Abstract
Context
Regionalization is intended to optimize outcomes by matching patient needs with institutional resources. The American College of Surgeons – Committee on Trauma (ACS-COT) recommends <5% under-triage (treatment of patients with moderate-severe injuries at non-trauma centers (NTCs)) and <50% over-triage (transfer of patients with minor injuries to trauma centers (TCs)).
Objective
To test the feasibility of accomplishing the ACS-COT benchmarks given current practice patterns by describing transfer patterns for patients taken initially to NTCs and estimating volume shifts and potential lives saved if full implementation occurred.
Design, Setting and Patients
Retrospective cohort study of adult trauma patients initially evaluated at NTCs in Pennsylvania (2001–2005). We used published estimates of mortality risk reduction associated with treatment at TCs.
Main Outcome Measures
Under- and over-triage rates; estimated patient volume shifts; number of lives saved.
Results
93,880 adult trauma patients were initially evaluated at NTCs in Pennsylvania between 2001–2005. Under-triage was 69%; over-triage was 53%. Achieving <5% under-triage would require the transfer of 18,945 patients/year, a five-fold increase from current practice (3,650 transfers/year). Given an absolute mortality risk reduction of 1.9% for patients with moderate-severe injuries treated at TCs, this change in practice would save 99 potential lives/year, or require 191 transfers/year to save 1 potential life.
Conclusion
Given current practice patterns, ACS-COT recommendations for the regionalization of trauma patients may not be feasible. To achieve 5% under-triage, TCs must increase their capacity 5-fold, physicians at NTCs must increase their capacity to discriminate between moderate-severe and other injuries, or the guidelines must be modified.
Keywords: decision making, compliance, safety, quality assurance, triage, discrimination
Regionalization in trauma has become the standard of care.1 Evidence suggests that inclusive trauma systems improve outcomes by matching patient needs with institutional resources.2–7 Ideally, therefore, patients with moderate-severe injuries should receive care at trauma centers (TCs), while those with minor injuries receive care at non-trauma centers (NTCs).8
Regionalization depends on the ability of providers to discriminate between patients with minor and moderate-severe injuries, or to correctly identify patients who would benefit from transfer to a TC. However, the clinical uncertainty associated with triage decisions makes discrimination necessarily imperfect. Balancing pragmatism with expert opinion regarding best practices, the ACS-COT has recommended that mature trauma systems strive to achieve rates of <5% under-triage (treatment of patients with moderate-severe injuries at NTCs) and <50% over-triage (treatment of patients with minor injuries at TCs).8 Nonetheless, the feasibility of accomplishing these benchmarks remains unclear.
The purpose of the current study was to explore the feasibility of implementing ACS-COT recommendations given current practice patterns. We used administrative data to describe the current patterns of regionalization in Pennsylvania, and then used our empiric observations to estimate the shifts in patient volume and number of lives saved if the ACS-COT under-triage target of <5% were achieved. Specifically, we focused on triage for patients taken initially to a NTC (secondary triage) because these decisions should theoretically have reflected only physicians’ judgments about the need for transfer.
METHODS
Data Sources
We conducted a retrospective cohort analysis of all trauma patients initially evaluated at a NTC in Pennsylvania, who were then admitted to the NTC or transferred to a TC during the period April 1, 2001 to March 31, 2005. Pennsylvania accounts for 9.2% of the US population and contains both rural and urban centers, which should result in a representative mix of trauma injury severity and mechanism.9 Additionally, it maintains both a statewide trauma registry and an administrative database of all hospitalizations. Pennsylvania Trauma Systems Foundation (PTSF) collects data from TCs on all transfers from outlying hospitals, all admissions to the ICU, all deaths, and all admissions from the field with a length of stay (LOS) >48 hours. It does not receive any information from NTCs. Pennsylvania Health Care Cost Containment Council (PHC4) coordinates an administrative database of all hospital admissions. However, it does not contain any information on transfers that occur prior to admission (i.e. from the Emergency Department (ED) of a NTC to a TC). Integrating information from both sources allowed us to construct a comprehensive picture of triage for patients who initially presented to the ED of a NTC.
Hospitals
We matched facilities in the PTSF and PHC4 databases using facility names. We identified TCs using a list published annually by PTSF of accredited facilities.10–14 All other hospitals were classified as NTCs. We excluded NTCs from the sample if they were from hospital referral regions (HRR) with a central city outside the state, were specialty hospitals (e.g., eye and ear infirmary), or federal hospitals. We further characterized hospitals by annual trauma admission volume, bed size, teaching status (major, minor, no teaching), participation in a health system that included a TC, and a previously validated measure of hospital treatment intensity (an empirically weighted index of treatment intensity among patients with a high probability of dying, calculated as factor score of 6 underlying standardized ratios including ICU admission, ICU length of stay, intubation/mechanical ventilation, tracheostomy, hemodialysis, and feeding tube insertion).15
Patients
Within PTSF, we identified patients over the age of 17 transferred to a regional TC after evaluation in a NTC. We excluded patients with burns, and patients admitted to the NTC prior to transfer (defined as having a LOS>24h). Within PHC4, we identified patients over the age of 17, admitted to a NTC for a primary diagnosis of trauma (ICD9-CM codes 800–959). We excluded patients with an admission related to the late effect of injuries, foreign bodies, burns, and isolated hip fractures.
We categorized injury severity as either minor (not requiring admission to a TC) or moderate-severe (requiring admission to a TC). We defined moderate-severe injuries as those patients with an ISS>15 or an injury defined by the ACS-COT as “life-threatening” or “critical.” If ACS-COT definitions required treatment information,8 we excluded the injury since PHC4 did not include the necessary data. [Table 1]
Table 1.
ICD9-CM diagnostic codes used to identify patients with moderate-severe injuries
| ACS-COT description of life- threatening or critical injury |
Assumption | ICD9-CM diagnostic codes |
|---|---|---|
| Injury to aorta, carotid and vertebral vessels | 900, 901 | |
| Injury to heart | 861.0, 861.1 | |
| >2 rib fractures or bilateral pulmonary contusions | >2 rib fractures, flail chest, or pulmonary contusions | 807.03–807.09, 807.4, 861.20–861.22, 861.30–32 |
| Injury to abdominal vasculature | 902 | |
| Open fracture with loss of distal pulses | Complete or partial amputation of upper/lower extremity | 887, 897 |
| Open skull fracture | 800.5–800.9, 801.5–801.9, 804.5–804.9 | |
| GCS<14 | Cerebral laceration with moderate-severe loss of consciousness | 851.03–851.05, 851.13–851.15, 851.23–851.25, 851.33–851.35, 851.43–851.45, 851.53–851.55, 851.63–851.65, 851.73–851.75, 851.83–851.85, 851.93–851.95 |
| Subarachnoid, subdural or epidural hemorrhage with moderate-severe loss of consciousness | 852.03–852.05, 852.13–852.15, 852.23–852.25, 852.33–852.35, 852.43–852.45, 852.53–852.55 | |
| Other intra-cranial hemorrhage with moderate-severe loss of consciousness | 853.03–853.05, 853.13–853.15 | |
| Intra-cranial injury of other and unspecified nature with moderate-severe loss of consciousness | 854.03–854.05, 854.13–854.15 | |
| Any vertebral column fracture | Fracture of vertebral column | 805, 806 |
| Open fracture of long bone | Open fracture of humerus, radius/ulna, femur, tibia, fibula | 812.1, 812.3, 812.5, 813.1, 813.3, 813.5, 813.8, 820.1, 820.3, 820.9, 821.1, 821.3, 823.1, 823.3, 823.9 |
| Severe torso injury with co-morbid disease | Injury to thoracic organs, GI tract, liver, spleen, kidney, pelvic organs, other intra-abdominal organs, unspecified intra-abdominal organs | 862–869 with co-morbid disease as defined by Elixhauser. |
| Grade IV liver laceration with >6 units pRBC transfused | Did not include | |
| Pelvic fracture with >6 units pRBC transfused | Did not include |
For each patient, we categorized the adherence to ACS-COT triage guidelines: true positive (patient with moderate-severe injury transferred to a TC), false positive (patient with minor injury transferred to a TC), false negative (patient with moderate-severe injury admitted to a NTC), and true negative (patient with minor injury admitted to a NTC). To assess the validity of using 2 separate datasets to describe Pennsylvania triage patterns, we confirmed that the cohort of people expected to appear in both datasets contained the same number of observations in each dataset over the same time period (PTSF (n=57,591) and PHC4 (n=57,451)).
We abstracted data on patient age, gender, and insurance status (Medicare only, Medicare and Medicaid, Medicare and commercial, Medicaid only, commercial only, uninsured). We categorized the time of the day of the transfer as peak (8 am – 6 pm) or off-peak (before 8 am or after 6 pm). We characterized comorbidities using the methodology of Elixhauser16 and the magnitude of injury using injury severity scores (ISS). In PTSF, trauma registrars had calculated ISS for patients based on information abstracted from the chart. For PHC4, we used a validated computer program (ICDMAP90) to translate ICD9-CM diagnostic codes into ISS.17 However, in a sensitivity analysis we observed that ICDMAP90 systematically underestimated injury severity when compared to registrar-calculated ISS for patients in PTSF. To address this bias, we developed a modified ICD9-ISS conversion program that resulted in a better approximation of the distribution of ISS in PTSF (see Appendix). Specifically, we calculated ISS by assigning an Abbreviated Injury Score (AIS) to each ICD9-CM diagnostic code using assumptions to translate diagnostic codes into descriptions of injury severity. We used this tool to calculate ISS for patients in PHC4.
Analysis
We calculated rates of secondary triage of trauma patients (i.e., triage after initial evaluation at a NTC) using the 2×2 table we constructed to categorize adherence to ACS-COT guidelines. We calculated secondary under-triage (sensitivity) as the number of patients with moderate-severe injuries admitted to a NTC divided by the total number of patients with moderate-severe injuries initially evaluated at a NTC. We calculated secondary over-triage (1-positive predictive value) as the number of patients with minor injuries transferred divided by the total number of patients transferred from a NTC to a TC. We compared patient and hospital-level covariables among patients admitted to NTCs and patients transferred to TCs with moderate-severe injuries, using Student’s t-test, Pearson’s χ2, or Spearman correlation test as appropriate. We performed multi-level hierarchical modeling to adjust for the association between patient- and hospital-level variables.
Simulation
To estimate the shifts in patient volume and number of lives saved if the ACS-COT recommended <5% under-triage rate were achieved in the context of these patterns, we simulated the transfer of 95% of moderate-severely injured patients from the NTC to a TC. Specifically, we used the empiric information regarding secondary under-triage and over-triage by NTCs to calculate the resulting number of patients with minor injuries who would also be transferred to the regional TC. We then used published estimates of mortality reduction to estimate the number needed to transfer (NNT) to save one life: 1.9% mortality risk reduction for patients with moderate-severe injuries treated at TCs, and 3.5% mortality risk reduction for patients with severe injuries treated at TCs.2
We conducted all analyses and data management with STATA 11/IC (College Station, TX). The University of Pittsburgh Institutional Review Board study reviewed and approved the study as exempt from the requirement of written informed consent.
RESULTS
Hospitals
Between April 1, 2001 and March 31, 2005, 197 acute care facilities in Pennsylvania evaluated trauma patients in their ED. We excluded 4 facilities in hospital referral regions (HRRs) that extended outside the state and 17 federal/specialty hospitals. Of the remaining 176 hospitals, 24 were adult TCs and 152 were NTCs.
Patients
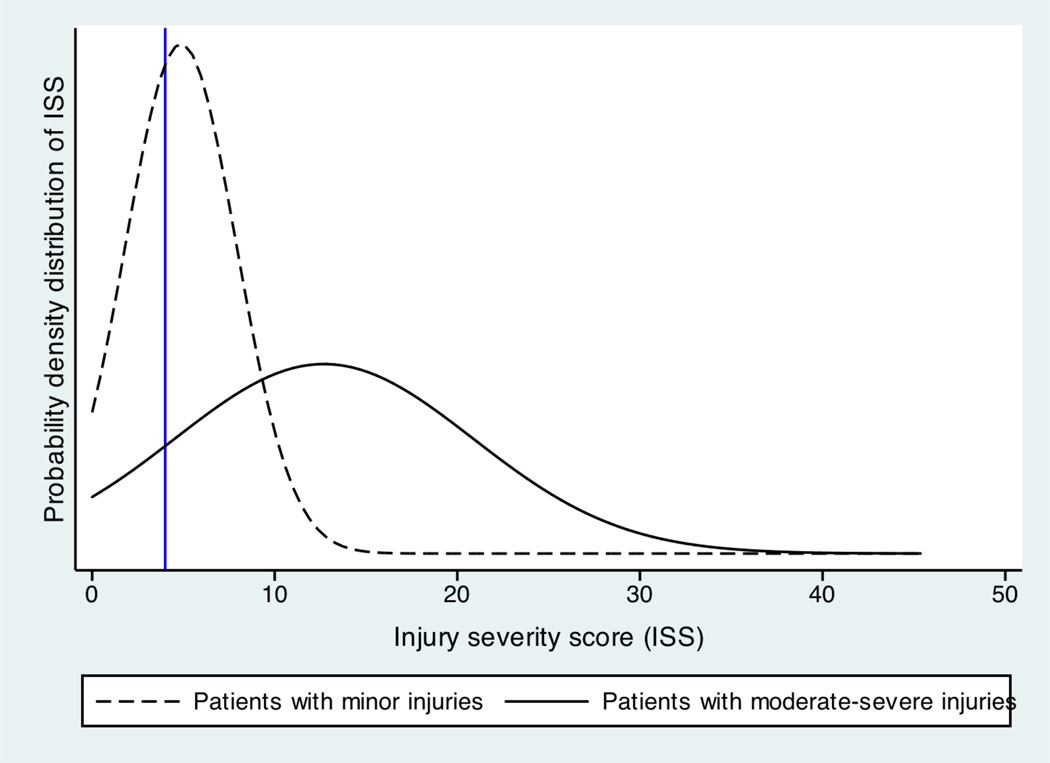
221,726 patients were admitted to these 176 hospitals. We excluded 61,250 (28%) patients evaluated initially in a TC, 63,340 (28%), patients whose injury complex did not meet our inclusion criteria, and 3,256 (2%) patients initially evaluated at a NTC who did not meet our inclusion criteria. Of the remaining cohort, 22,177 (24%) patients had a moderate-severe injury and 71,703 (76%) patients had a minor injury.
Triage Rates
Secondary under-triage occurred for 69% of patients with moderate-severe injuries initially evaluated at NTCs. Secondary over-triage occurred for 53% of patients transferred to TCs. [Figure 1]
Figure 1.
PHC4 and PTSF did not include information on patients discharged home from the ED (dark grey boxes), making our estimates of the total numbers of patients (dashed boxes) inexact.
In univariable analyses, hospitals more likely to transfer moderate-severely injured patients had fewer beds (p<0.001), had fewer average admissions (p<0.001), were less likely to have residents (p<0.001), were less likely to belong to a healthcare system with a TC (p<0.001), and were more likely to have lower treatment intensity (p<0.001).
Compared to patients with moderate-severe injuries who were under-triaged, patients who were appropriately transferred to TCs from NTCs were younger and more likely to be men. They were more likely either to have commercial insurance or no insurance, as expected for a younger population, and more likely to have been transferred during off-peak hours. They also had more co-morbidities and higher ISS. Patients with major vascular injuries, open skull fractures, and spinal cord injuries were more likely to be transferred to a regional TC. Patients with pulmonary injuries, spinal column fractures, or torso injuries were more likely to be admitted to the NTC. [Table 2]
Table 2.
Characteristics of patients with moderate-severe injuries admitted to NTC and transferred to TC
| Patients with moderate to severe injuries initially evaluated at a NTC |
p | |||
|---|---|---|---|---|
| Admissions to NTC | Transfers to TC | |||
| No patients, n(%) | 15,308 (69) | 6,869 (31) | ||
| Demographics | ||||
| Age (yr), mean± SEM | 71 years ± 0.16 | 54.8 years ± 0.27 | <0.001 | |
| Female (sex), n(%) | 8,807 (57.5) | 2,469 (36) | <0.001 | |
| Insurance | <0.001 | |||
| Commercial, n(%) | 3,020 (19.7) | 3,279 (48.1) | ||
| Medicare only, n(%) | 2,959 (19.3) | 886 (13) | ||
| Medicare medicaid, n(%) | 849 (5.6) | 134 (2) | ||
| Medicare commercial, n(%) | 7,309 (47.8) | 1,438 (21.1) | ||
| Medicaid only, n(%) | 883 (5.8) | 700 (10.3) | ||
| Uninsured, n(%) | 287 (1.9) | 377 (5.5) | ||
| Time of transfer | <0.001 | |||
| Peak time | 8,794 (57) | 2,986 (44) | ||
| Off-peak time | 6,514 (43) | 3,867 (56) | ||
| Comorbidities, mean ± SEM | 0.68 ± 0.01 | 1.34 ±0.02 | <0.001 | |
| ISS, mean±SEM | 10.3 ± 0.05 | 18.1 ± 0.11 | <0.001 | |
| Injuries | ||||
| Aortic, n(%) | 47 (0.31) | 111 (1.6) | <0.001 | |
| Cardiac, n(%) | 212 (1.4) | 71 (1.0) | 0.031 | |
| Rib fractures or pulmonary contusions, n(%) | 3,182 (20.8) | 1,261 (18.4) | <0.001 | |
| Great vessel injury, n(%) | 29 (0.2) | 70 (1.0) | <0.001 | |
| Open skull fracture, n(%) | 35 (0.2) | 116 (1.7) | <0.001 | |
| Open extremity fracture, n(%) | 25 (0.2) | 19 (0.3) | 0.08 | |
| Spinal column fracture, n(%) | 8,018 (52.4) | 2,644 (38.5) | <0.001 | |
| Spinal cord injury | 161 (1.1) | 143 (2.1) | <0.001 | |
| CNS injury, n(%) | 120 (0.8) | 126 (1.8) | <0.001 | |
| Significant torso injury with co-morbid condition, n(%) | 1,218 (8.0) | 613 (8.9) | 0.015 | |
In multivariable hierarchical models, hospitals with more beds (OR 0.95, 95% CI 0.94–0.98, p<0.001) and a higher number of average trauma admissions a year (OR 0.65, 95% CI 0.55–0.76, p<0.001) were less likely to transfer patients. Older patients (OR 0.96, 95% CI 0.95–0.96, p<0.001) and women (OR 0.73, 95% CI 0.67–0.79, p<0.001) were less likely to be transferred to a trauma center. Patients who had no insurance (OR 1.41, 95% CI 1.15–1.73, p<0.001), who presented at an off-peak time (OR 1.61, 95% CI 1.48–1.75, p<0.001), who had a greater number of co-morbidities (OR 2.45, 95% CI 2.34–2.56, p<0.001), and who had greater injury severity (OR 1.14, 95% CI 1.14–1.15, p<0.001) were more likely to be transferred to a trauma center.
Simulation
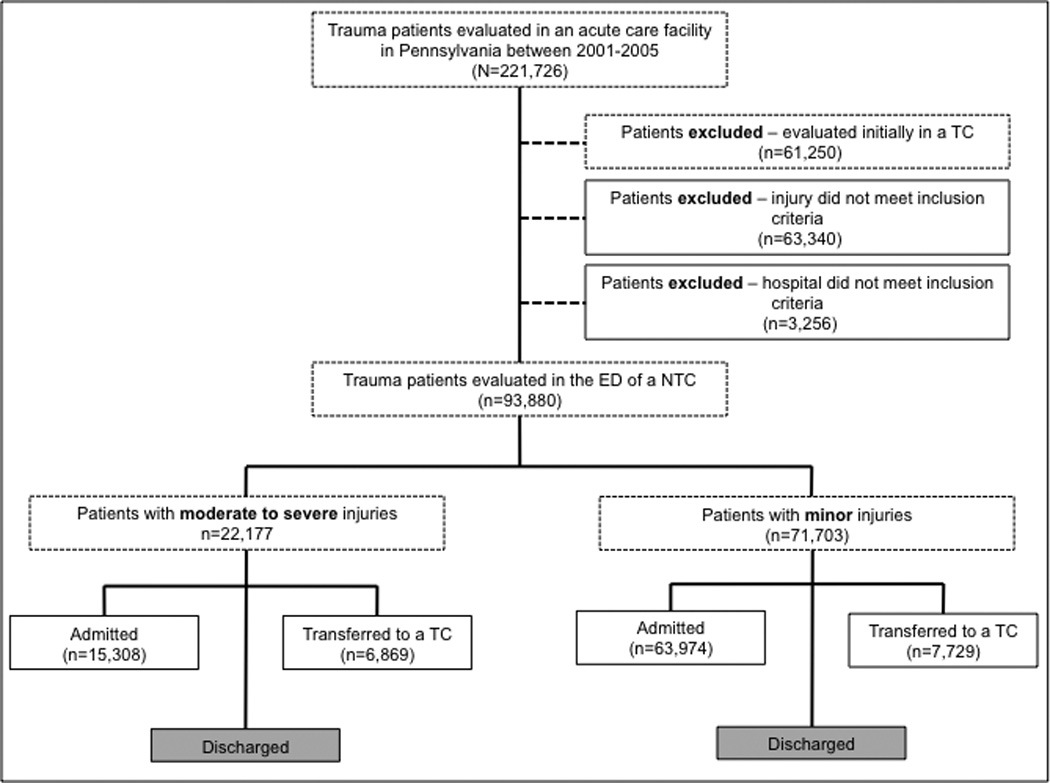
The distributions of injury severity for patients with minor and moderate-severe injuries overlap. [Figure 2] Therefore, physician discrimination (i.e., the identification of patients who do and do not require transfer) necessarily results in errors. Currently 3,650 transfers occur annually (1,717 with moderate-severe injuries and 1,932 with minor injuries). Using published mortality risk reduction estimates for patients with moderate-severe injuries treated at a TC,2 we estimate that current practice saves 32 lives, and the number needed to transfer (NNT) to save 1 life is 114.
Figure 2.
Overlap in the probability densities of minor and moderate-severe injuries implies that physician discrimination between the two populations is imperfect. Achieving <5% under-triage would require an ISS threshold of 4 (blue dashed line), resulting in the transfer 18,945 patients/year.
Meeting the ACS-COT benchmark of 5% under-triage for patients with moderate-severe injuries would result in the transfer of 18,945 patients/year: 5,267 with moderate-severe injuries and 13,678 with minor injuries. This represents a 5-fold increase in transfers; the largest TC would have to admit 4,649 transfers/year instead of 896 transfers/year and the smallest TC would have to admit 27 transfers/year instead of 5. This transfer pattern, provided the volume could be absorbed, would save 99 potential lives, or 67 more than current practice. The incremental NNT would be 228 and the total NNT would be 191.
One possible strategy to improve physician discrimination would be to amend the transfer criteria. Currently, transfer criteria include an amalgam of moderate to severe injuries (AIS≥2). If the ACS-COT mandated only the regionalization of treatment for patients with severe injuries (AIS≥4), there would be less overlap in the severity distributions of patients who did or did not require transfer. Meeting the ACS-COT benchmark for 5% under-triage for patients with severe injuries would then result in the transfer of 2,285 patients/year: 949 with severe injuries and 1,336 with moderate injuries. This represents 1,368 (40%) fewer transfers; the largest TC would admit 560 transfers/year and the smallest TC would admit 3 transfers/year. Of the 1,717 patients currently transferred with moderate-severe injuries, 590 would remain at the NTC. These modified criteria would save 58 potential lives/year, but lose 11/year. Consequently, adopting modified criteria would result in 47 potential lives saved/year, or 15 more than current practice. The total NNT would be 48 [Figure 3]
Figure 3.
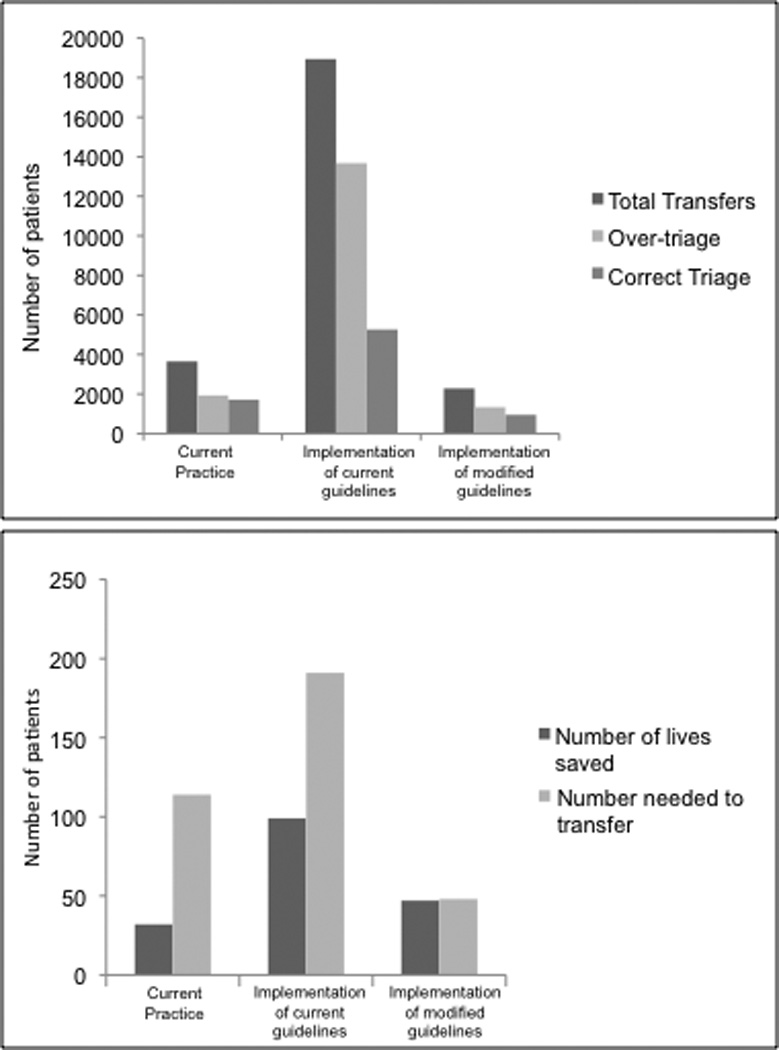
A) Distribution of transfers from NTCs to TCs. B) Number of lives saved (patients transferred with moderate-severe injuries divided by the reciprocal of the absolute mortality risk reduction) compared to the NNT (patients transferred divided by number of lives saved).
DISCUSSION
In this retrospective cohort analysis of trauma patients initially evaluated at NTCs in Pennsylvania between 2001 and 2005, we demonstrated that current rates of secondary under- and over-triage do not begin to approach ACS-COT recommendations. In the context of current practice patterns, full implementation ACS-COT guidelines would require a 5-fold increase in annual transfers from NTCs to TCs. Hospitals currently lack the capacity to absorb this volume, making the 67 incremental potential lives saved by implementation impossible to achieve. Changing the population targeted for an under-triage rate of <5% to those patients with severe injuries only increases the feasibility of achieving the target, but would compromise quality and safety.
Previous studies have described rates of 30% overall under-triage among patients with moderate-severe injuries.18,19,20 They have implicitly assumed that physicians can realistically accomplish 5% under-triage, and have attributed failures to regionalize patients either to bias20 or to unacceptable variations in care.18,19 Our analysis of secondary triage patterns brings into question the validity of these conclusions. Primary triage decisions made in the field reflect considerations of physiologic stability, injury severity, and proximity to a TC. Secondary triage decisions made in the ED of a NTC should reflect physicians’ best efforts to match patient needs with institutional resources. Our finding of 70% secondary under-triage suggests that physician discrimination between patients with minor and moderate-severe injuries may play a significant role in ongoing failures to accomplish complete regionalization. Given the existing ability of physicians to discriminate among patients with minor and moderate-severe injuries under conditions of uncertainty, the appropriate transfer of 95% of the moderate-severely injured would require transfer of a far higher proportion of patients with minor injuries than previously supposed. Quality improvement initiatives that raise the number of transfers without re-allocating resources would significantly burden TCs. Moreover, higher occupancy rates correlate with a risk of in-hospital mortality,21 so safely increasing the number of transfers five-fold would require substantial changes in personnel and infrastructure.
Instead, the ACS-COT might consider new educational strategies for helping physicians to discriminate between patients with minor and moderate-severe injuries beyond Advanced Trauma Life Support (ATLS), the predominant method by which the ACS-COT disseminates its guidelines. Educational techniques that modify heuristics, such as those described in the threat detection literature, might have better success at helping physicians to navigate the uncertainty of clinical diagnosis.22 Finally, the ACS-COT could amend how it defines criteria for transfer to a TC. Management of certain injuries categorized by the ACS-COT as ”life-threatening”, such as spinal column fractures (AIS 2), may not require the specialized services available in a TC. Limiting transfer criteria to injuries known to influence immediate and early mortality, such as a transected aorta (AIS 4), might improve discrimination and ensure that those transferred are most likely to benefit.
Regionalization has become the paradigm for allocation of resources in critical illness, including mechanical ventilation,23 cardiac catheterization,24 and stroke.25 Indeed, the Institute of Medicine uses trauma as an exemplar for these efforts.1 The safety of changing trauma regionalization guidelines remains unclear. Current practice may not achieve optimal results; however, simply increasing the volume of transfers without effecting system changes may have unintended consequences. Alternatively, reducing the total number of transfers by making transfer criteria more stringent may result in worsened outcomes for patients remaining at NTCs. Changing triage criteria might also have safety implications other than those considered here. Our estimates include only mortality benefits and do not account for the morbidity reduction resulting from care at a high volume center.
Our study has several limitations. First, we combine single state administrative data with state registry information to identify triage patterns for trauma. Privacy restrictions prevented us from linking data records to confirm we identify the same patients in both datasets. However, the degree of overlap between the two cohorts (99.7%) suggests that our inclusion criteria have allowed us to identify the same population of patients in both datasets. Second, we were unable to identify patients evaluated and then discharged from the ED of NTCs. However, exclusion of these patients should bias our results towards the null. Physicians who discharged patients home with moderate-severe injuries did not recognize the need to transfer these patients to a TC. Had they admitted them to an acute care facility at all, we assume they most probably would have chosen their own hospital, thereby increasing rates of under-triage. Third, we used ISS as a surrogate for the clinical cues that might inform physician decisions about whether a patient had a minor or a moderate-severe injury. Our ICD-9 to ISS conversion tool attempted to mimic the calculations of trauma registrars. Their assessments are widely accepted as best means of quantifying injury severity retrospectively. Nonetheless, ISS may not capture the degree of uncertainty experienced by physicians. Our findings of 70% under-triage would suggest that ISS inflates injury severity compared to that perceived by the clinician. Patients with moderate-severe injuries may appear even more similar to patients with minor injuries than our analysis would suggest, biasing our calculations of the number of patients needed to transfer to save additional lives towards the null.
In conclusion, our findings bring into question the feasibility of fully implementing the model of regionalization currently advocated by the ACS-COT given current practice patterns. Triaging all moderate-severely injured to TCs may require the transfer of so many patients with minor injuries that it would overwhelm the existing system. In the context of existing infrastructure, alternatives for feasibly achieving a regionalized trauma system either require that physicians at NTCs increase their capacity to discriminate between moderate-severe and other injuries or that ACS-COT guidelines and targets for under-triage be modified to reflect current limitations in discrimination.
Acknowledgements
Funding/Support: This work was supported by grant 1KL2RR024154 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research (Dr. Mohan). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp. This work was also funded in part by a seed grant from the Department of Critical Care Medicine at the University of Pittsburgh.
Additional Contributions: We thank Dr. Joyce Chang, PhD at the University of Pittsburgh for statistical support and Nathan McWilliams, MPA at the Pennsylvania Trauma Systems Foundation for help acquiring the PTSF registry data. Neither received compensation beyond their normal salaries.
Footnotes
The work was performed at the University of Pittsburgh, Pittsburgh, PA.
Publisher's Disclaimer: Pennsylvania Health Care Cost Containment Council Disclaimer
The Pennsylvania Health Care Cost Containment Council (PHC4) is an independent state agency and has provided data to this entity in an effort to further PHC4’s missions of educating the public and containing health care costs in Pennsylvania. PHC4, its agents, and staff have made no representation, guarantee or warranty (express or implied) that the data provided to this entity are error free or that the use of the data will avoid difference of opinion or interpretation. This analysis was not prepared by PHC4. It was prepared by the authors of this manuscript. PHC4, its agents, and staff bear no responsibility or liability for the results of this analysis, which are solely the opinion of the authors.
Pennsylvania Trauma Systems Foundation Disclaimer
These data were provided by the Pennsylvania Trauma Systems Foundation, Mechanicsburg, PA. The Foundation specifically disclaims responsibility for any analyses, interpretations, or conclusions.
Author contributions: Dr. Mohan had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Mohan, Rosengart, Farris, Angus, Barnato
Acquisition of data: Mohan, Rosengart, Barnato
Analysis and interpretation of data: Mohan, Rosengart, Farris, Cohen, Angus, Barnato
Drafting of the manuscript: Mohan
Critical revision of the manuscript for important intellectual content: Rosengart, Farris, Cohen, Angus, Barnato
Statistical analysis: Mohan, Cohen
Obtained funding: Mohan
Administrative, technical, or material support: Mohan, Cohen
Financial Disclosures: None
Role of the Sponsors: the funding agencies had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; or preparation, review or approval of the manuscript.
References
- 1.US Department of Health and Human Services. Model Trauma System Planning and Evaluation. [Accessed November 21, 2010]; https://www.socialtext.net/acs-demo-wiki/index.cgi?regional_trauma_systems_optimal_elements_integration_and_assessment_systems_consultation_guide. Published February 2006.
- 2.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. NEJM. 2006;354(4):366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 3.Celso B, Tepas J, Langland-Orban B, et al. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J Trauma. 2006;60(2):371–378. doi: 10.1097/01.ta.0000197916.99629.eb. [DOI] [PubMed] [Google Scholar]
- 4.Demetriades D, Martin M, Salim A, et al. The effect of trauma center designation and trauma voume on outcome in specific severe injuries. Ann Surg. 2005;242(4):512–517. doi: 10.1097/01.sla.0000184169.73614.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mann NC. Assessing the effectiveness and optimal structure of trauma systems: a consensus among experts. J Trauma. 1999;47(3S):S69–S74. doi: 10.1097/00005373-199909001-00015. [DOI] [PubMed] [Google Scholar]
- 6.Mullins RJ, Mann NC. Population based research assessing the effectiveness of trauma systems. J Trauma. 1999;47(3S):S59–S66. doi: 10.1097/00005373-199909001-00013. [DOI] [PubMed] [Google Scholar]
- 7.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. The impact of trauma-center care on functional outcomes following major lower-limb trauma. Jone Bone Joint Surg Am. 2008;90(1):101–109. doi: 10.2106/JBJS.F.01225. [DOI] [PubMed] [Google Scholar]
- 8.Committee on Trauma – American College of Surgeons. Resources for optimal care of the injured patient 2006. Chicago: American College of Surgeons; 2006. [Google Scholar]
- 9.US Census Bureau. State and County QuickFacts. [Accessed July 1, 2010]; Available at http://quickfacts.census.gov/qfd/states/42000.
- 10.Pennsylvania Trauma Systems Foundation. Trauma center accreditation status October 2000. [Accessed May 14, 2010]; Available from: www.ptsf.org. [Google Scholar]
- 11.Pennsylvania Trauma Systems Foundation. Trauma center accreditation status October 2001. [Accessed May 14, 2010]; Available from: www.ptsf.org. [Google Scholar]
- 12.Pennsylvania Trauma Systems Foundation. Trauma center accreditation status October 2002. [Accessed May 14, 2010]; Available from: www.ptsf.org. [Google Scholar]
- 13.Pennsylvania Trauma Systems Foundation. Trauma center accreditation status October 2003. [Accessed May 14, 2010]; Available from: www.ptsf.org. [Google Scholar]
- 14.Pennsylvania Trauma Systems Foundation. Trauma center accreditation status October 2004. [Accessed May 14, 2010]; Available from: www.ptsf.org. [Google Scholar]
- 15.Barnato AE, Farrell MH, Chang CH, Lave JR, Roberts MR, Angus DC. Development and validation of hospital “end-of-life” treatment intensity measures. Med Care. 2009;47(10):1098–1105. doi: 10.1097/MLR.0b013e3181993191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elixhauser A, Steinter C, Harris RD, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 17.MacKenzie EJ, Steinwachs DM, Shankar B. Classifying trauma severity based on hospital discharge diagnoses: validation of an ICD-9CM to AIS-85 conversion table. Med Care. 1989;27(4):412–422. doi: 10.1097/00005650-198904000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Macias CA, Rosengart MR, Puyana JC, et al. The effects of trauma center care, admission volume, and surgical volume on paralysis after traumatic spinal cord injury. Ann Surg. 2009;249(1):10–17. doi: 10.1097/SLA.0b013e31818a1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nathens AB, Jurkovich GJ, MacKenzie EJ, Rivara FP. A resource-based assessment of trauma care in the United States. J Trauma. 2004;56(1):173–178. doi: 10.1097/01.TA.0000056159.65396.7C. [DOI] [PubMed] [Google Scholar]
- 20.Schilling PL, Campbell DA, Englesbe MJ, Davis MM. A comparison of in-hospital mortality risk conferred by high hospital occupancy, differences in nurse staffing levels, weekend admission, and seasonal influenza. Med Care. 2010;48(3):224–232. doi: 10.1097/MLR.0b013e3181c162c0. [DOI] [PubMed] [Google Scholar]
- 21.Chang DC, Bass RR, Cornwell EE, MacKenzie EJ. Undertriage of elderly trauma patients to state-designated trauma centers. Arch Surg. 2008;143(8):776–781. doi: 10.1001/archsurg.143.8.776. [DOI] [PubMed] [Google Scholar]
- 22.Wolfe JM, Horowitz TS, Van Wert MJ, et al. Low target prevalence is a stubborn source of errors in visual search tasks. J Exp Psychol Gen. 2007;136(4):623–638. doi: 10.1037/0096-3445.136.4.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Branas CC, MacKenzie EJ, Williams JC. Access to trauma centers in the United States. JAMA. 2005;293(21):2626–2633. doi: 10.1001/jama.293.21.2626. [DOI] [PubMed] [Google Scholar]
- 24.Kahn JM, Linde-Zwirble WT, Wunsch H, et al. Potential value of regionalized intensive care for mechanically ventilated medical patients. Am J Respir Crit Care Med. 2008;177:285–291. doi: 10.1164/rccm.200708-1214OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Le May MR, So DY, Dionne R, et al. A citywide protocol for primary PCI in ST-segment elevation myocardial infarction. NEJM. 2008;358:231–240. doi: 10.1056/NEJMoa073102. [DOI] [PubMed] [Google Scholar]
- 26.Gropen T, Magdon-Ismail Z, Day D, Melluzzo S, Schwamm LH. Regional implementation of the stroke systems of care model. Stroke. 2009;40(5):1793–1802. doi: 10.1161/STROKEAHA.108.531053. [DOI] [PubMed] [Google Scholar]