Abstract
The role of basophils, the rarest of blood granulocytes, in the pathophysiology of allergic asthma is still incompletely understood. Indirect evidence generated over many decades is consistent with a role for basophils in disease promotion. Recent improvements in procedures to purify and analyze very small numbers of human cells have generally supported this view, but have also revealed new complexities.
This chapter focuses on our analyses of Fcε R1 function in basophils in the context of understanding and treating human allergic asthma. In long-term studies, we demonstrated that asthmatic subjects have higher circulating numbers of basophils than non-atopic non-asthmatic subjects and that their basophils show higher rates of both basal and anti-IgE or antigen-stimulated histamine release. These results hint at a direct role for basophils in promoting asthma. Supporting this interpretation, the non-releaser phenotype that we linked to the excessive proteolysis of Syk via the ubiquitin/proteasomal pathway is less common in basophils from asthmatic than non-asthmatic donors. The discovery of a basophil-specific pathway regulating Syk levels presents a clear opportunity for therapy. Another route to therapy was revealed by evidence that basophil FcεRI signaling can be downregulated by co-crosslinking the ITAM-containing IgE receptor, FcγRI, to the ITIM-containing IgG receptor, FcγRIIB. Based on this discovery, hybrid co-crosslinking fusion proteins are being engineered as potential therapies targeting basophils. A third distinguishing property of human basophils is their high dependence on IgE binding to stabilize membrane FcεRI. The circulating IgE scavenging mAb, Omalizumab, reduces FcεRI expression in basophils from asthmatics by over 95% and produces a substantial impairment of IL-4, IL-8 and IL-13 production in response to the crosslinking of residual cell surface IgE-FcεRI. A search for small molecule inhibitors that similarly impair high affinity IgE binding to basophils may yield reagents that mimic Omalizumab’s therapeutic benefits without the potential for immune side effects.
Although studies on allergen and FcεRI-mediated basophil activation all point to a role in promoting disease, a case can also be made for an alternative or additional role of basophil FcεRI in protection against allergic asthma. Human basophils have high affinities for IgE, they upregulate receptor levels over a >100-fold range as circulating IgE levels increase and they have short half-lives in the circulation. Thus, when allergen is absent, basophil FcεRI could serve as scavengers of serum IgE and therefore protectors against mast cell IgE-mediated inflammatory responses. Further studies are clearly needed to determine if FcεR-expressing basophils play pathogenic or protective roles – or both – in human allergic asthma and other IgE-mediated inflammatory disorders.
Keywords: Allergic asthma, basophils, FcεRI, IgE, pathogenesis, therapy
INTRODUCTION
With 23 million asthmatic Americans, including approximately 7 million children [1, 2], asthma is the fifth most common chronic disease in the USA and the third most common among children. The global prevalence, morbidity, mortality and economic burden of asthma are likewise devastating. According to World Health Organization estimates, over 300 million people suffer from asthma worldwide [3].
Bronchial asthma was first described in 1892 by Sir William Osler [4], 13 years after Paul Ehrlich first discovered mast cells and named human basophils after their metachromatic staining at low pH with basic dyes [5, 6]. Circulating basophils and tissue mast cells (MCs) share a number of similarities, including their similar granule staining properties and their expression of the αβγ2 form of FcεRI constitutively on their surface. Both cell types respond to FcεRI crosslinking by the release of preformed histamine and leukotrienes, and the synthesis of cytokines, chemokines and growth factors predominately of the Th-2 pattern [7]. However, mast cells are generally thought to play the more central role in allergic asthma and in a wide range of related diseases including allergic rhinitis, atopic dermatitis, and allergic and anaphylactic responses to foods, plant pollens and drugs. This is partly because mast cells are more abundant than basophils. It is also because most of the evidence that basophils contribute to asthma separately from mast cells is indirect. For example, basophils and basophil precursors can be recruited from the peripheral blood to sites of allergic reactions in asthmatic individuals and basophils are well-known constituents of the cellular infiltrate in bronchial tissues of atopic asthmatic patients [8, 9]. Bronchial responsiveness to acetylcholine has been shown to be highly correlated to airway basophil and mast cell numbers, and the total number of these cells in the lung is elevated in asthmatic versus control subjects [10]. Additionally, basophil chemotactic activity is higher in BAL fluids from asthmatic than normal subjects, and long-term glucocorticoid treatment reduces the proportion of basophils in BAL fluid in steroid-dependent intractable asthma [11,12]. In patients having an exacerbation of asthma, basophil numbers dropped after resolution of the exacerbation with inhaled corticosteroid treatment [13]. Furthermore, we and others have reported a significant accumulation of basophils in the lung tissues from individuals who died from asthma in comparison with the lungs of individuals with a history of asthma who died from nonasthmatic causes [14]. Although all these observations are consistent with a distinct role for basophils in asthma, none provides definitive proof.
Supporting the likely contribution of basophils to disease promotion, we now know that human basophils are a major source of IL-4 and IL-13 [15, 16], the key cytokines implicated in stimulating and amplifying the TH2 response, and thus the propagation of allergic inflammation. This putative immunomodulatory role of basophils is supported further by their ability to express CD40 ligand, which, together with IL-4 and IL-13, serves to induce B-cell proliferation and class switching to IgE and IgG4 [17]. It has also been discovered that basophils are capable of modulating their FcεRI expression in response to circulating IgE levels. McGlashan and colleagues were the first to show that the clinical improvement of symptomatic disease during treatment of asthmatics with IgE-scavenging humanized mAb, Omalizumab, causes a dramatic and reversible reduction in basophil FcεRI expression levels and reduced FcεRI-mediated basophil degranulation [18,19]. These alterations in basophil properties, which are induced by anti-IgE immunotherapy, are correlated with the clinical improvement of symptomatic disease and especially with reductions in hospitalizations for acute distress [20] These more contemporary data continue to support a positive role for basophils in disease progression.
Recently, innovative research using murine models has provided direct evidence that basophils can serve as effector cells in both host defense responses, particularly parasite expulsion, and in IgE-associated inflammatory and allergic reactions. Work by Sokol and colleagues revealed that basophils can function as antigen-presenting cells and as initiators of the T helper cell 2 (Th2) mediated immune response by providing the crucial Th2-skewing cytokines, interleukin (IL-4) and thymic stromal lymphopoietin [21, 22]. By adoptive transfer of basophils from normal to FcεRI-deficient mice, Karasuyama and colleagues showed that basophils can elicit IgE-mediated allergic inflammation independently of T cells and mast cells [23, 24]. Furthermore, Denzel and coworkers illustrated the role of basophils as important contributors to humoral memory immune responses [25]. These and other recent results provide compelling evidence that basophils play non-redundant roles in both the initiation and propagation of allergic inflammatory diseases in mice. However, murine models are not really capable of recapitulating basophil function in the complex context of human asthma nor the years of chronic allergen exposure experienced by patients. Thus, studies in mice encourage, but do not replace, the need to study human basophils in order to better understand the pathogenesis and therapy of human allergic inflammation.
This chapter focuses on our longitudinal studies of the signaling properties of basophils from volunteers with or without asthma. Our findings support a role for allergen and IgE-mediated human basophil FcεRI signaling in asthma and they reveal new potential targets for therapy. Several of these targets are based on properties unique to human basophils and could not have emerged from studies in mice. On the other hand, we also argue that, when allergen is absent, the FcεRI of circulating basophils could serve a protective role. Lymphocytes, neutrophils and other leukocytes often play both positive and negative roles in human immune disease; it would not be unreasonable for basophils to also play opposing roles under different conditions.
DEVELOPING A COHORT OF BASOPHIL DONORS FOR LONGITUDINAL STUDIES
Our work was performed using basophils from a cohort of young, healthy, nonsmoking volunteers consisting, at any time, of up to 75 atopic asthmatics and 75 non-atopic non-asthmatics [26]. Asthma, tested under physician supervision, was defined as either a >/= 15% increase of forced expiratory volume in one second (FEV1) in response to 200 µg of albuterol or a decrease of the FEV1 of at least 20% after inhalation of >/=16 mg/ml methacholine. Atopy, based on results of allergy skin tests using aeroallergens common in the Albuquerque area (Fremont cottonwood, juniper-mountain cedar, Bermuda grass, bluegrass, fescue, Russian thistle, kochia, western ragweed, cat dander, and house dust mite), was defined as two or more positive skin prick tests (>/=3 mm in wheal diameter) and no wheal in response to normal saline. Control subjects had no history of asthma, negative immediate type skin tests, normal spirometry and negative methacholine challenges. Asthmatics were positive for all four criteria. Most of the asthmatics were intermittent asthmatics, based on their spirometry symptoms and medication use (http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm). Their medications did not include systemic glucocorticosteroids, but could include inhaled, nasal and skin steroids, inhaled β2 agonists, oral contraceptives and antihistamines.
IMPROVING THE ISOLATION OF HUMAN BASOPHILS
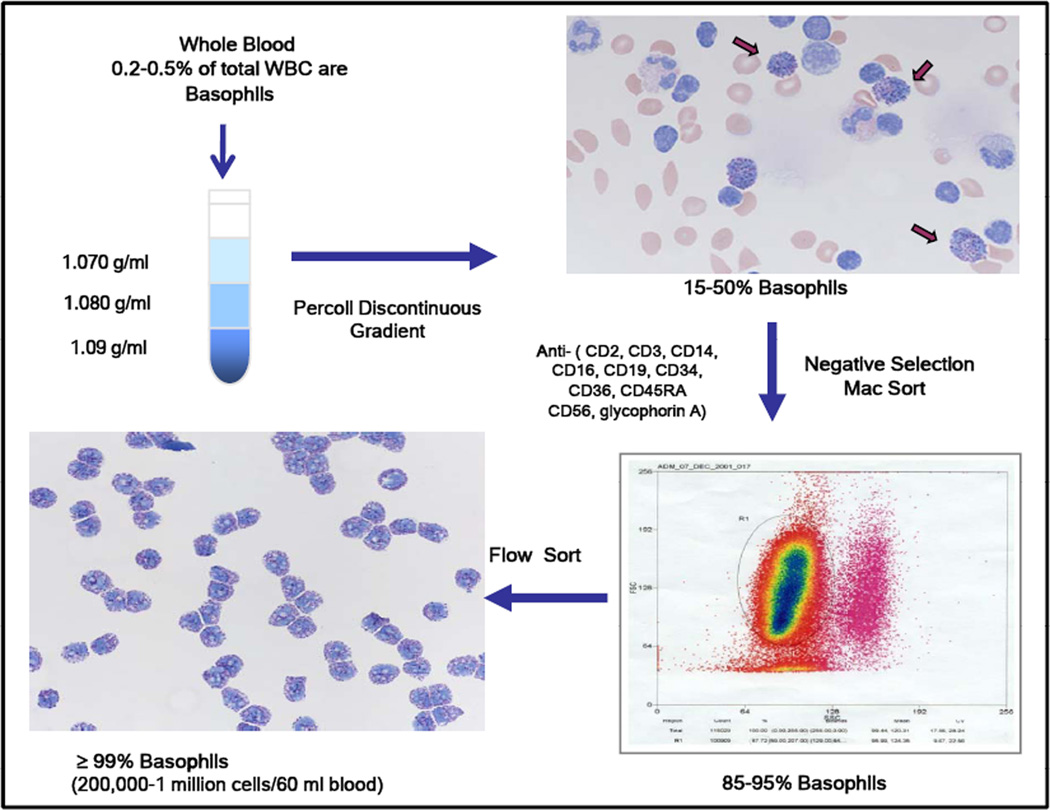
The challenge of isolating human basophils in numbers adequate for biochemical study was a major technical problem. In the early 1990s, Kepley and Schwartz made considerable progress towards improved basophil isolation [27]. In collaboration with C. Kepley, L. Youssef refined the original protocols to establish a 3-step process in which basophils are first enriched from peripheral blood by Percoll gradient centrifugation (to 10–55% purity) followed by negative selection (to > 95% purity) using magnetic beads and flow sorting to > 99% purity. The current protocol is described in multiple publications [28–30] and is shown schematically in Fig. (1). Basophil yields from 120 ml blood typically range from 500,000 to 2 million highly purified cells, a substantial improvement over previous protocols and a major advance for studies on basophil protein levels, gene expression and signaling to physiological responses.
Fig. 1.
Schematic view of basophil isolation. Details are in [28].
BASOPHIL NUMBERS AND BASOPHIL “RELEASI-BILITY” ARE BOTH HIGHER IN ASTHMATIC THAN NON-ASTHMATIC DONORS
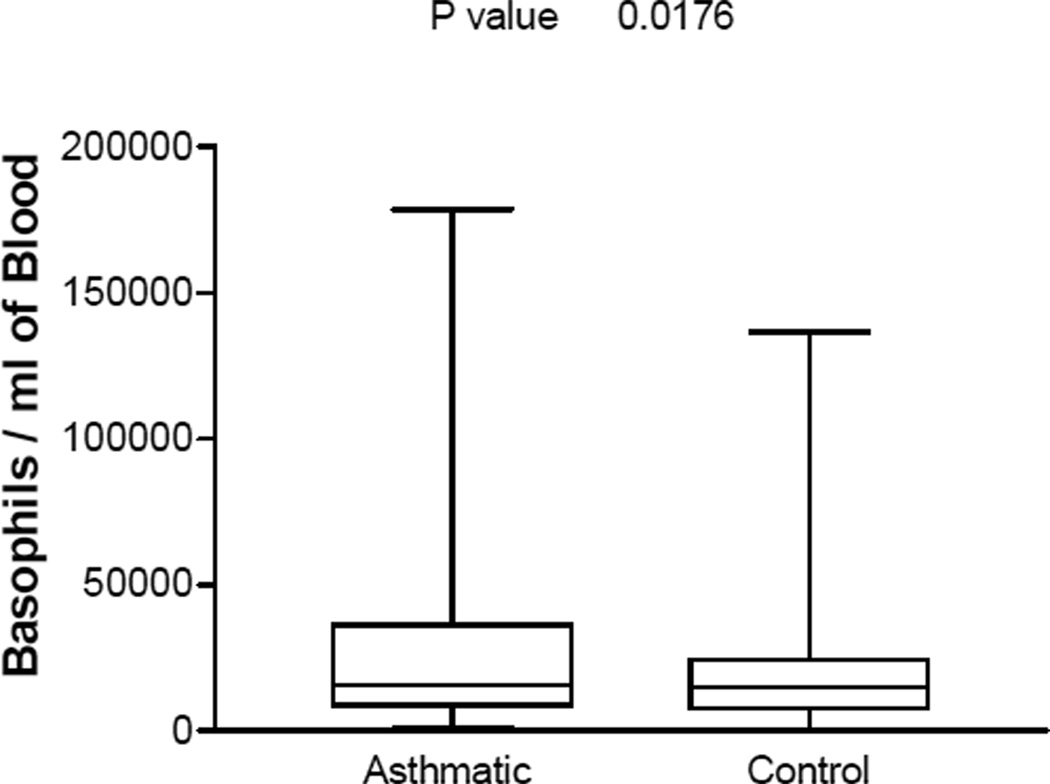
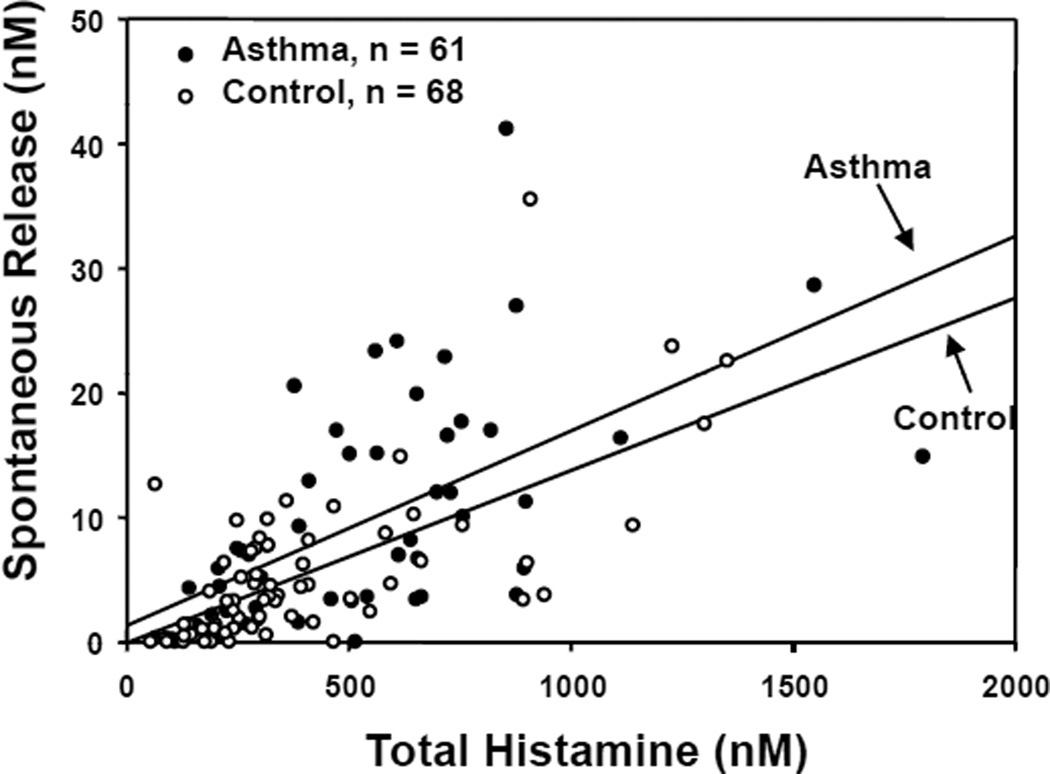
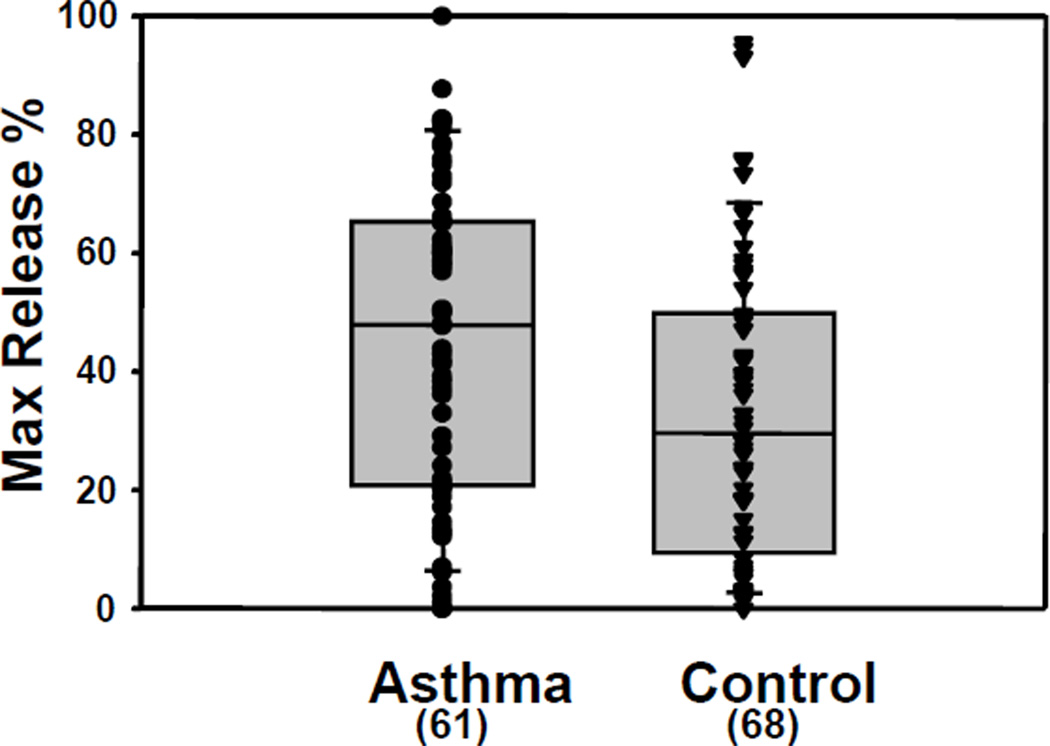
We generated basophils 2–3 times a week over 10 years. Basophils were counted and assays of total histamine content and of anti-IgE-stimulated histamine release were performed on the Percoll-enriched cells of every preparation. Review of these extensive data sets after the first 5 years established that circulating basophil numbers are statistically higher in blood from asthmatic donors than in blood from controls [30] (Fig. 2). Review additionally showed that the total amount of histamine is the same between the basophils of control and asthmatic donors, but both spontaneous (Fig. 3) and anti-IgE-stimulated (Fig. 4) histamine release is higher in the asthmatic group [26]. Although the differences are not huge, both the higher numbers of circulating basophils in asthmatics and the greater “releasibility” of these cells provided more support for a direct role for basophils in asthma.
Fig. 2.
Comparison of the numbers of basophils recovered from the blood of asthmatics and controls. Details are in [30].
Fig. 3.
Relationship between total histamine in basophils and spontaneous histamine release. Total histamine was the same in basophils from asthmatic and control donors (t test, p= 0.053), but spontaneous histamine release was higher in the asthmatic group (p = 0.008). Details are in [26].
Fig. 4.
Higher anti-IgE-induced histamine release from the basophils of asthmatic donors. Stimulated histamine release was higher in the asthmatic group (p= 0.02). Details are in [26].
We found that basophils from some donors fail to release histamine in response to FcεRI signaling even though their basophils express the receptor, contain a normal complement of histamine and indeed degranulate in response to other signals, including the calcium ionophores, ionomycin and A23178, and fMLP, a ligand for the G-protein coupled formyl peptide receptor that is expressed on human basophils [31]. Review of longitudinal data on the “non-releaser” basophils revealed two striking results [26]. First, basophils from some donors can cycle between the releaser and non-releaser phenotypes. Second, the non-releaser phenotype is much less often found in basophils from asthmatics than in control basophils. The rarity of “non-releaser” basophils in asthmatics again supports a connection between basophil physiology and the presence or absence of disease.
ESTABLISHING THE BASICS OF FcεRI SIGNALING IN HUMAN BASOPHILS
When we began our studies in 1996, the pathways linking FcεRI crosslinking to secretion were not yet defined. Thus, our initial mechanistic studies focused simply on the first steps in basophil signaling induced by crosslinking endogenous IgE-FcεRI complexes with polyclonal human anti-IgE or, alternatively, by loading unbound FcεRI with murine anti-DNP IgE and crosslinking with polyvalent DNP-BSA. Given our pioneering role in defining murine mast cell signaling through the FcεRI [eg. 32–35], it was straightforward to show that crosslinking the human basophil receptor led to the tyrosine phosphorylation of two key tyrosine kinases, Lyn and Syk, previously implicated in murine mast cell signaling and to establish that signaling to histamine release was abolished by the Syk-selective inhibitor, piceatannol [36]. In contrast to murine cells, highly purified human basophils also express low levels of the tyrosine kinase, Zap70, found previously only in T cells. The significance of basophil Zap70 remains to be determined [32].
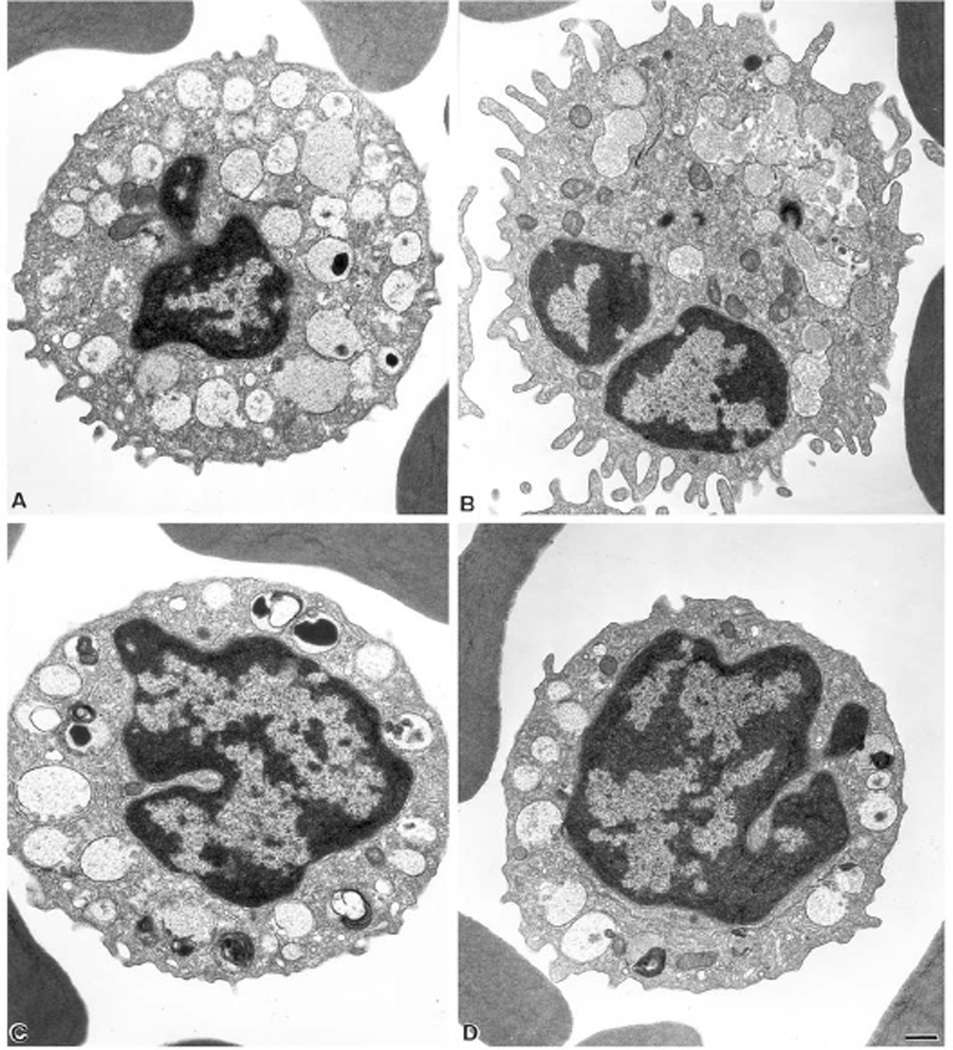
Further analysis revealed a series of other signaling responses to human basophil Fcε RI crosslinking. Immediate responses (occurring within minutes of stimulation) included a dramatic ruffling response [26] (Fig. 5A,B), linked to F-actin assembly as well as an increase in VLA4-mediated adhesive activity revealed first in a flow cytometry-based assay of conjugate formation between basophils and VCAM-transfected CHO cells [37] and later confirmed via an elegant assay for VLA4 affinity changes based on the binding of a fluorescent LDV peptide [38]. Both responses are expected to contribute to allergen-stimulated tissue invasion.
Fig. 5.
Ultrastructure of resting and activated releaser and non-releaser basophils. Releaser (A,B) and non-releaser (C,D) basophils were incubated without (A,C) and with (B,D) 1 µg/ml of anti-IgE for 30 miniutes, then washed and processed for electron microscopy as in [26]. Resting cells (A and C) show very similar membrane and granule morphologies. In releaser cells (B), FcεRI crosslinking induces granule-granule fusion, degranulation and membrane ruffling. Non-releaser cells (D) show little morphological changes following FcεRI crosslinking. Bar = 0.5 µm. Details are in [28].
Later responses to FcεRI crosslinking include the synthesis of well-known basophil cytokines and chemokines such as IL-4 and IL-13, and less well known products, including MIP-5, eotaxin, GM-CSF, IL-8, RANTES, MIP-1α, MIP-1p and Leptin [30, 39]. Basophils used in our studies of mediator production were stimulated immediately after isolation and were never pre-treated with IL-3, a manipulation used commonly by other groups to amplify basophil signaling to cytokine and chemokine production. Results were generated and validated using ELISA assays, Cartesian array assays and Luminex bead-based assays, often with RT-PCR verification [26, 30, 39]. They clearly support conclusions from studies in murine models that basophils may be a substantial source of Th2 cytokines implicated in propagating the allergic phenotype. The further implications of this cocktail of basophil protein products remains to be determined. We find the discovery of antigen-induced Leptin production [30] to be particularly provocative, given recent evidence that basophils can promote angiogenesis and that Leptin has proangiogenic properties.
We failed to demonstrate differences between basophils from asthmatic and non-asthmatic donors in cytokine or chemokine production. However, mediator production was surveyed in many fewer cases than histamine release, so that small differences would likely have been undetectable.
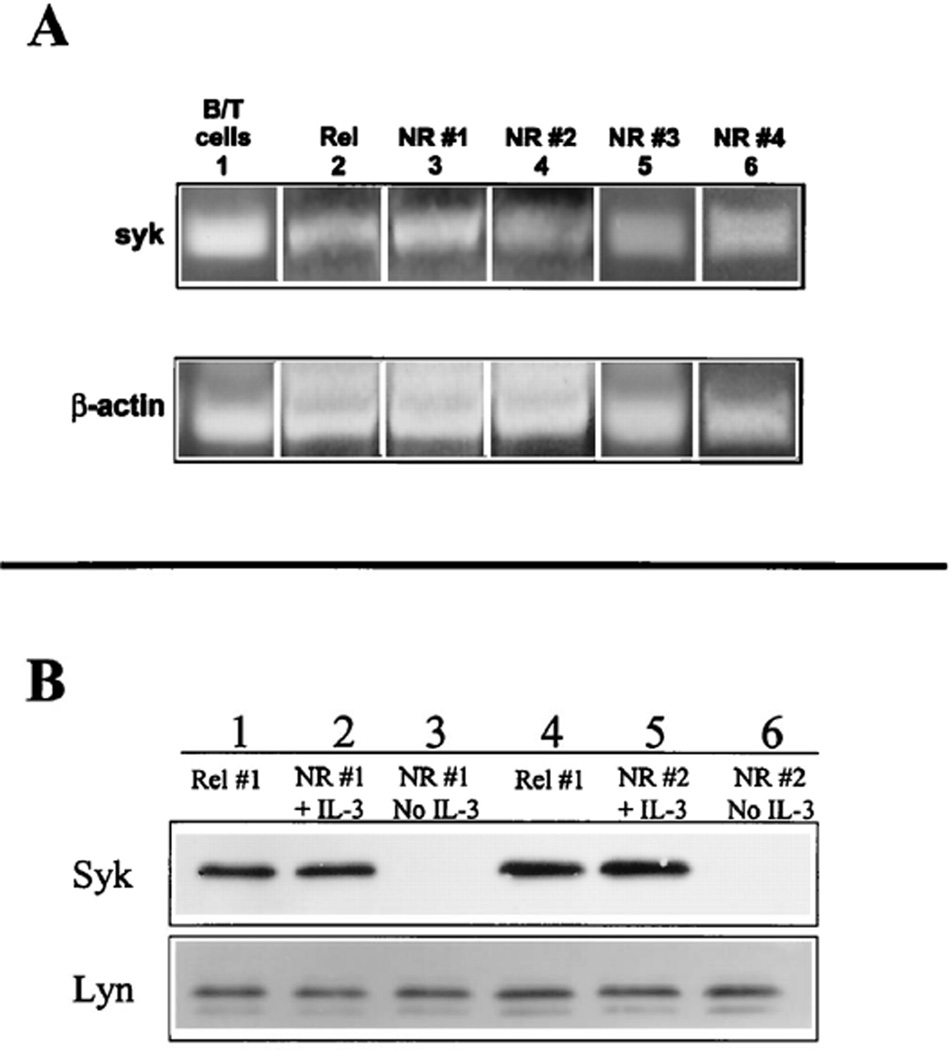
CHARACTERIZING NON-RELEASER BASOPHILS
We noted above the existence of donors, mainly in the non-atopic, non-asthmatic group, whose basophils fail to release histamine in response to FcεRI crosslinking [31]. Further studies revealed that these basophils also fail to ruffle (Fig. 5C,D), to upregulate VLA-4 avidity and affinity and to synthesize and release cytokines following allergen stimulation [28]. Western blotting provided an unexpected explanation. Donors with non-releaser basophils lack basophil Syk [28, 31]. In contrast their B cells and other leukocytes have normal Syk levels, suggesting a basophil-specific regulatory mechanism with potential for therapeutic applications in asthma and allergic inflammation [31]. Continued studies showed that the abnormality in Syk expression in non-releaser basophils is regulated at the post-transcriptional level. First, Syk mRNA appears to exist at normal levels in non-releaser basophils (Fig. 6A). Furthermore, Syk protein can be restored both by 3–4 day incubation of non-releaser basophils with IL-3 (Fig. 6B) [26] or by short-term incubation with a cell-permeable proteasome inhibitor [29]. It thus appears that Syk is destroyed in basophils from some donors via a ubiquitin-proteasomal-mediated pathway that is not active in other leukocytes. This pathway is likely activated in response to changes in the cytokine milieu, possibly linked in part to IL-3 (because IL-3 levels needed to stabilize Syk are high and we failed to show differences between donors with releaser and non-releaser basophils in serum IL-3 levels, we doubt this is the full story). Given the good health of our non-releaser donors, we inferred that basophil Syk deficiency is most likely harmless in humans.
Fig. 6.
Non-releaser basophils contain Syk mRNA but lack Syk protein. In A, RNA from purified basophils was transcribed into cDNA and PCR was performed with Syk-specific primers. A mixture of B and T cells served as a positive control. mRNA for Syk was detected in all samples. In B, Western blotting for Syk was performed before and after incubation of purified non-releaser basophils for 3 days with IL-3. Releaser basophils were used as a positive control. Syk protein was missing from the untreated non-releaser basophils and was substantially restored after incubation with IL-3. Details are in [28].
Mechanisms responsible for the differential regulation of Syk stability in basophils in comparison with other leukocyte populations remain unknown. A clue exists in the discovery of an acridone-related compound, ER-27319, that specifically blocks FcεRI-coupled Syk activation in human mast cells without affecting anti-IgM-induced activation of Syk in human peripheral B cells [40]. This observation suggests that cell type-specific Syk-receptor interactions may differentially determine the activation and perhaps the fate of Syk protein. The possibility of exploiting this vulnerability for therapy is discussed below.
GENE EXPRESSION IN HUMAN BASOPHILS: FcεRI CROSSLINKING MAY ACTIVATE MULTIPLE SIGNALING PATHWAYS
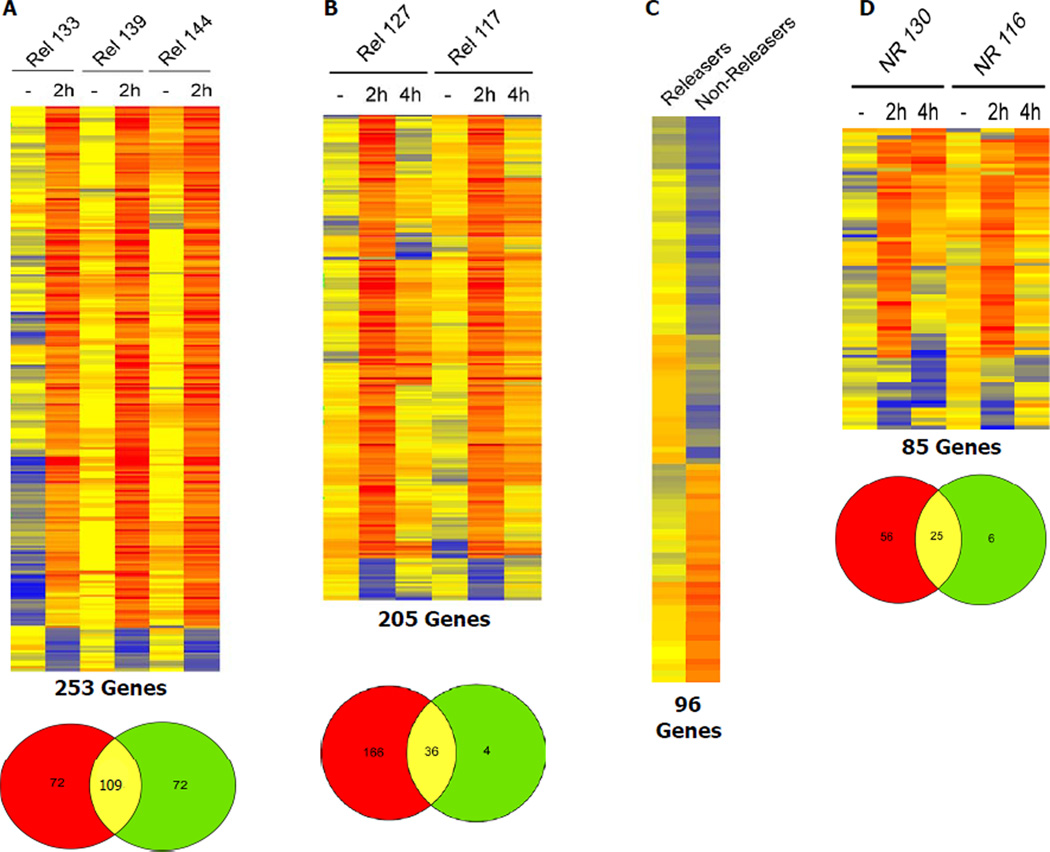
Due to the multitude of basophil responses to antigen stimulation, it was expected that gene expression would be substantially altered in response to basophil FcεRI crosslinking. Microarray analysis of basophil gene expression presented technical difficulties due to the scarcity of cells and their high concentrations of stored proteoglycans that complicate mRNA preparation. Nevertheless, from nanogram amounts of basophil RNA, we established a two round RNA amplification procedure via in vitro transcription to generate high quality labeled complementary RNA (cRNA) targets for hybridization. Our studies using Affymetrix GeneChip technology (Fig. 7A,B) revealed that FcεRI cross-linking in releaser basophils up-regulates more than 200 genes, including genes encoding angiogenic ligands (VEGF), signaling receptors (the FcεRI α and β subunits, the histamine 4 receptor, the chemokine (C-C motif) receptor 1), protein and lipid kinases implicated in multiple signaling pathways (Lyn, PI 3-kinase), transcription factors implicated in signal pathway responses (early growth response-1, early growth response-3, and AP-1) and chemokines (IL-8, RANTES, MIP-1α, MIP-1β) that may act in autocrine fashion to enhance the initial stimulus [26].
Fig. 7.
Heat map and Venn diagram representation of gene expression in resting and activated releaser and non-releaser basophils. The four heat maps represent genes that were up or down regulated by 2 fold or greater in four separate experiments. Each row represents 1 gene, each column one stimulus. A color scale represents the expression ratios. Map A) represents 253 genes that were differentially expressed in releaser basophils from 3 different donors in response to FcεRI crosslinking. Map B) represents 205 genes that were differentially expressed in releaser basophils from 2 different donors in response to FcεRI crosslinking with medium exchange after 30 minutes of activation. Map C) displays 96 genes that were differentially expressed between unstimulated releaser (5 donors) and nonreleaser (2 donors) basophils. Map D) represents the gene expression profile of nonreleaser basophils from 2 different donors in response to FcεRI crosslinking. The Venn representation of filtering results indicates numbers of genes identified as 2 fold or greater up or down regulated only when using the basic filter (red), only when using the Anova incorporating filter (green) and when using both filters (overlap). Details are in [26].
Gene expression for heat-shock proteins (HSPs) [26] was also prominently observed in the antigen-activated basophils and could be reduced by washing away the products of initial degranulation after 30 minutes of stimulation, then adding fresh stimulus and continuing the incubation to 2 or 4 hours. These results suggest a feedback loop in which a first wave of released mediators activates additional signaling pathways that may determine the fate of activated basophils. In particular, the enhanced expression of heat shock proteins may regulate the lifespan of activated basophils by accelerating or decelerating apoptosis. Conversely, histamine which is known for its proinflammatory, antiapoptotic and immunosuppressive capabilities, could inhibit the further release of mediators from human basophils through the engagement of the H2 receptor [41].
Gene expression patterns observed with and without washing away the products of initial degranulation may both reflect in vivo conditions. Activation of circulating blood basophils would be expected to generate mediators which get readily diluted in the blood stream, resulting in systemic (i.e., anaphylaxis) rather than local effects. The same induction event in tissue-recruited basophils may generate mediators that are less diffusible and may preferentially act in an autocrine fashion to amplify changes in basophil gene expression. For example basophil activation after the cells have infiltrated sites of allergic airway inflammation [42, 43] could favor an extended exposure of basophils and their neighboring cells to a high concentration of proinflammatory and angiogenic substances. VEGF is of obvious interest due to its pro-angiogenic properties.
It is noteworthy that activation of basophils up-regulates the expression of genes for CD83, a costimulatory molecule in antigen presentation and a surface marker that differentiates immature and mature human dendritic cell (DC) populations and B cells. If this increase of CD83 expression in basophils is confirmed at the protein level, it would support the evolving role of basophils as APCs in murine models. We observed that medium exchange after 30 minutes of basophil activation abolished CD83 upregulation. We therefore speculate that CD83 expression is induced by autocrine signaling not via the FcεRI receptor per se.
We were unable to distinguish between patterns of gene expression induced by the activation of release basophils from control and asthmatic subjects. As already noted for mediator production, gene expression was measured in many fewer cases than histamine release, so that small differences would likely have been undetectable.
However, we were easily able to distinguish between the gene expression profiles of donors with releaser and non-releaser basophils (Fig. 7C,D). FcεRI cross-linking induced fewer and quite distinct transcriptional responses in non-releaser cells. In particular, no chemokines or cytokines were found among the up-regulated genes in activated non-releaser basophils [26]. It thus seemed likely that interventions that favor the non-releaser phenotype should prove beneficial for the treatment of allergic asthma (see below).
TOWARDS NEW RATIONALLY DESIGNED THERAPEUTICS TARGETING BASOPHILS DOWN-REGULATING FcεRI SIGNALING BY CROSSLINK-ING TO FCTRIIB
Signaling through members of the multichain immune recognition receptor family, which includes the B-cell antigen receptor (BCR), the T-cell antigen receptor (TCR), the high-affinity IgE receptor (FcεR1), and the FcγR1 and FcγRIII classes of IgG receptors, is mediated by immunoreceptor tyrosine–based activation motifs (ITAMs) within receptor subunit cytoplasmic tails. ITAMs are 26- to 27-amino acid sequences consisting of dual YXXL sequences separated by approximately 10 amino acids. Receptor activation leads to tyrosine phosphorylation of ITAMs by Src kinase family members, including Lyn, creating binding sites for the tandem SH2 domains of Syk family members and initiating downstream signaling events. A related motif that transmits negative signals, the immunoreceptor tyrosine-based inhibitory motif (ITIM), was identified first in FcγRIIB and subsequently in a series of immune system receptors. The inhibitory function of ITIMs is generally attributed to the ability of phospho-ITIMs to recruit SH2 domain–containing phosphatases, particularly the protein tyrosine phosphatases SHP-1 and SHP-2, and the SH2 domain–containing poly-phosphatidlyinositol 5-phosphatase (SHIP) [44].
We showed by flow cytometry that human basophils express FcγRII (CD32) but not FcγRI (CD64) or FcγRIII (CD16) [45]. Subsequent RT-PCR studies established that basophil FcγRII includes both the ITIM-containing FcγRIIB and the ITAM-containing FcγRIIA forms. Despite the presence of mRNA for FcγRIIA, we demonstrated negative signaling between FcγRII and FcεRI in these cells. In the initial studies, FcεRI were primed with anti-DNP IgE, FcγRII were primed with anti-DNP IgG and crosslinking was induced with polyvalent DNP-BSA. Under co-crosslinking conditions, Syk phosphorylation and calcium mobilization were markedly impaired and signaling to secretion and IL-4 production were both reduced by approximately 40%. The results of Western blot analysis established that human basophils express all 3 phosphatases previously implicated in negative signaling: SHP-1, SHP-2, and SHIP. Further studies showed that SHP-1 is translocated from the cytosolic to membrane fractions of basophils during FcεR1 and FcγRII costimulation, and also that the synthetic phosphorylated, but not non-phosphorylated, FcγRIIB ITIM sequence recruits SHP-1 from basophil lysates. All of these data supported the hypothesis that new therapeutics inducing the co-crosslinking of FcεR1 and FcγRIIB on basophils might have efficacy against allergic inflammatory diseases.
Continued studies by C. Kepley in collaboration with A. Saxon have supported the initial promise of FcεR1-FcγRIIB co-crosslinking as a potential therapeutic strategy [46]. The Saxon lab engineered a new protein, GE2, consisting of a human Fcγ heavy chain linked to a Fcε heavy chain. GE2 protein was shown to inhibit degranulation from both cord blood-derived human mast cells and peripheral blood basophils. The inhibition was accompanied by reduced Syk phosphorylation and reduced calcium mobilization. In vivo, GE2 was found to block passive cutaneous anaphylaxis (PCA) driven by human IgE in mice expressing the human FcεR1 and to inhibit skin test reactivity to dust mite allergen in a dose-dependent manner in rhesus monkeys. In recent work, optimization of GE2 as an inhibitor of FcεRI-mediated functions showed that effectiveness was maintained when potentially immunogenic linker sequences were removed and Ig domain positions were reversed [47].
Aside from immunogenicity, a potential complexity of the hybrid Fcγ-Fcε molecule is that high affinity Fc binding stabilizes receptors at the cell surface, so that the therapeutic may potentially upregulate receptor expression. Perhaps to avoid this, Saxon and colleagues now report genetically engineered chimeric human Fcγ-allergen proteins, with Fcγ– Fel d1 (the cat allergen) as the prototype, as alternative reagents [48]. In these hybrid molecules, the allergen portion binds to specific IgE on FcεRs, while the Fcγ portion coaggregates inhibitory FcγRIIB and drives inhibition of allergic reactivity. These new molecules are likely to have other advantages, including a better match of binding affinities for FcγRIIB and for IgE-FcεR1, as well as better specificity for particular allergies.
DOWNREGULATING FcεRI SIGNALING BY UNCOUPLING SYK
As noted above, our analysis of non-releaser basophils revealed a basophil-specific regulation of Syk. Non-releaser basophils express normal levels of FcεRI and show normal Ca2+ mobilization, secretion and cytokine synthesis responses to Ca2+ ionophore, phorbol ester and formyl peptide, all stimuli that bypass the FcεRI [28,31]. However they have vanishingly low levels of basophil Syk, even though B cell, eosinophil and neutrophil Syk levels are normal. Importantly, the deficit is reversible [28]. The basophils of many normal subjects cycle between the releaser and non-releaser phenotype, accompanied by the gain or loss of Syk protein expression. As already noted, incubation of non-releaser basophils for 3 days with IL-3 results in a partial recovery of Syk expression and FcεR1-mediated histamine release. Syk protein expression is also restored by brief incubation of non-releaser basophils with cell-permeable proteasome inhibitors.
Because Syk plays critical roles in antibody production, adhesion signaling, the maintenance of endothelial intergrity and other processes, there are some obvious complexities to using generalized Syk inhibitors for therapy. On the other hand, it may be straightforward to screen drug libraries for small molecules that target the specific interaction of Syk with the phosphorylated ITAMs of FcεRIy. Inhibition of the FcεRIγ-Syk interaction is predicted to generate a basophil-specific deficiency similar to the non-releaser phenotype that appears to be protective against allergic asthma. We realize that the drug we seek would potentially interfere with functions of the high affinity IgG receptor, FcγRI, and the IgA receptor, FcαRI, that signal though the same γ subunit [42].
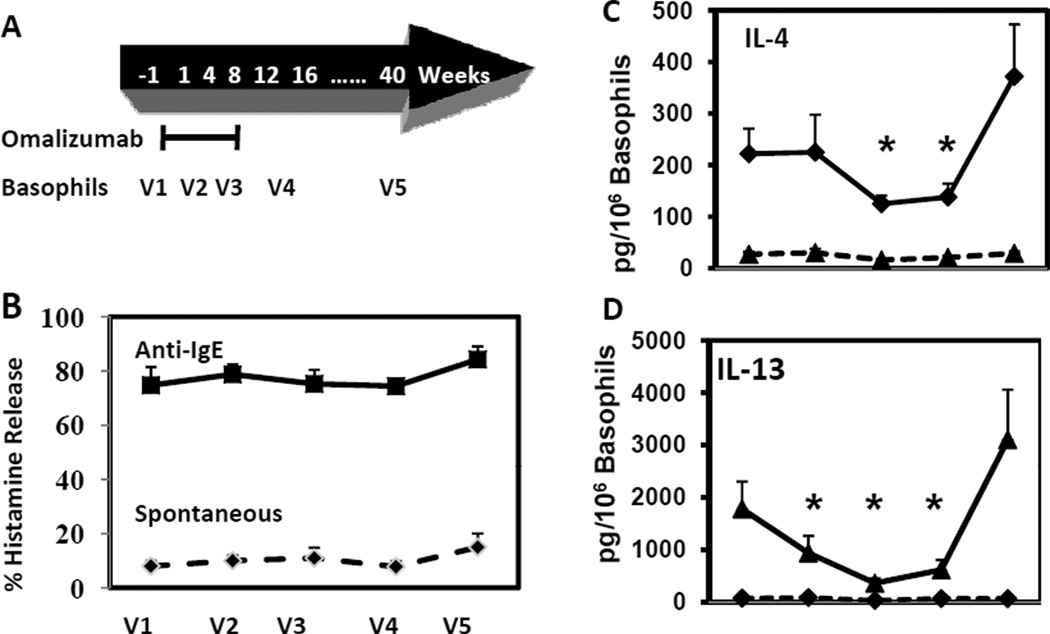
DOWNREGULATING FcεRI SIGNALING BY DESTABILIZING RECEPTOR
A third obvious route to downregulating basophil FcεRI signaling is to reduce cell surface receptor levels below some threshold needed for effective basophil (and mast cell) activation. In course of our 10 year study of basophil signaling, we undertook a long-term study of basophil responses to treatment of asthmatic subjects with Omalizumab, a humanized mAb that scavenges circulating IgE by binding to its Fc (FcsRI-binding) domain. Omalizumab has been shown to be useful in many asthmatics, especially in controlling exacerbations of asthma leading to repeated hospitalization [50,51]. Its effect on basophils was first studied in the mid-1990s in the MacGlashan group, resulting in the striking discovery that depleting circulating IgE causes a rapid and reversible loss of basophil FcεRI expression and that the loss of receptors results at least in part from accelerated receptor turnover [18,19,52]. We conducted an independent trial in which 12 asthmatics were studied before, during, immediately after and six months after a 12 week course with Omalizumab (Fig. 8A). We confirmed that scavenging circulating IgE with Omalizumab causes a more than 95% loss of basophil FcεRI expression in intermittent asthmatics. Receptor levels recovered fully after Omalizumab withdrawal [39].
Fig. 8.
Effects of Omalizumab on anti-IgE-mediated histamine release and IL-4 and IL-13 production. Basophils were isolated from 9 volunteers before, during and 6 months after a 12-week course of Omalizumab. Cells were incubated for 30 min (HR) or 4 hours (cytokine production) without (dashed lines) and with (solid lines) anti-IgE. There was no significant effect of Omalizumab on anti-IgE-stimulated histamine relase. In contrast, Omalizumab significantly decreased ani-IgE-stimulated cytokine production. Asterisks mark specific time-points when paired t tests yielded p<0.05 in comparison with pre- and post-treatment values. Details are in [39].
Under the conditions used in our study, histamine release induced by crosslinking all remaining cell surface IgE-FcεRI with polyclonal anti-IgE Ab was not reduced over the course of Omalizumab treatment and withdrawal (Fig. 8B). On the other hand, the results of ELISA assays for basal and antigen-mediated production of IL-4 and IL-13 revealed a rapid and reversible loss of FcεRI-mediated cytokine production during Omalizumab treatment. As shown in Fig. 8C,D), IL-4 production was reduced to less than 50% of pre- Omalizumab, while IL-13 production was reduced to only 20% of pre-Omalizumab levels. IL-8 production was also reduced to less than 50% of pre-Omalizumab levels. These results suggest that Omalizumab may prevent the exacerbation of asthma in part by reducing basophil Th2 cytokine production. We note that although anti-IgE-mediated histamine releae was not impaired, it is very likely that degranulation induced by specific allergen, expected to target only a subset of the remaining IgE-receptor complexes, would have been reduced as reported by the MacGlashan group.
Omalizumab, marketed as Xolair®, is administered by injection and costs around $20,000 per year. Furthermore, a small number of recipients have had anaphylactic responses, leading in July, 2007, to a FDA-issued safety warning. All of these negative factors encourage further work to identify therapeutics that might block high affinity IgE binding and mimic the Omalizumab-mediated destabilization of FcεRI without the high cost, inconvenience and risk of a whole antibody therapeutic. One approach is to search for small molecules that mimic Omalizumab’s ability to block the Fc (receptor-binding) portion of circulating IgE. Another approach, based on evidence that the dimeric and symmetrical Fc fragment of IgE achieves high affinity binding through its sequential interaction with two asymmetrical sites on the FcεRI α subunit, accompanied by marked conformational changes in the IgE [53], is to find small molecules that block one of the two IgE binding sites on the FcεRI α subunit without simultaneously stabilizing the receptor.
COULD BASOPHILS ALSO PROTECT AGAINST ALLERGIC INFLAMMATION?
All of the work summarized above is consistent with the hypothesis that IgE-primed, allergen-exposed basophils are well-equipped to participate in human allergic asthma as both initiators and promoters of symptomatic illness. Our work extends previous results by providing substantially more molecular detail to the analysis and, importantly, some specific targets for therapy.
To the best of our knowledge, the possibility that basophils, specifically in the absence of allergen, could play a protective role against allergic inflammation has not been considered. The rationale for this possibility is as follows. IgE binds to the FcεRI of basophils and mast cells with extremely high affinity (Kd around 10γεα−10 M), resulting in an estimated half-life of the IgE-FcεRI complex in vivo of 10 days or more. IgE binding to the basophil FcεRI stabilizes receptor and leads very rapidly to very high levels of receptor expression – perhaps up to 500,000 receptors per cell, almost all engaging IgE. Asthmatics express not only high receptor levels, but also high numbers of circulating basophils (if not in absolute numbers, at least relative to non-asthmatics). The half-lives of circulating basophils are thought to be relatively brief - from as short as 6 hours to perhaps 3 days. The fate of circulating basophils is thought to be death by apoptosis, either immediately or after extravasation to tissue where continued survival is likely variable, depending on the cytokine milieu in the tissue [54].
Given this set of properties, we hypothesize that the entry of basophils into the circulation will lower serum IgE levels, while their death by apoptosis and subsequent destruction by scavenging monocytes and macrophages will reduce the half-life of the IgE-FcεRI complex. From this perspective, the upregulation of basophil numbers and receptor densities in asthmatics could be protective, rather than harmful, to the patient. It follows that short-term treatments that upregulate basophil FcεRI levels could be an alternative to Omalizumab as a means to clear circulating IgE. The danger for the patient is that allergen needs to be excluded while the therapy proceeds.
SUMMARY
Basophils, long considered little more than a surrogate for mast cells, have started to gain a distinct position in the pathophysiology of allergic hypersensitivity, including asthma, and more generally in the immune response. Recent studies in murine systems provided compelling evidence for the importance of basophils in both the initiation and propagation of allergic inflammatory diseases. Our evidence that human basophils are more active in asthmatics than controls, having statistically higher circulating numbers, higher basal and antigen-stimulated histamine release and a much lower incidence of the non-releaser phenotype, supports other evidence that basophils may contribute directly to allergic inflammatory disease, including asthma.
In addition studies of human basophil signaling have revealed targets for therapy that could not be inferred from studies in mice. For example, there is no evidence as yet that murine basophils can selectively degrade Syk like human non-releaser basophils or modulate receptor levels over a >100-fold range like the basophils of asthmatics in response to Omalizumab. The increased accessibility of new multiplexed molecular screening technologies should accelerate the discovery of small molecules with specificity for the human IgE-FcsRIα interaction or for the human Syk-FcεRIγ interaction. New advances in protein engineering should make it easier to design hybrid molecules that crosslink basophil FcsRIα and FcγRII, also reducing basophil responsiveness to allergen.
Further studies on the regulation of human basophil FcεRI levels and survival are also needed. Circulating human basophils upregulate FcεRI levels in response to increased levels of serum IgE. They also have rather short half-lives in the circulation. Thus, in the absence of allergen they could play an entirely new role as scavengers of IgE and therefore protectors against allergy and asthma.
Perhaps both scenarios are possible in asthma - in the absence of allergen, circulating basophils could be protective by sequestering IgE that would otherwise sensitize lung mast cells, whereas they may promote symptomatic disease after their recruitment into the lungs or following allergen escape into the circulation. We urge continued support for research on FcsεRI expression and function in primary human basophils in order to better understand and treat human asthma and other allergic diseases.
ACKNOWLEDGEMENTS
Funding for this work came from NIH Grants P50-HL58364 (University of New Mexico Asthma Specialized Center of Research) and 5MO1 RR0997 (University of New Mexico General Clinical Research Center). We thank our colleagues in the UNM Asthma SCOR program, especially M. Lipscomb, as well as the many talented students, post-docs and staff, including C. Kepley, R. Andrews, L. Gilmartin, J. Pfeiffer, C. Tarleton, A. Chigaev, M. Martinez, J. Pfeiffer, D. Brown and T. Archibeque, who contributed to the project.
REFERENCES
- 1.Summary Health Statistics for U.S. Adults: National Health Interview Survey. 2008 Tables 3 and 4. http://www.cdc.gov/nchs/data/series/sr_10/sr10_242.pdf. [PubMed]
- 2.Summary Health Statistics for U.S. Children: National Health Interview Survey. 2008 Table 1. http://www.cdc.gov/nchs/data/series/sr_10/sr10_244.pdf. [PubMed]
- 3.Masoli M, Fabian D, Holt S, Beasley R. Global Initiative for Asthma (GINA) program: the global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy. 2004;59:469–478. doi: 10.1111/j.1398-9995.2004.00526.x. [DOI] [PubMed] [Google Scholar]
- 4.Osler W. The principles and practice of medicine. New York: D Appleton and Company; 1892. [Google Scholar]
- 5.Ehrlich P. Beiträge zur Theorie und Praxis der histologischen Färbung. Dissertation at Leipzig University; 1878. [Google Scholar]
- 6.Ehrlich P. Beitrage zur Kenntnis der gra-nulierten Bindegewebszellen und der eosino-philen Leukocyten. Arch Anat Physiol(Physiol Abt) 1879;3:166. [Google Scholar]
- 7.Kraft S, Kinet J-P. New developments in FcεRI regulation, function and inhibition. Nat Rev Immunol. 2007;7:365–378. doi: 10.1038/nri2072. [DOI] [PubMed] [Google Scholar]
- 8.Liu MC, Hubbard WC, Proud D, et al. Immediate and late inflammatory responses to ragweed antigen challenge of the peripheral airways in allergic asthmatics: cellular, mediator, and permeability changes. Am Rev Respir Dis. 1991;144:51–58. doi: 10.1164/ajrccm/144.1.51. [DOI] [PubMed] [Google Scholar]
- 9.Guo CB, Liu MC, Galli SJ, Bochner BS, Kagey-Sobotka A, Lichtenstein LM. Identification of IgE-bearing cells in the latephase response to antigen in the lung as basophils. Am J Respir Cell Mol Biol. 1994;10:384–390. doi: 10.1165/ajrcmb.10.4.7510984. [DOI] [PubMed] [Google Scholar]
- 10.Koshino T, Arai Y, Miyamoto Y, et al. Airway basopil and mast cell density in patients with bronchial asthma: Relationship to bronchial hyperresponsiveness. J Asthma. 1996;33:89–95. doi: 10.3109/02770909609054536. [DOI] [PubMed] [Google Scholar]
- 11.Murakami K, Sato S, Nagasawa S, Yamashita T. Regulation of mast cell signaling through high-affinity IgE receptor by CD45 protein tyrosine phosphatase. Int Immunol. 2000;12:169–176. doi: 10.1093/intimm/12.2.169. [DOI] [PubMed] [Google Scholar]
- 12.Tanizaki Y, Kitani H, Okazaki M, Mifune T, Mitsnobu F, Kimura I. Changes in the proportions of bronchoalveolar lymphocytes, neutrophils and basophilic cells and the release of histamine and leukotrienes from bronchoalveolar cells in patients with steroid-dependent intractable asthma. Int Arch Allergy Appl. 1993;101:196–202. doi: 10.1159/000236519. [DOI] [PubMed] [Google Scholar]
- 13.Gibson PG, Dolovich J, Girgisgabardo A, et al. The inflammatory response in asthma exacerbation: changes in circulating eosinophils, basophils and their progenitors. Clin Exp Allergy. 1990;20:661–668. doi: 10.1111/j.1365-2222.1990.tb02705.x. [DOI] [PubMed] [Google Scholar]
- 14.Kepley CL, McFeeley PJ, Oliver JM, Lipscomb MF. Immunohistochemical detection of human basophils in postmortem cases of fatal asthma. Am J Respir Crit Care Med. 2001;164:1053–1058. doi: 10.1164/ajrccm.164.6.2102025. [DOI] [PubMed] [Google Scholar]
- 15.Brunner T, Heusser CH, Dahinden CA. Human peripheral blood basophils primed by interleukin 3 (IL-3) produce IL-4 in response to immunoglobulin E receptor stimulation. J Exp Med. 1993;177:605–611. doi: 10.1084/jem.177.3.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li H, Sim TC, Alam R. IL-13 released by and localized in human basophils. J Immunol. 1996;156:4833–4838. [PubMed] [Google Scholar]
- 17.Gauchat JF, Henchoz S, Mazzei G, et al. Induction of human IgE synthesis in B cells by mast cells and basophils. Nature. 1993;365:340–343. doi: 10.1038/365340a0. [DOI] [PubMed] [Google Scholar]
- 18.MacGlashan DW, Bochner BS, Adelman DC, et al. Down-regulation of FcεRI expression on human basophils during in vivo treatment of atopic patients with anti-IgE antibody. J Immunol. 1997;158:1438–1445. [PubMed] [Google Scholar]
- 19.Saini SS, MacGlashan DW, Sterbinsky SA, et al. Down-regulation of human basophil IgE and FcεRI surface densities mediator release by anti-IgE-infusions is reversible in vitro and in vivo. J Immunol. 1999;162:5624–5630. [PubMed] [Google Scholar]
- 20.Milgrom H, Fick RB, Su JQ, et al. Treatment of allergic asthma with monoclonal anti-IgE antibody. N Eng J Med. 1999;341:1966–1973. doi: 10.1056/NEJM199912233412603. [DOI] [PubMed] [Google Scholar]
- 21.Sokol CL, Barton GM, Farr AG, Medzhitov R. A mechanism for the initiation of allergen-induced T helper type 2 responses. Nat Immunol. 2008;9:310–318. doi: 10.1038/ni1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sokol CL, Chu NQ, Yu S, Nish SA, Laufer TM, Medzhitov R. Basophils function as antigen-presenting cells for an allergen-induced T helper type 2 response. Nat Immunol. 2009;10:713–720. doi: 10.1038/ni.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Obata K, Mukai K, Tsujimura Y, et al. Basophils are essential initiators of a novel type of chronic allergic inflammation. Blood. 2007;110:913–920. doi: 10.1182/blood-2007-01-068718. [DOI] [PubMed] [Google Scholar]
- 24.Mukai K, Matsuoka K, Taya C, et al. Basophils play a critical role in the development of IgE-mediated chronic allergic inflammation independently of T cells and mast cells. Immunity. 2005;23:191–202. doi: 10.1016/j.immuni.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 25.Denzel A, Maus UA, Rodriguez Gomez M, et al. Basophils enhance immunological memory responses. Nat Immunol. 2008;9:733–742. doi: 10.1038/ni.1621. [DOI] [PubMed] [Google Scholar]
- 26.Youssef LA, Schuyler M, Gilmartin L, et al. Histamine release from the basophils of control and asthmatic subjects and a comparison of gene expression between ‘releaser’ and ‘nonreleaser’ basophils. J Immunol. 2007;178:4584–4594. doi: 10.4049/jimmunol.178.7.4584. [DOI] [PubMed] [Google Scholar]
- 27.Kepley C, Craig S, Schwartz L. Purification of human basophils by density and size alone. J Immunol Methods. 1994;175:1–9. doi: 10.1016/0022-1759(94)90326-3. [DOI] [PubMed] [Google Scholar]
- 28.Kepley CL, Youssef L, Andrews RP, Wilson BS, Oliver JM. Multiple defects in FceRI signaling in Syk-deficient nonreleaser basophils and IL-3-induced recovery of Syk expression and secretion. J Immunol. 2000;165:5913–5920. doi: 10.4049/jimmunol.165.10.5913. [DOI] [PubMed] [Google Scholar]
- 29.Youssef LA, Wilson BS, Oliver JM. Proteasome-dependent regulation of Syk tyrosine kinase levels in human basophils. J Allergy Clin Immunol. 2002;110:366–373. doi: 10.1067/mai.2002.127562. [DOI] [PubMed] [Google Scholar]
- 30.Gilmartin L, Tarleton CA, Schuyler M, Wilson BS, Oliver JM. A comparison of inflammatory mediators released by basophils of asthmatic and control subjects in response to high-affinity IgE receptor aggregation. Int Arch Allergy Immunol. 2008;145:182–192. doi: 10.1159/000109287. [DOI] [PubMed] [Google Scholar]
- 31.Kepley CL, Youssef L, Andrews RP, Wilson BS, Oliver JM. Syk deficiency in nonreleaser basophils. J Allergy Clin Immunol. 1999;104:279–284. doi: 10.1016/s0091-6749(99)70367-2. [DOI] [PubMed] [Google Scholar]
- 32.Li W, Deanin GC, Margolis B, Schlessinger J, Oliver JM. FcεRI-mediated tyrosine phosphorylation of multiple proteins, including pholspholipase Cγ1 and the receptor αβγ2 complex in RBL-2H3 rat basophilic leukemia cells. Mol Cell Biol. 1992;12:3176–3182. doi: 10.1128/mcb.12.7.3176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oliver JM, Burg DL, Wilson BS, McLaughlin JL, Geahlen RL. Inhibition of mast cell FcεRI-mediated signalling and effector function by the Syk-selective inhibitor, piceatannol. J Biol Chem. 1994;269:29697–29703. [PubMed] [Google Scholar]
- 34.Wilson BS, Kapp N, Lee RJ, et al. Distinct functions of the FcεRIp and γ subunits in the control of FcεRI-mediated tyrosine kinase activation and signalling responses in RBL-2H3 mast cells. J Biol Chem. 1995;270:4013–4022. doi: 10.1074/jbc.270.8.4013. [DOI] [PubMed] [Google Scholar]
- 35.Ortega EM, Lara M, Lee I, et al. Lyn dissociation from phosphorylated FcεRI subunits: a new regulatory step in the FcεRI signaling cascade revealed by studies of FceRI dimer signaling activity. J Immunol. 1999;162:176–185. [PubMed] [Google Scholar]
- 36.Kepley CL, Wilson BS, Oliver JM. Identification of the Fc epsilonRI-activated tyrosine kinases Lyn, Syk, and Zap-70 in human basophils. J Allergy Clin Immunol. 1998;102:304–315. doi: 10.1016/s0091-6749(98)70100-9. [DOI] [PubMed] [Google Scholar]
- 37.Andrews RP, Kepley CL, Youssef L, Wilson BS, Oliver JM. Regulation of the very late antigen-4-mediated adhesive activity of normal and nonreleaser basophils: roles for Src, Syk, and phosphatidylinositol 3-kinase. J Leukoc Biol. 2001;70:776–782. [PubMed] [Google Scholar]
- 38.Chigaev A, Blenc A, Braaten JV, et al. Real-time analysis of the affinity regulation of α4-integrin. J Biol Chem. 2001;276:48670–4868. doi: 10.1074/jbc.M103194200. [DOI] [PubMed] [Google Scholar]
- 39.Oliver JM, Tarleton C, Gilmartin L, et al. Reduced FcεRI-mediated release of asthma-promoting cytokines and chemokines from human basophils during Omalizumab therapy. Int Arch Allergy Immunol. 2010;151:275–284. doi: 10.1159/000250436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moriya K, Rivera J, Odom S, et al. ER-27319, an acridone-related compound, inhibits release of antigen-induced allergic mediators from mast cells by selective inhibition of Fcε receptor I-mediated activation of Syk. Proc Natl Acad Sci U S A. 1997;94:12539–12544. doi: 10.1073/pnas.94.23.12539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Belon P, Cumps J, Ennis M, et al. Histamine dilutions modulate basophil activation. Inflamm Res. 2004;53:181–188. doi: 10.1007/s00011-003-1242-0. [DOI] [PubMed] [Google Scholar]
- 42.Ying S, Robinson DS, Meng Q, et al. C-C chemokines in allergeninduced late-phase cutaneous responses in atopic subjects: association of eotaxin with early 6-hour eosinophils, and of eotaxin-2 and monocyte chemoattractant protein-4 with the later 24-hour tissue eosinophilia, and relationship to basophils and other C-C chemokines (monocyte chemoattractant protein-3 and RANTES) J Immunol. 1999;163:3976–3984. [PubMed] [Google Scholar]
- 43.KleinJan A, McEuen AR, Dijkstra MD, Buckley MG, Walls AF, Fokkens WJ. Basophil and eosinophil accumulation and mast cell degranulation in the nasal mucosa of patients with hay fever after local allergen provocation. J Allergy Clin Immunol. 2000;106:677–686. doi: 10.1067/mai.2000.109621. [DOI] [PubMed] [Google Scholar]
- 44.Daeron M, Vivier E. Immunoreceptor tyrosine-based inhibition motifs. New York: Springer-Verlag, Berlin, Heidelberg; 1999. [Google Scholar]
- 45.Kepley CL, Cambier JC, Morel PA, et al. Negative regulation of FcεRI signaling by FcγRII costimulation in human blood basophils. J Allergy Clin Immunol. 2000;106:337–348. doi: 10.1067/mai.2000.107931. [DOI] [PubMed] [Google Scholar]
- 46.Zhu D, Kepley CL, Zhang M, Zhang K, Saxon A. A novel human immunoglobulin Fc gamma Fc epsilon bifunctional fusion protein inhibits Fc epsilon RI-mediated degranulation. Nat Med. 2002;8:518–521. doi: 10.1038/nm0502-518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Allen LC, Kepley CL, Saxon A, Zhang K. Modifications to an Fcgamma-Fcepsilon fusion protein alter its effectiveness in the inhibition of FcepsilonRI-mediated functions. J Allergy Clin Immunol. 2007;120:462–468. doi: 10.1016/j.jaci.2007.04.019. [DOI] [PubMed] [Google Scholar]
- 48.Zhu D, Kepley CL, Zhang K, Terada T, Yamada T, Saxon A. A chimeric human-cat fusion protein blocks cat-induced allergy. Nat Med. 2005;11:446–449. doi: 10.1038/nm1219. [DOI] [PubMed] [Google Scholar]
- 49.Wines BD, Trist HM, Ramsland PA, Hogarth PM. A common site of the Fc receptor gamma subunit interacts with the unrelated im-munoreceptors FcalphaRI and FcepsilonRI. J Biol Chem. 2006;281:17108–17113. doi: 10.1074/jbc.M601640200. [DOI] [PubMed] [Google Scholar]
- 50.Holgate ST, Djukanović R, Casale T, Bousquet J. Antiimmunoglobulin E treatment with omalizumab in allergic diseases: an update on anti-inflammatory activity and clinical efficacy. Clin Exp Allergy. 2005;35:408–416. doi: 10.1111/j.1365-2222.2005.02191.x. [DOI] [PubMed] [Google Scholar]
- 51.Fahey JV. Anti-IgE: Lessons learned from effects on airway inflammation and asthma exacerbation. J Allergy Clin Immunol. 2006;117:1230–1232. doi: 10.1016/j.jaci.2006.01.046. [DOI] [PubMed] [Google Scholar]
- 52.MacGlashan DW, Xia HZ, Schwartz LB, Gong JP. IgE-regulated loss, not IgE-regulated synthesis, controls expression of FcεRI in human basophils. J Leuk Biol. 2001;70:207–218. [PubMed] [Google Scholar]
- 53.Wan T, Beavil RL, Fabiane SM, et al. The crystal structure of IgE Fc reveals an asymmetrically bent conformation. Nat Immunol. 2002;3:681–686. doi: 10.1038/ni811. [DOI] [PubMed] [Google Scholar]
- 54.MacGlashan D. IgE and the high affinity IgE receptor, FcεRI: the IgE-CD23 interaction. In: Pawankar R, Holgate ST, Rosenwasser LJ, editors. Allergy Frontiers: Classification and Pathomechanisms. New York: Springer; 2009. pp. 43–57. [Google Scholar]
- 55.Didichenko SA, Spiegl N, Brunner T, Dahinden CA. IL-3 induces a Pim1-dependent antiapoptotic pathway in primary human baso-phils. Blood. 2008;112:3949–3958. doi: 10.1182/blood-2008-04-149419. [DOI] [PubMed] [Google Scholar]