [PubMed] [Google Scholar]
- Jackson GM, Ludmir J, Bader TJ. The accuracy of digital examination and ultrasound in the evaluation of cervical length. Obstet Gynecol. 1992;79:214–218. doi: 10.3109/01443619209013646. [DOI] [PubMed] [Google Scholar]
- Kwee A, Smink M, Van Der Laar R, et al. Outcome of subsequent delivery after a previous early preterm casarean section. J Matern Fetal Neonatal Med. 2007;20:33–37. doi: 10.1080/14767050601036527. [DOI] [PubMed] [Google Scholar]
- Laencina AMG, Sanchez FG, Gimenez JH, et al. Comparison of ultrasonographic cervical length and the Bishop score in predicting successful labor induction. Acta Obst Gynecol Scand. 2007;86:799–804. doi: 10.1080/00016340701409858. [DOI] [PubMed] [Google Scholar]
- Pandis GK, Papageorghiou AT, Ramanathan VG, et al. Preinduction sonographic measurement of cervical length in the prediction of successful induction of labor. Ultrasound Obstet Gynecol. 2001;18:623–8. doi: 10.1046/j.0960-7692.2001.00580.x. [DOI] [PubMed] [Google Scholar]
- Rane SM, Pandis GK, Guirgis RR, et al. Pre-induction sonographic measurement of cervical length in prolonged pregnancy: the effect of parity in the prediction of induction-to-delivery interval. Ultrasound Obstet Gynecol. 2003;22:40–44. doi: 10.1002/uog.165. [DOI] [PubMed] [Google Scholar]
- Rane SM, Guirgis RR, Higgins B, et al. The value of ultrasound in the prediction of successful induction of labor. Ultrasound Obstet Gynecol. 2004;24:538–549. doi: 10.1002/uog.1100. [DOI] [PubMed] [Google Scholar]
- Roman H, Verspyck E, Vercoustre L, et al. Does ultrasound examination when the cervix is unfavorable improve the prediction of failed labor induction? Ultrasound Obstet Gynecol. 2004;23:357–362. doi: 10.1002/uog.1008. [DOI] [PubMed] [Google Scholar]
- Rozenberg P. Transvaginal Ultrasound of the Cervix: Hope in the Fight against Premature Delivery. J Radiol. 1999;80:421–429. [PubMed] [Google Scholar]
- Rozenberg P, Chevret S, Chastang C, et al. Comparison of digital and ultrasonographic examination of the cervix in predicting time interval from induction to delivery in women with a low Bishop score. . BJOG. 2005;112:192–196. doi: 10.1111/j.1471-0528.2004.00549.x. [DOI] [PubMed] [Google Scholar]
- Strobel E, Sladkevicius P, Rovas L, et al. Bishop score and ultrasound assessment of the cervix for prediction of time to onset of labor and time to delivery in prolonged pregnancy. Ultrasound Obstet Gynecol. 2006;28:298–305. doi: 10.1002/uog.2746. [DOI] [PubMed] [Google Scholar]
- Tan PC, Vallikkannu N, Suguna S, et al. Transvaginal sonographic measurement of cervical length vs. Bishop score in labor induction at term: tolerability and prediction of Cesarean delivery. Ultrasound Obstet Gynecol. 2007;29:568–573. doi: 10.1002/uog.4018. [DOI] [PubMed] [Google Scholar]
- Vrouenraets FPJM, Roumen FJME, Dehing CJG, et al. Bishop Score and Risk of Cesarean Delivery After Induction of Labor in Nulliparous Women. Obstet Gynecol. 2005;105:690–697. doi: 10.1097/01.AOG.0000152338.76759.38. [DOI] [PubMed] [Google Scholar]
- Ware V, Raynor BD. Transvaginal ultrasonographic cervical measurement as a predictor of successful labor induction. Am J Obstet Gynecol. 2000;182:1030–1032. doi: 10.1067/mob.2000.105399. [DOI] [PubMed] [Google Scholar]
- Yeast JD, Jones A, Poskin M. Induction of labor and the relationship to cesarean delivery: A review of 7001 consecutive inductions. Am J Obstet Gynecol. 1999;180:628–633. doi: 10.1016/s0002-9378(99)70265-6. [DOI] [PubMed] [Google Scholar]