Abstract
Diospyrobezoars are a rare cause of small intestinal obstruction. A 78-year-old man, with a history of persimmons ingestion and gastrectomy, presented with upper abdominal pain and weight loss. The upper gastrointestinal endoscopy showed a huge bezoar in the stomach. After initial endoscopic fragmentation, the abdominal X-ray revealed intestinal obstruction and the colonoscopy showed large fragments of the bezoar filling the terminal ileum. The migrated bezoar pieces were successfully removed by endoscopic fragmentation with a cutting lithotripter.
Background
Phytobezoars are the most common type of bezoars found in the gastrointestinal tract. A diospyrobezoar is a subtype of phytobezoar owing to excessive consumption of persimmons, and is difficult to treat due to its hard consistency.1 Small intestinal obstruction resulting from a primary bezoar is rare and usually caused by migration of a gastric bezoar,2 and is commonly removed by surgery. Our report presents the successful endoscopic treatment of bezoar pieces in the terminal ileum, which had migrated from the stomach after mechanical fragmentation of a large gastric persimmon bezoar.
Case presentation
A 78-year-old man was admitted in February 2014 with upper abdominal pain and weight loss. The patient had a history of persimmons ingestion in September 2013 and a history of Billroth I gastrectomy to treat a chronic gastric ulcer 30 years earlier. He had no symptoms of vomiting or distension. He also had no history of any other disease or surgery. Basic blood investigations including a full blood count, liver and renal panels were normal.
An upper gastrointestinal endoscopy (Olympus GIF-260, Japan) was performed, showing a large round bezoar with smooth surface dark green in colour (figure 1A) located on the greater curvature of gastric remnant. The patient was also detected with a gastric ulcer at the anastomosis. The result of abdominal X-ray was normal (figure 2A). A clinical diagnosis of gastric diospyrobezoar was carried out and the patient referred for endoscopic fragmentation. We broke the bezoar using a set of cutting lithotripters composed of handle, sheath and an oval-type snare (2.4×1700 mm, WF-2417DTH; Wilson-Cook Medical Inc, USA). The bezoar was snared by its longer diameter to create an imprint (figure 1B). After repeated cutting, we found the bezoar segments too firm to break into small pieces in one session, so we scheduled to break the large residual fragments (figure 1C) with multiple sessions.
Figure 1.

Endoscopic treatment of the diospyrobezoar in the stomach. (A) A huge diospyrobezoar in the stomach; (B) the bezoar was cut with a snare; and (C) the bezoar was broken into large fragments.
Figure 2.
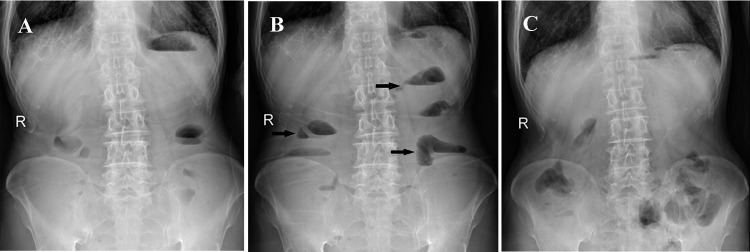
Intestinal obstruction caused by migrated bezoar fragments. (A) Radiograph before the initial endoscopic treatment; (B) radiograph after the initial endoscopic treatment showing gas-fluid levels in small intestine; and (C) re-examination of radiograph 7 days after the colonoscopic treatment.
On the second day after fragmentation, the patient reported of lower abdominal pain, distension and vomiting. In the physical examination, the abdomen was tender to direct palpation and the bowel sounds were increased, but signs of peritoneal irritation were negative. On the third day the small intestine was detected with dilated loops and gas-fluid levels in the plain abdominal radiography (figure 2B). Nasogastric tube decompression was performed and 100 mL of sesame oil was administered through the tube once daily. On the sixth day after initial treatment, the abdominal pain and distension were not relieved. The beside ultrasound examination revealed multiple masses with strong echo located in the lumen of the ileocecum. A diagnosis of intestinal obstruction induced by bezoar fragments migrated from the stomach was carried out.
Treatment
Because the location of bezoar fragments was relatively low in the small intestine and there were no indications for immediate surgical treatment, the patient was referred for an endoscopic intervention. During the colonoscopy (Pentax EC-3400 L, EPM-3500 system, Japan), one large and many small pieces of the bezoar were found filling the terminal ileum 10 cm from the ileocecal valve (figure 3A). In the process of fragmentation, the largest piece of the bezoar could not be easily moved and snared because of its longer diameter, so we created an imprint on the piece on which the snare could firmly grip, thereby avoiding slippage of the snare from its surface. Then we pulled the snare tightly and the first piece was successfully separated from the rest of the bezoar fragments. We repeated the procedure and finally all the large fragments were broken into small pieces to be easily passed through the ileocecal valve to colonic lumen (figure 3B). During the fragmentation, a large volume of fluid flowed distally from the small bowel. After all the fragments in the terminal ileum were removed (figure 3C), the patient was treated with enema once daily.
Figure 3.

Colonoscopic treatment of diospyrobezoar in the terminal ileum. (A) Large bezoar fragments filled in the terminal ileum. (B) The bezoar was cut with a snare. (C) Complete removal of bezoar pieces in the terminal ileum.
Outcome and follow-up
The patient recovered uneventfully. He gradually passed out the bezoar pieces over 5 days and no longer reported of abdominal pain and vomiting. The abdominal radiograph in re-examination revealed no signs of intestinal obstruction or perforation (figure 2C). Thereafter, the patient was discharged and had no relapse at 1-month follow-up.
Discussion
Diospyrobezoars are especially prevalent in some Asian countries where persimmons and similar fruits are commonly ingested. Although the aetiology is undefined, history of gastric surgery and delayed gastric emptying are risk factors.3 Small intestinal obstruction caused by a diospyrobezoar is usually caused by migration of a gastric bezoar.2 In our case, the initial abdominal radiograph showed no signs of intestinal obstruction; but dilated loops of small intestine and gas-fluid levels in the radiograph after initial endoscopic treatment revealed that the fragmented bezoar was not primary but had migrated from the stomach. The pylorus prevents large fragments from reaching the small intestine but in our case the patient had a history of gastrectomy, so resection of pylorus may have weakened this function and lead to the passage of large fragments of the bezoar into the small intestine. Postoperative adhesion is also a risk factor for an intestinal bezoar, but in our case no evidence was found that the adhesion (if there was any) contributed to the intestinal obstruction caused by the bezoar.
A diospyrobezoar is usually removed endoscopically or surgically.4 Recently, cola dissolution had also been demonstrated as an effective method to treat a gastric diospyrobezoar.5 However, the gastric diospyrobezoar has a hard consistency and treatment with mechanical fragmentation or cola dissolution is difficult and sometimes cannot be successful especially when the size of the bezoar is large. In our case, we tried to treat the huge diospyrobezoar with mechanical fragmentation but it could not be accomplished in one session. Unfortunately, the large fragments of the bezoar migrated to the small intestine after the initial treatment. Bezoars in the small intestine usually cannot be removed by endoscopic treatment or cola dissolution and commonly require surgical intervention.6 We found in our case that the bezoar fragments were at a lower location in the small intestine and no signs of peritoneal irritation or perforation were detected. Hence we tried to treat the bezoar in the terminal ileum by colonoscopic fragmentation. Finally we successfully relieved the intestinal obstruction by endoscopic treatment instead of surgical intervention. There are also several reports of successful removal of intestinal phytobezoars using double-balloon enteroscopy7 or colonoscopy,8 suggesting endoscopic intervention could be an alternative treatment in selected patients with intestinal obstruction caused by phytobezoars.
To our knowledge, intestinal obstructions caused by diospyrobezoars are uncommon and usually need surgery, which might incur higher expenses and longer recovery periods. The decision of colonoscopic treatment should be based on the judgement of the location of intestinal bezoar and exclusion of indications for immediate operation.
Learning points.
Diospyrobezoars in the small intestine are uncommon; but suspicion should be raised in any patient presenting with a gastric bezoar, especially when there is a history of gastrectomy.
Insufficient fragmentation may result in migration of the bezoar and intestinal obstruction.
Colonoscopic fragmentation is an alternative option for the treatment of diospyrobezoars in the terminal ileum.
Footnotes
Contributors: BQ wrote the case report. XL-W and LD performed the treatment of the patient and LD wrote the discussion. XY-G helped with patient follow-up and literature review.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Erzurumlu K, Malazgirt Z, Bektas A, et al. Gastrointestinal bezoars: a retrospective analysis of 34 cases. World J Gastroenterol 2005;11:1813–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Escamilla C, Robles-Campos R, Parrilla-Paricio P, et al. Intestinal obstruction and bezoars. J Am Coll Surg 1994;179:285–8 [PubMed] [Google Scholar]
- 3.Cifuentes Tebar J, Robles Campos R, Parrilla Paricio P, et al. Gastric surgery and bezoars. Dig Dis Sci 1992;37:1694–6 [DOI] [PubMed] [Google Scholar]
- 4.Walker-Renard P. Update on the medicinal management of phytobezoars. Am J Gastroenterol 1993;88:1663–6 [PubMed] [Google Scholar]
- 5.Ladas SD, Kamberoglou D, Karamanolis G, et al. Systematic review: Coca-Cola can effectively dissolve gastric phytobezoars as a first-line treatment. Aliment Pharmacol Ther 2013;37:169–73 [DOI] [PubMed] [Google Scholar]
- 6.Bedioui H, Daghfous A, Ayadi M, et al. A report of 15 cases of small-bowel obstruction secondary to phytobezoars: predisposing factors and diagnostic difficulties. Gastroenterol Clin Biol 2008;32:596–600 [DOI] [PubMed] [Google Scholar]
- 7.Chou JW, Lai HC. Obstructing small bowel phytobezoar successfully treated with an endoscopic fragmentation using double-balloon enteroscopy. Clin Gastroenterol Hepatol 2009;7:e51–2 [DOI] [PubMed] [Google Scholar]
- 8.Chae HS, Kim SS, Han SW, et al. Endoscopic removal of a phytobezoar obstructing the distal small bowel. Gastrointest Endosc 2001;54:264–6 [DOI] [PubMed] [Google Scholar]


