Abstract
Objective
The objective of this paper is to describe the methods of evaluating currently available triage models for their efficacy in appropriately triaging the surge of patients after an all-hazards disaster.
Design
We developed a method for evaluating currently available triage models using extracted data from medical records of the victims from the Graniteville chlorine disaster.
Setting
On January 6, 2005, a freight train carrying three tanker cars of liquid chlorine was inadvertently switched onto an industrial spur in central Graniteville, South Carolina. The train then crashed into a parked locomotive and derailed. This caused one of the chlorine tankers to rupture and immediately release ~60 tons of chlorine. Chlorine gas infiltrated the town with a population of 7,000.
Participants
This research focuses on the victims who received emergency care in South Carolina.
Results
With our data mapping and decision tree logic, we were successful in employing the available extracted clinical data to estimate triage categories for use in triage effectiveness research.
Conclusions
The methodology outlined in this paper can be used to assess the performance of triage models after a disaster. The steps are reliable and repeatable and can easily be extended or applied to other disaster datasets.
INTRODUCTION
Mass casualty triage describes the process to classify and prioritize victims according to predetermined severity algorithms to ensure the greatest survivability within a context of limited resources. However, there is a paucity of literature evaluating mass casualty triage models and no gold standard for measuring the effectiveness of information decision support data used in response to mass casualty incidents.1-4 Only one of the triage models currently used for mass casualty triage decision support has been tested under mass casualty conditions and validated by outcome data.5 Only three studies included assessments of incidents involving chemicals.6-8
Mass casualty events include natural, unintended and deliberate incidents that occur with little or no warning and have the potential to produce large numbers of casualties that can overwhelm existing healthcare facilities and resources4. Effective and timely management of mass casualties is dependent upon valid triage tools and models that provide decision support for emergency responders9-13. Because mass casualty incidents do not lend themselves to randomized, controlled, experimental trials, the science of disaster medical research is often anecdotal, observational, and more descriptive than analytical.14-32 The study of mass casualty incidents requires special procedures for data collection storage and analysis.33 The ability to collect accurate, timely and valid data at the time of an incident is difficult. Methods rely predominately on detailed observational field notes, collecting and analyzing data produced by responding agencies, and mass media sources such as photography and video.33 Methods employed after an incident include interviews and surveys which pose potential bias and recall errors.
OBJECTIVES
The main objective of this research is to use observed health outcome data from a large chlorine leak to analyze victim assessment using the four most frequently used triage models and to compare the modeled classification to observed patient outcomes. Specifically, the decision tree for four popular triage systems (Simple Triage and Rapid Treatment [START], 14,34,35 Emergency Severity Index [ESI],36-41 Sort, Assess, Life Saving Interventions Treatment and/or Transport [SALT],42-43
Chemical/Biological/Radiological/Nuclear Mass Casualty Triage System [CBRN])6 are modeled using data extracted from victim records to produce a predicted outcome for each triage model. The triage model outcome is then compared to the observed health effect severity level for each victim. The objective of this paper is to describe a successful approach to collect, extract, and analyze clinical data for disaster-related triage effectiveness research.
The purpose of this paper is to describe the selection and use of secondary data analysis methods to accurately capture the data used for triage decisions at the time of a large chlorine leak that occurred in Graniteville, South Carolina in 2005. The research methods described in this paper show the potential use of well designed secondary analysis methods to improve mass casualty research.
RESEARCH DESIGN AND METHODS
Study Population
On January 6, 2005, a freight train carrying tanker cars of liquid chlorine was inadvertently switched onto an industrial spur in the center of Graniteville, South Carolina, where it crashed into a parked locomotive. The train then derailed and one of the heavily damaged chlorine tankers was ruptured, immediately releasing approximately 60 tons of the 90 tons of chlorine it was carrying. Within minutes, the dense chlorine gas infiltrated the surrounding town with a population of over 7,000. Many people fled the town before they were overcome by the chlorine. Yet nine people died, 72 were hospitalized in nine regional hospitals, 840 were treated as outpatients, and 220 experienced immediate health problems, but did not receive any immediate medical care.44 Others experienced health problems only associated with the psychological trauma of the disaster. We know of 1,384 victims of this event. This study focuses on the observed clinical data collected at the time of the chlorine leak incident to determine if the criteria modeled in the four most frequently used triage systems accurately predict the severity of respiratory signs/symptoms necessitating medical intervention at the hospitals. This disaster site is located in South Carolina near the border of Georgia.7,8
This research applies an all hazards approach to study the validity of four triage models using physiological measurements, signs/symptoms, exposure severity ratings and medical outcome categories collected in six chlorine leak datasets. This is a retrospective study using data extracted from medical records of chlorine disaster victims. Specifically, mass casualty data were abstracted by the South Carolina Department of Health and Environmental Control (SC DHEC) in conjunction with the Centers for Disease Control and Prevention (CDC) from hospital records of victims who received medical care after the 2005 chlorine release in Graniteville, South Carolina8. Due to the scale of the disaster, medical chart abstraction was limited to both the hospitalized patients and those who were treated multiple times in the emergency room because it was assumed that those patients would have been hospitalized in the absence of a surge and if there were beds available. Our first step was creating a merged de-identified research dataset from these abstracted data that included the needed input data for each triage model, the patients’ clinical outcome, demographics, and other elements which were useful for developing an improved triage model. Then, the required data for each triage model were mapped to the collected data. The logic of the triage decision tree was then coded in Statistical Analysis System (SAS) software producing the predicted clinical outcome categories for each triage model. Observed patient outcome categories were derived from the clinical treatment records using the duration of required medical care and severity of reported injury.7,8 The predicted triage model outcome categories were then compared to the observed patient clinical outcome categories.
Table 1 includes data points for the adult triage models used in our study to assess mass casualty patients and the priority categories assigned to these assessments.
Table 1.
Summary of Triage Models, Data Points and Data Analysis Classification
| TRIAGE MODELS | START | ESI | CBRN | SALT |
|---|---|---|---|---|
| All ages | All Ages | Adults | Adults | |
| DATA POINTS | • Respirations | • Ability to follow commands | • Ability to walk | • Ability to follow commands |
| ■ If > 8 years old > 30 or < 10 | • # resources needed | • Ability to follow commands | • Respirations | |
| ■ If < 8 years old > 45 or < 15 | ■ If < 3 months old > 180 • Pulse | • Respirations | ■ > 0 | |
| ■ If > 3 months and < 3 years old > 160 | • Toxidrome | • Pulse | ||
| • Perfusion | ■ Eye burning | ■ > 0 | ||
| • Mental Status | ■ If > 3 years old and < 8 years old > 140 | ■ Cough | • Respiratory distress | |
| – Ability to walk | ■ Skin burning | |||
| – Ability to follow commands | ■ If > 8 years old > 100 | ■ Wheezing | • Number of injuries | |
| • Respirations | ■ ENT burning | |||
| ■ If < 3 months old > 50 | ■ Vomiting or nausea | • # resources needed | ||
| ■ If > 3 months and < 3 years old > 40 | • Injuries | |||
| • Decon prior to transport | ||||
| ■ If > 3 years old and < 8 years old > 30 | ||||
| ■ If > 8 years old > 20 | ||||
| • O2 Saturation | ||||
| ■ All ages < 92% | ||||
| • Pain | ||||
| CATEGORY | • Black -Deceased | • Level 0 | • T4 | • Dead |
| • Red - Immediate | • Levels 1 & 2 | • T1 | • Expectant | |
| • Yellow -Delayed | • Level 3 & 4 | • T2 | • Immediate | |
| • Green - Minor | • Level 5 | • T3 | • Minimal |
Wenck, et al.7 used medical care as the medical outcome measure in their epidemiologic surveillance after the event. They used nine medical outcome categories to classify the duration of hospitalization and need for intensive care support for patients who received care following the Graniteville chlorine exposure. The nine medical outcome categories and the relationship of the outcome category and the triage system classification are described in Table 2. These observed medical outcome categories (Observed Outcome Category – OUTCOMECAT) provide a suitable measure of medical outcome for our study.
Table 2.
Outcome Classification For Four Triage Models
| OBSERVED OUTCOME37 | START | ESI | CBRN | SALT |
|---|---|---|---|---|
| Deceased | BLACK | LEVEL 0 | T4 | DEAD |
| ICU/Ventilator | RED | LEVEL 1 and 2 | T1 | IMMEDIATE |
| Hospitalized 3+ days | RED | LEVEL 1 and 2 | T1 | IMMEDIATE |
| Hospitalized 1-2 days | RED | LEVEL 1, 2 and 3 | T1 | IMMEDIATE |
| ED repeat visits | YELLOW | LEVEL 3 and 4 | T2 | MINIMAL |
| ED with significant Symptoms | YELLOW | LEVEL 3 and 4 | T2 | MINIMAL |
| ED with moderate Symptoms | YELLOW | LEVEL 3 and 4 | T2 | MINIMAL |
| ED without Symptoms | GR EEN | LEVEL 5 | T3 | MINIMAL |
| Physician office visit | GREEN | LEVEL 5 | T3 | MINIMAL |
The SC DHEC datasets include information on patients hospitalized in nine hospitals, (n=71) examined as outpatients during the first few days after the accident (n=630), or those who died (n=9). The data included patients who ranged in age from 4 months to 85 years of age, were 58.9% male, 59.9% white, 35.2% black, 2.5% Hispanic and 2.4% other or unknown37.
All data have their inherent strengths and flaws, including the datasets that we proposed to study. We analyzed data from several datasets: the hospitalized (n=71) and multiple emergency room admitted patient abstracted medical records (n=49), medical service provider reports (n=630), the health registry (n=958), voluntary health screenings (3 datasets, n=259, n=69, and n=30), and the epidemiological follow-up interviews of reportedly exposed persons (n=287, n=94). All of these dataset were collected exclusively for public health purposes, not research. Therefore, the self-reported and voluntarily collected data from the interviews and health screenings had more missing data than traditional research-specific datasets. However, because these are public health datasets, the abstracted medical records and immediate epidemiological reporting data are rather complete as to reporting compliance because hospitals and doctor's offices were required by law to report cases of chlorine associated illness to SC DHEC. However, some record keeping was not as complete as we would have liked. The surge of patients into the regional hospitals forced the clinicians to first focus on treating the patients and providing detailed clinical notes second.45 Often there was only minimal detail provided in the clinical notes, which was understandable given the surge status at the hospitals. A standardized paper medical record abstraction form (The Graniteville Chlorine Chart Abstraction Form) was used for all medical record abstractions, and trained epidemiologists abstracted all medical records. Further details on the medical record abstraction process are found elsewhere.8 Likewise, health screenings were comparable to the rigorous data quality obtained from similar research-based studies44. All data from both self-report and abstracted hospital/doctor reported sources were duplicately entered and reviewed for quality assurance prior to being issued as the official study datasets. Of the available datasets, the following datasets were used in the study.
1) Hospitalization database. The medical records of all persons hospitalized (n=71) were abstracted. The following information were collected: demographics, clinical presentation, physical examination, laboratory, pulmonary, and radiological studies, pulse oximetry, medical treatment, medical outcome category (duration of hospitalization and need for intensive care support) and diagnosis.
2) Multiple Emergency Room Admitted Patients. The medical records of all persons seen in the emergency room multiple times (n=49) were abstracted. The rationale for abstracting these in addition to the hospitalized patient records was that these patients would have most likely been admitted under non-surge conditions rather than treated in the emergency department, observed for several hours, and then released with instructions to return if they required further medical care. The following information was collected: demographics, clinical presentation, physical examination, laboratory, pulmonary, and radiological studies, pulse oximetry, medical treatment, medications, medical outcome category (duration of hospitalization and need for intensive care support), and diagnosis.
3) Medical Service Provider Reports. The datasest includes emergency room logs, and a rapid epidemiological assessment database. Personnel from the CDC in conjunction with the SC DHEC collected data via interviews and medical record abstraction for individuals who sought medical care. Information includes exposure information, symptoms experienced, details about decontamination and transport to medical care, preexisting cardiac or pulmonary medical conditions, and exposure severity ratings (5 point scale). Patients (n=605) were classified according to nine medical categories. Demographic characteristics of people who received medical care are stratified by primary exposure location and duration.
The data were combined so that the variables across datasets were associated with the same patient correctly.
The datasets were explored, using SAS (SAS Institute Inc., Cary, NC, USA) version 9.2 statistical software, identifying data points as candidates for the decision tree model(s). To insure data quality, the combined datasets were analyzed using visualization techniques such as histograms and statistic measures such as range, mean, median, and outliers to quantify completeness and validity of responses. Spearman correlation was used to examine the relationship between four triage outcomes with signs/symptoms variables. The Kappa statistic was used to examine the agreement between the triage models. Decision algorithms were developed to aid in the evaluation of variables where the data points appear in multiple datasets and for the case when a direct variable was not available in any of the datasets. From these results, modifications were implemented to address issues of missing values, outliers or clustering of data. This study was approved by both the Institutional Review Board of the University of South Carolina and the South Carolina Department of Health and Environmental Control. All databases were linked within the South Carolina Office of Research and Statistics, de-identified, and provided with a unique personal identification number prior to our receipt of the study data.
DETAILS USING SAS
The steps below outline a repeatable process for evaluating mass casualty data. The process addresses (1) assessment of datasets and (2) columns, providing suggestions for managing incomplete data (3) creating variables from existing data points, and (4) coding the decision tree logic for triage models.
We were fortunate that de-identified data sets were available for our use. However, we took precautions to protect the datasets at all times. The files were delivered encrypted with a password key then stored on a password protected server that was backed up nightly.
Step 1 – Analyze data sets and data points
The public health data sets collected from the Graniteville chlorine disaster were merged to generate a research dataset useful for further analysis. The data were examined for completeness and to identify data points that fulfilled the needed input data points used in the triage models. The first step was to compare the data points across the datasets and choose which ones to include for further analysis. We made a decision to focus on the data recorded by the emergency room or the hospital on the day of the incident (the incident occurred at 2:39 am). This time period best represented when triage tools were being used to assess the victims at the hospitals.
The Graniteville Chlorine Chart Abstraction Form is a multi-page document used during the data abstraction; a portion of the data points are displayed in Table 3. The form was designed such that the abstractor filled in a blank or checked a box indicating if a condition was present or not. This form was examined for useful data points to be included in the research dataset. The last column indicates if the column was a candidate for use in the triage decision tree logic or in the creation of variables required for the decision tree. Many variables were considered as candidates, but many were discarded due to the large amount of missing data. If the variable was used in the logic model or in creation of derived variables, it was noted. For example, the emergency room visit date was considered and used, hence the ‘Yes / Yes’ in the final column in the table below. A blank in the second column (Variable Name) indicates the abstraction form data was not present in the dataset. A blank in the third column (Further Analysis / Used) indicates the data element was not used in our analysis. Many elements on the abstraction form were not considered useful and not included in Table 3.
Table 3.
Graniteville Chlorine Chart Abstraction Form Mapping
| I. Demographic Information | |
|---|---|
| Questionnaire Name | Further Analysis / Used |
| Study ID # | Yes |
| ER Visit Date | Yes / Yes |
| Admission Date | Yes |
| ICU Admission Date | Yes |
| Discharge Date | Yes |
| ICU Discharge Date | Yes |
| Gender | Yes / Yes |
| Date of Birth | Yes / Yes |
| Race | Yes / Yes |
| II Chief Complaint | |
| Questionnaire Name | Further Analysis / Used |
| PULMONARY | Yes / Yes |
| CARDIAC | Yes |
| DEMATOLOGIC | Yes |
| OPTHALMOLOGIC | Yes |
| EAR, NOSE, THROAT | Yes |
| OTHER | Yes |
| III. Past Medical History and Symptoms | |
| Questionnaire Name | Further Analysis / Used |
| MEDICATIONS | Yes |
| HISTORY OR PREVIOUS HOSPITALIZATION FOR PULMONARY DISEASE | Yes |
| IV. Data from Emergency Room | |
| Questionnaire Name | Further Analysis / Used |
| Date | Yes / Yes |
| Time | Yes |
| Vital: Temp | Yes |
| BP | Yes / Yes |
| BP | Yes |
| Respiratory rate | Yes / Yes |
| Heart rate | Yes / Yes |
| Time | |
| O2 Sat | Yes / Yes |
| On room Air | Yes / Yes |
| On liters of O2 via nasal canula (NC) or face mask | Yes |
| On 100% non-rebreather (NRB) | Yes |
| On continuous Positive Airway Pressure (CPAP)with | Yes |
| On ventilator with___%O2 | Yes |
| Notes from Emergency Room | Yes / Yes |
| Physical Exam | |
| Questionnaire Name | Further Analysis / Used |
| Eye | Yes / Yes |
| Red | Yes |
| Other | Yes |
| Ear, Nose, Throat | Yes / Yes |
| Rhinorrhea | Yes |
| Other | Yes / Yes |
| Yes / Yes | |
| Pulmonary | Yes |
| Tachupnea | Yes |
| Cough | Yes / Yes |
| Cyanosis | Yes |
| Decreased breath sounds | Yes |
| Stridor | Yes |
| Wheezing | Yes / Yes |
| Crackles | Yes |
| Rhonchi | Yes |
| Intercostals retractions | Yes |
| Cepitus | Yes |
| Other | Yes |
| Cardiac | Yes |
| Tachycardia | Yes |
| Murmur | Yes |
| Dematology | Yes |
| Burn | Yes / Yes |
| Other | Yes / Yes |
| Data from Repeat ER Visit or Admission H&P | |
| Questionnaire Name | Further Analysis / Used |
| Date | Yes |
| Time | Yes |
| Vitals: Temp | Yes |
| Ht | Yes |
| Wt | Yes |
| BP | Yes |
| BP | Yes |
| Respiratory rate | Yes / Yes |
| Heart rate | Yes / Yes |
| O2 Sat | Yes / Yes |
| On room Air | Yes |
| On liters of O2 via nasal canula (NC) or face mask | Yes |
| On 100% non-rebreather (NRB) | Yes |
| On continuous Positive Airway Pressure (CPAP)with | Yes |
| On ventilator with ___%O2 | Yes |
| Ventilator other | Yes |
| Physical Exam | |
| Questionnaire Name | Further Analysis / Used |
| Eye | Yes |
| Red | Yes |
| Other | Yes |
| Ear, Nose, Throat | Yes |
| Other | Yes |
| Pulmonary | Yes |
| Tachupnea | Yes |
| Cough | Yes |
| Cyanosis | Yes |
| Decreased breath sounds | Yes |
| Stridor | Yes |
| Wheezing | Yes |
| Crackles | Yes |
| Rhonchi | Yes |
| Intercostals retractions | Yes |
| Cepitus | Yes |
| Other | Yes / Yes |
| Cardiac | Yes |
| Tachycardia | Yes |
| Dermatology | Yes |
| Other | Yes |
| Outcomes | |
| Questionnaire Name | Further Analysis / Used |
| Outcome | Yes |
| Chlorine exposure | Yes |
| Other Disease | |
| Primary Diagnosis | Yes / Yes |
| Tests/Procedures | |
| Questionnaire Name | Further Analysis / Used |
| EKG Date | Yes / Yes |
| Brochoscopy 1ST Date | Yes / Yes |
| Pulmonary Date | Yes / Yes |
| Consults | |
| Questionnaire Name Further Analysis / Used | |
| Pulmonology Yes | |
| Dermatology Yes | |
| Opthalmology Yes / Yes | |
| Abstracted Information Not on Graniteville Abstraction Form but included in Dataset | |
| Abstracted Data | Further Analysis / Used |
| Victim transportation method | Yes / Yes |
| Repeat admission boolean | |
| First Symptoms | Yes / Yes |
| Outcome Category | Yes / Yes |
| Decontamination Location | Yes |
| ICU boolean | Yes |
| Number of days in ICU | Yes |
| Hospitalized | Yes |
| Days in hospital | Yes |
| Person exposed | Yes |
| Distance in miles from site | Yes |
We used SAS procedures (proc format and proc freq) to obtain the frequency distribution for the categorical data points in the data sets and we used proc means for the numeric data points. The analysis helped identify areas of missing data and outliers, therefore, aiding in the selection of the best data points to use in the analysis.
Step 2 – Select data points
Decisions were made to use a combination of data points to build variable(s) for the triage model(s) when the required data point was not directly collected and recorded. For example, the ability to walk is an input data point for triage. However, the value for the ability to walk was not recorded in any of the datasets. Instead, the ability to walk was derived from other collected data. We assumed a person was able to walk unless he or she was intubated or was hypoxic (<90% oxygen saturation measured by pulse oximetry). Other input variables such as heart rate or respiration rate were directly available for use in the models. Table 4 outlines the input data points for each model.
TABLE 4.
Clinical Data Points Used For The Decision Logic In Each Triage Model
| Data Point | DESCRIPTION | START | ESI | CBRN | SALT |
|---|---|---|---|---|---|
| AGE | Age in years on date of incident | x | x | x | x |
| CHLORINE EXPOSURE* | Evidence of toxidrome (chlorine) | x | |||
| FOLLOWS DIRECTIONS* | Ability to follow directions | x | x | x | x |
| HEART RATE | Heart rate | x | x | ||
| O2 SATURATION | O2 Saturation | x | |||
| RESPIRATORY DISTRESS | Evidence of respiratory distress | x | x | ||
| RESPIRATORY RATE | Respiration rate | x | x | x | x |
| SYSTOLIC BLOOD PRESSURE | Systolic pressure | x | |||
| ABLE TO WALK* | Ability to walk | x | x | ||
| INJURY OR HEMORRHAGE* | Major hemorrhage or severe injury | x | |||
| NUMBER OF RESOURCES* | Number of medical resources required for care | x | x | ||
| PAIN* | Evidence of pain | x |
Indicates that this data point was derived from several other recorded data points.
Step 3 – Create new data points and manage missing data
The Graniteville abstraction form was designed to capture the information needed to perform the descriptive epidemiology for the disaster and not for research purposes. Therefore, some information required for the triage models was not explicitly collected. As a result, we collectively made data point derivation decisions based on available data if sufficient information was available from multiple data points on the form to derive the value for the missing data point. For example, the CBRN model asks if there is evidence of toxidrome, or signs and symptoms consistent with exposure to a toxic chemical. We created a variable for chlorine exposure based on the data from the physical exam performed in the emergency department. The abstraction form has check boxes for yes/no answers to eye issues, ear/nose/throat issues, and presence of a cough, wheezing, or burning skin because these are the hallmark signs of injury resulting from chlorine exposure. If any were checked, we indicated that the victim was exposed and had evidence of toxidrome. Additionally, we considered the first symptoms and set the toxidrome status to indicate that the victim was exposed to chlorine if vomiting or nausea was reported. Our justification being swallowing mucus secreted in response to chlorine exposure in the airways can cause nausea and/or vomiting due to these mucus secretions becoming acidic after exposure to chlorine.
When applying the SALT triage tool in practice, the first responder is required to make a decision if the victim has a major hemorrhage. There was no indicator data point for a major hemorrhage on the abstraction form because the focus of the public health descriptive epidemiology was on the chlorine injuries, not any injuries from the train derailment itself. It was well known at the time that the abstraction form was designed that few people were directly injured by the derailment itself, and that such injuries were not the cause of the epidemic of illness within the community. Therefore, no data were specifically abstracted for assessing degree of traumatic injury or major hemorrhage. After examining the available notes and other data points abstracted, we decided to create a variable indicating a major hemorrhage. We looked for a specific term in the primary diagnosis variable or in the ophthalmology consult. When either variable had the text ‘inj’ we derived that they were injured and hemorrhaging.
The ESI triage model asks the question ‘How many different resources are needed?’ and the SALT triage model asks the question ‘Likely to survive given current resources?’ The ESI decision logic branches according to the number of resources utilized while the SALT decision logic branches if resources are available or not. We created a variable that counted the number of resources used on each victim. For example, if the victim was not breathing with room air we counted a resource. The methods that indicated the victim was not breathing room air were oxygen with a face mask or nasal canula, 100% oxygen with a re-breather, on Continuous Positive Airway Pressure (CPAP), or on a ventilator. We counted a resource if the victim received an EKG, a bronchoscopy, a pulmonary function test, or was on intravenous fluids. Lastly, we looked for the term ‘Intubated’ in the Emergency Department notes. The minimum resources a victim could have had was 0, the maximum was 6.
Evidence of pain was used in the decision logic for the ESI model. Once again, we derived a variable to indicate if the victim was in pain or not. We assumed the victim was not in pain unless we found indicators that he or she was in pain. We selected a subset of the check boxes abstracted from the physical exam performed in the Emergency Department to indicate pain was present. If any check box under the Ear, Nose, and Throat section was checked or any item under the Dermatology section was checked, we set the pain data point to yes. Similarly, if we found text indicating burning or pain, we set the pain data point to yes.
To manage the case when a victim was immediately admitted without going through the emergency department, we substituted the corresponding admission data points (AD) for the emergency department (ED) data points. This increased the number of victims which we could classify.
Step 4 – Code decision tree
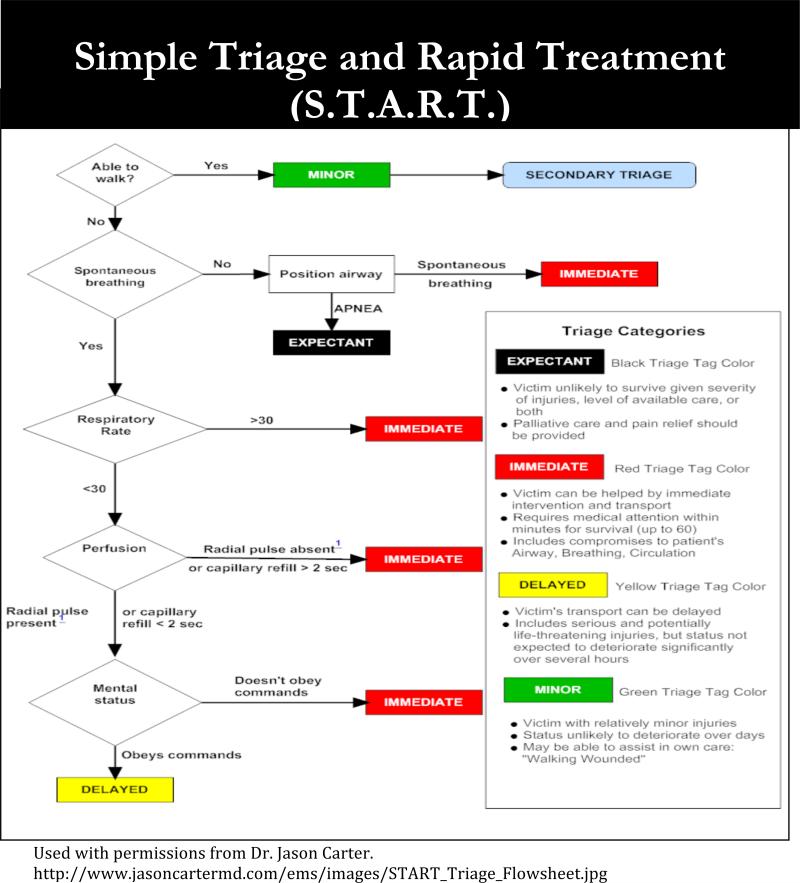
The triage models are decision trees to help emergency clinicians ascertain which patients need care first. We translated the triage decision logic into IF/THEN statements using SAS to implement the models. The diagram for the Simple Triage and Rapid Treatment (START) tool for adults (Age > 8) is provided in Figure 1 as an illustration. There is a similar diagram for children.
Figure 1.
START Triage Tool Diagram
The first decision in the model is to determine if the victim can walk. As described earlier in the document, we derived the ability to walk. The next decision in the model is if the victim is breathing. We matched breathing to ‘Respiratory rate’ on the abstraction form. If the rate is 0, then the victim is assigned the classification of black. If the rate is too low or too high then the victim is classified as red. Next, the circulation is considered, specifically if a pulse is present. We chose to use the systolic blood pressure reading as an indicator for measuring capillary refill. The value of 70 was chosen as the cutoff point to match to a capillary refill of > 2 sec. The final decision for START is if the victim can follow directions. The START triage rules for the young victims, those 8 years old or less, consider only the respiratory rate in the logic. SAS code for the START and other triage trees can be provided upon request. Pseudo code for the START logic is provided below:
S.T.A.R.T. Simple Treatment and Rapid Transport
Inputs: AGE, EDFOLLOW, EDRR, EDSYSTOLIC, EDWALK
IF EDWALK = ‘Y’ THEN GREEN
IF AGE <=8 THEN
IF EDRR = 0 THEN BLACK
IF EDRR > 45 OR EDRR < 15 THEN RED
IF EDRR <= 45 AND EDFOLLOW = N THEN RED
IF EDRR <=45 AND EDFOLLOW = Y THEN YELLOW
IF AGE >8 THEN
IF EDRR = 0 THEN BLACK
IF EDRR > 30 OR EDRR < 10 THEN RED
IF EDRR <= 30 AND EDSYSTOLIC < 70 THEN RED
IF EDRR <= 30 AND EDSYTOL IC >= 70 AND EDFOLLOW = N THEN RED
IF EDRR <=30 AND EDSYSTOLIC >= 70 AND EDFOLLOW = Y THEN YELLOW
ELSE NOT CLASSIFIED
We evaluated version 4 of the Emergency Severity Index (ESI) triage tool. A diagram for the ESI model is provided in Figure 2.
Figure 2.
ESI Triage Tool Diagram
The ESI tool applies to all ages taking into account different thresholds for the vital signs of each age category. The first assessment is whether the victim requires immediate intervention. Immediate intervention includes issues with the airway, requiring emergency medications, needs to be intubated, is in respiratory distress (oxygen concentration < 90%), has no pulse or is unresponsive. We used the derived variables respiratory distress and inability to follow directions to mean unresponsive along with oxygen saturation value < 90% for the first decision. The next assessment is whether the victim is in a high risk situation, has abnormal responsiveness (confused/lethargic/disoriented), or is in severe pain taking into consideration the vital signs of heart rate, respiratory rate and oxygen saturation. We mapped the high risk situation to having an oxygen concentration < 92%, having a high heart rate, or a high respiratory rate. The comparison values for heart rate and respiratory rate differ by age category. We mapped abnormal responsiveness to the inability to follow directions and pain to the derived pain data point. The next assessment is based on the number of resources required and if many resources are required then the vital signs for the heart rate, respiratory rate and the oxygen saturation are considered. The model has four age categories for age when considering the vital signs. The age categories are less than 3 months, between 3 months and 3 years, age 3 to 8 years, and over 8 years of age.
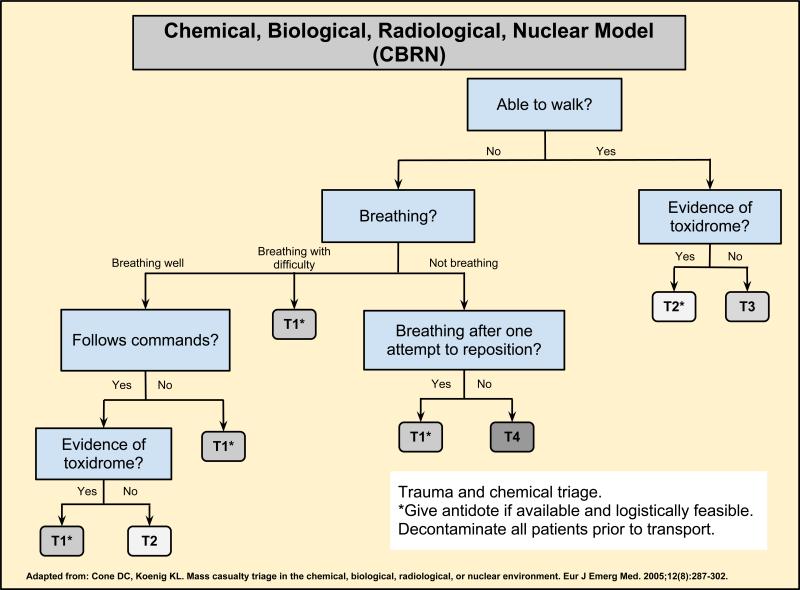
A diagram for the Chemical/Biological/Radiological/Nuclear (CBRN) triage tool is provided in Figure 341. CBRN triage addresses primary triage for immediate action and secondary triage for decontamination. The CBRN model classifies victims into four categories (T1, T2, T3, T4) and is valid for victims over the age of 8. The first decision in the model is whether the victim can walk. If the victim can walk, the next assessment is for evidence of toxidrome to ascertain the decontamination classification. We used the derived chlorine exposure data point to indicate the evidence of toxidrome. If the victim is unable to walk, the next decision is based on the ability to breath - which is further categorized into breathing well, breathing with difficulty or not breathing. We mapped breathing with difficulty to being in respiratory distress. We mapped not breathing to having a respiratory rate of 0. Otherwise, we assumed the victim was breathing well. For victims breathing well, the next decision is based on the ability to follow directions followed by if there is evidence of toxidrome.
Figure 3.
CBRN Triage Tool Diagram
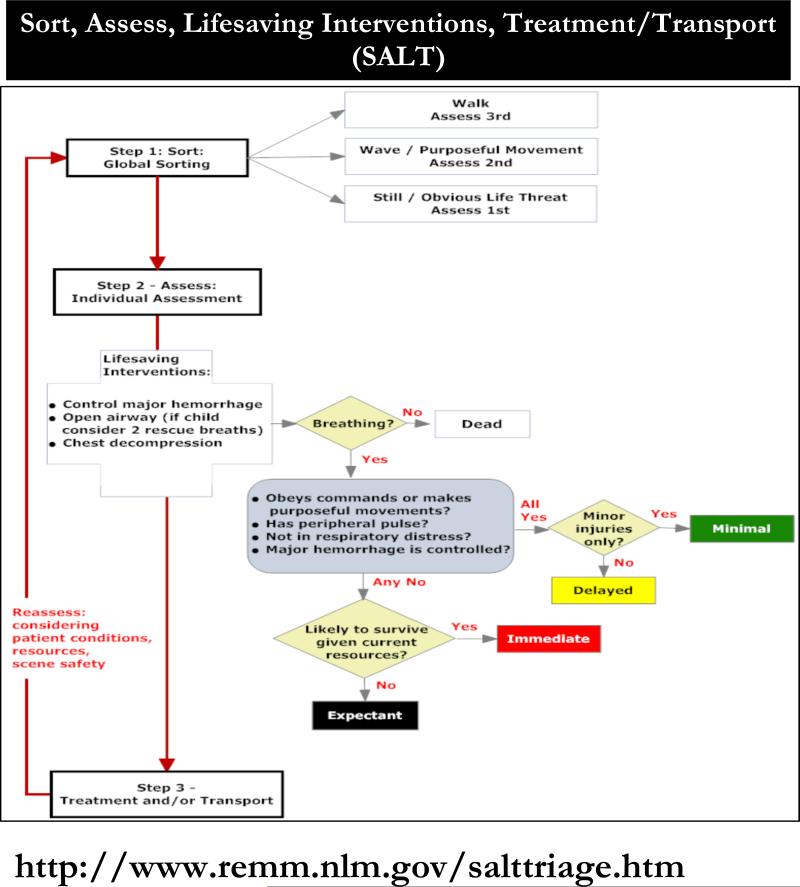
The SALT triage model, illustrated in Figure 442, has a multi step solution to victim prioritization and classification. The first step is to quickly sort the victims into groups then to assess individuals within each group giving priority to the victims that are not moving or have an obvious life-threatening situation. We did not implement the sorting in our SAS code. The first decision for the individual assessment is whether the victim is breathing. We used the respiratory rate > 0 to indicate if the victim is breathing. The next decision is based on answers to the following questions: (1) Obeys commands or makes purposeful movements? (2) Has peripheral pulse? (3) Not in respiratory distress? (4) and Major hemorrhage controlled? We mapped the ability to obey commands to this previously mentioned derived data point, having a peripheral pulse to having a heart rate > 0 (since only heart rate was available in the abstracted data), not in respiratory distress to this previously mentioned derived data point, and we assumed all major hemorrhages were controlled. If the victim could pass the four questions, the next decision is based on the presence of minor injuries. We used the derived injury data point to determine if the victim was classified as minimal or delayed. If the victim did not pass all four questions, the next decision is based on the available resources. We mapped the derived resource data point > 0 to classify the victim as immediate or expectant. We then compared the modeled results against the derived outcome category.
Figure 4.
SALT Triage Tool Diagram
DISCUSSION
The methods and steps followed for management of data, analysis of data, coding of triage decision logic can easily be followed and implemented for similar situations. The SAS implementation is provided in Appendix A and serves as a guide for other researchers to follow. Note, the creation of variables is performed in one section before the triage decision logic, making it easy to adjust the derivation logic without interfering or requiring any changes in the triage decision logic. This proved to be quite helpful as we analyzed the data and altered the rules for deriving the missing variables. The major decisions revolved around the data and the fact that similar data were found across the available datasets along with the fact that we had incomplete data, missing data and additional data points not referenced in the available documentation related to the data sets. Once we obtained answers to detailed questions regarding the datasets we were able to move forward. Using SAS to compare data with frequency distributions for the categorical data and min, max, count, average for the numeric data proved extremely helpful in data point selection.
Coding the triage logic is straight forward and likely not subject to question or accuracy. However, the derivation for missing data points required for the triage decision logic is subject to opinion. The hope is that we gain access to more complete data for the victims so we can re-run the triage decision models without derived data points. In the absence of this information, we relied on our clinical expertise to guide the decision making.
CONCLUSIONS
We conclude that the methodology outlined in this paper can be followed or extended in evaluating the performance efficacy of triage models. The steps are reliable and repeatable and can easily be extended to other triage models or applied to other datasets or data sources. Our specific research has two areas where the data has room for improvement. The first area is the reliance on secondary data in the creation of derived data points required for the triage modeling in SAS. The second area is in the reliance on using the observed outcome category as the value to compare the predicted triage model classifications to. In both cases, secondary data was used in the creation of the variables. Ideally, we would not have to rely on derived variables at all.
ACKNOWLEDGEMENT
This study was supported by the National Institutes of Health/The National Library of Medicine (5R21LMO10833-01) and approved by the Institutional Review Boards from the University of South Carolina and the South Carolina Department of Health and Environmental Control (SC DHEC). We would like to acknowledge Dr. David Van Sickle and his team from the CDC and the SC DHEC for their efforts to abstract and enter the epidemiological surveillance data which we used for this research. We wish to thank Chris Finney from the South Carolina Office of Research and Statistics for providing the merged data in a de-identified format for this study, and Ben Card for providing the technology resources to protect the data and for teleconferencing support.
Credits: This study was supported by the National Institutes of Health/The National Library of Medicine (5R21LMO10833-01)
Contributor Information
Jean B. Craig, Office of Biomedical Informatics Services, Medical University of South Carolina 55 Bee Street Charleston, SC 29425 Telephone: 843-792-5350; Fax: 843-792-1262 craigje@musc.edu.
Joan M. Culley, College of Nursing, University of South Carolina.
Abbas Tavakoli, Director of Statistical Lab, College of Nursing, University of South Carolina.
Erik R Svendsen, Tulane University School of Public Health and Tropical Medicine, Department of Environmental Sciences.
REFERENCES CITED
- 1.Culley JM, Effken JA. Development and validation of a mass casualty conceptual model. J Nurse Scholarship. 2009;42(1):66–75. doi: 10.1111/j.1547-5069.2009.01320.x. DOI:10.1111/j.1547-5069.2009.01320.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McGarvey D, Shroy B. Modeling chemical terrorism risk through probabilistic risk assessment.. Paper presented at the 2011 Chemical and Biological Defense Science Technology Conference; Las Vegas, NV. Available at http://cbdstconf2011.sainc.com/parallelSessionView2.aspx?ConferenceSessionId=29. Accessed 16 July 2012. [Google Scholar]
- 3.Ash S, Stoto M, Mendes M, Valdez R, Gallagher M, Halverson P, Lurie N. A review of instruments assessing public health preparedness. Pub Health Rep. 2005;120(5):532–542. doi: 10.1177/003335490512000508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cone DC, Koenig KL. Mass casualty triage in the chemical, biological, radiological, or nuclear environment. Eur J Emerg Med. 2005;12(6):287–302. doi: 10.1097/00063110-200512000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Kahn C, Schultz C, Miller K, Anderson C. Does START triage work? An outcomes level assessment of use at a mass casualty event. Acad Emerg Med. 2009;53(3):424–430. doi: 10.1016/j.annemergmed.2008.12.035. [DOI] [PubMed] [Google Scholar]
- 6.Cone DC, MacMillan DS, Parwani V, et al. Pilot test of a proposed chemical/biological/radiation/nuclear-capable mass casualty triage system. Prehosp Emerg Care. 2008;12(2):236–240. doi: 10.1080/10903120801907620. [DOI] [PubMed] [Google Scholar]
- 7.Wenck MA, Van Sickle D, Drociuk D, et al. Rapid assessment of exposure to chlorine released from a train derailment and resulting health impact. Public Health Reports. 2007;122(6):784–792. doi: 10.1177/003335490712200610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Sickle D, Wenck MA, Belflower A, et al. Acute health effects after exposure to chlorine gas released after a train derailment. The American Journal of Emergency Medicine. 2009;27:1–7. doi: 10.1016/j.ajem.2007.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frykberg ER. Medical management of disaster and mass casualties from terrorist bombings: How can we cope? J Traum. 2002;53(2):201–212. doi: 10.1097/00005373-200208000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Jenkins J, McCarthy M, Sauer L, et al. Mass-casualty triage: Time for an evidence-based approach. Prehosp Disaster Med. 2008;23(1):3–8. doi: 10.1017/s1049023x00005471. [DOI] [PubMed] [Google Scholar]
- 11.Armstrong J, Frykberg E, Burnis D. Toward a national standard in primary mass casualty triage. Disaster Med Public Health Prep. 2008;2(1):S8–S10. doi: 10.1097/DMP.0b013e31818582a5. [DOI] [PubMed] [Google Scholar]
- 12.Fernandes C, Tanabe P, Gilboy N, et al. Five-level triage: A report from the ACEP/ENA five-level triage task force. J Emerg Nurs. 2005;31(1):39–50. doi: 10.1016/j.jen.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 13.Joint Commission on Accreditation of Healthcare Organizations (JCAHO) Standing Together: An Emergency Planning Guide for America's Communities. Oakbrook; Terrace, Ill: 2005. [Google Scholar]
- 14.Task Force on Quality Control of Disaster Management Health Disaster Management: Guidelines For Evaluation And Research in The Utstein Style: Executive Summary. Available at www.laerdalfoundation.org/dok/Health_Disaste_%20Management.pdf. Accessed 16 July 2012. [PubMed]
- 15.Birnbaum M. Disaster medicine: Status, roles, responsibilities, and needs. J Prehosp Disaster Med. 2002;17(3):II7–I18. doi: 10.1017/s1049023x00000327. [DOI] [PubMed] [Google Scholar]
- 16.Chan T, Killeen J, Griswold W, et al. Information technology and emergency medical care during disasters. Acad Emerg Med. 2004;II:1229–1236. doi: 10.1197/j.aem.2004.08.018. [DOI] [PubMed] [Google Scholar]
- 17.Benson M, Koenig KL, Schultz CH. Disaster triage: START, then SAVE – a new method of dynamic triage for victims of a catastrophic earthquake. Prehosp Disaster Med. 1996;11(2):117–124. doi: 10.1017/s1049023x0004276x. [DOI] [PubMed] [Google Scholar]
- 18.Ihlenfeld JT. A primer on triage and mass casualty events. Dimens Crit Care Nurs. 2003;22(5):204–207. doi: 10.1097/00003465-200309000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Knopp R, Yanagi A, Kallsen G, et al. Mechanisms of injury and anatomic injury as criteria for prehosiptal trauma triage. Ann Em Med. 1988;17(9):895–902. doi: 10.1016/s0196-0644(88)80666-8. [DOI] [PubMed] [Google Scholar]
- 20.Landau TP, Ledley RS, Champion HR, et al. Decision theory model of the emergency medical triage process. Comput Biol Med. 1982;12(1):27–42. doi: 10.1016/0010-4825(82)90010-5. [DOI] [PubMed] [Google Scholar]
- 21.Schultz DH, Koenig KL, Noji EK. A medical disaster response to reduce immediate mortality after an earthquake. New Engl J Med. 1996;334(7):438–444. doi: 10.1056/NEJM199602153340706. [DOI] [PubMed] [Google Scholar]
- 22.Kilner T. Triage decisions of prehospital emergency health care providers, using a multiple casualty scenario paper exercise. Emerg Med J. 2002;19:348–353. doi: 10.1136/emj.19.4.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Burstein JL, Henry MC, Alicandro JM, et al. Evidence for and impact of selective reporting of trauma triage mechanisms criteria. Acad Med. 1996;3(110):1011–1015. doi: 10.1111/j.1553-2712.1996.tb03344.x. [DOI] [PubMed] [Google Scholar]
- 24.Parker M. Critical care and disaster management. Crit Care Med. 2006;34(3 Suppl):S52–55. doi: 10.1097/01.CCM.0000199988.96002.CC. [DOI] [PubMed] [Google Scholar]
- 25.MacKenzie MH, Alcorta EJ, Kelen GD. Compliance with prehospital triage protocols for major trauma patients. J Trauma. 1999;46(1):168–175. doi: 10.1097/00005373-199901000-00029. [DOI] [PubMed] [Google Scholar]
- 26.Hoey GA, Schwab CW. Level I center triage and mass casualties. Clin Orthop Relat Res. 2004;422:23–29. doi: 10.1097/01.blo.0000129151.99893.0b. [DOI] [PubMed] [Google Scholar]
- 27.Domres B, Koch M, Mange A, et al. Ethics and triage. Prehosp Disaster Med. 2001;16(1):53–58. doi: 10.1017/s1049023x00025590. [DOI] [PubMed] [Google Scholar]
- 28.Sharma R. Development of pre-hospital trauma-care-system—an overview. Injury. 2005;36(5):579–587. doi: 10.1016/j.injury.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 29.Gebbi K, Merill J. Public health worker competencies for emergency response. J Public Health Man. 2002;8(3):73–81. doi: 10.1097/00124784-200205000-00011. [DOI] [PubMed] [Google Scholar]
- 30.Rüter A. Disaster Medicine- Performance Indicators, Information Support and Documentation. Liu-Tryck; Linköping, Sweden: 2006. [Google Scholar]
- 31.Birnbaum M. Disaster research: Why how and when? Prehosp Disaster Med. 2000;15(3):s88. [Google Scholar]
- 32.Auf der Heide E. The importance of evidence-based disaster planning. Ann Emerg Med. 2006;47(1):34–49. doi: 10.1016/j.annemergmed.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 33.Tierney K. CARRI Research Report 6. University of Colorado at Boulder; Disaster response: Research Findings and their implications for resilience measures. Available at: http://www.resilientus.org/library/Final_Tierney2_dpsbjs_1238179110.pdf. Accessed August 2, 2012. [Google Scholar]
- 34.Mulholland S, Gabbe B, Cameron P, et al. Is paramedic judgment useful in prehospital trauma triage? Injury. 2005;36(11):1298–1305. doi: 10.1016/j.injury.2005.07.010. 2005. [DOI] [PubMed] [Google Scholar]
- 35.Albright S. Simple Triage and Rapid Treatment: START. Available at www.scems.com/starttriage/StartTriage.pdf. Accessed 16 July 2012.
- 36.Gilboy N, Tanabe P, Travers D, et al. Emergency Severity Index, Version 4: Implementation Handbook. Agency for Health Care Research and Quality; Rockville, MD: 2011. AHRQ Publication No. 05-0046-2. [Google Scholar]
- 37.Eitel D, Travers D, Rosenau A, et al. The emergency severity index triage algorithm version 2 is reliable and valid. Acad Emerg Med. 2003;10(10):1070–1080. doi: 10.1111/j.1553-2712.2003.tb00577.x. [DOI] [PubMed] [Google Scholar]
- 38.Tanabe R, Travers D, Gilboy N, et al. Refining emergency severity index triage criteria. Acad Emerg Med. 2005;12(6):497–501. doi: 10.1197/j.aem.2004.12.015. [DOI] [PubMed] [Google Scholar]
- 39.Wuerz RC, Travers D, Gilboy N, Eitel DR, Rosenau A, Yazhari R. Implementation and refinement of the emergency severity index. Acad Emerg Med. 2001;8(2):170–176. doi: 10.1111/j.1553-2712.2001.tb01283.x. [DOI] [PubMed] [Google Scholar]
- 40.Gimbel T, Yarnold P, Adams J. The emergency severity index (version 3) 5-level triage system scores predict D resource consumption. J Emerg Nurse. 2004;30(1):22–29. doi: 10.1016/j.jen.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 41.Baumann M, Strout T. Evaluation of the emergency severity index (version 3) triage algorithm in pediatric patients. Acad Emerg Med. 2005;12(3):219–224. doi: 10.1197/j.aem.2004.09.023. [DOI] [PubMed] [Google Scholar]
- 42.SALT mass casualty triage: concept endorsed by the American College of Emergency Physicians. American College of Surgeons Committee on Trauma. American Trauma Society. National Association of EMS Physicians. National Disaster Life Support Education Consortium. State and Territorial Injury Prevention Directors Association SALT mass casualty triage. Disaster Med Public Health Prep. 2008;2(4):245–246. doi: 10.1097/DMP.0b013e31818d191e. 2008. [DOI] [PubMed] [Google Scholar]
- 43.Lee CH. Disaster and Mass Casualty Triage. Virtual Mentor. 2010;12(6):466–470. doi: 10.1001/virtualmentor.2010.12.6.cprl1-1006. [DOI] [PubMed] [Google Scholar]
- 44.Ginsberg JP, Holbrook JR, Chanda D, et al. Posttraumatic stress and tendency to panic in the aftermath of the chlorine gas disaster in Graniteville, South Carolina. Social psychiatry and psychiatric epidemiology. 2011 doi: 10.1007/s00127-011-0449-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ball LJ, Dworak J. Disaster in Graniteville. S C Nurse. 2005;12(2):1. [PubMed] [Google Scholar]