Abstract
In Iran, Leishmania major or L. tropica cause almost all of the human cutaneous leishmaniasis (CL). Unfortunately, the detection methods frequently used for CL (the microscopical examination of direct smears or the culture of biopsies) are not very sensitive and the Leishmania species causing each case of CL in Iran is usually only tentatively identified from extrinsic factors, such as the case’s clinical manifestations and region of residence. Recently, however, a nested PCR that targets the parasites’ kinetoplast DNA has been used in the city of Ahvaz (the capital of the province of Khouzestan, in south–western Iran) to confirm the microscopical diagnosis of CL and to identify the causative parasites, to species level. Smears from the lesions on 100 suspected cases of CL were fixed, stained with Wright’s eosin–methylene blue, and checked for amastigotes under a light microscope. Scrapings from the same smears were then tested for leishmanial DNA, using a nested PCR that allows the DNA from L. tropica to be identified and distinguished from that of L. major. The 100 smears investigated were all found amastigote-positive by microscopy and PCR-positive for either L. major DNA (97 smears) or L. tropica DNA (three smears). The predominant species causing CL in Ahvaz is therefore L. major.
The various forms of human leishmaniasis are an important public-health problem in many tropical and subtropical countries (WHO, 1990; Razmjou et al., 2009). The cutaneous form of the disease has a wide spectrum of clinical manifestations, depending on the causative species (WHO, 1990; Dowlati, 1996). Although such cutaneous leishmaniasis (CL) rarely causes severe morbidity, the lesions may take several months to heal and often leave ugly scars on the face or other exposed areas of skin. At least two species of Old World Leishmania are responsible for the CL seen in Iran, which usually presents as self-healing ulcerative lesions but occasionally takes on a metastatic form (Javadian et al., 1976; Nadim et al., 1977; Motazedian et al., 2006). Atypical, mucosal infections with leishmanial parasites have also been observed in Iran, albeit rarely (Yaghoobi, 2001).
Both zoonotic cutaneous leishmaniasis (ZCL) caused by Leishmania major and anthroponotic cutaneous leishmaniasis (ACL) caused by L. tropica occur in Iran, ZCL being endemic in rural areas in the centre, north–east, south–west and south–east of the country and ACL being largely confined to some large and medium-sized cities (Nadim et al., 1994). In the subtropical province of Khouzestan, which lies in south–western Iran and shares a border with Iraq, the annual incidence of CL has risen worryingly over the last decade, with major outbreaks of the disease in 2003 and 2004 and an increase in the percentage of CL cases attributed to L. major (Maraghi et al., 2007).
In areas where two or more species of CL-causing Leishmania co-occur, the accurate identification of the parasite(s) causing each case of CL is necessary if the local measures for the control of the disease are to be effective (Grimaldi and Tesh, 1993). The detection methods frequently used for CL (i.e. the microscopical examination of direct smears and/or the culture of biopsies) are not very sensitive and the Leishmania species causing each case of CL in Iran is usually only tentatively identified from extrinsic factors, such as the case’s clinical manifestations and region of residence. Diagnostic methods based on deoxyribonucleic acid (DNA) have, however, now made the sensitive and rapid detection and identification of many microorganisms possible. Over the last couple of decades, for example, assays based on PCR have proved to be sensitive and powerful tools for the detection and identification of Leishmania in clinical samples, without the need to culture the parasites (Rodgers et al., 1990; Smyth et al., 1992; Lopez et al., 1993; Noyes et al., 1998). In the present study, based in Ahvaz (the capital city of Khouzestan), a nested PCR was used to confirm the microscopical diagnosis of CL and identify the causative parasites to species level.
PATIENTS AND METHODS
Study Area
The city of Ahvaz (31°19′39″N, 48°41′38″E; Fig. 1) lies at a mean elevation of 20 m above sea level and has long, hot summers and short, mild winters. Summer temperatures often exceed 50°C.
Figure 1.
Map of Iran, showing the locations of Khouzestan province and the city of Ahvaz.
Preparation of Slit Smears
Slit biopsies were collected, with a sterile vaccinostyle, from the edge of a cutaneous lesion on each of 100 suspected cases of CL who presented, consecutively, in Ahvaz in 2003–2004. Each biopsy was spread on a glass slide, allowed to dry, fixed in methanol, stained with Wright’s eosin–methylene blue (Merck, Darmstadt, Germany) and checked for amastigotes, under oil immersion at ×1000, by light microscopy. For each suspected case of CL, the case’s age and gender, the time between the lesion being first noticed and presentation at a health facility, the number of skin lesions and the location of each lesion, on the patient’s body, were recorded.
DNA Extraction
After the microscopy, the immersion oil on each smear was gently wiped off with xylol on a paper tissue. The entire smear was then scraped off the slide, with a sterile scalpel, so that the total DNA in the smear could be extracted by digestion, in a 1·5-ml microcentrifuge tube, with 200 μl lysis buffer [50 mM Tris-HCl (pH 7·6), 1 mM EDTA, 1% (v/v) Tween 20] containing 8·5 μl of a proteinase-K solution that had 19 mg enzyme/ml (Yokota et al., 1995; Motazedian et al., 2002). The tube was incubated overnight, at 37°C, before 200 μl phenol/chloroform/isoamyl alcohol (25∶24∶1, by vol.) were added to it. The tube was then shaken vigorously and centrifuged at 6000×g for 10 min. The resultant supernatant solution was transferred to another tube and mixed with 400 μl absolute ethanol. The DNA that precipitated was centrifuged down (at 6000×g for 20 min), dried, dissolved in 50 μl ultrapure water [produced in a Purelab® UHQ system (Siemens Water Technologies, Warrendale, PA)], and stored at 4°C (Motazedian et al., 2002) before use in the PCR-based assay.
Nested-PCR-based Assay
The variable segments on minicircles of kinetoplast DNA from any Leishmania parasites present in the smear scraping were amplified with two rounds of nested PCR (Noyes et al., 1998). The primers were CSB1XR (ATT TTT CGC GAT TTT CGC AGA ACG) and CSB2XF (CGA GTA GCA GAA ACT CCC GTT CA) for the first round, and LiR (TCG CAG AAC GCC CCT) and 13Z (ACT GGG GGT TGG TGT AAA ATAG) for the second. Each 25-μl, first-round reaction mixture contained 5 μl template DNA, 200 μm of each deoxynucleoside triphosphate (Roche, Penzberg, Germany), 1·5 mm MgCl2, 1·0 U Taq polymerase, 50 mm Tris-HCl (pH 7·6), 10 μm CSB1XR and 10 μm CSB2XF. The thermocycler used (MyCycler; Bio-Rad, Hercules, CA) was set to give 5 min at 94°C, followed by 30 cycles, each of 30 s at 94°C, 1 min at 55°C and 1·5 min at 72°C, and then a final extension for 5 min at 72°C. The product of this first round of PCR was diluted 1∶9 with ultrapure water and then 1 μl of this dilution was used as the template for the second round of PCR, which used the same conditions and reaction mixture as the first round except that LiR and 13Z were used as the primers. A 5-μl sample of the second-round product was subjected to electrophoresis in 1·5% (w/w) agarose gel, stained with ethidium bromide and visualized by ultraviolet trans-illumination (Moemenbellah–Fard et al., 2003). The size of each amplicon detected was estimated by comparison with a 100-bp–1500-bp molecular-weight ‘ladder’ (Roche) run on the same gel.
As positive controls, DNA extracted from promastigote cultures of reference strains of L. major(MHOM/IR/54/LV39) and L. tropica (MHOM/IR/89/ARA2) was run on each gel (Pourmohammadi et al., 2008). These strains, which were routinely maintained on Novy–MacNeal–Nicolle medium, were transferred to Roswell Park Memorial Institute medium 1640 (Invitrogen, Carlsbad, CA) enriched with 20% (v/v) foetal calf serum (Invitrogen) prior to the extraction of their DNA. Negative controls (the products of PCR in which ultrapure water replaced the template DNA) were also run.
RESULTS
All 100 smears investigated were found positive for amastigotes by microscopy and positive for leishmanial DNA in the nested PCR. Three (3%) of the smears gave the 750-bp second-round amplicon indicative of L. tropica and the rest (97%) gave the 560-bp product indicative of L. major (Fig. 2). No other sizes of second-round amplicon were seen, no sample gave more than one amplicon (indicating a mixed infection), and no amplicons were detected in the negative-control samples.
Figure 2.
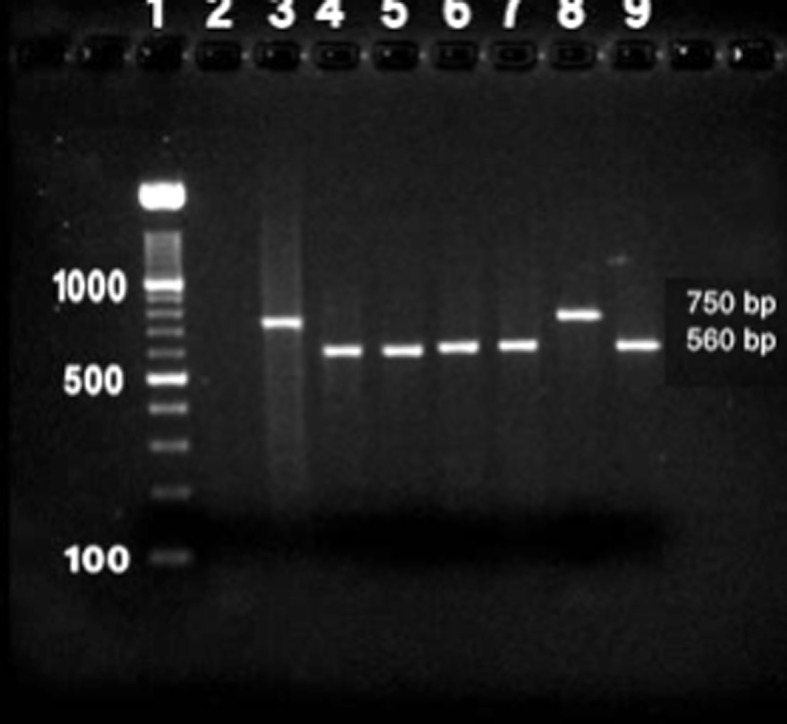
The results of the electrophoresis of the products of the nested-PCR-based amplification of DNA extracted from the stained smears. The nine lanes contained a molecular-weight ‘ladder’ (lane 1), a negative control (lane 2) and the products from reference strains of Leishmania tropica (lane 3) and L. major (lane 4) and test samples identified as L. tropica (lane 8) or L. major (lanes 5, 6, 7 and 9).
Most (57) of the suspected cases of CL investigated were aged <21 years but the number of male cases was similar to the number of female cases (see Table). The time between the appearance of the lesion and presentation was 1–3 months for the 97 cases infected with L. major but >3 months for the three cases infected with L. tropica. Although most of the lesions caused by L. major were seen on the hand, whereas those caused by L. tropica were equally likely to occur on the face, neck and hands, this difference did not reach statistical significance. The number of lesions/case tended to be greater with L. major than with L. tropica, the greatest number of lesions seen on a case (14) occurring on a patient infected with L. major. In the present study, although (as expected) ‘wet’ lesions were mainly attributed to L. major and ‘dry’ lesions to L. tropica (Fig. 3), dry lesions were seen in 15 of the 97 patients found PCR-positive for L. major DNA while one of the three cases found PCR-positive for L. tropica DNA had a wet lesion.
The numbers of male and female cases of cutaneous leishmaniasis who were investigated, split by age-group.
| Age | No. of cases: | ||
| (years) | Male | Female | Investigated |
| <10 | 18 | 13 | 31 |
| 11–20 | 9 | 17 | 26 |
| 21–30 | 6 | 9 | 15 |
| 31–40 | 4 | 11 | 15 |
| >40 | 5 | 8 | 13 |
Figure 3.
The lesions of cutaneous leishmaniasis seen on two patients from Ahvaz, in south–western Iran, who were found to be infected with Leishmania tropica (a) or L. major (b).
DISCUSSION
With the incidence of the disease in the city increasing over the last decade, many local clinicians now consider CL to be the most important public-health problem in Ahvaz (unpubl. obs.). Identifying the Leishmania species that is responsible for each case of CL or, at least, for the vast majority of cases (if any species predominates) can be important for effective treatment and the design of an appropriate and effective programme for the control of the disease (WHO, 1990). Lesions caused by L. major, for example, should not be treated with antimonal compounds except in severe cases (Markle and Makhoul, 2004). Until now, the Leishmania parasites causing CL in Iran (and in many other areas where the disease is endemic) — which, whether in their promastigote or amastigote forms, are morphologically quite similar — have only been tentatively identified to species level, on the basis of extrinsic factors such as clinical manifestations and the existing (and often outdated) knowledge of the geographical distributions of each Leishmania species. Although such factors may improve the accuracy of any parasite identification, they are insufficient for the definitive identification of the causative agents of CL.
Various molecular, immunological and biochemical methods have been developed to identify and characterise Leishmania species (Pourmohammadi et al., 2010). Currently, the most commonly used methods involve iso-enzyme electrophoresis, monoclonal antibodies, specific DNA probes or PCR with or without RAPD analysis (Jaffe and McMahon–Pratt, 1983; Rioux et al., 1990). Several PCR-based assays have been developed to detect and identify leishmanial parasites (Barker, 1989; De Bruijin and Barker, 1992; Piarroux et al., 1994; Osman et al., 1997; Noyes et al., 1998; Fakhar et al., 2008). The results of the present study were encouragingly clear-cut; every test sample produced a single amplicon (that matched, in size, the single amplicon produced from the reference strains of L. major or L. tropica) and the absence of amplicons from the negative-control samples indicated the absence of contamination that could have given false-positive results.
In the present study, curiously, patients infected with L. major presented more quickly (after their lesion appeared) than the patients infected with L. tropica. Although Maraghi et al. (2007) made the same observation in another study in Khouzestan, the reasons behind this difference remain unclear.
It appears that, in 2003–2004, L. major was the cause of almost all the CL in Ahvaz with L. tropica-attributable disease present but relatively rare. Although L. major and the ZCL that it causes are generally considered rural, it appears that the citizens of Ahvaz are much more likely to be infected with L. major than with (the usually more urban) L. tropica, perhaps because the local development of a sugar-cane industry and irrigation systems and the outward spread of the city’s human populations have increasingly brought the city’s residents into the habitats of the local vectors and reservoir hosts of L. major (Javadian et al., 1998). Maraghi et al. (2007) made similar observations in the city of Shoush, which lies, in Khouzestan, to the north–west of Ahvaz. It appears that the epidemiological pattern of CL in several endemic areas of Iran has changed in recent years, with L. major becoming the predominant causative agent of CL in urban areas as many cities expand into rural areas where the colonies of the rodents that act as reservoir hosts in ZCL are found (Davami et al., 2010).
In conclusion, the CL found in Ahvaz is now predominantly ZCL. The PCR-based assay used in the present study appears to be a suitable and powerful tool for the characterisation of at least two Leishmania species and the confirmation of CL.
Acknowledgments
The authors would like to express their thanks to Drs R. Yaghoubi, M. Radmanesh and Z. Omidian and several other dermatologists who referred patients to the Iran-Zamin Laboratory of the Leishmania Research Centre in Ahvaz. They also express their gratitude to Dr B. Sarkari and M. Karamian, for advice and help with this article, and to K. Shashok (of AuthorAID in the Eastern Mediterranean) for improving the English in the manuscript.
REFERENCES
- Barker DC.(1989)Molecular approaches to DNA diagnosis. Parasitology 99125–146. [DOI] [PubMed] [Google Scholar]
- Davami MH, Motazedian MH, Sarkari B.(2010)The changing profile of cutaneous leishmaniasis in a focus of the disease in Jahrom district, southern Iran. Annals of Tropical Medicine and Parasitology 104377–382. [DOI] [PubMed] [Google Scholar]
- De Bruijn MH, Barker DC.(1992)Diagnosis of New World leishmaniasis: specific detection of species of the Leishmania braziliensis complex by amplification of kinetoplast DNA. Acta Tropica 5245–58. [DOI] [PubMed] [Google Scholar]
- Dowlati Y.(1996)Cutaneous leishmaniasis: clinical aspect. Clinics in Dermatology 14425–431. [DOI] [PubMed] [Google Scholar]
- Fakhar M, Motazedian MH, Hatam GR, Asgari Q, Kalantari M, Mohebali M.(2008)Asymptomatic human carriers of Leishmania infantum possible reservoirs for Mediterranean visceral leishmaniasis in southern Iran. Annals of Tropical Medicine and Parasitology 102577–583. [DOI] [PubMed] [Google Scholar]
- Grimaldi G, Jr, Tesh RB.(1993)Leishmaniasis of the New World: current concepts and implications for future research. Clinical Microbiology Reviews 6230–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffe CL, McMahon-Pratt D.(1983)Monoclonal antibodies specific for Leishmania tropica. I. Characterization of antigens associated with stage- and species-specific determinants. Journal of Immunology 1311987–1993. [PubMed] [Google Scholar]
- Javadian E, Nadim A, Tahvildar-Bidruni G, Assefi V.(1976)Epidemiology of cutaneous leishmaniasis in Iran: B. Khorassan. Bulletin de la Société de Pathologie Exotique 69140–143. [PubMed] [Google Scholar]
- Javadian E, Dehestani M, Nadim A, Rassi Y, Tahvildar-Bidruni CH, Seyedi-Rashti MA, Shadmehr A.(1998)Confirmation of Tatera indica (Rodentia: Gerbillidea) as the main reservoir host of zoonotic cutaneous leishmaniasis in the west of Iran. Iranian Journal of Public Health 2755–60. [Google Scholar]
- Lopez M, Inga R, Cangalaya M, Echevarria J, Lianoscuentas A.(1993)Diagnosis of Leishmania using the polymerase chain reaction: a simplified procedure for fieldwork. American Journal of Tropical Medicine and Hygiene 49348–356. [DOI] [PubMed] [Google Scholar]
- Maraghi S, Samarbaf Zadeh A, Sarlak AA, Ghasemian M, Vazirianzadeh B.(2007)Identification of cutaneous leishmaniasis agents by nested polymerase chain reaction (nested-PCR) in Shush city, Khuzestan province, Iran. Iranian Journal of Parasitology 213–15. [Google Scholar]
- Markle WH, Makhoul K.(2004)Cutaneous leishmaniasis: recognition and treatment. American Family Physician 691455–1460. [PubMed] [Google Scholar]
- Moemenbellah-Fard MD, Kalantari M, Rassi Y, Javadian E.(2003)The PCR-based detection of Leishmania major infections in Meriones libycus (Rodentia: Muridae) from southern Iran. Annals of Tropical Medicine and Parasitology 97811–816. [DOI] [PubMed] [Google Scholar]
- Motazedian H, Karamian M, Noyes HA, Ardehali S.(2002)DNA extraction and amplification of Leishmania from archived, Giemsa-stained slides, for the diagnosis of cutaneous leishmaniasis by PCR. Annals of Tropical Medicine and Parasitology 9631–34. [DOI] [PubMed] [Google Scholar]
- Motazedian MH, Mehrabani D, Oryan A, Asgari Q, Karamian M, Kalantari M.(2006)Life cycle of cutaneous leishmaniasis in Larestan, southern Iran. Infectious Diseases and Tropical Medicine Research Center 1137–143. [Google Scholar]
- Nadim A, Mesghali A, Javadian E.(1977)Cutaneous leishmaniasis in southern Iran. In Ecologies des Leishmanioses (Colloques Internationaux No. 239)pp.215–218.Paris: Centre National de la Recherche Scientifique [Google Scholar]
- Nadim A, Javadian E, Seyedi-Rashti MA.(1994)Epidemiology of leishmaniasis in Iran. In Leishmania Parasites and LeishmaniasesedsArdehaliRezaiNadim S H R A.ed pp.178–180.Tehran: Iran University Press [Google Scholar]
- Noyes HA, Reyburn H, Bailey JW, Smith D.(1998)A nested PCR-based schizodeme method for identifying Leishmania kinetoplast minicircle classes directly from clinical samples and its application to the study of the epidemiology of Leishmania tropica in Pakistan. Journal of Clinical Microbiology 362877–2881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osman OF, Oskam L, Zijlstra ED, Kroon CM, Schoone GJ, Khalil G, Elsan AM, Kager PA.(1997)Evolution of PCR for diagnosis of visceral leishmaniasis. Journal of Clinical Microbiology 352454–2457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piarroux R, Gambarelli F, Umon H, Fontes M, Dunan S, Mary C, Toga B, Quilici M.(1994)Comparison of PCR with direct examination of bone marrow aspiration, myeloculture, and serology for diagnosis of visceral leishmaniasis in immunocompromised patients. Journal of Clinical Microbiology 32746–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pourmohammadi B, Motazedian MH, Kalantari M.(2008)Rodent infection with Leishmania in a new focus of human cutaneous leishmaniasis, in northern Iran. Annals of Tropical Medicine and Parasitology 102127–133. [DOI] [PubMed] [Google Scholar]
- Pourmohammadi B, Motazedian MH, Hatam GR, Kalantari M, Habibi P, Sarkari B.(2010)Comparison of three methods for diagnosis of cutaneous leishmaniasis. Iranian Journal of Parasitology 51–8. [PMC free article] [PubMed] [Google Scholar]
- Razmjou S, Hejazy H, Motazedian MH, Baghaei M, Emamy M, Kalantari M.(2009)A new focus of zoonotic cutaneous leishmaniasis in Shiraz, Iran. Transactions of the Royal Society of Tropical Medicine and Hygiene 103727–730. [DOI] [PubMed] [Google Scholar]
- Rioux JA, Lanotte G, Serres E, Pratlong F, Bastien P, Perieres J.(1990)Taxonomy of Leishmania. Use of isoenzymes. Suggestions for a new classification. Annales de Parasitologie Humaine et Comparée 65111–125. [DOI] [PubMed] [Google Scholar]
- Rodgers MR, Popper SJ, Wirth DF.(1990)Amplification of kinetoplast DNA as a tool in the detection and diagnosis of Leishmania. Experimental Parasitology 71267–275. [DOI] [PubMed] [Google Scholar]
- Smyth AJ, Ghoshm A, Hassanm MQ, Basu D, de Bruijn MH, Adhya S, Mallik KK, Barker DC.(1992)Rapid and sensitive detection of Leishmania kinetoplast DNA from spleen and blood samples of kala-azar patients. Parasitology 105183–192. [DOI] [PubMed] [Google Scholar]
- World Health Organization(1990)Control of the Leishmaniases: Report of a WHO Expert Committee. Technical Report Series No. 793Geneva: WHO; [PubMed] [Google Scholar]
- Yaghoobi MR.(2001)Mucosal leishmaniasis: report of three cases. Archives of Iranian Medicine 4138–140. [Google Scholar]
- Yokota M, Tatsumi M, Tsuda I, Yano L.(1995)DNA extraction and amplification from Giemsa-stained blood smears. Journal of Clinical Laboratory Analysis 9387. [DOI] [PubMed] [Google Scholar]




