Abstract
Background:
Previous studies supported a link between the ABO blood type and survival for several types of malignancies. Nonetheless, the relationship between ABO blood type and survival in colon cancer patients has not been rigorously evaluated. The goal of this retrospective analysis was to discern the correlations between ABO blood group and colon cancer survival.
Methods:
A total of 1555 colon cancer patients that underwent curative-intent surgery between October 1995 and June 2002 were eligible for this study. The primary outcomes measured were the association between ABO blood group and patient survival.
Results:
Compared with patients with non-AB blood types (blood types A, B, and O), patients with blood type AB were more likely to have better survival. The mean overall survival (OS) of the blood type AB patients was 113.9 months, whereas the mean OS of the non-AB blood type patients was significantly lower, 106.1 months (P<0.001, log-rank test). Compared with patients with blood type AB, the hazard ratios for patients with A, B, and O were 4.37 (95% confidence interval (95% CI), 2.65–7.20), 2.99 (95% CI, 1.81–4.96), and 2.78 (95% CI, 1.69–4.56), respectively.
Conclusions:
Blood type AB is a favourable prognostic factor for patients with colon cancer.
Keywords: ABO blood type, colon cancer, prognosis, survival
Colorectal cancer is the third-most commonly diagnosed cancer in males and the second-most common in females (Jemal et al, 2011). Each year, more than 1.2 million new cases of colorectal cancer are diagnosed worldwide (Jemal et al, 2011). During the past three decades, substantial developments and advances have been made in the screening, diagnosis, staging, and treatment of this neoplastic condition. However, worldwide, the disease-specific mortality rate of colorectal cancer is nearly 33% (Jemal et al, 2011). A better understanding of the predisposing environmental and genetic factors of colorectal cancer could improve the prognoses of patients and provide therapies that are more appropriate.
The ABO gene on chromosome 9q34 encodes glycosyltransferases that catalyse the transfer of nucleotide donor sugars to the H antigen and forms the ABO blood group antigens (Yazer, 2005). ABO blood group antigens are expressed on the surface of red blood cells and several other tissue types, including cells from the gastrointestinal tract. The relationships between ABO blood group and cancer have been a subject of interest since the mid 1900s. Laboratory investigations have provided several plausible mechanisms to explain the observed associations between ABO blood groups and cancer. These proposed mechanisms involve inflammation, immune surveillance for malignant cells, intercellular adhesion, and membrane signalling (Itzkowitz et al, 1987; Matsumoto et al, 1993; Wolpin et al, 2009). Previous investigations have also suggested a link between inherited human blood group and malignancy, including gastric cancer (Hoskins et al, 1965), skin cancer (Xie et al, 2010), and breast cancer (Holdsworth et al, 1985).
However, to date, studies of the impact of ABO blood group on the survival of patients with colon cancer are of limited number and scope. Therefore, the goal of this retrospective analysis was to discern the correlations between ABO blood group and colon cancer survival in 1555 patients with colon cancer who underwent complete colon resection as their primary treatment.
Materials and Methods
Patients
This was a longitudinal investigation, which was conducted between October 1995 and June 2002 at Sun Yat-Sen University Cancer Center. The eligibility criteria for the 1555 participants included histologically confirmed colon cancer without distant metastasis and with no previous treatment other than complete surgical resection (R0). Exclusion criteria included previous malignant disease, occurrence of a second primary tumour, non-curative resection (R1/2), or death from postoperative complications. Tumour differentiation grades were defined according to the World Health Organization criteria. Cancer staging was based on the American Joint Committee on Cancer Staging system (AJCC, 2002; Greene, American Joint Committee on Cancer., American Cancer Society, 2002). This study was approved by the medical ethics committee of Sun Yat-Sen University Cancer Center. All patients have given their informed consent before their inclusion in this study.
All the patients underwent curative-intent surgery. Adjuvant chemotherapy, unless refused, was administered to patients with stage II (high risk: Grade III, lymphatic/vascular invasion, bowel obstruction, <12 lymph nodes examined, perineural invasion, and localised perforation) and stage III disease if they could tolerate additional treatments after curative-intent surgery. In total, 917 patients with stage II/III disease received 4–6 cycles of systemic chemotherapy. 5-fluorouracil/leucovorin regimens were performed on 594 colon cancer patients (stage II, 324 cases; stage III, 270 cases). A 5-fluorouracil/leucovorin/oxaliplatin regimen was also administered to 323 patients (stage II, 186 cases; stage III, 137 cases).
Follow-up
After completion of primary treatment, patients were followed up every 3 months in the first 2 years and every 6 months, thereafter. In May 2010, survival status was verified again using the best available methods, including checking clinical attendance records and direct telecommunication with the patients or their families (performed by The Medical Information Unit in our Cancer Center).
Assessment of ABO blood type and covariates
For the complete medical history, participants were asked their blood type (A, B, AB, O, or unknown) and their Rh factor (positive, negative, or unknown). We serologically examined the ABO blood group type and Rh factor of all recruited patients before their surgery. These determinations were carried out in the Immunohematologic Laboratory of Sun Yat-Sen University Cancer Canter.
For the complete medical history, the patients were asked the information about their tobacco use. Smoking status was classified as follows: (i) never-smoker; (ii) former-smoker who had quit>1 year before diagnosis; (iii) current-smoker who was smoking at the time of diagnosis or had quit<1 year prior.
Statistical analysis
Overall survival (OS) was defined as the time from the date of surgery to the date of death or final clinical follow-up. Actuarial survival rates were plotted against time using the Kaplan–Meier method, and a log-rank test was used to compare the differences between the curves. P-values were derived from two-sided tests and P-values <0.05 were considered statistically significant. The statistical analyses were performed using the SPSS 13.0 software package (SPSS, Chicago, IL, USA).
Results
Patient characteristics
Between October 1995 and June 2002, 1555 participants at the Sun Yat-Sen University Cancer Center were eligible for analysis. The median age of the patients was 59 years (range, 19–86 years). The distribution of the ABO blood type was 452 A blood type patients (29.1%), 382 B blood type patients (24.6%), 598 O blood type patients (38.5%), and 123 AB blood type patients (7.8%). Table 1 summarises the characteristics of the study population. χ2 test showed that AB blood type positively correlated with body mass index (P=0.027, more common in higher body mass index than low body mass index), and tumour location (P<0.001, more common in left hemicolon than right hemicolon). The frequency distributions of ABO blood groups were similar to those of the population of China (Supplementary Table).
Table 1. Patients characteristics according to ABO blood type.
|
ABO blood type (%) |
|||||||
|---|---|---|---|---|---|---|---|
|
Non-AB |
|||||||
| Characteristics | Number of Patients (%) | AB | A/B/O | A | B | O | Pa |
| Total |
1555 |
123 (7.8%) |
1432 (92.2%) |
452 (29.1%) |
382 (24.6%) |
598 (38.5%) |
|
| Rh factor |
|
|
|
|
|
|
0.481 |
| Positive | 1547 (99.5%) | 122 (99.2%) | 1425 (99.5%) | 450 (99.6%) | 380 (99.5%) | 595 (99.5%) | |
| Negative |
8 (0.005%) |
1 (0.8%) |
7 (0.5%) |
2 (0.4%) |
2 (0.5%) |
3 (0.5%) |
|
| Age, yearsb |
|
|
|
|
|
|
0.195 |
| Median | 59 | 63 | 59 | 58 | 60 | 58 | |
| <45 | 299 (19.2%) | 18 (14.6%) | 281 (19.6%) | 86 (19.0%) | 75 (19.6%) | 120 (20.1%) | |
| 45–59 | 493 (31.7%) | 35 (28.5%) | 458 (32.0%) | 147 (32.5%) | 113 (29.6%) | 198 (33.1%) | |
| ⩾60 |
763 (49.1%) |
70 (56.9%) |
693 (48.4%) |
219 (48.5%) |
194 (50.8%) |
280 (46.8%) |
|
| Gender |
|
|
|
|
|
|
0.135 |
| Female | 690 (44.4%) | 63 (51.2%) | 627 (43.8%) | 218 (48.2%) | 173 (45.3%) | 236 (39.5%) | |
| Male |
865 (55.6%) |
60 (48.8%) |
805 (56.2%) |
234 (51.8%) |
209 (54.7%) |
362 (60.5%) |
|
| BMI, kg m−2
c |
|
|
|
|
|
|
0.027 |
| Median | 21.5 | 21.6 | 21.5 | 20.9 | 22.0 | 21.5 | |
| <18.5 | 238 (15.3%) | 10 (8.1%) | 228 (15.9%) | 88 (19.5%) | 45 (11.8%) | 95 (15.9%) | |
| 18.5–23.9 | 944 (60.7%) | 77 (62.6%) | 867 (60.5%) | 281 (62.2%) | 222 (58.1%) | 364 (60.9%) | |
| ⩾24 |
373 (24.0%) |
36 (29.3%) |
337 (23.6%) |
83 (18.3%) |
115 (30.1%) |
139 (23.2%) |
|
| Smoking statue |
|
|
|
|
|
|
0.08 |
| Never | 839 (54.0%) | 57 (46.3%) | 782 (54.6%) | 240 (53.1%) | 209 (54.7%) | 333 (55.6%) | |
| Past | 327 (21.0%) | 36 (29.3%) | 291 (20.3%) | 105 (23.2%) | 87 (22.8%) | 99 (16.6%) | |
| Current |
389 (25.0%) |
30 (24.4%) |
359 (25.1%) |
107 (23.7%) |
86 (22.5%) |
166 (27.8%) |
|
| Location |
|
|
|
|
|
|
<0.001 |
| Left | 941 (60.5%) | 96 (78.0%) | 845 (59.0%) | 258 (57.1%) | 206 (53.9%) | 381 (63.7%) | |
| Right |
614 (39.5%) |
27 (22.0%) |
587 (41.0%) |
194 (42.9%) |
176 (46.1%) |
217 (36.3%) |
|
|
Pathology | |||||||
| Adenocarcinoma |
1555 (100%) |
123 (7.8%) |
1432 (92.2%) |
452 (29.1%) |
382 (24.6%) |
598 (38.5%) |
|
| pT status |
|
|
|
|
|
|
0.055 |
| pT1 | 54 (3.5%) | 3 (2.4%) | 51 (3.6%) | 9 (2.0%) | 18 (4.7%) | 24 (4.0%) | |
| pT2 | 207 (13.3%) | 15 (12.2%) | 192 (13.4%) | 51 (11.3%) | 45 (11.8%) | 96 (16.1%) | |
| pT3 | 619 (39.8%) | 36 (29.3%) | 583 (40.7%) | 209 (46.2%) | 162 (42.4%) | 212 (35.5%) | |
| pT4 |
675 (43.4%) |
69 (56.1%) |
606 (42.3%) |
183 (40.5%) |
157 (41.1%) |
266 (44.4%) |
|
| pN status |
|
|
|
|
|
|
0.068 |
| pN0 | 1011 (65.0%) | 69 (56.1%) | 942 (65.8%) | 294 (65.1%) | 244 (63.9%) | 404 (67.6%) | |
| pN1 | 391 (25.1%) | 35 (28.5%) | 356 (24.8%) | 96 (21.2%) | 117 (30.6%) | 143 (23.9%) | |
| pN2 |
153 (9.9%) |
19 (15.4%) |
134 (9.4%) |
62 (13.7%) |
21 (5.5%) |
51 (8.5%) |
|
| Grade |
|
|
|
|
|
|
0.172 |
| Grade I | 93 (6.0%) | 12 (9.8%) | 81 (5.7%) | 30 (6.6%) | 21 (5.5%) | 30 (5.0%) | |
| Grade II | 1256 (80.8%) | 95 (77.2%) | 1161 (81.1%) | 341 (75.5%) | 322 (84.3%) | 498 (83.3%) | |
| Grade III |
206 (13.2%) |
16 (13.0%) |
190 (13.2%) |
81 (17.9%) |
39 (10.2%) |
70 (11.7%) |
|
| pTNM stage |
|
|
|
|
|
|
0.076 |
| Stage I | 228 (14.7%) | 12 (9.8%) | 216 (15.1%) | 54 (11.9%) | 54 (14.1%) | 108 (18.1%) | |
| Stage II | 783 (50.4%) | 57 (46.3%) | 726 (50.7%) | 240 (53.1%) | 190 (49.8%) | 296 (49.5%) | |
| Stage III |
544 (35.0%) |
54 (43.9%) |
490 (34.2%) |
158 (35.0%) |
138 (36.1%) |
194 (32.4%) |
|
| Chemotherapy |
|
|
|
|
|
|
0.572 |
| Yes | 917 (59.0%) | 69 (56.1%) | 848 (59.2%) | 249 (55.1%) | 237 (62.0%) | 362 (60.5%) | |
| No |
638 (41.0%) |
54 (43.9%) |
584 (40.8%) |
203 (44.9%) |
145 (38.0%) |
236 (39.5%) |
|
| Operationd |
|
|
|
|
|
|
0.462 |
| Elective | 1454 (93.5%) | 116 (95.1%) | 1338 (93.4%) | 416 (92.0%) | 358 (93.7%) | 564 (94.3%) | |
| Emergency |
101 (6.5%) |
7 (4.9%) |
94 (6.6%) |
36 (8.0%) |
24 (6.3%) |
34 (5.7%) |
|
| Postoperative complicatione |
|
|
|
|
|
|
0.626 |
| No | 1463 (94.1%) | 117 (95.1%) | 1347 (94.1%) | 422 (93.4%) | 355 (92.95) | 570 (95.3%) | |
| Yes | 92 (5.9%) | 6 (4.9%) | 85 (5.9%) | 30 (6.6%) | 27 (7.1%) | 28 (4.7%) | |
Abbreviations: BMI=body mass index; pN status=pathological node status; pT statue=pathological tumour status; pTNM status=pathological tumour-node-metastasis stage.
χ2 test (AB blood type vs non-AB blood type).
World Health Organization criteria.
Chinese definition.
Emergency includes lose blood, obstruction, and perforation.
Postoperative complication includes infection, anastomotic leak, and various reasons result in re-operation and/or prolonged hospitalisation.
Associations between ABO blood type and patient survival
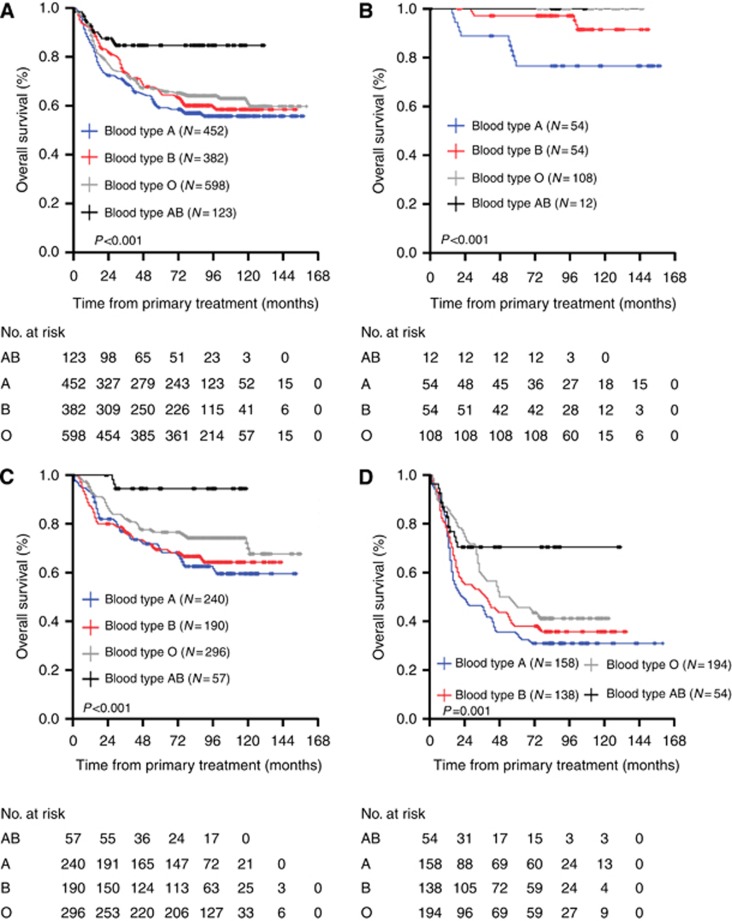
The median follow-up period of the 1555 colon cancer patients was 78 months with 975 alive and 580 cancer-related deaths at the last clinical follow-up. The mean OS for all patients was 108.2 months. In the Kaplan–Meier analysis, ABO blood type was closely associated with OS. For the whole cohort, the OS was 7.8 months longer in patients with AB blood type (mean, 113.9 months) than those with non-AB blood type (mean, 106.1 months) (P<0.001, Figure 1A). However, they were similar in those patients with A/B/O blood type (P=0.081). The mean OS times were as follows: blood type AB, 113.9 months (95% CI, 106.4–121.4 months); blood type O, 108.9 months (95% CI, 103.5–114.4 months); blood type B, 103.4 months (95% CI, 97.6–109.6 months); blood type A, 99.8 months (95% CI, 93.6–106.1 months). Because ABO blood type was found to be an important prognostic factor for OS, we examined the relationship between ABO blood type and survival based on patients' pathological stage. This analysis showed that ABO blood group could distinguish OS when stratified by pathological stage (stage I, P<0.001; stage II, P<0.001; stage III, P=0.001) (Figure 1B–D). Furthermore, we examined the relationship between ABO blood group and survival based upon tumour location. We observed a significant different in OS in patients with left hemicolon (mean OS was longer in patients with AB blood group than those with non-AB blood group, P<0.001), whereas OS was similar between AB and non-AB blood group subsets in patients with right hemicolon (P=0.123).
Figure 1.
Overall survival, by ABO blood type, among patients in our study. (A) Overall survival for the whole cohort of patients with colon cancer; (B) OS for the stage I patients with colon cancer; (C) OS for the stage II patients with colon cancer; (D) OS for the stage III patients with colon cancer.
To determine whether ABO blood type could serve as an independent prognostic parameter, we examined OS using the Cox proportional hazards model. All the parameters found to be significant in the univariate analysis were further analysed by multivariate analysis, and the results revealed that smoking statue (P<0.001), tumour grade (P=0.002), pathologic tumour-node-metastasis stage (P<0.001), adjuvant chemotherapy (P<0.001), and ABO blood type (P<0.001) were independent, significant predictors for OS. The details of this analysis are presented in Table 2.
Table 2. Univariate and multivariate Cox regression analysis for overall survival in patients with colon cancer.
|
Univariate analysis |
Multivariate analysis |
|||||
|---|---|---|---|---|---|---|
| Characteristics | HR | 95% CI | Pa | HR | 95% CI | Pa |
| Age |
1.00 |
0.99–1.01 |
0.932 |
— |
— |
— |
| Gender |
|
|
0.815 |
|
|
— |
| Female | 1.00 | Reference | — | — | ||
| Male |
1.02 |
0.87–1.20 |
|
— |
— |
|
| BMI, kg m−2
b |
|
|
0.073 |
|
|
— |
| <18.5 | 1.32 | 1.06–1.64 | — | — | ||
| 18.5–23.9 | 1.00 | Reference | — | — | ||
| ⩾24 |
0.89 |
0.73–1.11 |
|
— |
— |
|
| Smoking statue |
|
|
<0.001 |
|
|
<0.001 |
| Never | 1.00 | Reference | 1.00 | Reference | ||
| Past | 3.34 | 2.61–4.26 | 1.37 | 0.97–1.93 | ||
| Current |
13.31 |
10.75–16.48 |
|
8.07 |
6.20–10.51 |
|
| Location |
|
|
0.087 |
|
|
— |
| Left | 1.00 | Reference | — | — | ||
| Right |
1.15 |
0.98–1.36 |
|
— |
— |
|
| Grade |
|
|
<0.001 |
|
|
0.002 |
| Grade I | 1.00 | Reference | 1.00 | Reference | ||
| Grade II | 1.19 | 0.82–1.73 | 1.96 | 1.34–2.86 | ||
| Grade III |
2.20 |
1.46–3.29 |
|
2.18 |
1.45–3.28 |
|
| pTNM stage |
|
|
<0.001 |
|
|
<0.001 |
| Stage I | 1.00 | Reference | 1.00 | Reference | ||
| Stage II | 4.42 | 2.74–7.14 | 2.43 | 1.48–4.00 | ||
| Stage III |
12.14 |
7.55–19.52 |
|
4.82 |
2.79–8.34 |
|
| Operation |
|
|
0.565 |
|
|
— |
| Elective | 1.00 | Reference | — | — | ||
| Emergencyc |
1.11 |
0.79–1.53 |
|
— |
— |
|
| Postoperative complication |
|
|
0.71 |
|
|
— |
| No | 1.00 | Reference | — | — | ||
| Yesd |
1.07 |
0.76–1.50 |
|
|
— |
— |
| Adjuvant chemotherapy |
|
|
<0.001 |
|
|
<0.001 |
| Yes | 1.00 | Reference | 1.00 | Reference | ||
| No |
2.01 |
1.70–2.36 |
|
1.43 |
1.21–1.69 |
|
| ABO blood type |
|
|
<0.001 |
|
|
<0.001 |
| AB | 1.00 | Reference | 1.000 | Reference | ||
| Non-AB | 2.70 | 1.67–4.38 | 3.22 | 1.98–5.22 | ||
| O | 2.47 | 1.51–4.05 | 2.78 | 1.69–4.56 | ||
| B | 2.65 | 1.61–4.37 | 2.99 | 1.81–4.96 | ||
| A |
3.04 |
1.80–5.03 |
|
4.37 |
2.65–7.20 |
|
| Rh factor |
|
|
0.573 |
|
|
— |
| Positive | 1.00 | Reference | — | — | ||
| Negative | 1.33 | 0.49–3.55 | — | — | ||
Abbreviations: BMI=body mass index; 95% CI=95% confidence interval; HR=hazard ratio; pTNM stage=pathological tumour-node-metastasis stage.
Cox proportional hazards model.
Chinese definition.
Emergency includes lose blood, obstruction, and perforation.
Postoperative complication includes infection, anastomotic leak, and various reasons result in re-operation and/or prolonged hospitalisation.
Discussion
For several decades, a role for ABO blood type antigens in the development of cancer has been suspected, and earlier investigations have noted a relationship between ABO blood type and the risk of malignances (Hoskins et al, 1965; Xie et al, 2010). However, to date, associations between blood type and colon cancer survival have not been well developed. Based on its unique aetiology, patient characteristics, blood typing, uniform treatment modalities, and long follow-up time, the current study is the first to identify the prognostic significance of ABO blood type among patients with resected colon cancer.
Among the 1555 colon cancer cases examined in this retrospective study from Sun Yat-Sen University Cancer Center, we observed significantly better survival for participants with blood group AB compared with non-AB blood group participants (blood groups A, B, and O). The worst survival was observed for participants with blood type A, and intermediate survival was observed for those with blood types O and B. Using multivariate analysis, significant associations with colon cancer survival were found for smoking status, tumour grade, pathologic tumour-node-metastasis stage, adjuvant chemotherapy, and ABO blood group.
Although some earlier studies have reported associations between ABO blood group and cancer survival, the results have been inconsistent. Studies from England (Holdsworth et al, 1985) and Italy (Costantini et al, 1990) have reported poor survival among breast cancer participants with blood types AB or B or any non-O blood type. In contrast, Gates et al (2012) indicated that ABO blood group was not associated with breast cancer survival. However, a growing body of plausible mechanisms, including inflammation, immunosurveillance for malignant cells, intracellular adhesion, and membrane signalling have been proposed to explain the relationships between ABO blood group and tumour metastasis and prognosis (Nozoe et al, 2004).
The ABO blood group are defined by carbohydrate moieties displayed on the surface of red blood cells and attached to membrane proteins and lipids. Three variant alleles (A, B, and O) of a single gene on chromosomes 9q34, the ABO gene, determine a person's blood type by encoding three glycosyltransferases with different substrate specificities. In addition to their expression on the surface of red blood cells, the ABO blood antigens are highly expressed on the surface of many epithelial cells, including gastrointestinal, bronchopulmonary, urogenital, and skin cells (Hakomori, 1999; Le Pendu et al, 2001). Alterations of ABO antigen expression on the surface of malignant cells, compared with normal epithelium, have been seen for a variety of tumour types (Strauchen et al, 1980; Hakomori, 1999). Glycosyltransferase specificity has broad implications, beyond defining ABO blood type. Glycoconjugates are important mediators of intercellular adhesion and membrane signalling, two processes integral to malignant progression and spread (Hakomori, 1999). In addition, these surface molecules are recognised by the host immune response and may have a role in facilitating immunosurveillance for malignant cells (Hakomori, 2001).
Alterations in the host inflammatory state due to ABO blood group antigens may provide a further mechanism to explain the associations between blood type and colon cancer progression. Several studies have demonstrated a link between chronic inflammation and malignant initiation. A study of United Kingdom has revealed that two single-nucleotide polymorphisms at the ABO locus were associated with serum levels of tumour necrosis factor-alpha, an inflammatory cytokine known to modulate cell apoptosis and inhibit tumourigenesis (Locksley et al, 2001; Melzer et al, 2008). Furthermore, Pare et al (2008) published a study which indicated a statistically significant relationship between single-nucleotide polymorphisms at the ABO locus and plasma levels of intercellular adhesion molecule 1, a molecule which has classically been associated with the functioning the inflammatory response (Yang et al, 2005). Recently, Barbalic et al (2010) and Qi et al (2010) have replicated this finding for other serum markers of inflammation, such as E-selectin and P-selectin. These results reveal the possibility that chronic inflammation is significantly linked with tumour initiation and metastasis and suggest an additional potential mechanism by which ABO blood type may influence cancer survival.
Furthermore, the loss of expression of blood group antigens with malignant transformation and tumour progression is intriguing as a possible mechanism for the association of ABO blood type and colon cancer survival in our study (Tauchi et al, 1991). In addition, the loss of expression of blood group antigens A and B occurs during wound healing (Mackenzie et al, 1977). Within hours following wounding, epithelial cells adjacent to the wound site exhibit loss of blood group antigens. After the healing process is complete, the antigens are expressed again. It has been hypothesised that the association between the loss expression of blood group antigens and the risk of metastasis may partially explain our observed differences in colon cancer survival. Indeed, a growing body of evidence suggests that loss of expression of ABH blood type and/or Lea antigens is linked with more aggressive tumours in cancers of the breast (Holdsworth et al, 1985; Costantini et al, 1990) and uterine cervix (Davidsohn, 1972).
We acknowledge the limitations of our retrospective analysis. First, our study population was composed of yellow participants (Chinese population), which somewhat limits the generalisability of our results. Accordingly, the results of further investigations including more diverse populations (white/black/brown participants) from other institutes are needed to confirm our findings. In addition, not all patients had computed tomography scans or magnetic resonance imaging of the chest and/or brain at the time of diagnosis, and it is possible that some patients had asymptomatic disease at the time of primary treatment. However, this would have had a negative influence, if any, on survival.
In summary, our results suggested an association between ABO blood group and colon cancer survival. Compared with patients with non-AB blood types (blood types A, B, and O), patients with blood type AB were more likely to have a better survival. The impact of ABO blood type on malignant potential and prognosis in patients with colon cancer remains an interesting area of research, which warrants additional investigation.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on British Journal of Cancer website (http://www.nature.com/bjc)
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Material
References
- Barbalic M, Dupuis J, Dehghan A, Bis JC, Hoogeveen RC, Schnabel RB, Nambi V, Bretler M, Smith NL, Peters A, Lu C, Tracy RP, Aleksic N, Heeriga J, Keaney JF, Jr, Rice K, Lip GY, Vasan RS, Glazer NL, Larson MG, Uitterlinden AG, Yamamoto J, Durda P, Haritunians T, Psaty BM, Boerwinkle E, Hofman A, Koenig W, Jenny NS, Witteman JC, Ballantyne C, Benjamin EJ. Large-scale genomic studies reveal central role of ABO in sP-selectin and sICAM-1 levels. Hum Mol Genet. 2010;19 (9):1863–1872. doi: 10.1093/hmg/ddq061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costantini M, Fassio T, Canobbio L, Landucci M, Resasco M, Boccardo F. Role of blood groups as prognostic factors in primary breast cancer. Oncology. 1990;47 (4):308–312. doi: 10.1159/000226839. [DOI] [PubMed] [Google Scholar]
- Davidsohn I. Early immunologic diagnosis and prognosis of carcinoma. Philip Levine Award Address. Am J Clin Pathol. 1972;57 (6):715–730. doi: 10.1093/ajcp/57.6.715. [DOI] [PubMed] [Google Scholar]
- Gates MA, Xu M, Chen WY, Kraft P, Hankinson SE, Wolpin BM. ABO blood group and breast cancer incidence and survival. Int J Cancer. 2012;130 (9):2129–2137. doi: 10.1002/ijc.26220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene FL, American Joint Committee on Cancer, American Cancer Society 2002AJCC Cancer Staging Manual6th edn.Springer-Verlag: New York [Google Scholar]
- Hakomori S. Antigen structure and genetic basis of histo-blood groups A, B and O: their changes associated with human cancer. Biochim Biophys Acta. 1999;1473 (1):247–266. doi: 10.1016/s0304-4165(99)00183-x. [DOI] [PubMed] [Google Scholar]
- Hakomori S. Tumor-associated carbohydrate antigens defining tumor malignancy: basis for development of anti-cancer vaccines. Adv Exp Med Biol. 2001;491:369–402. doi: 10.1007/978-1-4615-1267-7_24. [DOI] [PubMed] [Google Scholar]
- Holdsworth PJ, Thorogood J, Benson EA, Clayden AD. Blood group as a prognostic indicator in breast cancer. Br Med J (Clin Res Ed) 1985;290 (6469):671–673. doi: 10.1136/bmj.290.6469.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoskins LC, Loux HA, Britten A, Zamcheck N. Distribution of ABO blood groups in patients with pernicious anemia, gastric carcinoma and gastric carcinoma associated with pernicious anemia. N Engl J Med. 1965;273 (12):633–637. doi: 10.1056/NEJM196509162731204. [DOI] [PubMed] [Google Scholar]
- Itzkowitz SH, Yuan M, Ferrell LD, Ratcliffe RM, Chung YS, Satake K, Umeyama K, Jones RT, Kim YS. Cancer-associated alterations of blood group antigen expression in the human pancreas. J Natl Cancer Inst. 1987;79 (3):425–434. [PubMed] [Google Scholar]
- Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61 (2):69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- Le Pendu J, Marionneau S, Cailleau-Thomas A, Rocher J, Le Moullac-Vaidye B, Clement M. ABH and Lewis histo-blood group antigens in cancer. APMIS. 2001;109 (1):9–31. doi: 10.1111/j.1600-0463.2001.tb00011.x. [DOI] [PubMed] [Google Scholar]
- Locksley RM, Killeen N, Lenardo MJ. The TNF and TNF receptor superfamilies: integrating mammalian biology. Cell. 2001;104 (4):487–501. doi: 10.1016/s0092-8674(01)00237-9. [DOI] [PubMed] [Google Scholar]
- Mackenzie IC, Dabelsteen E, Zimmermann K. The relationship between expression of epithelial B-like blood group antigen, cell movement and cell proliferation. Acta Pathol Microbiol Scand A. 1977;85A (1):49–56. doi: 10.1111/j.1699-0463.1977.tb03867.x. [DOI] [PubMed] [Google Scholar]
- Matsumoto H, Muramatsu H, Shimotakahara T, Yanagi M, Nishijima H, Mitani N, Baba K, Muramatsu T, Shimazu H. Correlation of expression of ABH blood group carbohydrate antigens with metastatic potential in human lung carcinomas. Cancer. 1993;72 (1):75–81. doi: 10.1002/1097-0142(19930701)72:1<75::aid-cncr2820720116>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Melzer D, Perry JR, Hernandez D, Corsi AM, Stevens K, Rafferty I, Lauretani F, Murray A, Gibbs JR, Paolisso G, Rafiq S, Simon-Sanchez J, Lango H, Scholz S, Weedon MN, Arepalli S, Rice N, Washecka N, Hurst A, Britton A, Henley W, van de Leemput J, Li R, Newman AB, Tranah G, Harris T, Panicker V, Dayan C, Bennett A, McCarthy MI, Ruokonen A, Jarvelin MR, Guralnik J, Bandinelli S, Frayling TM, Singleton A, Ferrucci L. A genome-wide association study identifies protein quantitative trait loci (pQTLs) PLoS Genet. 2008;4 (5):e1000072. doi: 10.1371/journal.pgen.1000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nozoe T, Ezaki T, Baba H, Kakeji Y, Maehara Y. Correlation of ABO blood group with clinicopathologic characteristics of patients with esophageal squamous cell carcinoma. Dis Esophagus. 2004;17 (2):146–149. doi: 10.1111/j.1442-2050.2004.00392.x. [DOI] [PubMed] [Google Scholar]
- Pare G, Chasman DI, Kellogg M, Zee RY, Rifai N, Badola S, Miletich JP, Ridker PM. Novel association of ABO histo-blood group antigen with soluble ICAM-1: results of a genome-wide association study of 6,578 women. PLoS Genet. 2008;4 (7):e1000118. doi: 10.1371/journal.pgen.1000118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi L, Cornelis MC, Kraft P, Jensen M, van Dam RM, Sun Q, Girman CJ, Laurie CC, Mirel DB, Hunter DJ, Rimm E, Hu FB. Genetic variants in ABO blood group region, plasma soluble E-selectin levels and risk of type 2 diabetes. Hum Mol Genet. 2010;19 (9):1856–1862. doi: 10.1093/hmg/ddq057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauchen JA, Bergman SM, Hanson TA. Expression of A and B tissue isoantigens in benign and malignant lesions of the breast. Cancer. 1980;45 (8):2149–2155. doi: 10.1002/1097-0142(19800415)45:8<2149::aid-cncr2820450823>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- Tauchi K, Kakudo K, Machimura T, Makuuchi H, Mitomi T. Immunohistochemical studies of blood group-related antigens in human superficial esophageal carcinomas. Cancer. 1991;67 (12):3042–3050. doi: 10.1002/1097-0142(19910615)67:12<3042::aid-cncr2820671219>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Wolpin BM, Chan AT, Hartge P, Chanock SJ, Kraft P, Hunter DJ, Giovannucci EL, Fuchs CS. ABO blood group and the risk of pancreatic cancer. J Natl Cancer Inst. 2009;101 (6):424–431. doi: 10.1093/jnci/djp020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J, Qureshi AA, Li Y, Han J. ABO blood group and incidence of skin cancer. PLoS One. 2010;5 (8):e11972. doi: 10.1371/journal.pone.0011972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L, Froio RM, Sciuto TE, Dvorak AM, Alon R, Luscinskas FW. ICAM-1 regulates neutrophil adhesion and transcellular migration of TNF-alpha-activated vascular endothelium under flow. Blood. 2005;106 (2):584–592. doi: 10.1182/blood-2004-12-4942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yazer MH. What a difference 2 nucleotides make: a short review of ABO genetics. Transfus Med Rev. 2005;19 (3):200–209. doi: 10.1016/j.tmrv.2005.02.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.