Abstract
Phage amplification detected by MALDI-TOF MS was investigated for rapid and simultaneous Burkholderia pseudomallei identification and ceftazidime resistance determination. B. pseudomallei ceftazidime susceptible and resistant ΔpurM mutant strains Bp82 and Bp82.3 were infected with broadly targeting B. pseudomallei phage ϕX216 and production of the m/z 37.6 kDa phage capsid protein observed by MALDI-TOF MS over the course of 3 h infections. This allowed for repoducible phage-based bacterial ID within 2 h of the onset of infection. MALDI-TOF MS-measured time to detection correlated with in silico modeling, which predicted an approximate 2 h detection time. Ceftazidime susceptible strain Bp82, while detectable in the absence of the drug, owing to the reliance of phage amplification on a viable host, was not detectable when 10 μg/mL ceftazidime was added at the onset of infection. In contrast, resistant strain Bp82.3 was detected in the same 2 h timeframe both with and without the addition of ceftazidime.
Keywords: phage amplification, bacterial identification, antibiotic resistance, Burkholderia, MALDI-TOF MS
Introduction
Burkholderia pseudomallei is an aerobic, saprophytic Gram-negative bacillus endemic to Southeast Asia and northern Australia but is increasingly found in other parts of the world.1,2 It is the etiologic agent of melioidosis, a debilitating disease of humans and animals, with a mortality rate of 20–50% in endemic regions.1-4 Disease manifestations range widely from acute localized septic infection to severe pneumonia, neurologic impairment, and disseminated septicemia to asymptomatic disease.2,4 The Centers for Disease Control and Prevention has categorized B. pseudomallei as a Tier 1 select agent. Melioidosis is difficult to treat due to acquired and intrinsic antibiotic resistance.5-7 Because of this, a protracted regimen consisting of a 10 to 14 d intensive phase of intravenous ceftazidime followed by a three-month eradication phase of oral co-trimoxazole is the current recommendation for treatment of melioidosis.5,6,8 Several recent reports from around the world suggest that although still rare, the number of ceftazidime resistant B. pseudomallei infections may be on the rise.9-13
The increasing occurrence of antibiotic resistant infections has led to the need for more rapid methods of bacterial identification and antibiotic resistance determination in order to provide efficacious therapy. Culturing and disk diffusion assays are presently the standard for identification (ID) and antimicrobial susceptibility testing, but these methods are laborious and time-consuming, taking upwards of 72 h to complete.5,6 Furthermore, some ceftazidime resistant clinical isolates grow poorly on standard media and thus take even longer to culture and identify.10 MALDI-TOF MS has proven useful for bacterial detection and ID and is widely accepted in a growing number of clinical and industrial laboratories.14-16 Two commercially available MALDI-TOF MS protein profiling instruments, the Bruker Microflex Biotyper and Biomérieux VITEK MS, have been approved by the U.S. Food and Drug Administration (FDA) for clinical bacterial ID. However, while promising with regards to bacterial ID and relatively rapid testing times in the 24–48 h range, these units currently do not provide antibiotic resistance profiling capabilities. There are limited recent reports on the use of the Biotyper in combination with secondary methods for antibiotic resistance determination. Bruker has described a culture-based hydrolysis assay (Bruker Biotyper Spectrum Beta Lactamase) for Gram-negative β-lactam resistance determination17,18 and is experimenting with the use of stable isotope labeling of target strains prior to Biotyper analysis for differentiation of methicillin resistant Staphylococcus aureus.19 In contrast, in this report we demonstrate the application of phage amplification-based MALDI-TOF MS as a single method for simultaneous bacterial ID and antibiotic resistance determination. Phages have been used for decades for bacterial identification20-24 and methods for combining phage amplification with the capabilities of MALDI-TOF MS have been reported for sensitive bacterial detection in the 1 to 4 h range.25,26 In this report we extend the utility of MALDI-TOF MS by demonstrating its use not only for Burkholderia ID, but also for simultaneous antibiotic resistance determination using the previously described broadly infective B. pseudomallei phage ϕX216.27
Results and Discussion
MALDI-TOF MS detection of phage amplification as a means of B. pseudomallei ID
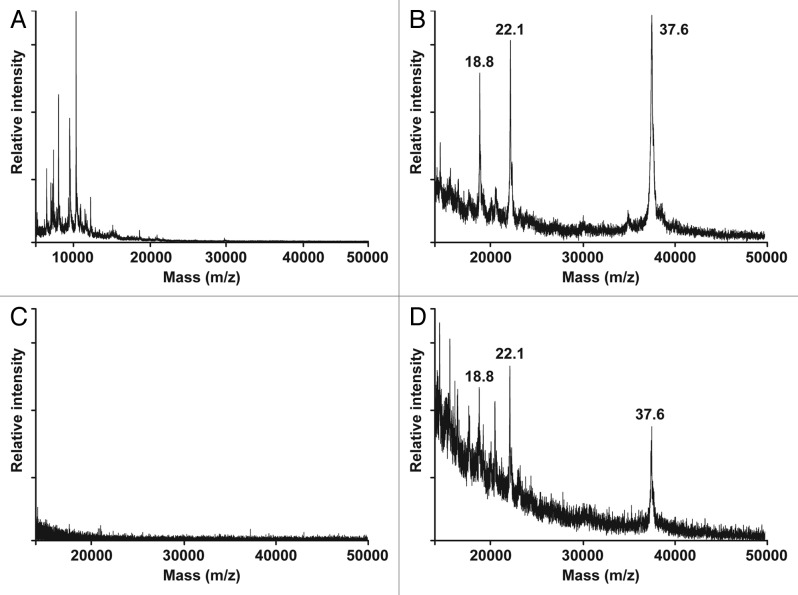
MALDI-TOF MS analyses of B. pseudomallei (Fig. 1A) resulted in spectra displaying a myriad of small bacterial proteins in a mass range from 5 to 50 kDa. In comparison, the ϕX216 spectrum shown in Figure 1B contained only 3 peaks: a 37.6 kDa peak corresponding to the phage major capsid protein, its doubly charged ion at 18.8 kDa, and the phage tail protein at 22.1 kDa. These masses were in agreement with our previously published report describing the isolation, characterization, genome sequencing and annotation of ϕX216.27 The MALDI-TOF MS ϕX216 limit of detection was determined to be 2.6 × 107 pfu/mL. Based on this data, all subsequent phage amplification reactions were initiated with concentrations below this value in order to only detect phage proteins resulting from amplification (rather than those from input phage used to initiate infection). Spectra were taken at the onset of ϕX216 infection of B. pseudomallei Bp82 at bacterial and phage concentrations below the MALDI-TOF MS limit of detection (3.2 × 105 cfu/mL, and 1.6 × 105 pfu/mL, respectively). Immediately following infection, as anticipated, no discernable signal was observed for either analyte (Fig. 1C). As shown in Figure 1D, once phage amplification proceeded and ϕX216 virions were released during cell lysis, a peak at 37.6 kDa was observed within 2 h that served as a secondary biomarker for the presence of B. pseudomallei. Results were similar for identical experiments conducted with B. pseudomallei Bp82.3 (not shown).
Figure 1. MALDI-TOF MS spectra of (A) B. pseudomallei Bp82, (B) phage ϕX216, (C) at onset of ϕX216 infection, and (D) 2 h post infection. Masses are indicated in kDa.
Determination of ϕX216 burst size
One-step growth curves (Fig. 2) showed that ϕX216 had an approximate burst size of 160 pfu per infected cell in B. pseudomallei Bp82 and a burst time of 150 min. Results were identical with B. pseudomallei Bp82.3 (not shown). This burst is slightly higher than the previously reported value of 120 pfu per infected cell.27 However, burst size was previously determined using B. mallei ATCC23344 as a host, which may explain the slight differences in observed burst sizes.
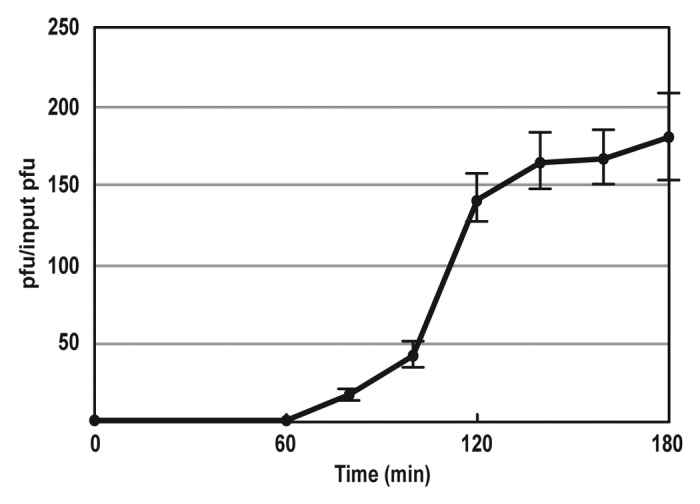
Figure 2. ϕX216 one-step growth curve for determination of burst size and time during infection of B. pseudomallei Bp82.
In silico prediction of ϕX216 amplification-based MALDI-TOF MS signal detection
In order to detect only progeny phage resulting from the presence of the bacterial target of interest (as opposed to detection of the input phage used to start an infection), it was necessary to initiate amplification at a phage concentration below the limit of detection. To address this and significantly reduce the labor and time for repeated preparation and analysis, the previously described method for in silico modeling26 was used to predict the time during ϕX216 infection of B. pseudomallei when a detectable MALDI-TOF MS signal would first be achieved.
The MALDI-TOF MS ϕX216 limit of detection (2.6 × 107 pfu/mL) is indicated in Figure 3 by a dashed line. Based on this value, an input ϕX216 concentration (vi) of 1.6 × 105 pfu/mL (well below instrument limit of detection) was used to infect B. pseudomallei at an initial concentration (xi) of 3.2 × 105 cfu/ml; multiplicity of infection (MOI) = 0.5). All parameters used in the algorithm are given in Table 1. As shown in Figure 1D, a ϕX216 burst, exemplified by the appearance of the 37.6 kDa major capsid protein peak, was observable within 2 h of phage amplification. The corresponding in silico model (Fig. 3) accurately predicted that phage concentrations would surpass instrument limit of detection within 2 h. This calculation eliminated the need to collect and prepare aliquots prior to 2 h post infection.
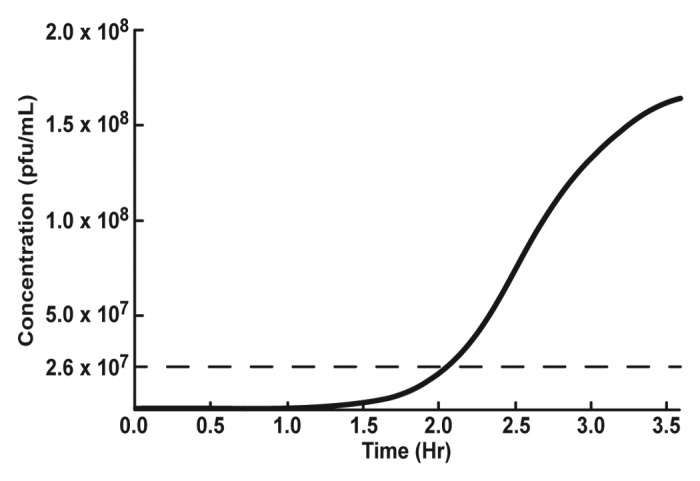
Figure 3. In silico prediction of ϕX216 amplification in B. pseudomallei. Dashed line: MALDI-TOF MS limit of phage detection.
Table 1. In silico ϕX216 amplification modeling parameters.
| Parameter | Description | Experimental values |
|---|---|---|
| a | Uninfected bacterial replication rate | 1.0 at 37 °C |
| b | Transmission coefficient (Measure of phage binding efficiency) |
1 × 10−7 |
| L | Burst size | 160 |
| k | Lysis rate | 1.5 |
| xi | Initial uninfected bacterial concentration | 3.2 × 105 cfu/mL |
| vi | Initial infecting phage concentration | 1.6 × 105 pfu/mL |
| m | Phage decay rate | 0 |
Phage amplification and MALDI-TOF MS for simultaneous B. pseudomallei antibiotic resistance determination
With the increasing occurrence of antibiotic resistant bacterial infections, it is often critical to the success of treatment and patient survival to quickly identify a suspected pathogen and determine its antibiotic resistance profile. Previous reports identified clinical B. pseudomallei strains harboring a C69Y substitution in the chromosomal penA gene encoding a putative twin arginine translocase (TAT)-exported β-lactamase that conveyed high-level ceftazidime resistance.13 Rholl et. al constructed a B. pseudomallei Bp82 mutant derivative that carried the PenA C69Y mutation and found that this not only increased ceftazidime resistance greater than 85-fold, but also sensitized mutants to other β-lactams including amoxicillin, ampicillin, carbenicillin, and imipenem.28 This made the Bp82-Bp82.3 isogenetic strain pair ideally suited for BSL2 studies investigating ϕX216 amplification-based Burkholderia ID in the same host background with and without exposure to ceftazidime. By exploiting the host-specificity of phage amplification and its natural reliance on a viable host,29 it was hypothesized that MALDI-TOF MS analysis for the appearance of a ϕX216-specific protein profile both with and without the addition of ceftazidime could serve to simultaneously ID and differentiate sensitive and resistant strains using a single technique; this effectively eliminated one day of testing time in comparison to current methods. Figure 4 shows the results of a 3 h ϕX216 infection of ceftazidime-sensitive B. pseudomallei Bp82 without the addition of the antibiotic. A major capsid peak was clearly observed within 2 h of the onset of phage infection (Fig. 4A). In contrast, as shown by the lack of a capsid protein peak at 37.6 kDa at any of the four time points shown in Figure 4B, the addition of ceftazidime at a concentration of 10 μg/mL killed the susceptible strain and therefore precluded phage amplification. In comparison, as shown in Figure 4C, phage amplification was detected during ϕX216 infection of isogenetic resistant mutant B. pseudomallei strain Bp82.3, even when amplification reactions were treated with 10 μg/mL ceftazidime. Importantly, parallel measurements of uninfected, phage-free bacterial controls (Fig. 5) showed no observable bacterial protein signal over the duration of phage amplification experiments. In addition, uninfected cultures were also allowed to incubate overnight and measured 18 h later to confirm culture viability, at which point bacterial protein profiles were observed (data not shown). This confirmed that any increase in bacterial concentration during the 2 h required to observe a reproducible phage signal was not sufficient to detect bacteria on their own. Taken together, the data in Figure 4 and Figure 5 clearly indicate the enhanced capability of phage amplification in comparison to bacterial protein profiling, detected by MALDI-TOF MS, for rapid and definite ID of B. pseudomallei and simultaneous antibiotic resistance determination. By this method and using a typical 96 to 384 well MALDI-TOF MS target plate, high throughput analysis of multiple parallel phage amplification reactions can be used to effectively assay a large collection of antibiotics of interest and determine the resistance profile.
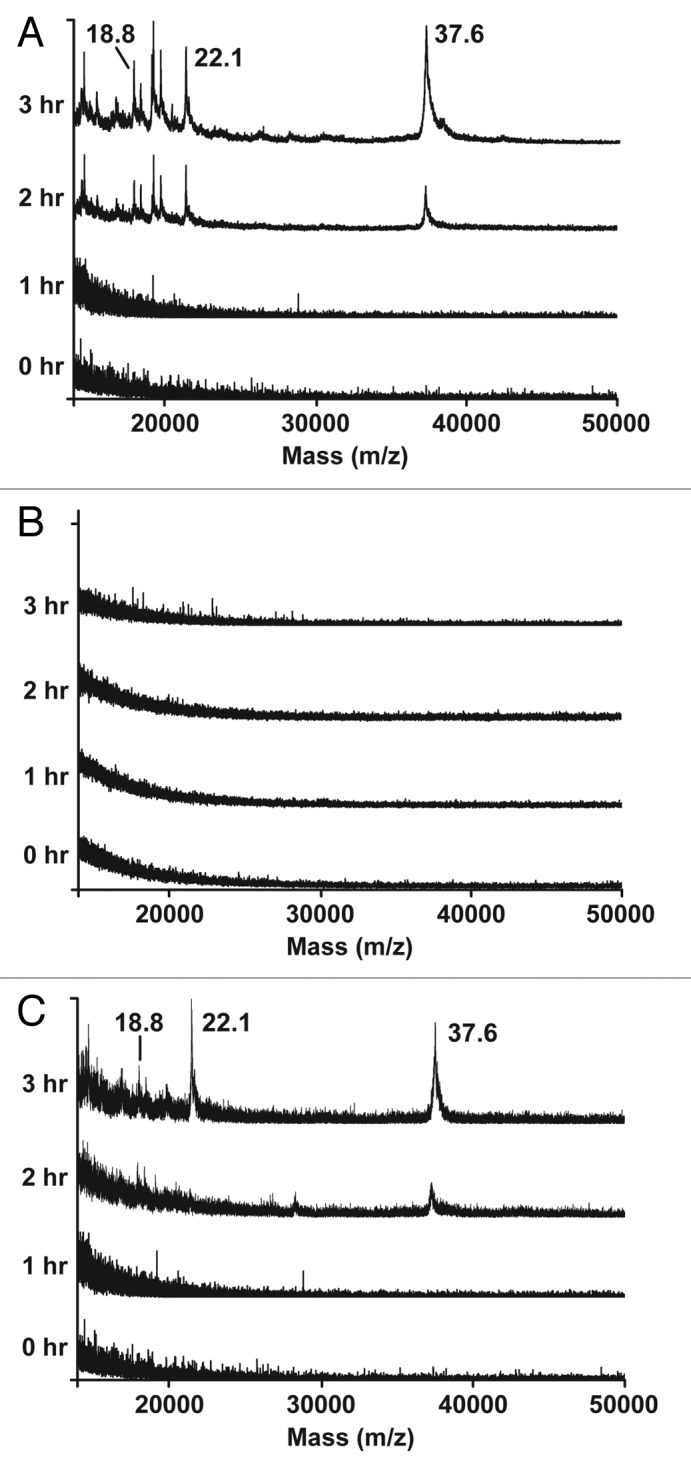
Figure 4. MALDI-TOF MS spectra of ϕX216 amplification in ceftazidime-susceptible B. pseudomallei Bp82 with (A) no addition of antibiotic, (B) addition of 10 μg/mL ceftazidime, (C) ceftazidime-resistant strain Bp82.3 with 10 μg/mL ceftazidime.
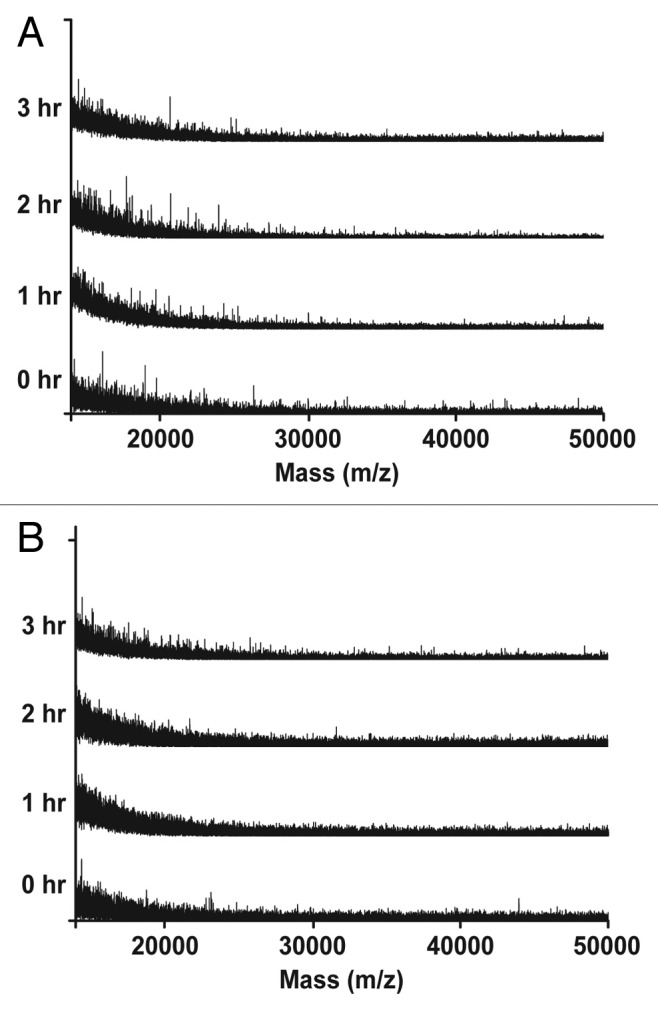
Figure 5. MALDI-TOF MS spectra of phage-free bacterial controls of (A) B. pseudomallei Bp82; without antibiotic and (B) B. pseudomallei Bp82.3 with 10 μg/mL ceftazidime.
In addition to its utility for B. pseudomallei ID, ϕX216 lyses 100% (9/9) of B. mallei strains tested.27 Although not explicitly assessed in this study, the described approach should therefore also be applicable for identification of B. mallei but not for differentiation of the two species. Phage resistance in some strains is a notable caveat to the application of phage amplification for identification and antibiotic resistance determination. Although ϕX216 only infected 78% of B. pseudomallei strains tested, it has one of the broadest ranges of infectivity for a single Burkholderia phage.27 To cover any remaining subset of resistant strains, one or more additional phages that infect these organisms must be isolated and characterized. B. pseudomallei phages are readily found in soil samples from endemic regions.30,31
Conclusions
We conclude that MALDI-TOF MS combined with phage amplification is a rapid, sensitive, and reproducibly predictable approach for protein-based bacterial ID and simultaneous antibiotic resistance determination. This method could be utilized with existing clinical and industrial MALDI-TOF MS systems such as the FDA approved Bruker Biotyper and Biomérieux VITEK MS, which are already in place in a growing number of laboratories. This method offers two new capabilities to conventional MALDI-TOF MS-based bacterial ID assays. First, phage amplification affords a significant increase in sensitivity and reduction in ID testing time. Also, by exploiting the reliance of phages on the presence of a viable host, phage-based MALDI-TOF MS provides the capability to simultaneously assay for bacterial antibiotic resistance. Currently available commercial MALDI-TOF MS-based systems do not have this capacity, but could directly benefit from the incorporation of phage amplification methods, which can be applied to any bacterial host for which a lytic phage exists. Although ceftazidime resistance in B. pseudomallei is yet rare, emergence of resistant clinical isolates of B. pseudomallei is being increasingly reported and the available literature suggests that resistance may be more widespread than previously thought.9-13 Furthermore, B. pseudomallei is considered a biothreat agent and malicious use of an antibiotic resistant organism is a prime concern. In both instances, (diagnosis of clinical melioidosis in endemic regions as well as malicious use of a biothreat agent), rapid diagnosis of both the organism and its susceptibility status are paramount for initiation of proper therapy. In this regard, our newly described method is highly advantageous in terms of time required for proper diagnosis, that is 3 h or less vs. conventional agar plate based methods that provide the same information in 24 h or more.
Materials and Methods
Bacterial strains and growth conditions
B. pseudomallei Bp82 and Bp82.3, which are attenuated, select agent excluded ΔpurM derivatives of B. pseudomallei strain 1026b, were grown under BLS2 conditions as described previously.28,32 Stains were either cultured overnight at 37 °C with continuous aeration in Luria Bertani (LB) broth (BD-Difco, 244620) with the addition of 80 μg/mL adenine or streaked onto LB-adenine agar.
Phage propagation and purification
ϕX216 phage stocks were obtained by liquid lysis of B. pseudomallei Bp82 at 37 °C in LB-adenine medium at an MOI of 0.5, as previously described.27,33 Lysates were centrifuged at 12,000 × g for 20 min at 4 °C to pellet bacterial debris. Supernatants were filtered-sterilized using 0.22 μm low-protein binding polyethersulfone filters (Nalgene, 564-0020). Phage particles were purified by polyethylene glycol (PEG) (8000 molecular weight) precipitation as previously described34 with the following modifications: 20 mL of crude lysate were mixed with a 20% w/v PEG solution containing 1.76 M NaCl and incubated overnight at 4 °C with continuous inversion. Precipitated phage particles were collected by centrifugation at 14,000 × g for 15 min at 4 °C. Resulting pellets were resuspended in 1 mL SM buffer (100 mM NaCl, 8 mM MgSO4, 50 mM TRIS-HCl, pH 7.4),35 refiltered, titered by spot titer assay,33 and stored at 4 °C.
Determination of burst size and time
The ϕX216 burst size and time were determined by generation of one-step growth curves as described previously.33 Briefly, mid-log phase cultures of B. pseudomallei Bp82 (1.0 × 108 cfu/mL) were inoculated with ϕX216 at an MOI of 0.005 and monitored by spot titer assay. Triplicate samples were taken at 20 min intervals beginning at the onset of infection over 180 min and 10 μL aliquots were spotted onto Bp82 lawns on LB adenine agar. Plates were incubated overnight at 37 °C. Plaques were counted at each time point as described36 and the burst size determined by dividing the resulting phage concentration values by the initial concentration for one cycle of amplification. Burst time was likewise taken after one cycle of amplification.
MALDI-TOF MS
Samples were prepared for MALDI-TOF MS as previously described.37 Briefly, 10 μL sample aliquots were treated with 2 µL of neat β-mercaptoethanol (BME) (Sigma, M6250) for 15 min at room temperature prior to analysis. One microliter of ferulic acid matrix (15 mg/mL) (Sigma, 46278) in a formic acid (Sigma, F0507), acetonitrile (Sigma, 271004), and de-ionized water mixture was then applied to a polished stainless steel sample plate (Bruker, 209520) followed by addition of 1 µL of treated sample and 1 µL of additional matrix in a sandwich fashion. Sample spots were allowed to air dry before MALDI-TOF MS analysis.
Mass spectrometric measurements were made with a Bruker Ultraflextreme MALDI-TOF mass spectrometer (Bruker Daltonics) equipped with a 355 nm Nd:YAG laser. Measurements were taken in reflector mode with a grid voltage of 50.3%, a delayed extraction time of 120 ns, and low mass cutoffs of 5 kDa and 15 kDa for bacterial and phage analyses, respectively. Three replicate spectra were collected for each analysis as 500 shot composites at a sampling frequency of 1 kHz using automated laser rastering.
Determination of MALDI-TOF MS limit of detection
To determine the limit of MALDI-TOF MS ϕX216 detection, B. pseudomallei ID, and antibiotic-resistance differentiation studies, 10-fold serial dilutions in phosphate buffered saline (PBS, pH 7.4) of a high-titer (3.0 × 109 pfu/mL) PEG-purified phage stock were assayed by MALDI-TOF MS. The lowest dilution that produced a ϕX216 protein spectra was considered as the limit of detection.
In silico prediction of phage amplification
In silico estimation of the time during a given ϕX216 infection when phage concentrations would surpass the MALDI-TOF MS detection threshold was conducted using a modified phage therapy prediction algorithm as previously described.26 Modeling parameters used are given in Table 1.
ID and differentiation of drug sensitive and resistant B. pseudomallei
For bacterial identification and antibiotic resistance determination, ceftazidime-susceptible ΔpurM strain Bp82 and its resistant PenA C69Y mutant derivative Bp82.332 were subjected to phage infection and amplification using ϕX216. Strains were grown in LB + adenine at 37 °C with or without the addition of 10 μg/mL ceftazidime (Sigma, C3809) to an optical density (OD620 nm) of 0.17, which corresponded to an approximate bacterial concentration of 1.0 × 108 cfu/mL. Cultures were next back diluted to 3.2 × 105 cfu/mL in fresh LB adenine and infected with 1.6 × 105 pfu/mL ϕX216 (MOI 0.5). Aliquots of each infected culture were assayed by MALDI-TOF MS with spectra obtained every hour for 3 h. Results were confirmed by plaque assay.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Acknowledgments
This work was supported by a Career Development Award to C.R.C from the Rocky Mountain Regional Center of Excellence for Biodefense and Emerging Infectious Diseases Research supported by National Institute of Allergy and Infectious Diseases grant U54 AI065357 and Defense Threat Reduction Agency contract W81XWH-07-C0061. Acquisition of the MALDI-TOF mass spectrometer was supported in part by National Science Foundation MRI grant CHE-1229156.
Glossary
Abbreviations:
- MALDI-TOF MS
matrix-assisted laser desorption ionization time-of-flight mass spectrometry
- ID
identification
- kDa
kilodalton
- CFU
colony forming unit
- PFU
plaque forming unit
- MOI
multiplicity of infection
- PEG
polyethylene glycol
- Nd:YAG
neodymium-doped yttrium aluminum garnet
- PBS
phosphate buffered saline
References
- 1.Cheng AC, Currie BJ. Melioidosis: epidemiology, pathophysiology, and management. Clin Microbiol Rev. 2005;18:383–416. doi: 10.1128/CMR.18.2.383-416.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wiersinga WJ, Currie BJ, Peacock SJ. Melioidosis. N Engl J Med. 2012;367:1035–44. doi: 10.1056/NEJMra1204699. [DOI] [PubMed] [Google Scholar]
- 3.Wiersinga WJ, van der Poll T, White NJ, Day NP, Peacock SJ. Melioidosis: insights into the pathogenicity of Burkholderia pseudomallei. Nat Rev Microbiol. 2006;4:272–82. doi: 10.1038/nrmicro1385. [DOI] [PubMed] [Google Scholar]
- 4.Limmathurotsakul D, Peacock SJ. Melioidosis: a clinical overview. Br Med Bull. 2011;99:125–39. doi: 10.1093/bmb/ldr007. [DOI] [PubMed] [Google Scholar]
- 5.Wuthiekanun V, Peacock SJ. Management of melioidosis. Expert Rev Anti Infect Ther. 2006;4:445–55. doi: 10.1586/14787210.4.3.445. [DOI] [PubMed] [Google Scholar]
- 6.Cheng AC. Melioidosis: advances in diagnosis and treatment. Curr Opin Infect Dis. 2010;23:554–9. doi: 10.1097/QCO.0b013e32833fb88c. [DOI] [PubMed] [Google Scholar]
- 7.Schweizer HP. Mechanisms of antibiotic resistance in Burkholderia pseudomallei: implications for treatment of melioidosis. Future Microbiol. 2012;7:1389–99. doi: 10.2217/fmb.12.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lipsitz R, Garges S, Aurigemma R, Baccam P, Blaney DD, Cheng AC, et al. Consensus guidelines for treatment of and post-exposure prophylaxis for infection with Burkholderia pseudomallei (melioidosis) and B. mallei (glanders): summary of the 2010 U.S. Department of Health and Human Services Burkholderia workshop, Townsville, Australia. Emerging Infectious Diseases, 2012
- 9.Kung CT, Lee CH, Li CJ, Lu HI, Ko SF, Liu JW. Development of ceftazidime resistance in Burkhoderia pseudomallei in a patient experiencing melioidosis with mediastinal lymphadenitis. Ann Acad Med Singapore. 2010;39:945–3. [PubMed] [Google Scholar]
- 10.Chantratita N, Rholl DA, Sim B, Wuthiekanun V, Limmathurotsakul D, Amornchai P, Thanwisai A, Chua HH, Ooi WF, Holden MT, et al. Antimicrobial resistance to ceftazidime involving loss of penicillin-binding protein 3 in Burkholderia pseudomallei. Proc Natl Acad Sci U S A. 2011;108:17165–70. doi: 10.1073/pnas.1111020108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Behera B, Prasad Babu TL, Kamalesh A, Reddy G. Ceftazidime resistance in Burkholderia pseudomallei: first report from India. Asian Pac J Trop Med. 2012;5:329–30. doi: 10.1016/S1995-7645(12)60050-9. [DOI] [PubMed] [Google Scholar]
- 12.Sarovich DS, Price EP, Von Schulze AT, Cook JM, Mayo M, Watson LM, Richardson L, Seymour ML, Tuanyok A, Engelthaler DM, et al. Characterization of ceftazidime resistance mechanisms in clinical isolates of Burkholderia pseudomallei from Australia. PLoS One. 2012;7:e30789. doi: 10.1371/journal.pone.0030789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sam IC, See KH, Puthucheary SD. Variations in ceftazidime and amoxicillin-clavulanate susceptibilities within a clonal infection of Burkholderia pseudomallei. J Clin Microbiol. 2009;47:1556–8. doi: 10.1128/JCM.01657-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holland RD, Wilkes JG, Rafii F, Sutherland JB, Persons CC, Voorhees KJ, Lay JO., Jr. Rapid identification of intact whole bacteria based on spectral patterns using matrix-assisted laser desorption/ionization with time-of-flight mass spectrometry. Rapid Commun Mass Spectrom. 1996;10:1227–32. doi: 10.1002/(SICI)1097-0231(19960731)10:10<1227::AID-RCM659>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 15.Lay JO., Jr. MALDI-TOF mass spectrometry of bacteria. Mass Spectrom Rev. 2001;20:172–94. doi: 10.1002/mas.10003. [DOI] [PubMed] [Google Scholar]
- 16.Seng P, Drancourt M, Gouriet F, La Scola B, Fournier PE, Rolain JM, Raoult D. Ongoing revolution in bacteriology: routine identification of bacteria by matrix-assisted laser desorption ionization time-of-flight mass spectrometry. Clin Infect Dis. 2009;49:543–51. doi: 10.1086/600885. [DOI] [PubMed] [Google Scholar]
- 17.Sparbier K, Schubert S, Weller U, Boogen C, Kostrzewa M. Matrix-assisted laser desorption ionization-time of flight mass spectrometry-based functional assay for rapid detection of resistance against β-lactam antibiotics. J Clin Microbiol. 2012;50:927–37. doi: 10.1128/JCM.05737-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jung JS, Popp C, Sparbier K, Lange C, Kostrzewa M, Schubert S. Evaluation of matrix-assisted laser desorption ionization-time of flight mass spectrometry for rapid detection of β-lactam resistance in Enterobacteriaceae derived from blood cultures. J Clin Microbiol. 2014;52:924–30. doi: 10.1128/JCM.02691-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sparbier K, Lange C, Jung J, Wieser A, Schubert S, Kostrzewa M. MALDI biotyper-based rapid resistance detection by stable-isotope labeling. J Clin Microbiol. 2013;51:3741–8. doi: 10.1128/JCM.01536-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abshire TG, Brown JE, Ezzell JW. Production and validation of the use of gamma phage for identification of Bacillus anthracis. J Clin Microbiol. 2005;43:4780–8. doi: 10.1128/JCM.43.9.4780-4788.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nicolle P, Le Minor L, Buttiaux R, Ducrest P. [Phage typing of Escherichia coli isolated from cases of infantile gastroenteritis. II. Relative frequency of types in different areas and the epidemiological value of the method] Bull Acad Natl Med. 1952;136:483–5. [PubMed] [Google Scholar]
- 22.Wallmark G, Laurell G. Phage typing of Staphylococcus aureus some bacteriological and clinical observations. Acta Pathol Microbiol Scand. 1952;30:109–14. [PubMed] [Google Scholar]
- 23.Postic B, Finland M. Observations on bacteriophage typing of Pseudomonas aeruginosa. J Clin Invest. 1961;40:2064–75. doi: 10.1172/JCI104432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Felix A. Phage typing of Salmonella typhimurium: its place in epidemiological and epizootiological investigations. J Gen Microbiol. 1956;14:208–22. doi: 10.1099/00221287-14-1-208. [DOI] [PubMed] [Google Scholar]
- 25.Madonna AJ, Van Cuyk S, Voorhees KJ. Detection of Escherichia coli using immunomagnetic separation and bacteriophage amplification coupled with matrix-assisted laser desorption/ionization time-of-flight mass spectrometry. Rapid Commun Mass Spectrom. 2003;17:257–63. doi: 10.1002/rcm.900. [DOI] [PubMed] [Google Scholar]
- 26.Cox CR, Rees JC, Voorhees KJ. Modeling bacteriophage amplification as a predictive tool for optimized MALDI-TOF MS-based bacterial detection. J Mass Spectrom. 2012;47:1435–41. doi: 10.1002/jms.3087. [DOI] [PubMed] [Google Scholar]
- 27.Kvitko BH, Cox CR, DeShazer D, Johnson SL, Voorhees KJ, Schweizer HP. φX216, a P2-like bacteriophage with broad Burkholderia pseudomallei and B. mallei strain infectivity. BMC Microbiol. 2012;12:289. doi: 10.1186/1471-2180-12-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rholl DA, Papp-Wallace KM, Tomaras AP, Vasil ML, Bonomo RA, Schweizer HP. Molecular Investigations of PenA-mediated β-lactam Resistance in Burkholderia pseudomallei. Front Microbiol. 2011;2:139. doi: 10.3389/fmicb.2011.00139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Majors LK, Doan LG, Rees JC, Voorhees KJ. A Rapid Method to Determine Minimum Inhibitory Concentration of Antibiotics in Staphylococcus aureus by Bacteriophage Amplification MALDI-TOF MS. 52nd American Society of Mass Spectrometry Conference on Mass Spectrometry and Allied Topics. Nashville, TN, 2004 [Google Scholar]
- 30.Gatedee J, Kritsiriwuthinan K, Galyov EE, Shan J, Dubinina E, Intarak N, Clokie MR, Korbsrisate S. Isolation and characterization of a novel podovirus which infects burkholderia pseudomallei. Virol J. 2011;8:366. doi: 10.1186/1743-422X-8-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yordpratum U, Tattawasart U, Wongratanacheewin S, Sermswan RW. Novel lytic bacteriophages from soil that lyse Burkholderia pseudomallei. FEMS Microbiol Lett. 2011;314:81–8. doi: 10.1111/j.1574-6968.2010.02150.x. [DOI] [PubMed] [Google Scholar]
- 32.Propst KL, Mima T, Choi KH, Dow SW, Schweizer HP. A Burkholderia pseudomallei ΔpurM mutant is avirulent in immunocompetent and immunodeficient animals: candidate strain for exclusion from select-agent lists. Infect Immun. 2010;78:3136–43. doi: 10.1128/IAI.01313-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carlson K. Working with Bacteriophages: Common Techniques and Methological Approaches. In: Kutter E, Sulakvelidze A, eds. Bacteriophages Biology and Applications. New York CRC Press, 2005:437-94 [Google Scholar]
- 34.Yamamoto KR, Alberts BM, Benzinger R, Lawhorne L, Treiber G. Rapid bacteriophage sedimentation in the presence of polyethylene glycol and its application to large-scale virus purification. Virology. 1970;40:734–44. doi: 10.1016/0042-6822(70)90218-7. [DOI] [PubMed] [Google Scholar]
- 35.Handbook of Molecular and Cellular Methods in Biology and Medicine. Third Edition. Ceske LJ, Kirakosyan A, Kaufman PB and Westfall MV (eds.). Boca Raton, FL: CRC Press, 2011 [Google Scholar]
- 36.Jett BD, Hatter KL, Huycke MM, Gilmore MS. Simplified agar plate method for quantifying viable bacteria. Biotechniques. 1997;23:648–50. doi: 10.2144/97234bm22. [DOI] [PubMed] [Google Scholar]
- 37.McAlpin CR, Cox CR, Matyi SA, Voorhees KJ. Enhanced matrix-assisted laser desorption/ionization time-of-flight mass spectrometric analysis of bacteriophage major capsid proteins with beta-mercaptoethanol pretreatment. Rapid Commun Mass Spectrom. 2010;24:11–4. doi: 10.1002/rcm.4349. [DOI] [PubMed] [Google Scholar]