Abstract
Background and Aims:
Literature suggests that glottic view is better when using McGrath® Video laryngoscope and Truview® in comparison with McIntosh blade. The purpose of this study was to evaluate the effectiveness of McGrath Video laryngoscope in comparison with Truview laryngoscope for tracheal intubation in patients with simulated cervical spine injury using manual in-line stabilisation.
Methods:
This prospective randomised study was undertaken in operation theatre of a tertiary referral centre after approval from the Institutional Review Board. A total of 100 consenting patients presenting for elective surgery requiring tracheal intubation were randomly assigned to undergo intubation using McGrath® Video laryngoscope (n = 50) or Truview® (n = 50) laryngoscope. In all patients, we applied manual-in-line stabilisation of the cervical spine throughout the airway management. Statistical testing was conducted with the statistical package for the social science system version SPSS 17.0. Demographic data, airway assessment and haemodynamics were compared using the Chi-square test. A P < 0.05 was considered significant.
Results:
The time to successful intubation was less with McGrath video laryngoscope when compared to Truview (30.02 s vs. 38.72 s). However, there was no significant difference between laryngoscopic views obtained in both groups. The number of second intubation attempts required and incidence of complications were negligible with both devices. Success rate of intubation with both devices was 100%. Intubation with McGrath Video laryngoscope caused lesser alterations in haemodynamics.
Conclusions:
Both laryngoscopes are reliable in case of simulated cervical spine injury using manual-in-line stabilisation with 100% success rate and good glottic view.
Keywords: McGrath video laryngoscope, simulated difficult airway, Truview laryngoscope
INTRODUCTION
Airway management is a crucial responsibility of the anaesthesiologists. During direct laryngoscopy, proper positioning of the head and neck is essential for optimal laryngeal visualisation which requires a neck flexion of 35° and a head extension of 15° for the alignment of oral, pharyngeal and laryngeal axes. This position is also known as sniffing position.[1]
In patients with cervical spine injury, airway management poses a bigger challenge due to risk of neurological damage related to neck movements; thus manual-in-line stabilisation is commonly applied to minimise neck movement during tracheal intubation. Such immobilisation can render intubation under direct laryngoscopy more difficult.[2,3] Difficulties in airway management increases the risk of hypoxia, which can also lead to devastating neurological outcome. These issues have prompted the development of number of alternatives to Macintosh laryngoscope such as Truview EVO2®, McGrath® Video laryngoscope, Glidescope®, Airtraq®, etc., These laryngoscopes do not require the alignment of pharyngeal, laryngeal and oral axis and thus do not require sniffing position. In difficult airway scenarios, both McGrath Video laryngoscope and Truview EVO2 have proved to be better than Macintosh laryngoscope.[4,5] However, the relative efficacy of McGrath Video laryngoscope and Truview EVO2 have not been studied.
The McGrath® video laryngoscope (Aircraft Medical, Edinburgh, United Kingdom) is a video-based system for tracheal intubation that utilises a video camera embedded into a ‘camera stick’. The unit is powered by a single easily-replaceable 1.5 v AA battery and features a single electronic control; an on/off switch located on the top of the unit. It therefore offers the user an image of the vocal cords and the surrounding airway anatomy on a liquid crystal display (LCD) screen.
The Truview EVO2 is based on a combination of an optical system with a steel blade, provides a 42° angled view (refracted) through a 15-mm eyepiece based on prism principle to give an angular view of the glottic area. In addition, it has a port which connects to the auxiliary oxygen flow of the anaesthesia machine.
The primary objective of our study was to compare the McGrath video laryngoscope and Truview EVO2 laryngoscope when performing tracheal intubation in adult patients using manual-in-line stabilisation simulating cervical spine injury, and also to compare the haemodynamic changes associated with the two techniques of laryngoscopy.
METHODS
This was a prospective, parallel, randomised clinical trial. After enrolment, group assignments were determined by a computer-generated number sequence and were contained in sequentially numbered opaque envelopes to ensure blinding. After obtaining institutional ethical committee approval, 100 patients of either sex within the age group of 20-60 years, American Society of Anaesthesiologists Grades I or II undergoing elective surgery requiring general anaesthesia and endotracheal intubation were divided randomly into two groups of 50 patients each. Exclusion criteria included anticipated difficult airway (Mallampatti Class III and IV; thyromental distance <6 cm; and inter-incisor distance <3.5 cm), obesity, cardiovascular disease, endocrine disease, presence of risk factors for gastric aspiration e.g. pregnancy, diabetes, etc., After pre-anaesthetic check-up, an informed consent was obtained. Patients were given oral alprazolam 0.5 mg night before surgery and were kept fasting for 6 h. All patients received standardised general anaesthetic regime. Standard monitoring included electrocardiography, non-invasive arterial blood pressure, pulse oximeter, end-tidal carbon-dioxide. Heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean blood pressure (MBP) were recorded before induction, after induction, after intubation and thereafter at 3 min and 5 min post-intubation.
Pre-oxygenation was performed with 100% oxygen for 3 min. Before induction of anaesthesia, all patients were administered fentanyl 1.5μg/kg intravenous (i.v.). After thiopentone sodium induction, and checking for the adequacy of the bag and mask ventilation, vecuronium bromide 0.1mg/kg was administered and patient ventilated with 100% O2 with 1% isoflurane. At 3 min after the administration of muscle relaxant, the pillow was removed and the neck was immobilised using manual-in-line axial stabilisation. During this procedure, an assistant stood at the head end of the patient placing his/her fingers firmly on the mastoid process and the thumbs on the temporo-parietal area of the skull. The hands were then pressed against the OT table vertically downwards thus opposing any movements of the head and neck caused by the anaesthesiologist. Intubation was performed with a 7.5 mm endotracheal tube in females, and an 8.0 mm endotracheal tube in males, by an experienced anaesthesiologist (>10 years of experience in anaesthesia and who had performed at least 30 intubations with each of the two laryngoscopes under study) using either McGrath video laryngoscope (Group M) or Truview laryngoscope (Group T) as per the randomisation.
A Truview EVO2 stylet was used in both groups. After successful tracheal intubation, in all the patients, anaesthesia was maintained with isoflurane (1%) in a mixture of oxygen and nitrous oxide in 40:60 ratio. Surgery was allowed to start 5 min after the tracheal intubation.
The laryngeal view was assessed using Cormack and Lehane grading (CL grade) system. Other data collected was time to achieve successful tracheal intubation. Intubation time was defined as the time between the insertion of the allocated laryngoscope in patients mouth until end-tidal carbon-dioxide was detected. A failed intubation attempt was defined as an attempt in which the trachea could not be intubated, or which required >60 s to perform. Only two intubation attempts were allowed. In those cases where intubation was not successful during the first attempt, a second attempt was undertaken after bag and mask ventilation until SpO2 reached 100%. After a failed second attempt manual-in-line stabilization was discontinued and intubation performed. Additional observations included the number of intubation attempts and the number of times optimisation manoeuvre were required. Any complication associated with tracheal intubation such as injury to lips, oral mucosa or dentition, oesophageal intubation, or hypoxia (SpO2 < 92%) during intubation were also recorded.
The primary objective of this study was the duration of intubation. It was estimated to be 10 s, based on the previous study in order to detect a 13 s standard deviation difference in duration of intubation between the two groups (α =0.05, 2-sided, β =0.1), 50 patients/group were required.[6]
Statistical testing was conducted with the statistical package for the social science system (version 17.0; SPSS Inc., Chicago, IL, USA). Continuous variables are presented as mean ± standard deviation, and categorical variables are presented as absolute numbers and percentage. The comparison of normally distributed continuous variables between the groups was performed using Student's t-test. Nominal categorical data between the groups were compared using Chi-square test or Fisher's exact test as appropriate. For all statistical tests, a P < 0.05 was taken to indicate a significant difference
RESULTS
Both male and female patients were adequately represented. There was no difference between the two groups with regard to demographic data and baseline airway assessment parameters [Table 1]. Glottic view in both groups was either Cormack and Lehane Grade I or II. Incidence of Grade I view was 78% in Group M and 90% in Group T and Grade II view was 22% in Group M and 10% in Group T [Table 2]. The results were statistically insignificant (P > 0.05). Time taken to successfully intubate was significantly less with Group M (30.02 ± 9.87 s) when compared with Group T (38.72 ± 9.50 s) (P < 0.05) [Figure 1]. No second attempt was required in Group M, but in Group T, two patients needed a second attempt. The results were statistically insignificant (P > 0.05). All the patients during the study got intubated in 1st or a 2nd attempt. The success rate was 100% in both groups [Table 2]. Use of external laryngeal manoeuvre was needed in two cases with Group M and four cases with Group T. The difference was found to be statistically insignificant (P > 0.05). None of the patients in Group M experienced trauma whereas in Group T, two patients had gingival bleed as a complication of laryngoscopy [Table 2].
Table 1.
Patient characteristics of patients enrolled into the study. Group M, McGrath video laryngoscope; Group T, Truview EVO2
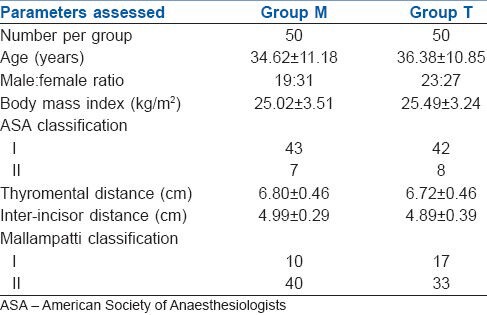
Table 2.
Comparison of results between the two groups. Group M, McGrath video laryngoscope group; Group T, Truview EVO2 Group
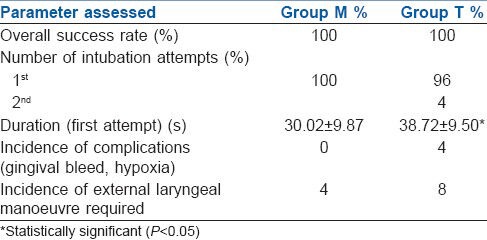
Figure 1.
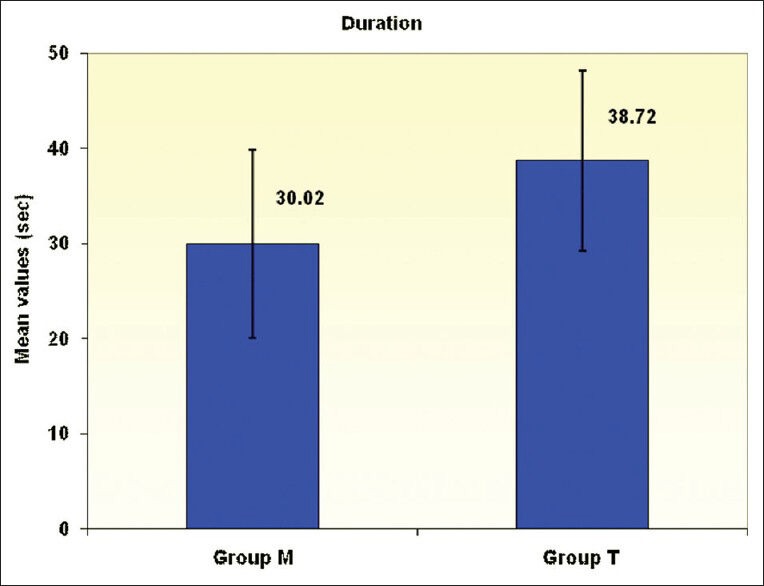
Bar graph depicting the duration of intubation in seconds during the first attempt with each laryngoscope. The data are given as mean (standard deviation). Group M, McGrath® video laryngoscope group; Group T, Truview EVO2® group
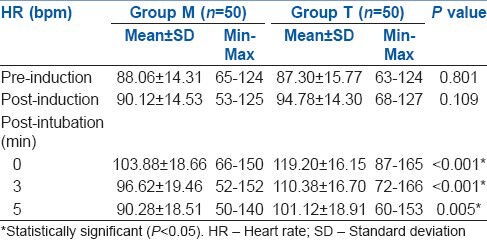
HR and blood pressure increased immediately after intubation with both the laryngoscopes, but the increase was more with Truview EVO2® laryngoscope and this difference was statistically significant (P < 0.05) [Tables 3 and 4]. The blood pressure (SBP, DBP and MBP) returned to pre-intubation values in both groups after 3 min of intubation. The HR at 3 and 5 min after intubation was significantly higher in Group T than in Group M [Table 4].
Table 3.
Comparison of MBP. Group M, McGrath Video laryngoscope Group; Group T, Truview EVO2 group
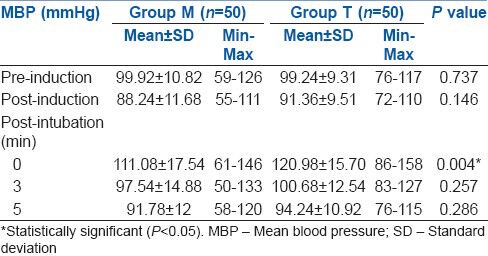
Table 4.
Comparison of HR. Group M, McGrath video laryngoscope group; Group T, Truview EVO2 Group
DISCUSSION
The primary aim of our study was to compare the McGrath® Video laryngoscope and Truview EVO2® laryngoscope while performing tracheal intubation in adult patients using manual-in-line stabilisation simulating cervical spine injury, and secondarily to compare the haemodynamic changes associated with the above two techniques.
With simulated difficulty by performing manual-in-line stabilisation during intubation, both the laryngoscopes provided similar laryngoscopic views (CL Grade I or II glottic view) in all the cases signifying good glottic exposure. As already mentioned, there have been no studies directly comparing these two devices, although many studies comparing these two individual devices with conventional laryngoscopes have been reported.
Savoldelli et al.,[7] Piepho et al.[8] and Burdett et al.[9] found in manikin studies that in difficult airway scenario using cervical spine immobilisation, McGrath video laryngoscope offered better laryngoscopic view using Cormack and Lehane grading as compared with Macintosh laryngoscope. They explained, that with a direct laryngoscope it is necessary to obtain a line of sight from the maxillary teeth to the glottis, which is difficult to obtain using cervical spine immobilisation technique, whereas with the use of McGrath video laryngoscope the image of glottis is captured near the tip of the blade, only a few centimetres of line of sight is required and the need to align the oral, pharyngeal and laryngeal axes is not there.
Similarly, Malik et al.[10] concluded that laryngoscopic views in manikins with cervical spine immobilisation obtained by Truview EVO2 was significantly (P < 0.05) better than Macintosh laryngoscope because it uses an optical system, which provides a 42° deflection view without the need for alignment of the oral, pharyngeal, and laryngeal axes.
In our study, the mean time required for intubation using McGrath Video laryngoscope was less than the time required for intubation using Truview EVO2 laryngoscope and was statistically significant [Table 2]. The reason behind this difference could be that Truview EVO2 gives a smaller field of vision, where the image of the vocal cords has to be focused on the prism to get the correct view which takes a few seconds, whereas McGrath video laryngoscope has an LCD screen which gives a clear image of the vocal cords and the surrounding anatomy with a larger field of vision. However, other investigators[7,8,11] found that intubation time using McGrath Video laryngoscope was significantly more (P < 0.05) as compared with Macintosh laryngoscope in manikins with cervical spine immobilisation. The reason behind more time taken by McGrath Video laryngoscope than Macintosh laryngoscope was that although video laryngoscopes offer superior visualisation of the glottis, a good laryngeal view does not guarantee easy or successful tracheal tube insertion. All video laryngoscopes without an integrated guide channel for the endotracheal tube could face the challenge of advancing the tube into the trachea as the tip of the tracheal tube must pass through an acute angle to enter the larynx and has significant potential of coming in contact with the anterior tracheal wall. On the contrary, Burdett et al.[9] found in a manikin study that in difficult airway scenario McGrath video laryngoscope required less time for intubation as compared with Macintosh laryngoscope.
Barak et al.[6] and Nasim et al.[12] found that Truview EVO2 laryngoscope took significantly longer time (P < 0.05) for intubation than Macintosh laryngoscope when used in the cervical spine rigidity scenarios in manikins.
In another study in patients with cervical spine immobilisation,[10] the time for intubation was significantly more when using Truview EVO2 laryngoscope than Macintosh laryngoscope. In the above studies comparing Truview EVO2 and Macintosh laryngoscope the authors demonstrated that the tube needs to be advanced blindly until its tip enters the Truview visual field, thereafter, the tube should be introduced through the vocal cords while looking through the lens, which requires good eye-hand coordination and could be the reason behind more time taken by Truview EVO2 laryngoscope.
None of the patients had significant desaturation (SpO2 < 92%), oesophageal intubation or lip injury, though two patients in Group T (Truview EVO2) had slight gingival bleed. The incidence was negligible as compared to McGrath video laryngoscope.
Success rate in both groups was found to be 100% indicating good overall performance which correlated with the previous studies. In previous manikin studies (7,8,11) the success rate for McGrath video laryngoscope was found to be 100% in the scenario with decreased cervical spine motion. In a manikin study by Barak et al.[6] Truview EVO2 had a success rate of 100% and that of Macintosh laryngoscope was 90% in a scenario with decreased cervical spine motion.
The exposure of the glottis during laryngoscopy requires the elevation of the epiglottis by a forward and upward lifting force of the laryngoscope blade which is associated with an increase in HR and blood pressure secondary to sympathetic discharge. This hypertensive response is directly proportional to the amount of lifting force[13] and the duration of laryngoscopy and intubation.[14]
Haemodynamic response to laryngoscopy and intubation was more with Truview EVO2 as compared to McGrath video laryngoscope in the present study. The reason for this may be that the McGrath video laryngoscope is designed to fit into the natural anatomy of the orotracheal conduit and requires lesser vertical force to achieve glottic alignment as compared with Truview EVO2. Moreover, intubation with Truview EVO2 was associated with longer mean intubation time.
CONCLUSIONS
In patients with simulated cervical spine injury, intubation with McGrath video laryngoscope required lesser time then using Truview EVO2 laryngoscope. No significant difference was found in laryngoscopic view, requirement of optimisation manoeuvre and need for second attempt for intubation with both the instruments. Both are safe to use in patients with cervical spine immobilisation considering high overall success rate and no significant trauma involved. Haemodynamic response to intubation was greater with Truview EVO2 laryngoscope than McGrath video laryngoscope.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Horton WA, Fahy L, Charters P. Defining a standard intubating position using “angle finder”. Br J Anaesth. 1989;62:6–12. doi: 10.1093/bja/62.1.6. [DOI] [PubMed] [Google Scholar]
- 2.Heath KJ. The effect of laryngoscopy of different cervical spine immobilisation techniques. Anaesthesia. 1994;49:843–5. doi: 10.1111/j.1365-2044.1994.tb04254.x. [DOI] [PubMed] [Google Scholar]
- 3.Asai T, Neil J, Stacey M. Ease of placement of the laryngeal mask during manual in-line neck stabilization. Br J Anaesth. 1998;80:617–20. doi: 10.1093/bja/80.5.617. [DOI] [PubMed] [Google Scholar]
- 4.Shippey B, Ray D, McKeown D. Use of the McGrath videolaryngoscope in the management of difficult and failed tracheal intubation. Br J Anaesth. 2008;100:116–9. doi: 10.1093/bja/aem303. [DOI] [PubMed] [Google Scholar]
- 5.Malik MA, O‘Donoghue C, Carney J, Maharaj CH, Harte BH, Laffey JG. Comparison of the Glidescope, the Pentax AWS, and the Truview EVO2 with the Macintosh laryngoscope in experienced anaesthetists: A manikin study. Br J Anaesth. 2009;102:128–34. doi: 10.1093/bja/aen342. [DOI] [PubMed] [Google Scholar]
- 6.Barak M, Philipchuck P, Abecassis P, Katz Y. A comparison of the Truview blade with the Macintosh blade in adult patients. Anaesthesia. 2007;62:827–31. doi: 10.1111/j.1365-2044.2007.05143.x. [DOI] [PubMed] [Google Scholar]
- 7.Savoldelli GL, Schiffer E, Abegg C, Baeriswyl V, Clergue F, Waeber JL. Comparison of the Glidescope, the McGrath, the Airtraq and the Macintosh laryngoscopes in simulated difficult airways*. Anaesthesia. 2008;63:1358–64. doi: 10.1111/j.1365-2044.2008.05653.x. [DOI] [PubMed] [Google Scholar]
- 8.Piepho T, Weinert K, Heid FM, Werner C, Noppens RR. Comparison of the McGrath® Series 5 and GlideScope® Ranger with the Macintosh laryngoscope by paramedics. Scand J Trauma Resusc Emerg Med. 2011;19:4. doi: 10.1186/1757-7241-19-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burdett E, Ross-Anderson DJ, Makepeace J, Bassett PA, Clarke SG, Mitchell V. Randomized controlled trial of the A.P. Advance, McGrath, and Macintosh laryngoscopes in normal and difficult intubation scenarios: A manikin study. Br J Anaesth. 2011;107:983–8. doi: 10.1093/bja/aer295. [DOI] [PubMed] [Google Scholar]
- 10.Malik MA, Maharaj CH, Harte BH, Laffey JG. Comparison of Macintosh, Truview EVO2, Glidescope, and Airwayscope laryngoscope use in patients with cervical spine immobilization. Br J Anaesth. 2008;101:723–30. doi: 10.1093/bja/aen231. [DOI] [PubMed] [Google Scholar]
- 11.Maharaj CH, McDonnell JG, Harte BH, Laffey JG. A comparison of direct and indirect laryngoscopes and the ILMA in novice users: A manikin study. Anaesthesia. 2007;62:1161–6. doi: 10.1111/j.1365-2044.2007.05216.x. [DOI] [PubMed] [Google Scholar]
- 12.Nasim S, Maharaj CH, Butt I, Malik MA, O‘ Donnell J, Higgins BD, et al. Comparison of the Airtraq and Truview laryngoscopes to the Macintosh laryngoscope for use by Advanced Paramedics in easy and simulated difficult intubation in manikins. BMC Emerg Med. 2009;9:2. doi: 10.1186/1471-227X-9-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Forbes AM, Dally FG. Acute hypertension during induction of anaesthesia and endotracheal intubation in normotensive man. Br J Anaesth. 1970;42:618–24. doi: 10.1093/bja/42.7.618. [DOI] [PubMed] [Google Scholar]
- 14.Stoelting RK. Circulatory changes during direct laryngoscopy and tracheal intubation: Influence of duration of laryngoscopy with or without prior lidocaine. Anesthesiology. 1977;47:381–4. doi: 10.1097/00000542-197710000-00012. [DOI] [PubMed] [Google Scholar]


