Abstract
Background:
It was observed that a good number of patients presenting with psychiatric manifestations when investigated later because of unresponsiveness to treatment or late development of organic features turned out to be treatable limbic syndromes.
Introduction:
The aim of this study is to assess the patients presenting with new onset neuropsychiatric symptoms satisfying the criteria for probable limbic encephalitis.
Patients and Methods:
Patients referred to neurology department following a period of treatment for neuropsychiatric symptoms, which did not respond to conventional treatment were analyzed using Electroencephalography (EEG), magnetic resonance imaging, cerebrospinal fluid, screening for malignancy Vasculitic work-up, histopathology and autoantibody done when feasible.
Results:
There were 22 patients satisfying criteria for probable limbic encephalitis. Their mean age was 34.5 years. Symptoms varied from unexplained anxiety, panic and depression, lack of inhibition, wandering, incontinence, myoclonus, seizures and stroke like episodes. Three had systemic malignancy, 10 had chronic infection, one each with vasculitis, acute disseminated encephalomyelitis, Hashimoto encephalitis and two each with non-convulsive status, cryptogenic and Idiopathic inflammation.
Conclusion:
All patients who present with new onset neuropsychiatric symptoms need to be evaluated for sub-acute infections, inflammation, autoimmune limbic encephalitis and paraneoplastic syndrome. A repeated 20 minute EEG is a very effective screening tool to detect organicity.
Keywords: Chronic infection, limbic encephalitis, neuropsychology, paraneoplastic limbic encephalitis
Introduction
Limbic system comprises the thalamus, hypothalamus, amygdale, and hippocampus. These areas are mainly concerned with emotions, memory, personality appetite, social and sexual behavior. When inflammation occurs in these regions patients present with a sub-acute onset syndrome of confusion, psychiatric symptoms, seizures, memory problems, apathy, panic, autistic and schizophreniform features, myoclonus etc. It can present with multifaceted and atypical initial features resulting in diagnostic difficulties and there is no clear consensus as to the definitions and diagnosis. The clinical phenotype varies from new onset non-familial psychiatric syndrome to fatal neurological conditions such as Creutzfeldt-Jakob disease (CJD) and Sub-Acute Sclerosing Panencephalitis (SSPE). A high degree of suspicion is essential as early diagnosis is highly rewarding with reference to the outcome. Clinical criteria for limbic encephalitis include; Age at onset >25 years, and at least one of the following; a) features suggestive of temporal lobe epilepsy. b) Short term memory loss c) exclusion of viral infections, tumors and infarcts. It is considered to be definite if clinical features are corroborated by evidence of the limbic brain inflammation or onco neuronal antibodies such as Hu, Ma2, Cv2, CRMPS, Amphiphysin or tumor detected anywhere else. It is considered as possible if the clinical criteria is satisfied and laboratory data not available.[1,2]
Limbic encephalopathy can result due to infective, auto-immune or cryptogenic causes. Infections may be herpetic or non-herpetic and autoimmune may be non-paraneoplastic or paraneoplastic. The antibodies commonly seen are directed against classic paraneoplastic intracellular antigens including Hu, Ma2, Cv2/CRMP5, Amphiphysin or cell membrane antigens such as voltage gated potassium channels (VGKC), N-Methyl D-Aspartate receptor (NMDAR), glutamic acid dehydrogenase, AMPAR, GABABR and others expressed in the neuropil of the hippocampus and cerebellum.[3,4] N-Methyl D-Aspartate (NMDA) encephalitis, due to NMDAR autoantibodies, occurs in ovarian teratoma. NMDA encephalitis causes schizophrenia-like psychiatric symptoms, impaired consciousness, seizures and extrapyramidal symptoms and can be fatal.[7,8] GABA-B encephalitis also occurs with underlying neoplasms and causes brainstem symptoms such as dysphagia, dysarthria, facial palsy, nausea, vomiting, cerebellar ataxia and respiratory failure.[9]
Anti-VGKC encephalitis causes hyponatremia, impaired learning, memory and seizures.[1] Antibodies previously attributed to potassium channels are actually against 3 proteins complexed with these channels namely (1) contactin-associated protein 2 (Caspr2) that is present in myelinated axons; (2) leucine rich, glioma inactivated 1 (LGI1) protein that is strongly expressed in the hippocampus and neocortex and (3) tag-1/contactin-2 that is associated with Caspr2.[10,11,13,15,16] This explains the occurrence of different clinical features with these different antibodies. LGI1 associated LE is the most common non-paraneoplastic limbic encephalitis (PLE), while Caspr2 antibody has a risk of underlying neoplasm and has a poor prognosis.[15]
Good numbers of patients are treated with electroconvulsive therapy (ECT) as pharmacoresistant psychosis, resulting in no benefit. Hence, we decided to analyze consecutive patients from 1st January 2010 to 1st January 2011 in a prospective way.
Patients and Methods
Consecutive patients who were referred to the Neurology Department of our center with a new onset psychopharmaco-resistant limbic syndrome with or without seizures and seen from 1st January 2010 to 1st January 2011 were analyzed. A consultant neurologist and a resident assessed the history and clinical features and patients who were having psychiatric illness and definite herpes simplex encephalitis (HSV) encephalitis were not included. All of them underwent routine magnetic resonance imaging with 1.5 Tesla, 20 min Electroencephalography (EEG), few cases underwent video telemetric EEG, Neuropsychological assessment and cerebrospinal fluid (CSF) analysis for known viral and bacterial infections, malignant cells and culture for tuberculosis, Fungus and Cryptococcus were done. Neuropsychological tests included Hindi Mental Status Examination, NIMHANS battery consisting of Digit symbol substitution test, Motor speed by finger tapping, category fluency by animal naming, Attention and working memory by color trails 1 and 2 planning by Tower of London, set shifting by Wisconsin card sorting technique, response inhibition by Stroop test, verbal learning and memory by Auditory Verbal learning test, Visuospatial involvement and visual learning and memory by complex figure of Rey test as well as specific tests for focal signs to rule out apraxia, agnosia and aphasias. The obtained values were compared with normative data.[2]
Screening for malignancy was done whenever felt indicated with clinical assessment, X-ray chest, ultrasound scan-abdomen and endoscopy. Onco-neural antibodies, autoantibody profile, and antibody for autoimmune encephalitis and whole body positron emission tomography (PET) were done in few patients who could afford. Histopathological evaluation of brain tissue was done in one case.
Results
Distribution
Out of 78 patients screened 22 were satisfying the criteria for possible limbic encephalitis and at the time of recruitment definite features of known infections of the brain causing limbic syndromes were not there. There were 10 females and 12 males. Their age group varied from 25 to 54 years with the mean age of 34.5 years with majority (>50%) belonging to an age group of 30-40 years [Figure 1].
Figure 1.
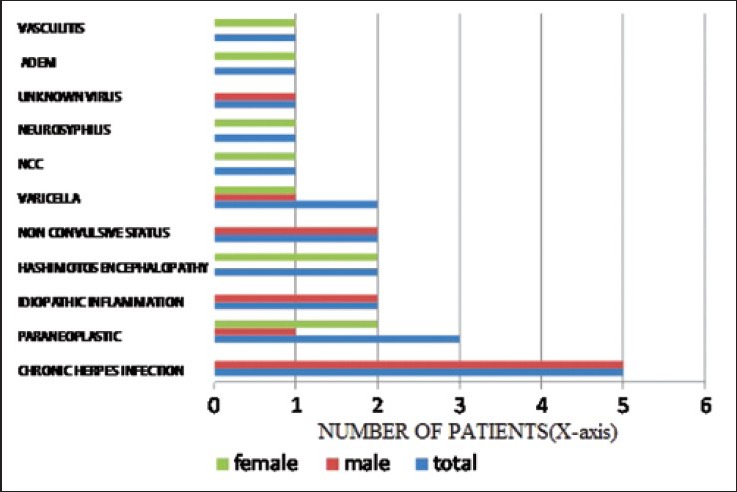
Demographic details
The commonest symptom was unexplained anxiety found in 86.3% (males-10 and females-9) followed by unexplained panic seen in 44.6% (males-2 and females-8), uninhibited behavior-9.8% (both females), social incontinence 9.8% (both females), depression in 13.3% (Females-2 and males-1), psychotic features in 4.8% (2 females) and unexplained paroxysmal symptoms of vague sensations on the right side with transient speech arrest in 4.8% (male-1). Wandering tendency is seen in 4.8% (1 female), myoclonic jerks in 33.66% (females-3 and males-5), seizures in 50% (females-4 and males-7) and stroke like episodes in 13.6% (females-1 and males-2). Examination revealed papilledema in one female (vasculitis), Optic atrophy in one female (neurosyphilis), mild hemiparesis-in one male (paraneoplastic) and in one male (cytomegalovirus [CMV] infection), hemiparesis in one female (Vasculitis). On examination of the other systems the following asymptomatic signs were detected; Mass in the breast in one patient with computed tomography (CT) scan showing Paraneoplastic limbic encephalitis (PLE): Axial Contrast enhanced CT image revealed heterogeneous hypodensity in the left medial temporal lobe (arrow) with patchy enhancement. There is edema producing mass effect in the form of effacement of left temporal horn and narrowing of adjacent supra-sellar cistern [Figure 2a]. Left supraclavicular node enlargement in one and splenomegaly in one patient. Modified Rankin score on admission was Grade zero to two and four in none, Grade three in seven and Grade five in thirteen. At 6 months follow-up, the scores changed as follows; Grade zero in none, Grade one in three (2 Hashimottos and 1 vasculitis), Grade two in four (acute disseminated encephalomyelitis/neurosyphilis/non convulsive status), Grade three in five (HSV-3/nonherpetic non neoplastic-2), Grade four in two (HSV), Grade five in four patients (Varicella 2/NCC1/unknown etiology-1) and death occurred in four patients-(Ca-breast/adenocarcinoma/lymphoma/CMV meningoencephalitis).
Figure 2.
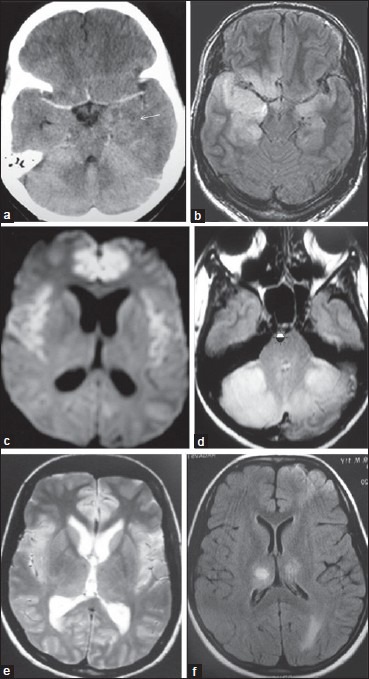
(a) Computed tomography — hypo density in the left medial temporal lobe-paraneoplastic. (b) FLAIR hyper intensity both hippocampi, parahippocampi, adjacent anterior temporal lobes-Herpes simplex. (c) Autoimmune limbic encephalitis: Axial DWI reveals (d) bilateral symmetrical foci of diffusion restriction involving cingulate, medial superior frontal gyriand Insula. (e) Case of varicella encephalitis: Axial T2WI shows abnormal bilaterally symmetrical hyperintensities involving cingulate (arrow), insula and thalami. (f) Axial FLAIR imageshyperintensities involving bilateral thalami, cingulate and anterior frontal lobes
After detailed assessment, 14 patients satisfied criteria for probable limbic encephalitis and 8 patients were atypical psychiatric illness in the form of new onset symptoms without a family history, rapid deterioration and resistant to psychiatric treatment.
Laboratory assessment
Cerebrospinal fluid analysis was performed in all patients, which showed the following; Cells were increased in nine patients with majority lymphocytes, Proteins were elevated in eight patients (68-100 mg), HSV PCR positive in five patients, CMV antibodies (IgM and IgG) positive in one patient, VDRL positive in one patient and cysticercal antibody positive in one patient respectively.
Blood parameters showed the following; raised ESR in five patients (range: 20-50), Varicella antibody seen in two patients and Vasculitis work-up was negative in all cases.
Histopathological assessment of the left supraclavicular node showed adenocarcinomatous deposit in one patient. Carcinoma breast was confirmed in one patient. There was a bone marrow evidence of Lymphoreticular malignancy in one patient and meningocortical biopsy showed-lymphocytic meningitis, cortical microglial nodules and perivascular inflammation predominantly of T cell (CD3) type [Figure 3] consistent with viral meningoencephalitis. No viral inclusions were detectable. Serum CMV IGM and IgG antibodies were positive.
Figure 3.
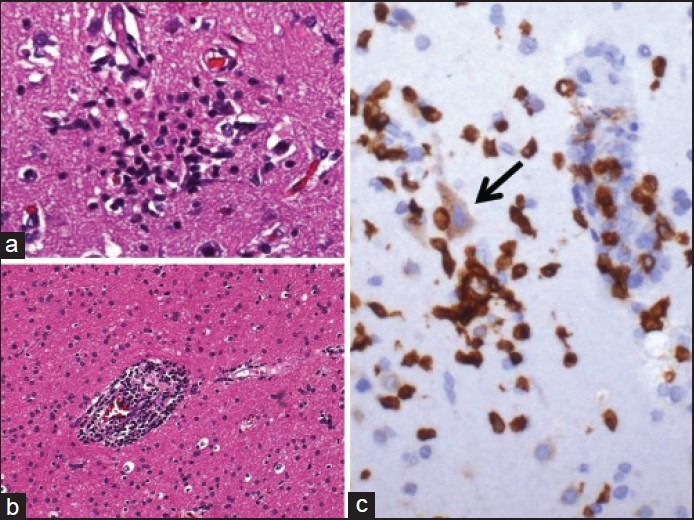
Pathology viral meningoencephalitis. (a) Microglial nodule in the grey matter marking a focus of neuronophagia. (b) White matter with perivascular inflammation. (c) CD3 immunostaining shows mainly T lymphocytes in the microglial nodule with neuronophagia (arrow)
EEG showed an abnormality in the maximum number of patients: 95.5%. Periodic Lateralized Epileptiform Discharges were seen 18.5%. Diffuse epileptiform discharges were seen in 18.5% suggestive of probable non-convulsive status. Midpositive triphasic waves were seen in 13.6% [Figure 4] and nonspecific abnormality in the form of excessive Theta and multifocal sharp waves were seen in 45.45% of patients.
Figure 4.
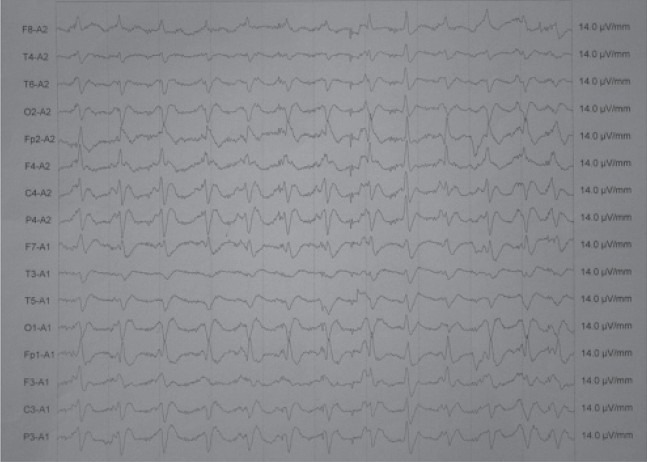
Electroencephalography-EEG shows mid positive triphasic waves
Imaging abnormalities were as follows; Medial temporal, cingulated gyrus and amygdala signal changes were seen in six cases (HSV-5 and CMV-1), cerebellum showed signal changes in two patients (Varicella). Frontal lobe and Corpus callosum showed signal changes in one patient (Hashimotos encephalopathy), Infarcts and micro bleeds were seen in one patient. Bilatateral Thalamic change was seen in one case, white matter signal changes were seen in 11 cases (50%) [Figure 1]. Neurocysticercosis was seen in one case and meningeal changes seen in one case.
Autoimmune encephalitis affects symmetrical regions in the brain as it is caused by anti-neuronal auto antibodies targeted against the various components of the nervous system that attack similar targets bilaterally. Axial CT image reveals heterogeneous hypodensity in the left medial temporal lobe (arrow) with patchy enhancement and edema producing mass effect in the form of effacement of left temporal horn and narrowing of adjacent supra-sellar cistern [Figure 1a].
Anteromedial temporal lobes (hippocampi, parahippocampi and amygdala) are often earliest to be affected and are best seen on Fluid Attenuation Inversion Recovery(FLAIR) sequences, which suppress free water (CSF) [Figure 2b]. Posterior orbito-frontal lobes and insular cortex are also frequently involved.[5] Diffusion weighted images might depict diffusion restriction and is helpful along with FLAIR sequence [Figure 2c]. Contrast enhancement can occur rarely in the acute phase. The affected areas undergo atrophy in the following months. Other areas that can be affected include cerebral cortex, thalamus, hypothalamus, basal ganglia, brainstem, cerebellum and spinal cord [Figure 2d]. Bilateral posterior thalamic hyper intensities (pulvinar sign) similar to CJD have also been described in PLE (in a case of lymphoma).[6,17] [Figure 2e]. Axial FLAIR images reveal hyper intensities involving bilateral thalami, cingulate and anterior frontal lobes. Periventricular white matter hyperintensities are visualized in bilateral occipital lobes suggestive of demyelination [Figure 2f].
Signal changes on FLAIR occur in 80% of cases and fluorodeoxyglucose-PET is more sensitive. PLE is often caused by small cell lung cancer and testicular germ cell tumors and rarely by lymphoma, thymoma, breast, esophageal, bladder and renal cancers. It develops when the antibodies produced cross react with self-antigens of the nervous system. PLE is a diagnosis of exclusion.
Neuropsychology on admission showed the following; Hindi mental status score was less than 10 in all cases. The areas of deficits were in attention, calculation, naming and construction. The complete neuropsychological battery could not be carried out in any of the patients on admission. At 6 months follow-up, HMSE scores had improved to more than 20 in all cases. Areas of deficits were in attention and memory. NIMHANS battery showed defects in color trails 2, Digit Symbol Substitution, Tower of London and Wisconsin's Card sorting test suggesting defective planning and set shifting. We had four mortalities involving the patient with adenocarcinoma secondary deposits, lymphoreticular malignancy and CMV encephalitis and carcinoma breast within 1 year of follow-up.
Treatment and follow-up
All patients were on antipsychotics at the time of assessment by the neurologist. Duration of illness at the time of presentation to the neurologist varied from 3 months to 9 months. Six patients had received repeated ECT. When organicity was suspected based on EEG abnormality and the features described above, all patients were started on Acyclovir 500 mg eight hourly, which was discontinued when the results of HSV titers and Varicella titers were reported negative and alternative diagnosis became available and those who showed positivity received the complete course. Patients with malignancy were referred for the treatment of the malignancy in addition to symptomatic measures for neurological symptoms. Those who turned out to be cryptogenic limbic encephalitis received pulse methyl prednisolone monthly for a minimum period of 6 months. The patient who showed CMV encephalitis was put on Gancyclovir and steroids as per recommendations. Patients received anti-convulsants and anti-psychotics when required. The minimum period of follow-up is 6 months and maximum period is 2½ years.
Discussion
This study reveals that subgroup of patients who present with sub-acute progressive behavioral symptoms, which are refractory to treatment are suffering from atypical presentation of organic brain syndrome. Organicity is detected quite late after patients have received even treatment like ECT, which is potentially harmful in the inflamed brain. Neuropsychiatric symptoms precede the overt manifestations of organicity making early diagnosis difficult. Symptoms beyond limbic system suggests Paraneoplastic involvement and antibody negativity does not exclude the diagnosis.[3,5] It was observed that EEG was a very sensitive predictor of organicity being abnormal in more than 95% of the cases. Sub-acute presentation of a behavioral syndrome without the classical features of infection seem to occur in good number of patients with herpes encephalitis, varicella encephalitis and CMV virus encephalitis and high degree of suspicion is essential as they are potentially treatable.[4,5,6,7] Herpetic limbic encephalitis is reported in patients with post-transplant state and those who have undergone stem cell therapy.[10,11] One patient was found to be suffering from syphilitic meningoencephalitis and responded well to treatment.[10,11] The Patient who had adenocarcinomatous deposits presented with vague recurrent symptoms on the right side with no abnormality detected on examination or in any of the investigations except EEG and lymph node biopsy.[10,11,12] The only clinical clue was transient speech arrest noticed during these episodes. The cryptogenic limbic encephalitis included the patients where we could not complete the autoantibody work-up for financial reasons. However, the responses to treatment in these patients were very good even when initiated late. Radiological changes vary from normal to extensive changes in the limbic structures. Diffusion weighted images have superior sensitivity compared to conventional imaging except the patients with malignancy associated limbic syndrome all other patients have shown very good response to treatment as evidenced by modified Rankin scale and neuropsychological assessment at 6 months.[6,8,12] When in doubt EEG is a cheap and superior screening instrument. Limbic encephalitis is an under recognized entity and a high degree of suspicion is needed as a good number of them may be seronegative to known antibodies.
Acknowledgments
The authors would like to thank NIMHANS institute for utilizing the facilities.[18]
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.Tüzün E, Dalmau J. Limbic encephalitis and variants: Classification, diagnosis and treatment. Neurologist. 2007;13:261–71. doi: 10.1097/NRL.0b013e31813e34a5. [DOI] [PubMed] [Google Scholar]
- 2.Rao SL, Subbakrishna DK, Gopukumar K. 1st ed. Bangalore: Published by National Institute of Mental Health and Neurosciences; 2004. NIMHANS Neuropsychology Battery-2004, Manual. [Google Scholar]
- 3.Correll CM. Antibodies in epilepsy. Curr Neurol Neurosci Rep. 2013;13:348. doi: 10.1007/s11910-013-0348-1. [DOI] [PubMed] [Google Scholar]
- 4.Gultekin SH, Rosenfeld MR, Voltz R, Eichen J, Posner JB, Dalmau J. Paraneoplastic limbic encephalitis: Neurological symptoms, immunological findings and tumour association in 50 patients. Brain. 2000;123:1481–94. doi: 10.1093/brain/123.7.1481. [DOI] [PubMed] [Google Scholar]
- 5.Grisold W, Giometto B, Vitaliani R, Oberndorfer S. Current approaches to the treatment of paraneoplastic encephalitis. Ther Adv Neurol Disord. 2011;4:237–48. doi: 10.1177/1756285611405395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thuerl C, Müller K, Laubenberger J, Volk B, Langer M. MR imaging of autopsy-proved paraneoplastic limbic encephalitis in non-Hodgkin lymphoma. AJNR Am J Neuroradiol. 2003;24:507–11. [PMC free article] [PubMed] [Google Scholar]
- 7.Suzuki S, Seki M, Suzuki N. Recent concept of limbic encephalitis: Progress in anti-NMDA receptor encephalitis. Nihon Rinsho Meneki Gakkai Kaishi. 2013;36:86–94. doi: 10.2177/jsci.36.86. [DOI] [PubMed] [Google Scholar]
- 8.Steiner J, Walter M, Glanz W, Sarnyai Z, Bernstein HG, Vielhaber S, et al. Increased prevalence of diverse N-methyl-D-aspartate glutamate receptor antibodies in patients with an initial diagnosis of schizophrenia: Specific relevance of IgG NR1a antibodies for distinction from N-methyl-D-aspartate glutamate receptor encephalitis. JAMA Psychiatry. 2013;70:271–8. doi: 10.1001/2013.jamapsychiatry.86. [DOI] [PubMed] [Google Scholar]
- 9.Mundiyanapurath S, Jarius S, Probst C, Stöcker W, Wildemann B, Bösel J. GABA-B-receptor antibodies in paraneoplastic brainstem encephalitis. J Neuroimmunol. 2013;259:88–91. doi: 10.1016/j.jneuroim.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 10.Tyler KL. Emerging viral infections of the central nervous system: Part 1. Arch Neurol. 2009;66:939–48. doi: 10.1001/archneurol.2009.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Isaacson E, Glaser CA, Forghani B, Amad Z, Wallace M, Armstrong RW, et al. Evidence of human herpesvirus 6 infection in 4 immunocompetent patients with encephalitis. Clin Infect Dis. 2005;40:890–3. doi: 10.1086/427944. [DOI] [PubMed] [Google Scholar]
- 12.Tunkel AR, Glaser CA, Bloch KC, Sejvar JJ, Marra CM, Roos KL, et al. The management of encephalitis: Clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2008;47:303–27. doi: 10.1086/589747. [DOI] [PubMed] [Google Scholar]
- 13.Derouich I, Messouak O, Belahsen MF. Syphilitic limbic encephalitis revealed by status epilepticus. BMJ Case Rep 2013. 2013 doi: 10.1136/bcr-2012-008073. pii:bcr2012008073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jeong YM, Hwang HY, Kim HS. MRI of neurosyphilis presenting as mesiotemporal abnormalities: A case report. Korean J Radiol. 2009;10:310–2. doi: 10.3348/kjr.2009.10.3.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ramos-Rivas M, Rojas-Velasco G, Acuña-Hidalgo R, Márquez-Valero OA, Arellano-Bernal RH, Castro-Martínez E. Paraneoplastic limbic encephalitis: A difficult-to-diagnose condition. Rev Neurol. 2009;48:311–6. [PubMed] [Google Scholar]
- 16.Kiroğlu Y, Calli C, Yunten N, Kitis O, Kocaman A, Karabulut N, et al. Diffusion-weighted MR imaging of viral encephalitis. Neuroradiology. 2006;48:875–80. doi: 10.1007/s00234-006-0143-7. [DOI] [PubMed] [Google Scholar]
- 17.Mihara M, Sugase S, Konaka K, Sugai F, Sato T, Yamamoto Y, et al. The “pulvinar sign” in a case of paraneoplastic limbic encephalitis associated with non-Hodgkin's lymphoma. J Neurol Neurosurg Psychiatry. 2005;76:882–4. doi: 10.1136/jnnp.2004.049783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grisold W, Giometto B, Vitaliani R, Oberndorfer S. Current approaches to the treatment of paraneoplastic encephalitis. Ther Adv Neurol Disord. 2011;4:237–48. doi: 10.1177/1756285611405395. [DOI] [PMC free article] [PubMed] [Google Scholar]


