Abstract
Helicobacter pylori has been incriminated in human diseases, such as peptic ulcer, gastritis and gastric malignancy. Although modern triple-drug regimens are usually highly effective in the treatment of H. pylori infection, the emergence of resistance to two of the most used antibiotics, metronidazole (Mtz) and clarithromycin (Cla), is a serious and increasing problem. Truncations in the rdxA and frxA genes of H. pylori are thought to be associated with Mtz resistance whereas mutations in the pathogen’s 23S-ribosomal-RNA (23S-rRNA) genes are associated with Cla resistance. In a recent study, PCR and sequence analysis of the rdxA, frxA and 23S-rRNA genes were used to explore the genetic basis of resistance to Mtz and Cla in H. pylori. When 200 isolates of H. pylori from the Eastern Cape province of South Africa were tested for antibiotic susceptibility, almost all (95·5%) were found resistant to Mtz and 20·0% were found resistant to Cla. Only the Mtz-resistant isolates showed rdxA and frxA truncation. Two point mutations were detected in the 23S-rRNA genes of the Cla-resistant isolates. Many significant changes (resulting in 13 amino-acid substitutions in nine loci and truncated proteins in 14 loci) were observed in the rdxA genes of the Mtz-resistant isolates, and it appears that, compared with the rarer changes detected in frxA, such mutations may contribute more significantly to the high prevalence of Mtz resistance. To guide empiric treatment, the genotypes and antibiotic susceptibility of H. pylori in the Eastern Cape province of South Africa need to be monitored regularly.
Helicobacter pylori is a gastric pathogen that infects >50% of the world’s population, the major cause of several gastro–duodenal pathologies in infected patients (Tankovic et al., 2000; Cover and Blanke, 2005), and an early risk factor for gastric cancer (Matsuhisa et al., 2003). The large number of individuals infected, the tenacity of H. pylori infection and the associated morbidity make effective treatment regimens extremely important. Eradication of the organism usually leads to a feeling of general well-being among the treated patients (Sepulvedo and Coelho, 2002). The triple therapy that is generally recommended for eradicating H. pylori consists of a proton-pump inhibitor, clarithromycin (Cla) and either metronidazole (Mtz) or amoxicillin (Kalach et al., 2001). Unfortunately, H. pylori has acquired resistance to many classes of antibiotics (Kwon et al., 2001; Ahmad et al., 2009) and such resistance is now a primary cause of treatment failure, especially in Africa (Asrat et al., 2004; Ndip et al., 2008).
Although Mtz has been the cornerstone of many triple-drug regimens for the eradication of H. pylori, resistance to this drug can now be detected in 80%–90% of H. pylori isolates from many developing countries (Asrat et al., 2004; Ndip et al., 2008) and in 5%–50% of such isolates (depending on geographical region and patient group) from Western Europe (Alarcón et al., 1999; Ables et al., 2007). Such resistance clearly decreases the effectiveness of Mtz-containing anti-H. pylori therapies, which tend to be popular because they are relatively inexpensive (Kim et al., 2009).
If patients infected with Mtz-susceptible H. pylori are treated with the drug, reduction of the nitro moiety of the Mtz produces highly reactive compounds that cause DNA strand breakage, helix destabilization, helix unwinding and, ultimately, death of the bacterial cells (Kwon et al., 2001; Kim et al., 2009). Acquisition of Mtz resistance by H. pylori is highly associated with mutational inactivation of the bacterium’s rdxA gene, which encodes an oxygen-insensitive NADPH nitroreductase (Tankovic et al., 2000). Inactivation of frxA, which encodes NAD(P)H-flavin oxidoreductase, may also contribute to the Mtz-resistant phenotype, either alone or in association with rdxA (Jeong et al., 2000; Kwon et al., 2001; Llanes et al., 2010). Although gene sequencing has provided some support for the idea that frxA and/or rdxA play a role in resistance to Mtz, frameshift mutations in frxA have been found to occur with similar frequencies in Mtz-sensitive and -resistant isolates (Chisholm and Owen, 2004). According to Jeong et al. (2000), most Mtz resistance in H. pylori depends on rdxA inactivation (although mutations in frxA can enhance such resistance), and genes conferring Mtz resistance without rdxA inactivation are either rare or non-existent in H. pylori populations.
Clarithromycin resistance is also becoming increasingly prevalent in H. pylori (Lee et al., 2005). Most (>90%) of the macrolide resistance seen in H. pylori appears to be mediated by a transition (A→G) mutation at position 2142 or 2143 in one or both of the bacterium’s two 23S-rRNA genes (Matsuoka et al., 1999). Other mutations in these 23S-rRNA genes, such as A→C, A→T and G→T, have also been detected (Doorn et al., 2001; Kim et al., 2002).
About 50%–60% of the people living in South Africa are thought to be infected with H. pylori (Tanih et al., 2010a). In the country’s Eastern Cape province, the resistance of H. pylori to Mtz is a common problem (Tanih et al., 2010b). Resistance to Mtz and/or Cla is clinically significant because it increases the risk of treatment failure (Mégraud, 1997). The main aim of the present study was to employ PCR and sequence analysis of the genes that are believed to be involved in Mtz resistance (rdxA and frxA) and Cla resistance (the 23S-rRNA genes) to determine if specific mutations in these genes were responsible for the drug resistance seen in H. pylori isolates from Eastern Cape province. It was hoped that the results would improve prognosis and empiric treatment.
MATERIALS AND METHODS
Study Population and Ethics
The H. pylori isolates used in this study were isolated from patients from Eastern Cape province who were suffering from gastric-related morbidities and, when the isolates were collected, had no recorded history or memory of treatment with Cla or Mtz. After informed consent was obtained, gastric biopsies were collected by a resident gastro-enterologist.
The study protocol was approved by the institutional review board of the University of Fort Hare and the Eastern Cape Department of Health (protocol number EcDoH-Res 0002).
Bacteriology
Helicobacter pylori was isolated from the gastric biopsies by following standard microbiological procedures (Ndip et al., 2008). Briefly, biopsies were homogenized, under aseptic conditions, in sterile brain–heart-infusion (BHI) broth (Oxoid, Basingstoke, U.K.) supplemented with cysteine (0·2 g/litre) and glycerol (20%, v/v). A loopful of this homogenate was then plated on freshly prepared Columbia agar base (Oxoid) containing 7% (v/v) sheep’s blood (Oxoid) and Skirrow’s supplement (Oxoid; two vials/litre, giving 5 mg trimethoprim, 10 mg vancomycin, 5 mg cefsulodin and 5 mg amphotericin/litre). All plates were incubated at 37°C for 3–5 days under micro-aerophilic conditions (5%–6% O2, 10% CO2, 80%–85% N2) produced using the Anaerocult® P reagent (Merck, Darmstadt, Germany). Isolates were identified based on colony morphology and positive results in oxidase, urease and catalase tests. A reference strain of H. pylori (NCTC 11638) was included as a positive control. Isolates identified as H. pylori were suspended in 20% (v/v) glycerol and stored at −80°C, for use in future experiments.
Testing Antibiotic Susceptibility
Susceptibility testing was carried out by the disk-diffusion (Kirby–Bauer) technique (Tanih et al., 2010b), using disks (Mast Group, Bootle, U.K.) pre-dosed with Cla (15 µg) or Mtz (5 µg) on plates of BHI agar (Oxoid) containing 7% (v/v) horse blood and Helicobacter pylori selective supplement (Oxoid; two vials/litre). Reference strains of H. pylori (NCTC 11638 and J99) were included in all of the experiments.
Determination of Minimum Inhibitory Concentration (MIC)
The MIC of Mtz and Cla were determined, for each isolate, using the agar-dilution method (Osato, 2000). After incubation, the MIC value was read as the lowest concentration of the antibiotic that inhibited all visible bacterial growth. An isolate was considered Mtz-resistant if it had an MIC of >8 µg Mtz/ml and Cla-resistant if it had an MIC of >1·0 µg Cla/ml (Osato, 2000; Ndip et al., 2008).
Molecular Characterisation
DNA extraction
The QIAamp DNA kit (QIAGEN, Hilden, Germany) was used, according to the manufacturer’s recommendations, to extract the DNA from cell pellets produced from 14 of the test isolates found Mtz-resistant, three of the isolates found Mtz-susceptible and three of the test isolates found Cla-resistant. The extracted DNA was stored at −20°C until analysis.
PCR-based Amplification
PCR-based analysis of the targeted genes was performed using Thermo-stat Taq DNA polymerase (ABgene, Epsom, U.K.) and the reaction buffer provided by the enzyme’s manufacturer. Each 50-µl reaction mixture contained 5 µl DNA in 1×PCR buffer containing 3 mm MgCl2, 0·2 mm of each deoxynucleotide (Abgene), 62·5 U Thermo-stat Taq DNA polymerase and either 0·5 µm (rdxA and 23S-rRNA genes) or 0·2 µm (frxA) of each of the two relevant oligonucleotide primers (see Table 1). The thermal cycler (MJ Research, Waltham, MA) was set to give an initial denaturation of target DNA at 95°C for 15 min and then 35 cycles of denaturation at 94°C for 1 min, primer annealing at 56°C for 1 min and extension at 72°C for 1 min before a final extension step, at 72°C for 5 min. As a negative control (used in each PCR run), the template DNA was replaced with ultrapure water (Sigma–Aldrich, Gillingham, U.K.).
Table 1. The primers used for the PCR-based amplification of sequences from the rdxA, frxA and 23S-rRNA genes of Helicobacter pylori.
| Amplicon size | |||
| Gene | Primer sequences | (bp) | Reference |
| rdxA | 5′-GTTAGGGATTTTATTGTAATG-3′ | 427 | Kwon et al. (2001) |
| 3′-ACGCCAAGCATTTGAGCAAA-5′ | |||
| frxA | 5′-TCTCAAGCGGAAAAATCCGG-3′ | 445 | Kwon et al. (2001) |
| 3′-AATTTTTGATGATTTGAGCG-5′ | |||
| 23S-rRNA | 5′-ACGGCGGCCGTAACTATA-3′ | 307 | Wang et al. (2001) |
| 5′-ACAGGCCAGTTAGCTA-3′ |
The amplicons produced (5 µl) were separated by electrophoresis in 2% (w/v) high-resolution agarose gel, using Tris–acetate–EDTA buffer and staining with ethidium bromide (0·5 µg/ml). The bands were visualized under ultraviolet light and photographed.
mutational analysis
Mutations and genetic diversity in the genes of interest were explored by sequencing the PCR products. Each sample of amplified DNA (20 µl) was first cleaned by mixing with 2 µl shrimp alkaline phosphatase (Promega, Madison, WI) and 2 µl Exonuclease solution (Promega). This mixture was then incubated for 30 min at 37°C, 15 min for 72°C, and then 5 min at 8°C. Sequencing was carried out using version 3.1 of the Big Dye® Terminator DNA sequencing kit (Applied Biosystems, Carlsbad, CA) and a mixture of 2 µl chromosomal DNA, 0·25 µl primer (10 pmol/µl), 2 µl Big Dye buffer and 2 µl Big Dye. The thermal cycler used was set to give 30 cycles, each of denaturation at 96°C for 10 s, annealing at 50°C for 20 s, and extension at 60°C for 4 min. The cycling was followed first by dye-terminator removal, using the Agencourt® CleanSeq® system (Agencourt Bioscience, Beverly, MA), and then by sequencing on the ABI 3130xl automated sequencer (Applied Biosystems). The sequences were edited, aligned and analysed using BioEdit (www.mbio.ncsu.edu/bioedit/bioedit.html), Clustalw2 (www.ebi.ac.uk/Tools/msa/clustalw2/) and the DNAMAN software package (Lynnon, Pointe-Claire, Canada).
RESULTS
Patient Characteristics
Overall, 254 patients (90 males and 164 females) were enrolled in a larger study on H. pylori (Tanih et al., 2010c) of which this investigation forms part. Their mean (s.d.) age was 44·5 (15·7) years (range = 5–93 years). Most (83%) were older than 35 years.
Susceptibility Testing and MIC Determination
Of the 200 isolates of H. pylori (from the 254 patients) that were subjected to tests of antibiotic susceptibility, 95·5% were found Mtz-resistant and 20·0% Cla-resistant. The isolates showed MIC of 1–256 µg/ml for Mtz and 0·125–256 µg/ml for Cla.
PCR Amplification of 23S-rRNA, frxA and rdxA Genes
As expected, PCR based on the primers for the 23S-rRNA, frxA and rdxA produced amplicons of 307, 445 (Fig. 1) and 427 (Fig. 2) bp, respectively.
Figure 1.
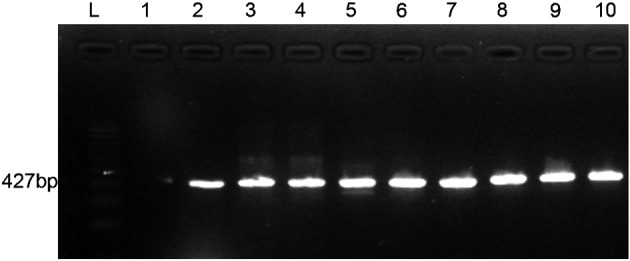
The results of the electrophoresis of the amplicons produced in PCR targeting the rdxA gene of Helicobacter pylori. The lanes contained a molecular-weight ‘ladder’ (L), the products from a negative-control reaction (lane 1) and samples produced from test isolates of H. pylori (lanes 2–10).
Figure 2.
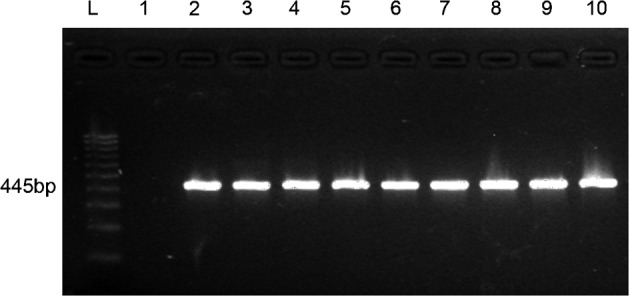
The results of the electrophoresis of the amplicons produced in PCR targeting the frxA gene of Helicobacter pylori. The lanes contained a molecular-weight ‘ladder’ (L), the products from a negative-control reaction (lane 1) and samples produced from test isolates of H. pylori (lanes 2–10).
Characterisation of rdxA and frxA Genes of the Mtz-sensitive and Mtz-resistant Isolates
rdxA
Although a Mtz-sensitive isolate (237C) exhibited a Glu(27)Val amino-acid substitution (i.e. a missense mutation) in its rdxA gene that was not seen in the Mtz-resistant isolates, the other two Mtz-susceptible isolates checked by sequencing (238A and 238C) remained unchanged for their rdxA genes (Table 1). Of the 14 Mtz-resistant isolates investigated by sequencing, two (279C and 305C) had missense mutations, nine (243A, 243C, 265C, 266A, 268C, 293A, 294A, 308A and 308C) showed a total of 13 amino-acid substitutions, and seven (243A, 243C, 266A, 268C, 279A, 293C and 296C) had nonsense mutations; 243A, 243CA, 266A and 268C therefore showed both nonsense mutations and amino-acid substitutions (Table 2). The changes seen in the Mtz-resistant isolates resulted in an rdxA protein truncated at position 16, 22, 27, 32, 56, 60, 71, 78, 97, 106, 111, 113, 115 or 121.
Table 2. Detection of mutations in the rdxA and frxA genes in 17 Helicobacter pylori isolates, only three of which (237C, 238A and 238C) were considered metronidazole-susceptible.
| Minimum inhibitory concentration of metronidazole | Changes in rdxA | Changes in frxA | |||
| Isolate | (µg/ml) | Nucleotide (nt) sequence | Amino-acid sequence | Nucleotide sequence | Amino-acid sequence |
| 237C | 1 | – | Glu(27)Val | Frameshift (nt deletion at position 54) | Val(44)Gly, Tyr(60)Phe |
| 238A | 8 | – | – | Frameshift (nt deletion at position 54) | Stop codon at position 39 |
| 238C | 1 | – | – | Frameshift (nt deletion at position 54) | Stop codon at position 39 |
| 243A | 256 | – | Leu(71)Phe, Gln(113)stop codon | Frameshift (nt deletion at position 54) | Stop codon at position 39 |
| 243C | 256 | – | Pro(106)Ser, Ser(111)Leu, Arg(16)stop codon | Frameshift (nt deletion at position 54) | Stop codon at position 84 |
| 265C | 256 | – | Arg(16)Cys, Met(56)Val | Frameshift (nt deletion at position 98) | Stop codon at position 39, His(6)Leu, Ser(7)Phe |
| 266A | 64 | – | Ser(111)Leu, Arg(56)stop codon | – | Stop codon at position 39, Thr (110)Ser, Glu(169)Lys |
| 268C | 256 | – | Arg(16)His, Thr(16)Ala, Glu(60)stop codon | Frameshift (nt deletion at position 54) | Thr(26)Glu |
| 279A | 128 | – | Leu(121)stop codon | Frameshift (nt deletion at position 54) | Stop codon at position 39 |
| 279C | 64 | Missense [deletion of three nt (80–82)] | – | Frameshift (nt deletion at position 54) | Stop codon at position 39 |
| 293A | 128 | – | Glu(27)Gln | Frameshift (nt deletion at position 54) | Glu(199)stop codon |
| 293C | 128 | – | Glu(60)stop codon | Frameshift (nt insertion at position 224) | Stop codon at position 72 |
| 294A | 256 | – | Val(32)Ala | Frameshift (nt deletion at position 54) | Stop codon at position 39 |
| 296C | 256 | – | Glu(78)stop codon | Frameshift (nt deletion at position 54) | Stop codon at position 39 |
| 305C | 64 | Missense [deletion of four nt (80–83)] | – | Frameshift (nt deletion at position 54) | Stop codon at position 72 |
| 308A | 64 | – | Asn(22)Ser | – | Ala(112)stop codon |
| 308C | 128 | – | His(97)Tyr, Arg(115)Ile | Frameshift (nt deletion at position 54) | Glu(120)Lys, Met(126)Phe, Thr(26)Glu |
frxA
In almost all of the isolates investigated by sequencing (including all of the three Mtz-susceptible isolates), the open reading frame for the frxA gene was disrupted by a deletion of a nucleotide at position 54 or 98 (Table 2). In one Mtz-resistant isolate (293C), such disruption was caused by a nucleotide insertion at position 224 (Table 2). These deletion/insertion events led to the occurrence of a stop codon at positions corresponding to amino acids 39, 72 or 84. Some point mutations were also observed, in five of the Mtz-resistant isolates (Table 2).
Detection of Mutation in the 23S-rRNA Gene, by Sequencing
Mutations of the 23S-rRNA genes of three isolates showing high levels of resistance to Cla (with MIC no higher than 256 µg/ml) were investigated by sequencing. All three of the isolates showed a mutation at position A2142G, and one also showed an A2143G mutation.
DISCUSSION
The present results add to the description of Mtz and Cla resistance and MIC values reported, for the same H. pylori isolates, by Tanih et al. (2010b). Resistance to Mtz is currently the most common type of resistance found in H. pylori and is, along with other types of antibiotic resistance, a major cause of elimination failure (Marais et al., 2003; Nahar et al., 2004; Tanih et al., 2010b). In South Africa, the high prevalence of resistance to Mtz in H. pylori might be due to the drug’s frequent use against intestinal parasites and in the treatment of gynaecological disorders; among patients attending the primary healthcare system in South Africa, Mtz is one of the most widely used antibiotics (Tanih et al., 2010b). Given that patients who admitted taking Mtz for their current gastric morbidity were excluded from the present study, it is unlikely (but not impossible) that any of the tested isolates came from patients who had failed Mtz treatment (i.e. patients who were particularly likely to be infected with Mtz-resistant H. pylori).
Mtz resistance in H. pylori has previously been associated with inactivation of rdxA and/or frxA (Jeong et al., 2000; Tankovic et al., 2000; Kwon et al., 2001). Both of these genes can be inactivated without leading to the death of the pathogen (Kwon et al., 2001) and mutations in them appear to be quite common, allowing the selection of resistance during the clinical use of Mtz (Kwon et al., 2001; Jeong et al., 2000; Tanih et al., 2010b). The Glu(27)Val mutation detected, in the present study, in a Mtz-susceptible isolate, was not observed in any of the Mtz-resistant isolates and therefore cannot be required for resistance to occur. Some of the mutations detected in the rdxA genes of the Mtz-resistant isolates that were investigated, by sequencing, in the present study — Arg(115)Ile, Arg(16)His, Ser(111)Leu and Arg(16)Cys — have also been described previously (Kwon et al., 2001; Wang et al., 2001; Yang et al., 2004). The other mutations detected, either in the rdxA genes [Thr(16)Ala, Glu(27)Gln, Val(32)Ala, Asn(22)Ser, His(97)Tyr, Met(56)Val, Ser(111)Leu, Leu(71)Phe, Pro(106)Ser, Gln(113)stop codon, Arg(16)stop codon, Arg(56)stop codon, Glu(60)stop codon, Leu(121)stop codon, and Glu(78)stop codon] or frxA genes [Val(44)Gly, Tyr(60)Phe, His(6)Leu, Ser(7)Phe, Thr (110)Ser, Glu(169)Lys, Thr(26)Glu, Glu(120)Lys, Met(126)Phe, Thr(26)Glu, Ala(112)stop codon, and Glu(199)stop codon] of the Mtz-resistant isolates have not been previously described in the literature. The phenotypic changes resulting from any of these mutations may include antibiotic resistance (Jeong et al., 2000).
It has been suggested that inactivation of frxA cannot cause Mtz resistance in the absence of mutations in rdxA (Kwon et al., 2001; Yang et al., 2004). In the present study, however, not only did some of the Mtz-resistant isolates have no mutations in their frxA genes but also the mutations seen in the frxA genes of many of the Mtz-resistant isolates were identical to those seen in the Mtz-susceptible isolates (Table 2). It therefore seems unlikely that the detected frxA mutations contributed to the observed Mtz resistance. The present results are in accordance with the notion that Mtz susceptibility is dependent on the level of nitroreductase activity produced by rdxA (Kwon et al., 2001).
Resistance to Cla can considerably reduce the success of the standard triple therapies used against H. pylori infection, as Cla is generally used in such treatments (Duck et al., 2004; Ahmad et al., 2009). The prevalence of Cla resistance among H. pylori isolates has been found to vary from 1% to 29%, the value depending on the location of the study site and tending to increase with the amount the drug is used locally, many respiratory-tract infections being treated with the drug (Kato et al., 2002). The resistance of H. pylori to Cla has been associated with an adenosine-to-guanosine (A-to-G) substitution within the peptidyltransferase-encoding region of the pathogen’s 23S-rRNA genes (Versalovic et al., 1996). Mégraud (2004) stated that most Cla-resistant isolates of H. pylori show the A2142G mutation seen in the present study and/or the A2143C mutation, although, previously, Kim et al. (2002) had described A2143G as the mutation that was most frequently detected in Cla-resistant H. pylori. In the present study, A2142G appeared more common than A2143G but only three Cla-resistant isolates were investigated for mutations in their 23S-rRNA genes. The A2142G mutation detected, in the present study, in all three Cla-resistant isolates might be responsible for the high level of Cla resistance seen in H. pylori from the present study area (Tanih et al., 2010b). Both of the 23S-rRNA mutations detected in the present study (A2142G and A2143G) have, however, already been associated with resistance to Cla (Versalovic et al., 1996; Matsuoka et al., 1999; Mégraud, 2004; Ahmad et al., 2009).
It is hoped that the present results help guide clinicians in the study area to choose effective (Mtz-free) regimens for the treatment of H. pylori infection.
Acknowledgments
This study received financial support from the South African National Research Foundation (via grant UID 69816) and the Govan Mbeki Research and Development Centre at the University of Fort Hare. The authors are also grateful to the staff of the Gastro-intestinal-tract Unit, Livingston Hospital, Port Elizabeth, and B. Clarke, for their technical assistance.
REFERENCES
- Ables AZ, Simon I, Melton ER.(2007)Update on Helicobacter pylori treatment. American Family Physician 75351–358. [PubMed] [Google Scholar]
- Ahmad N, Zakaria WR, Abdullah SA, Mohamed R.(2009)Characterisation of clarithromycin resistance in Malaysian isolates of Helicobacter pylori. World Journal of Gastroenterology 153161–3165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alarcón T, Domingo D, López-Brea M.(1999)Antibiotic resistance problems with Helicobacter pylori. International Journal of Antimicrobial Agents 1219–26. [DOI] [PubMed] [Google Scholar]
- Asrat D, Kassa E, Mengistu Y, Nilsson I, Wadstrom T.(2004)Antimicrobial susceptibility pattern of Helicobacter pylori strains isolated from adult dyspeptic patients in Tikur Ambassa University Hospital, Addis Ababa. Ethiopian Medical Journal 4279–85. [PubMed] [Google Scholar]
- Chisholm SA, Owen RJ.(2004)Frameshift mutations in frxA occur frequently and do not provide a reliable marker for metronidazole resistance in UK isolates of Helicobacter pylori. Journal of Medical Microbiology 53135–140. [DOI] [PubMed] [Google Scholar]
- Cover TL, Blanke SR.(2005)Helicobacter pylori vacA, a paradigm for toxin multifunctionality. Nature Reviews. Microbiology 3320–332. [DOI] [PubMed] [Google Scholar]
- Doorn LJ, Glupczynski Y, Kusters JG, Mégraud F, Midolo P, Maggi-Solcà N, Queiroz DMM, Nouhan N, Stet E, Quint WGV.(2001)Accurate prediction of macrolide resistance in Helicobacter pylori by a PCR line probe assay for detection of mutations in the 23S rRNA gene: multicenter validation study. Antimicrobial Agents and Chemotherapy 451500–1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duck WM, Sobel J, Pruckler JM, Song Q, Swerdlow D, Friedman C, Sulka A, Swaminathan B, Taylor T, Hoekstra M, Griffin P, Smoot D, Peek R, Metz DC, Bloom PB, Goldschmidt S, Parsonnet J, Triadafilopoulos G, Perez-Perez GI, Vakil N, Ernst P, Czinn S, Dunne D, Gold BD.(2004)Antimicrobial resistance, incidence and risk factors among Helicobacter pylori infected persons, United States. Emerging Infectious Diseases 101088–1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeong JY, Mukhopadhyay AK, Dailidiene D, Wang Y, Velapatiño B, Gilman RH, Parkinson AJ, Nair GB, Wong BC, Lam SK, Mistry R, Segal I, Yuan Y, Gao H, Alarcon T, Brea ML, Ito Y, Kersulyte D, Lee HK, Gong Y, Goodwin A, Hoffman PS, Berg DE.(2000)Sequential inactivation of rdxA (HP0954) and frxA (HP0642) nitroreductase genes causes moderate and high-level metronidazole resistance in Helicobacter pylori. Journal of Bacteriology 1825082–5090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalach N, Benhamou PH, Campeotto F, Bergeret M, Doupont C, Raymond J.(2001)Clarithromycin resistance and eradication of Helicobacter pylori in children. Antimicrobial Agents and Chemotherapy 452134–2135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kato S, Fujimura S, Udagawa H, Shimizu T, Maisawa S, Ozawa K, Linuma K.(2002)Antibiotic resistance of Helicobacter pylori strains in Japanese children. Journal of Clinical Microbiology 40649–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim KS, Kang JO, Eun CS, Han DS, Chi TY.(2002)Mutations in the 23S rRNA gene of Helicobacter pylori associated with clarithromycin resistance. Journal of Korean Medical Science 17599–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SY, Young MJ, Hak SL, Chung IS, Yoo JY, Merrell DS, Cha JS.(2009)Genetic analysis of Helicobacter pylori clinical isolates suggest resistance to metronidazole can occur without the loss of functional rdxA. Journal of Antibiotics 6443–50. [DOI] [PubMed] [Google Scholar]
- Kwon DH, Hulten K, Kato M, Kim JJ, Lee M, El-Zaatari FAK, Osato MS, Graham DY.(2001)DNA sequence analysis of rdxA and frxA from 12 pairs of metronidazole-sensitive and -resistant clinical Helicobacter pylori isolates. Antimicrobial Agents and Chemotherapy 452609–2615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JH, Shin J.-H, Roe IH, Sohn SG, Lee JH, Kang GH, Lee H.-K, Jeong BC, Lee SH.(2005)Impact of clarithromycin resistance on eradication of Helicobacter pylori in infected patients. Antimicrobial Agents and Chemotherapy 491600–1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llanes R, Soria C, Nagashima S, Kobayashi N, Gala A, Guzmán D, Feliciano O, Valdés L, Gutiérrez O, Fernández H, Llop A, Wada A.(2010)Phenotypic and genetic characterization of antimicrobial profiles of Helicobacter pylori strains in Cuba. Journal of Health, Population and Nutrition 28124–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marais A, Bilardi C, Cantet F, Mendz GL, Mégraud F.(2003)Characterisation of the genes rdxA and frxA involved in metronidazole resistance in Helicobacter pylori. Research in Microbiology 154137–144. [DOI] [PubMed] [Google Scholar]
- Matsuhisa TM, Yamada NY, Kato SK, Matsukura NM.(2003)Helicobacter pylori infection, mucosal atrophy and intestinal metaplasia in Asian populations: a comparative study in age-, gender- and endoscopic diagnosis-matched subjects. Helicobacter 829–35. [DOI] [PubMed] [Google Scholar]
- Matsuoka M, Yoshida Y, Hayakawa K, Fukuchi S, Sugano K.(1999)Simultaneous colonisation of Helicobacter pylori with and without mutations in the 23SrRNA gene in patients with no history of clarithromycin exposure. Gut 45503–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mégraud F.(1997)Resistance of Helicobacter pylori to antibiotics. Alimentary Pharmacology and Therapeutics 11(Suppl. 1)43–53. [DOI] [PubMed] [Google Scholar]
- Mégraud F.(2004)Helicobacter pylori antibiotic resistance: prevalence, importance, and advances in testing. Gut 531374–1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahar S, Mukhopadhyay AK, Khan R, Ahmad MM, Datta S, Chattopadhyay S, Dhar SC, Sarker SA, Engstrand L, Berg DE, Nair GB, Rahman M.(2004)Antimicrobial susceptibility of Helicobacter pylori strains isolated in Bangladesh. Journal of Clinical Microbiology 424856–4859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ndip RN, Malange Takang AE, Ojongokpoko AEJ, Luma HN, Malongue A, Akoachere KTJ.-F, Ndip LM, MacMillan M, Weaver TL.(2008)Helicobacter pylori isolates recovered from gastric biopsies of patients with gastro–duodenal pathologies in Cameroon: current status of antibiogram. Tropical Medicine and International Health 13848–854. [DOI] [PubMed] [Google Scholar]
- Osato MS.(2000)Antimicrobial susceptibility testing for Helicobacter pylori: sensitivity test results and their clinical relevance. Current Pharmaceutical Design 61545–1555. [DOI] [PubMed] [Google Scholar]
- Sepulvedo AR, Coelho LGV.(2002)Helicobacter pylori and gastric malignancies. Helicobacter 737–42. [DOI] [PubMed] [Google Scholar]
- Tanih NF, McMillan M, Naidoo N, Ndip LM, Weaver LT, Ndip RN.(2010a) Prevalence of Helicobacter pylori vacA, cagA and iceA genotypes in South African patients with upper gastrointestinal diseases. Acta Tropica 11668–73. [DOI] [PubMed] [Google Scholar]
- Tanih NF, Okeleye BI, Green E, Mkwetshana N, Clarke AM, Ndip LM, Ndip RN.(2010b)Marked susceptibility of South African Helicobacter pylori strains to ciprofloxacin and amoxicillin: clinical implications. South African Medical Journal 10049–52. [PubMed] [Google Scholar]
- Tanih NF, Okeleye BI, Ndip LM, Clarke AM, Naidoo N, Mkwetshana N, Green E, Ndip RN.(2010c)Helicobacter pylori prevalence in dyspeptic patients in the Eastern Cape Province of South Africa: race and disease status. South African Medical Journal 100734–737. [DOI] [PubMed] [Google Scholar]
- Tankovic J, Lamarque D, Delchier JC, Soussy CJ, Labigne A, Jenks PJ.(2000)Frequent association between alteration of the rdxA gene and metronidazole resistance in French and North African isolates of Helicobacter pylori. Antimicrobial Agents and Chemotherapy 44608–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Versalovic J, Shortridge D, Kibler K, Griffy MV, Beyer J, Flamm RK, Tanaka SK, Graham DY, Go MF.(1996)Mutations in 23S rRNA are associated with clarithromycin resistance in Helicobacter pylori. Antimicrobial Agents and Chemotherapy 40477–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang G, Wilson TJM, Jiang Q, Taylor DE.(2001)Spontaneous mutations that confer antibiotic resistance in Helicobacter pylori. Antimicrobial Agents and Chemotherapy 45727–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang YJ, Wu JJ, Sheu BS, Kao AW, Huang AH.(2004)The rdxA gene plays a more major role than frxA gene mutation in high-level metronidazole resistance of Helicobacter pylori in Taiwan. Helicobacter 9400–407. [DOI] [PubMed] [Google Scholar]


