Abstract
Background and Aims:
Aging population is a major demographic trend worldwide. Globally, 50% of all the elderly individuals are estimated to undergo atleast one surgical procedure and post-operative cognitive dysfunction (POCD) is one of the most common and often poorly understood post-operative complications in this section of the population. This randomised prospective study was conducted to assess the post-operative cognitive status in the elderly undergoing non-cardiac surgery, evaluate the cognitive parameters affected, evaluate the potential risk factors and thereby analyse the potential for implementation of preventive strategies.
Methods:
This study was conducted on 200 patients aged 60 years or older scheduled for elective non-cardiac surgeries. The baseline cognitive status of the patients was assessed 2 days prior to the date of the surgery. The post-operative cognitive status was assessed on the 3rd day, 7th day and after 1 month. Statistical analysis was performed using SAS and SPSS.
Results:
The incidence of POCD showed a gradual decline from postoperative day 3 to 30. Females were found to be at significant risk in developing POCD. Advancing age and level of education emerged as dominant factors, while type of anaesthesia, duration of surgery, and presence of coexisting comorbidities had no influence on the incidence of cognitive dysfunction.
Conclusion:
POCD is a definite complication after surgery and anaesthesia in the elderly population. Gender emerged as a significant risk factor with increasing age as a dominating factor contributing to POCD.
Keywords: Anaesthesia, cognitive function, dementia, neuroprotection, neuropsychological testing, post-operative cognitive dysfunction
INTRODUCTION
The recent advancements in medical technology and anaesthetic care have made it possible for older patients with several comorbidities to safely undergo surgery. Physiological age and chronological age seldom complement each other and the changes that accompany aging in turn influence the individual's ability to withstand stress associated with surgery and anaesthesia. However, in the elderly, central nervous system (CNS) dysfunction has been recognised as an alarming complication after cardiac and non-cardiac surgery. Post-operative CNS derangements range from post-operative cognitive dysfunction (POCD) to delirium to dementia.
Post-operative cognitive dysfunction is defined as a “more than expected” post-operative deterioration in cognitive domains, including short-term and long-term memory, mood, consciousness, and circadian rhythm.[1] The precise threshold of deterioration and the domains affected are matters of debate. POCD is diagnosed by specific neuropsychological tests, which are conducted before and after exposure to anaesthesia. The syndrome may be detected days to weeks after surgery and may also remain a permanent disorder resulting in significant functional impairment and socioeconomic burden for weeks to months after the procedure. Though pathophysiology remains obscure, many potential risk factors such as increasing age, genetic pre-disposition, and pre-existing cognitive impairment have been identified. The use of potentially neurotoxic drugs, low cerebral oxygenation and neuroinflammation are possible aetiological factors.
Majority of the POCD reports are on cardiac surgeries evidencing a significant proportion of patients that have problems with memory, attention, concentration, speed of motor and mental response, and difficulties with learning. This study was conducted to assess the cognitive performances in the elderly patients undergoing non-cardiac surgery following general anaesthesia (GA) and regional anaesthesia (RA). In particular, we analysed the cognitive parameters affected and evaluated the potential risk factors in order to consider preventive modalities and symptomatic pharmacotherapeutic interventions.
METHODS
This prospective, descriptive study was approved by the institutional ethical committee. Informed consent was obtained from all the patients. Subjects were recruited pre-operatively during the period from July 2011 to July 2013. The study was conducted employing randomised sampling technique and conformed to the CONSORT guidelines.
The subjects included were ≥60 years of age, scheduled for elective minor or major non-cardiac surgeries under GA or RA. The patients had an expected postoperative stay of 1 week and a long-term follow-up of 1 month. The exclusion criteria included refusal to provide informed consent, patients who presented mini mental state examination score of <23, patients with pre-existing cognitive dysfunction, severe auditory or visual disability, and patients with prior cardiac or neurosurgical procedures.
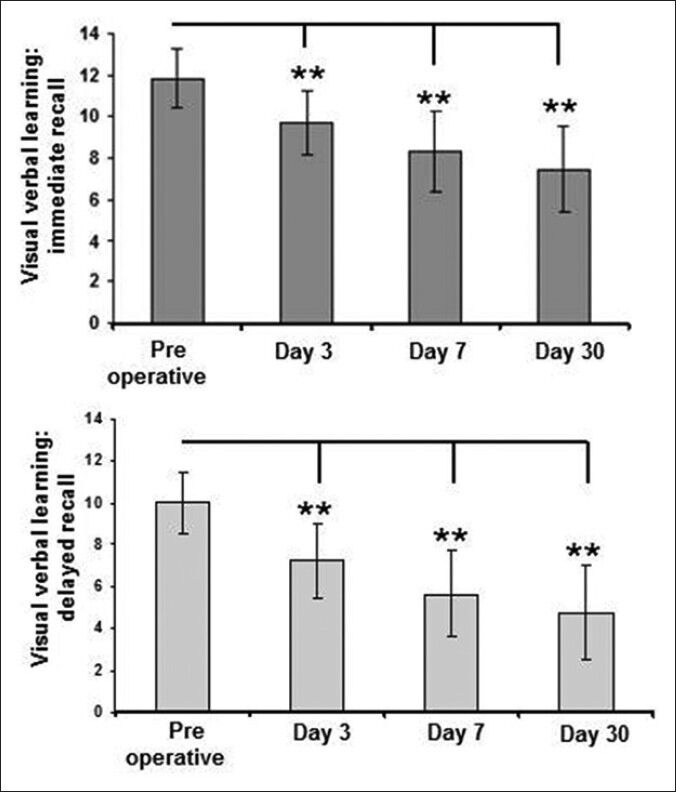
The cognitive assessment was done by using a series of neuropsychological tests as described below. Pre-operative baseline session was performed 2 days before the surgery and post-operative sessions, at days 3, 7, and 1 month after the surgery. Stroop colour word tests, selective attention, mental speed, and interference susceptibility. It involves two cards displaying 40 stimuli each; names of the colours and names of the colours are printed in incongruously coloured ink. The dependent variables are the time taken to read the colour of printing ink (Stroop colour word test-part 1) and the time taken to identify the colour name (Stroop colour word test-part 2) the errors in both parts are noted.[2]
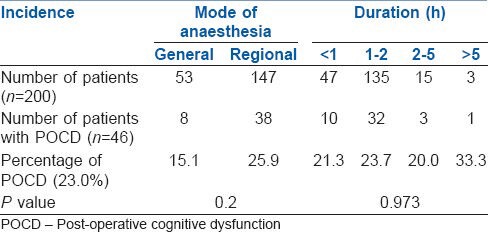
Visual verbal learning test is a visual version of a test of secondary memory. Two consecutive trials are performed in which the patient has to memorise and reproduce a list of 15 words. The dependent variable is the number of words recalled in the trials. The first part involves immediate recall after 5 min and the second part assesses delayed recall after 20 min. This exercise enables measurement of learning ability and memory retrieval, respectively.[2]
In the letter digit substitution test, the patients are supplied with a code where digit corresponds to a letter and have a minute to fill in the blanks with the correct code. This test measures the speed of processing of general information. The dependent variable is the number of correct answers in 1 min.[2]
Descriptive and inferential statistical analysis were performed using SAS 9.2, SPSS 15.0 and Stata 10.1 Student's t-test is used to find the significance of study parameters on the continuous scale within each group. Chi-square test was used to calculate the incidence of POCD. Statistical significance was accepted with P < 0.05.
RESULTS
A total of 200 patients studied showed a steady decline in POCD over time, tightly associated with gender as a predominant factor. Highly educated patients were less affected with POCD. Figure 1 shows a gradual decline of POCD incidence with 12% at day 3, 8% at day 7, and 7.5% at day 30. Analysis conducted on demographic variables [Table 1], showed that the incidence of POCD stood at 12.5 and 20.5% in the age groups ≈60 years and 61-70 years, respectively, 40.9% in the age group 71-80 years and 100% in the age group >80. Age did not emerge as a significant factor contributing to the incidence of POCD (P = 0.06), but indicated a trend. There was a significant effect on the incidence of POCD based on gender (P = 0.04); females were more prone than males. Only four patients with the level of education more than high school had POCD. There was no significant difference in the incidence of POCD in patients managed with RA over GA (P = 0.2). The duration of the surgery had no significant role (P = 0.97) [Table 2].
Figure 1.
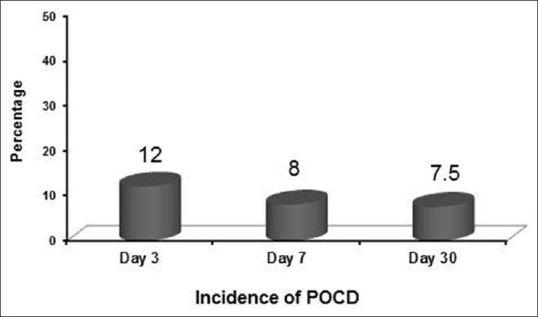
Incidence of post-operative cognitive dysfunction at different time points
Table 1.
Incidence of POCD according to demographic variables
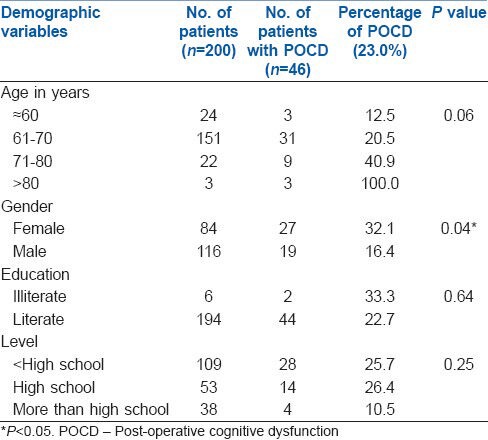
Table 2.
Incidence of POCD according to mode of anaesthesia and duration of surgery
There was no association of co-morbidities such as hypertension, diabetes mellitus, ischaemic heart disease and thyroid abnormalities with POCD (data not shown).
Learning ability and memory retrieval capacity were measured in two parts; immediate recall and delayed recall. In both scenarios, compared to the performance on the pre-operative day, visual verbal learning test was significantly reduced at days 3, 7 and 30 post-surgery [Figure 2]. Similarly, compared to performance on pre-operative day, there was a significant decline in the letter digit coding test at days 3, 7, and 30 post-surgery [Figure 3].
Figure 2.
Visual verbal learning test
Figure 3.
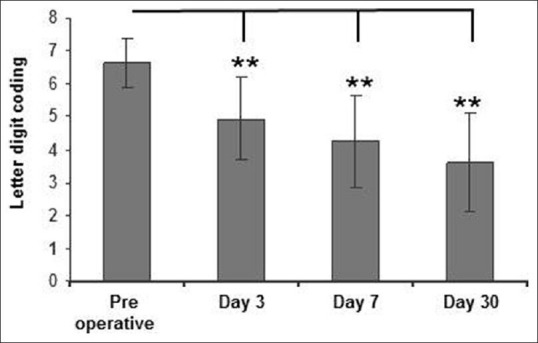
Letter digit coding test
Selective attention, mental speed and interference susceptibility areas of the cognitive domain were significantly affected as evidenced from the Stroop colour word test. The patients required more time to complete the task [Figure 4] compared to the pre-operative levels.
Figure 4.
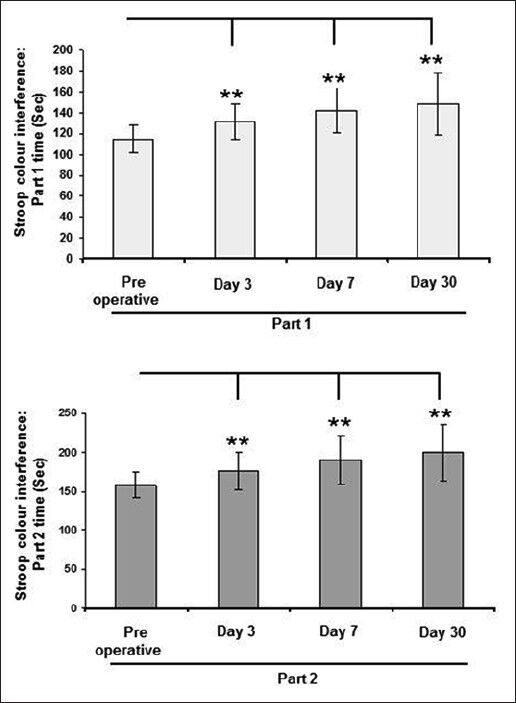
Stroop colour word test
DISCUSSION
In this study, we found that the incidence of POCD in elderly patients who underwent non-cardiac surgeries was in line with other published literature. The neuropsychological test results showed that patients who had POCD performed progressively poorer on days 3, 7, and 30 compared to baseline performance. As for the incidence, POCD was detected in 12% of our patients at day 3 and 7.5% after 1 month irrespective of type of anaesthesia (GA/RA) and the duration of surgery. Interestingly, females were found at a significant risk for POCD; irrespective of gender, increasing age dominated as a potential risk factor for POCD.
Majority of the studies reported have evaluated POCD at an early stage (hospital discharge as an early time point, or week 1 if still hospitalised) and 3 months post-surgery as a long-term POCD time point. In comparison to early stage POCD, the results show a decline in incidence of POCD at 3 months.[3] Our short-term POCD evaluation at post-operative days 3, 7, and 30 also showed a gradual decline in the incidence of POCD, suggesting that it is temporary in few patients and could persist long-term in certain patients, probably even beyond 30 days. To the best of our knowledge, this is the first study to have evaluated the incidence of POCD at intermediate early time points compared to the existing literature. The results presented are in accordance with earlier reports and most importantly, highlights the early onset of trend in decline of POCD, thus stressing the importance of evaluating POCD at earlier time points before 3 months.
The International Study of Post-operative Cognitive Dysfunction 1 (ISPOCD 1) estimated the overall incidence of POCD to be 25.8% at 1 week and 9.9% after 3 months, with age as a significant and independent risk factor for POCD. We found a similar association, though not significant with the data supporting a trend in that direction. A larger pool of patients would have provided evidence to this effect. The incidence of POCD after 3 months was 7% in those aged 60-69 years and 14% in those over 69 years.[3] Monk et al., have reported that the prevalence of POCD is significantly higher in the elderly than in the young or middle-aged patients. They found that lesser education levels, higher grades of American Society of Anaesthesiologists (ASA) physical status, more complicated surgery, and longer hospital stays were other precipitating factors.[4]
We found that patients with a level of education more than high school had a lower incidence of POCD compared to those with lower educational levels. In educated population the brain is exposed to continuous challenging mental activities that could delay the manifestations of dementia by utilising neuronal reserves and increasing the efficacy of synapses to re-route around damaged areas. A hypothetical construct coined “cognitive reserve” has been utilised to describe models of cognitive ageing and circumstances where the brain sustains injury.[5] Surrogates of cognitive reserve have included education level, occupational attainment and performance on tests of knowledge such as vocabulary. Higher educational levels are associated with a reduced relative risk of developing Alzheimer's disease. There are several reports on the correlation between lower occupational attainment and incident. Although cognitive reserve is mainly used as an important concept in dementia research, there is evidence on its protective role against POCD.[6]
Clinicians and patients presume that RA is not associated with cognitive disturbances and is a safer option compared to GA. Rasmussen et al., in a randomised study of RA versus GA found no causative relationship between GA and long-term POCD. Furthermore, RA does not offer any apparent direct physiologic benefit on cognitive function.[7] Studies reported by O’Dwyer et al., Casati et al., and Somprakit et al., found no statistical difference in the incidence of POCD after either GA or RA.[8,9,10]
Since the type of anaesthesia does not seem to affect POCD, it is imperative to study the influence of the conduct of anaesthesia and POCD. Benzodiazepines are known for their effect on cognitive function; this could be related to slow and variable metabolism, particularly of diazepam which also has several active metabolites. Several studies however report that benzodiazepines do not play a major role in cognitive dysfunction after anaesthesia.[11,12] Increasing evidence supports that inhalational anaesthetics may increase the risk of developing POCD. Numerous animal experiments suggest that inhalational anaesthetics may alter cognitive function by amyloid β accumulation, modify neurotransmission, influence synaptic changes and alter calcium haemostasis. However, reported clinical studies evaluating the incidence of POCD and inhalational anaesthetics fail to show an association.[13]
Canet et al., concluded that the incidence of POCD at 7 days was remarkably lower after minor surgery (6.8%) than after major surgery (25.8%). After 3 months, no statistical difference was present between the two groups.[14] Factors such as duration of anaesthesia, surgical trauma, postoperative stress response, hospitalisation and post-operative pain and analgesics are implicated to explain the difference in rates of POCD between major and minor surgery.[15,16,17] A correlation between inflammatory response as measured by interleukin 6 and late functional recovery after hip arthroplasty implies a relationship between surgical trauma and recovery.[16] In the ISPOCD1 study, duration of anaesthesia was a significant risk for POCD at 7 days. The incidence was 18% when the duration was <2 h and 27% when the duration was longer.[3] However, we did not find any correlation between duration of anaesthetic exposure and POCD.
Neuropsychological test batteries are subject to large variability and no particular battery is deemed to be devoid of the statistical drawbacks. The ISPOCD study results revealed that the letter digit coding, Stroop colour interference and visual verbal learning tests had a high correlation with both age and IQ along with a high test-retest reliability coefficient.[3] Hence, these were chosen for our evaluation. The degree of change in a test deemed to constitute POCD has varied widely between studies ranging from deterioration of one standard deviation in one or more tests in a battery to the more rigorous Z score, wherein a Z score >2 is significant.[18] A major methodological issue in the study of POCD is lack of uniformly accepted battery of neuropsychological tests and no general consensus established regarding the optimum timing of assessments after surgery.
Several limitations must be discussed in the estimation of incidence. Only patients without pre-existing neurological limitations were included and hence those with dementia, alcohol dependence were excluded in this study. Patient participation required cooperation and interest, and therefore the included patients represent a group of relatively well-functioning subjects where the expected incidence of POCD may not correlate with the general patient population at that age.[19]
Patients presenting for emergency surgery with uncorrected comorbidities, high stress and metabolic derangement levels have shown significant incidence of neurobehavioural deficiencies postoperatively. Unfortunately this substantial group of patients were excluded as their baseline neuropsychological status prior to surgery could not be assessed. Increased post-operative morbidity and stay in high dependency care units makes this subset highly susceptible for an overall decline in their physiologic reserves.
Patient compliance for follow-up was a major hurdle. It is likely that reluctance to follow-up could be explained as intent to conceal cognitive deficits. Elaborate neuropsychological assessment was challenging to pursue as the majority of the patient population were naïve to the technological skills required.
CONCLUSION
Cognitive impairment can reduce patient compliance, distress family members, delay hospital discharge, and inevitably unmask the vulnerable elderly of their dignity and independence. In this short-term POCD study in the elderly, the incidence of POCD showed a gradual decline with gender emerging as a significant factor. In addition, increasing age and the level of education had a major influence on incidence of POCD.
With the increasing trend of the aged population presenting for surgery, only now are we beginning to graze the surface of its proclivity, aetiopathogenesis, and diagnosis. Further research efforts should emphasise on elucidating the mechanisms involved in contributing to POCD and directed towards developing novel therapeutic interventions or altering the delivery of current regimens to prevent the devastating consequences in this population.
ACKNOWLEDGMENT
Dr. K.P. Suresh, Scientist (Biostatistics), Project Directorate on Animal Disease Monitoring and Surveillance, Bangalore - 560 024.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Caza N, Taha R, Qi Y, Blaise G. The effects of surgery and anesthesia on memory and cognition. Prog Brain Res. 2008;169:409–22. doi: 10.1016/S0079-6123(07)00026-X. [DOI] [PubMed] [Google Scholar]
- 2.Dijkstra JB, Houx PJ, Jolles J. Cognition after major surgery in the elderly: Test performance and complaints. Br J Anaesth. 1999;82:867–74. doi: 10.1093/bja/82.6.867. [DOI] [PubMed] [Google Scholar]
- 3.Moller JT, Cluitmans P, Rasmussen LS, Houx P, Rasmussen H, Canet J, et al. Long-term postoperative cognitive dysfunction in the elderly ISPOCD1 study. ISPOCD investigators. International Study of Post-Operative Cognitive Dysfunction. Lancet. 1998;351:857–61. doi: 10.1016/s0140-6736(97)07382-0. [DOI] [PubMed] [Google Scholar]
- 4.Monk TG, Weldon BC, Garvan CW, Dede DE, van der Aa MT, Heilman KM, et al. Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology. 2008;108:18–30. doi: 10.1097/01.anes.0000296071.19434.1e. [DOI] [PubMed] [Google Scholar]
- 5.Stern Y. What is cognitive reserve? Theory and research application of the reserve concept. J Int Neuropsychol Soc. 2002;8:448–60. [PubMed] [Google Scholar]
- 6.Tsai TL, Sands LP, Leung JM. An update on postoperative cognitive dysfunction. Adv Anesth. 2010;28:269–84. doi: 10.1016/j.aan.2010.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rasmussen LS, Johnson T, Kuipers HM, Kristensen D, Siersma VD, Vila P, et al. Does anaesthesia cause postoperative cognitive dysfunction? A randomised study of regional versus general anaesthesia in 438 elderly patients. Acta Anaesthesiol Scand. 2003;47:260–6. doi: 10.1034/j.1399-6576.2003.00057.x. [DOI] [PubMed] [Google Scholar]
- 8.O‘Dwyer PJ, Serpell MG, Millar K, Paterson C, Young D, Hair A, et al. Local or general anesthesia for open hernia repair: A randomized trial. Ann Surg. 2003;237:574–9. doi: 10.1097/01.SLA.0000059992.76731.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Casati A, Aldegheri G, Vinciguerra E, Marsan A, Fraschini G, Torri G. Randomized comparison between sevoflurane anaesthesia and unilateral spinal anaesthesia in elderly patients undergoing orthopaedic surgery. Eur J Anaesthesiol. 2003;20:640–6. doi: 10.1017/s0265021503001030. [DOI] [PubMed] [Google Scholar]
- 10.Somprakit P, Lertakyamanee J, Satraratanamai C, Wanicksamban S, Silapadech A, Chainchop P, et al. Mental state change after general and regional anesthesia in adults and elderly patients, a randomized clinical trial. J Med Assoc Thai. 2002;85(Suppl 3):S875–83. [PubMed] [Google Scholar]
- 11.Rasmussen LS, Steentoft A, Rasmussen H, Kristensen PA, Moller JT Benzodiazepines and postoperative cognitive dysfunction in the elderly. ISPOCD Group. International Study of Postoperative Cognitive Dysfunction. Br J Anaesth. 1999;83:585–9. doi: 10.1093/bja/83.4.585. [DOI] [PubMed] [Google Scholar]
- 12.Fredman B, Lahav M, Zohar E, Golod M, Paruta I, Jedeikin R. The effect of midazolam premedication on mental and psychomotor recovery in geriatric patients undergoing brief surgical procedures. Anesth Analg. 1999;89:1161–6. [PubMed] [Google Scholar]
- 13.Ologunde R, Ma D. Do inhalational anesthetics cause cognitive dysfunction? Acta Anaesthesiol Taiwan. 2011;49:149–53. doi: 10.1016/j.aat.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 14.Canet J, Raeder J, Rasmussen LS, Enlund M, Kuipers HM, Hanning CD, et al. Cognitive dysfunction after minor surgery in the elderly. Acta Anaesthesiol Scand. 2003;47:1204–10. doi: 10.1046/j.1399-6576.2003.00238.x. [DOI] [PubMed] [Google Scholar]
- 15.Lynch NM, Trousdale RT, Ilstrup DM. Complications after concomitant bilateral total knee arthroplasty in elderly patients. Mayo Clin Proc. 1997;72:799–805. doi: 10.4065/72.9.799. [DOI] [PubMed] [Google Scholar]
- 16.Hall GM, Peerbhoy D, Shenkin A, Parker CJ, Salmon P. Relationship of the functional recovery after hip arthroplasty to the neuroendocrine and inflammatory responses. Br J Anaesth. 2001;87:537–42. doi: 10.1093/bja/87.4.537. [DOI] [PubMed] [Google Scholar]
- 17.Mann C, Pouzeratte Y, Boccara G, Peccoux C, Vergne C, Brunat G, et al. Comparison of intravenous or epidural patient-controlled analgesia in the elderly after major abdominal surgery. Anesthesiology. 2000;92:433–41. doi: 10.1097/00000542-200002000-00025. [DOI] [PubMed] [Google Scholar]
- 18.Rasmussen LS, Larsen K, Houx P, Skovgaard LT, Hanning CD, Moller JT, et al. The assessment of postoperative cognitive function. Acta Anaesthesiol Scand. 2001;45:275–89. doi: 10.1034/j.1399-6576.2001.045003275.x. [DOI] [PubMed] [Google Scholar]
- 19.Rasmussen LS. Postoperative cognitive dysfunction: Incidence and prevention. Best Pract Res Clin Anaesthesiol. 2006;20:315–30. doi: 10.1016/j.bpa.2005.10.011. [DOI] [PubMed] [Google Scholar]


