Abstract
Objectives
To assess the costs of the health effects of cigarette smoking and secondhand smoke (SHS) exposure to society.
Design
Prevalence-based, disease-specific cost-of-illness study. We used an epidemiological population-attributable risk method to determine the costs that can be attributed to smoking and SHS exposure.
Setting
Taiwan.
Participants
All adult population aged 35 and older.
Primary outcome measures
Direct costs of healthcare expenditures spent for treating tobacco-related diseases, indirect mortality costs measured by the value of lost productivity due to tobacco-related premature deaths and indirect morbidity costs measured by the value of time lost from work due to tobacco-related illness.
Results
In 2010, direct costs of smoking and SHS exposure amounted to US$828 million, accounting for 3.4% of Taiwan's total personal healthcare expenditures. Smoking and SHS exposure also contributed to 15 555 premature deaths—corresponding to a loss of 284 765 years of life and US$820 million in productivity—and US$22 million in indirect morbidity costs. These direct and indirect costs totalled US$1670 million, representing 0.4% of Taiwan's gross domestic product and averaging about US$720/adult smoker. The share of the total costs was greater from active smoking (92%) than SHS exposure (8%), and greater for men (92%) than women (8%).
Conclusions
Smoking and SHS exposure impose a huge financial loss in Taiwan. Sustained tobacco control efforts to encourage people to quit smoking, prevent smoking uptake by children and young adults and protect all people from SHS exposure are needed.
Keywords: HEALTH ECONOMICS, PUBLIC HEALTH, STATISTICS & RESEARCH METHODS
Strengths and limitations of this study.
Little is known about the economic costs of secondhand smoke (SHS) exposure in East Asian countries. This is the first study to assess the health effects of smoking by taking into account the economic impact of SHS exposure in Taiwan.
This study provides evidence on the economic effect of the recent reduction in smoking prevalence and SHS exposure on healthcare costs and productivity losses to Taiwanese society as a result of implementing a comprehensive tobacco control programme in 2009.
Only adults aged 35 and older were included in the study.
The relative risks of healthcare cost for smokers are assumed to be the same as the relative risks of death for smokers because of data limitation.
Introduction
East Asia is the world's largest tobacco epidemic region, responsible for nearly half of total global cigarette consumption.1 Although all East Asian countries ratified the WHO Framework Convention on Tobacco Control (FCTC) in 2004 or 2005, a recent assessment study2 revealed that the majority of countries in East Asia lagged behind in implementing the FCTC recommended tobacco control programmes according to WHO's MPOWER (Monitoring, Protect, Offer, Warn, Enforcement and Raise) criteria.3 As of 2010, 37−53% of adult men in East Asia were current smokers and more than 46% of men were exposed to passive smoking at workplaces.2 To enhance the incentives to implement the promises of the ratified FCTC to reduce the tobacco epidemic in East Asia, updating of evidence on the economic costs due to active and passive smoking-caused illness, disability and premature mortality in this region is imperative.
Taiwan is regarded as a model in East Asia in tobacco control.2 During the 1960s and 1970s, smoking prevalence among Taiwanese aged 35 and above exceeded 75% for men and 8–12% for women.4 In 1987, Taiwan's cigarette market was forced to open to foreign brands, leading to a 6% jump in adult male smoking and a 13% jump in youth smoking within 3 years.4 As a consequence, the government launched a series of tobacco control initiatives such as school-based antismoking programmes and the 1997 Tobacco Hazards Prevention Act through which indoor workplaces and public places became partially smoke free.5 In 2002, the government levied a tobacco tax amounting to five New Taiwan Dollars (NT$) per pack and started the Outpatient Smoking Cessation Services.5 During the period of 1990–2005, smoking prevalence among men aged 18 and older had declined from 59.4% to 40%.5 Taiwan's legislature ratified the WHO FCTC in 2005. Based on the FCTC recommendations,6 an amendment to the Tobacco Hazards Prevention Act went into effect in 2009 (hereafter called the 2009 Act) to strengthen existing tobacco control measures by adding graphic warning labels on cigarette packets, extending smoke-free areas to almost all enclosed workplaces and public places, completely banning tobacco advertisements, promotion and sponsorship, as well as increasing tobacco taxes.
As a result of the 2009 Act, smoking prevalence among men aged 18 and older in Taiwan further decreased from 40% to 33.5% and exposure to passive smoking in workplaces decreased substantially from 33.2% to 18.2% between 2005 and 2011.5 7 Given this sizeable reduction in active and passive smoking, it is policy relevant to assess the current level of the costs of active and passive smoking-attributable illness, disability and premature mortality, and to determine whether or not these costs have decreased.
Two previous studies estimated the cost of smoking in Taiwan. Using a prevalence-based approach, Yang et al8 estimated that in 2001, smoking contributed to US$398 million in excess medical expenditures and US$1390 million in productivity loss from premature death among people aged 35 and older in Taiwan. Using an incidence-based approach, Chung et al9 estimated that the present value of lifetime smoking-attributable medical costs among people aged 35 and older ranged from US$291 to US$336 million depending on discount rate for the year 2001 in Taiwan. There has been no study to update these cost estimates in Taiwan since 2001. Furthermore, none of the studies on the cost of smoking in Taiwan and few of those in the literature have included any health costs attributed to passive smoking, also known as secondhand smoke (SHS).
The main objective of this study is to assess the costs of the health effects of cigarette smoking and SHS exposure in Taiwan in 2010. This is the first attempt to quantify the economic costs of SHS exposure in Taiwan. This study will also provide an evaluation on the hypothesis that implementation of the 2009 Act was associated with decreases in economic costs of smoking and SHS exposure. Because of the similarities in the tobacco epidemic and culture among East Asian countries, the findings of this study can serve as a valuable reference for understanding the economic benefits of tobacco control programmes in the region.
Methods
We considered three components of costs: direct costs of healthcare expenditures spent for treating tobacco-related diseases; indirect mortality costs measured by the value of lost productivity due to premature death and indirect morbidity costs measured by the value of time lost from work due to tobacco-related illness. A prevalence-based, disease-specific cost-of-illness approach10 was used to estimate the healthcare expenditures, workloss days and deaths due to smoking-related diseases in 2010. We used an epidemiological population-attributable risk method11 to determine the smoking-attributable fraction (SAF), which measures the proportion of expenditures, workloss days or deaths that can be attributed to smoking, and applied it to the total measure. A SHS-attributable fraction (SAFSHS) was estimated in a similar manner. Our analyses focused on adults aged 35 years and older.
Data sources
Population-based data from the annual Adult Smoking Behavior Survey (ASBS) were used to determine the prevalence of smoking and SHS exposure. The ASBS is a telephone interview survey collecting information on individuals’ demographic characteristics, cigarette smoking and quitting behaviours, and SHS exposure from a nationally representative sample (around 16 000/year) of a non-institutionalised population aged 18 and older in Taiwan. Disease-specific inpatient and outpatient expenditures, and number of hospital inpatient days were obtained from the 2010 National Health Insurance (NHI) claims database. Taiwan’s NHI, launched in 1995, is a mandatory single-payer social health insurance system administered by the government that provides universal healthcare coverage to virtually all citizens in Taiwan.
Population data came from the 2010 Population Census,12 number of deaths for each disease from the 2010 Statistics of Causes of Death13 and life expectancy by age and gender from the 2010 life tables.14 The age-specific and gender-specific employment rates and monthly earnings were obtained from the 2010 Report on the Manpower Utilization Survey.15
Smoking-related and SHS-associated diseases
We included 19 smoking-related diseases which were identified to have a significant association between cigarette smoking and mortality risk by two large epidemiological studies conducted in Taiwan.16 17 We considered six SHS-associated diseases: lung cancer, ischaemic heart disease, cerebrovascular disease, chronic obstructive pulmonary disease, asthma and breast cancer; and four SHS-associated causes of death: lung cancer, ischaemic heart disease, cerebrovascular disease and asthma as reported by the California Environmental Protection Agency (EPA)18 and WHO.19 20 Details of these diseases and their diagnosis codes are listed in table 1.
Table 1.
Smoking-related cause of death, SHS-associated disease and cause of death, and RR by disease and gender, Taiwan
| RR of smoking-related death |
RR of SHS-associated disease |
RR of SHS-associated cause of death | ||||||
|---|---|---|---|---|---|---|---|---|
| Male |
Female |
|||||||
| Disease (ICD-9 code) | CS | FS | CS | FS | Male | Female | Male | Female |
| Smoking-related cause of death | ||||||||
| All causes (001–998) | 1.55 | 1.33 | 1.89 | 1.33 | ||||
| Cancer | ||||||||
| Lip/oral cavity/pharynx (140–149) | 2.60 | 1.96 | – | – | ||||
| Oesophagus (150) | 3.18 | 2.31 | 15.57 | 6.40 | ||||
| Stomach (151) | 1.68 | 1.41 | – | – | ||||
| Rectum (154) | 2.06 | 1.64 | – | – | ||||
| Liver/gallbladder/bile ducts (155–156) | 1.46 | 1.28 | 5.03 | 2.49 | ||||
| Lung (162)* | 2.73 | 2.04 | 3.36 | 1.88 | 1.29 | 1.29 | 1.29 | 1.29 |
| Cervix uteri (180) | – | – | 5.78 | 2.77 | ||||
| Cardiovascular disease | ||||||||
| Rheumatic HD (390–398) | – | – | 9.43 | 4.13 | ||||
| Ischaemic HD (410–414)* | 2.06 | 1.64 | 3.58 | 1.96 | 1.49 | 1.49 | 1.23 | 1.23 |
| Cardiac arrest and other HD (420–429) | 1.60 | 1.36 | – | – | ||||
| Cerebrovascular disease (430–438)* | 1.65 | 1.39 | – | – | 1.82 | 1.82 | 1.65 | 1.65 |
| Respiratory disease | ||||||||
| Chronic bronchitis (491) | 3.13 | 2.28 | – | – | ||||
| Asthma (493)* | – | – | 7.12 | 3.27 | 1.97 | 1.97 | 1.97 | 1.97 |
| Chronic airway obstruction (496) | 2.65 | 1.99 | – | – | ||||
| Digestive system disease | ||||||||
| Peptic ulcer, GI haemorrhage (531–533) | 3.00 | 2.20 | 22.28 | 8.89 | ||||
| Liver cirrhosis (571) | 2.01 | 1.61 | – | – | ||||
| Other smoking-related disease | ||||||||
| Diabetes mellitus (250) | 1.51 | 1.31 | – | – | ||||
| Kidney diseases (580–589) | 2.23 | 1.74 | – | – | ||||
| Accidents (800–949) | 1.66 | 1.40 | – | – | ||||
| Other SHS-associated disease | ||||||||
| COPD (490–492, 496) | 1.55 | 1.55 | ||||||
| Breast cancer (174)† | – | 1.68 | ||||||
*Also a SHS-associated disease and SHS-associated cause of death.
†Only among premenopausal women younger than age 50.
COPD, chronic obstructive pulmonary disease; CS, current smoker; FS, former smoker; GI, gastrointestinal; HD, heart disease; ICD, International Classification of Diseases; RR, relative risk; SHS, secondhand smoke.
SAF and SAFSHS
We calculated the SAF for each component of costs by disease, gender and age group (35–49, 50–64 and ≥65 years). Based on two fundamental data elements, smoking prevalence and relative risk (RR) of disease-specific death for smoking, the SAF for death measures can be calculated using the following epidemiological formula: 10 11
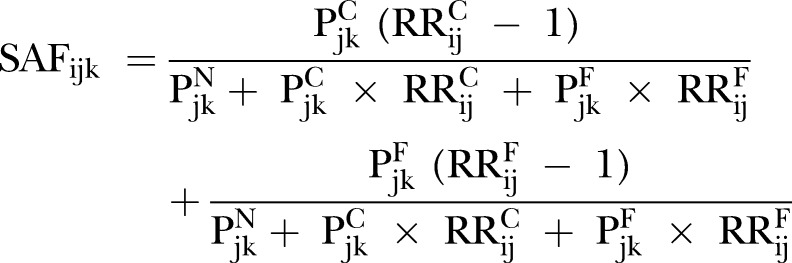 |
1 |
where PN, PC and PF denote the prevalence of never-smokers, current smokers and former smokers, respectively; RRC (or RRF) denotes the RR of disease-specific death for current (or former) smokers in comparison to never-smokers; the subscript i denotes disease, j denotes gender and k denotes age group. Note that (RRC−1) denotes the excess risk of disease-specific death for current smokers over never-smokers, and similarly, (RRF−1) denotes the excess risk of disease-specific death for former smokers over never-smokers. The first term of equation (1) is the SAF for current smokers, and the second term is the SAF for former smokers.
Prevalence rates of current smokers, former smokers and never-smokers among adults aged 35 and older were obtained from the ASBS data. The RR of death for smokers is defined as the ratio of the death rate for smokers to that for never-smokers. Given the huge body of scientific evidence that smokers have a greater risk of mortality compared with never-smokers, the RR should be greater than 1 and the excess risk should be greater than 0. The disease-specific RRs for current smokers (RRC) specific among Taiwanese adults were taken from the two aforementioned epidemiological studies in Taiwan16 17; however, the disease-specific RRs for former smokers (RRF) were not available in published sources. Instead of adopting the assumption that the RRF equals 1 and forcing the SAF for former smokers to become 0, as other studies have done,8 9 we derived a proxy measure for the RRF based on the assumption that the ratio between the excess risk for former smokers and the excess risk for current smokers is the same for any disease-specific death and all-cause death. Fortunately, in the same data sources which provided the disease-specific RRC, the all-cause RRC (RRAC) and the all-cause RRF (RRAF) were also provided.16 17 Based on these RR data and our assumption, we estimated the disease-specific RRF via the following calculation: (RRC−1)×(RRAF−1)/(RRAC−1)+1.
To estimate the SAF for healthcare costs, we assumed the RRs of disease-specific healthcare cost for current and former smokers were the same as those of disease-specific death for current and former smokers because of data limitation.
Similarly, based on two fundamental data elements, prevalence of SHS exposure and RR of disease-specific death or illness for SHS exposure, we calculated the SAFSHS among non-smokers for each component of costs by disease, gender and age group as:
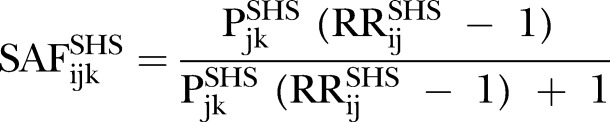 |
2 |
where PSHS denotes the prevalence of SHS exposure among non-smokers, and RRSHS is the RR of disease-specific death or illness for exposed non-smokers compared with unexposed non-smokers.
Prevalence rates of SHS exposure among non-smokers aged 35 and older were obtained from the ASBS data. Non-smokers included never-smokers and former smokers. SHS exposed non-smokers were those who either answered ‘yes’ to the question: “During the past week has anyone smoked in front of you at home?” or those who were employed and worked in indoor settings and answered ‘yes’ to the question: “During the past week has anyone smoked in front of you at your workplace?” The RRSHS of disease-specific death and the RRSHS of disease-specific illness were obtained from published sources as reported by the California EPA18 and WHO.19 20
The RRs for each disease and each cause of death for current smokers, former smokers and SHS exposure are shown in table 1.
Direct costs
Expenditures paid by the NHI for inpatient hospitalisations and outpatient visits were included as direct costs. Expenditures for prescribed medications during the hospitalisations or outpatient visits were included in the respective inpatient or outpatient expenditure categories. Outpatient visits comprised ambulatory care visits at outpatient or emergency departments of hospitals, and those at western medicine clinics. The smoking-attributable inpatient or outpatient expenditure for each subgroup stratified by disease, gender and age was calculated by multiplying the SAF by the total annual inpatient or outpatient expenditures for that subgroup.
The SHS-attributable inpatient or outpatient expenditure for each disease was derived by multiplying the SAFSHS by the total annual inpatient or outpatient expenditures for that disease among non-smokers. Because the NHI claims database does not contain individuals’ smoking statuses, it does not allow for distinguishing health expenditures for smokers from those for non-smokers. We determined the amount of total inpatient (similarly, outpatient) expenditures for non-smokers (INPNON) using the following method as used by two recent studies.19 21
 |
3 |
where INP is total annual inpatient expenditures among all individuals regardless of smoking status, PC is the prevalence of current smokers and SAFC is the SAF for current smokers as expressed by the first term of equation (1).
Indirect mortality costs
For each subgroup stratified by gender and 5-year age group, we estimated the number of smoking-attributable deaths (SAD) for each disease by multiplying the SAF by the total number of deaths for that disease. The number of smoking-attributable years of potential life lost (YPLLs) was estimated by the product of the SAD and life expectancy remaining at the age of death. Smoking-attributable mortality cost was estimated by the product of the SAD and the present value of lifetime earnings (PVLEs) expected at the age of death. The PVLEs were calculated by gender and 5-year age groups based on a human capital approach developed by Max et al.22 A discount rate of 3% was used to convert the earnings into their current worth. A growth rate of 4%, which was approximately the average annual growth rate of gross domestic product (GDP) in Taiwan during 2005−2009, was used to take into account the potential growth of future earnings.
We estimated the number of SHS-attributable deaths, YPLLs and mortality costs following the same approach as described for active smoking-attributable indirect mortality measures except that the estimation only focused on non-smokers. Total number of deaths among non-smokers was determined using a similar method as described for equation (3).
Indirect morbidity costs
We defined smoking-attributable indirect morbidity cost as the value of time lost from work due to active or passive smoking-caused illness. The lost time from work is commonly measured by the number of workloss days23; however, because the data on workloss days by disease were not available, we used inpatient days as a proxy. The smoking-attributable indirect morbidity cost for each subgroup stratified by disease, gender and age was calculated by the product of the SAF, total annual inpatient days for that group, the proportion of the population currently employed and daily earnings among employed persons.
Likewise, the SHS-attributable indirect morbidity cost was estimated by multiplying the SAFSHS by total annual inpatient days among non-smokers, employment rate and daily earnings. Total number of inpatient days among non-smokers was determined using a similar method as described for equation (3).
Sensitivity analysis
To evaluate whether or not implementation of the 2009 Act in Taiwan was associated with decreases in active and passive smoking-attributable costs, we simulated what the cost estimates would be in 2010 by assuming two scenarios: smoking prevalence and SHS exposure rates remained at the same levels as in 2008, and smoking prevalence and SHS exposure rates were at the mean value of the 2008 and 2010 levels. We also performed sensitivity analyses to see how sensitive our cost estimates were to different assumptions about the RR values and productivity growth rates.
Results
In 2010, the total population of Taiwan was 23.2 million. Among the 12.4 million adults aged 35 and older, 2.3 million were current smokers. The smoking prevalence and SHS exposure rates by gender and age in 2008 and 2010 are shown in table 2. In 2010, smoking prevalence rates among men were about 10 times as high as those among women: 33.9% vs 3.8% for current smoking, and 15.7% vs 1.5% for former smoking. The SHS exposure rates among non-smokers were similar between men and women. From 2008 to 2010, the current smoking prevalence among men decreased by nearly 10% and SHS exposure among both genders decreased by 13%.Table 3 shows the deaths and YPLLs attributed to smoking and SHS exposure by cause of death and gender. The three leading causes of SAD among men were lung cancer, ischaemic heart disease and chronic airway obstruction, and among women were cancers of liver/gallbladder/bile ducts, lung cancer and ischaemic heart disease. The leading cause of SHS-associated deaths was stroke for both genders. There was a substantial gender difference in the number of active SAD—13 744 for men and 615 for women. SHS exposure almost equally affected both genders by contributing to 613 deaths among men and 583 deaths among women. Smoking and SHS exposure contributed to a total of 15 555 deaths, which comprised about 20% of the total 19-cause deaths (77 953) among persons aged 35+ and 11% of the total all-cause deaths (144 709) among persons aged 0+. They were responsible for 284 765 YPLLs, averaging 18.3 years/death.
Table 2.
Prevalence (%) of smoking and SHS exposure by gender and age among adults aged 35 and older: Taiwan, 2008 and 2010
| 2008* |
2010* |
|||||
|---|---|---|---|---|---|---|
| Smoking |
SHS exposure† | Smoking |
SHS exposure† | |||
| CS | FS | CS | FS | |||
| Total | 21.6 | 7.8 | 28.3 | 19.2 | 8.8 | 24.7 |
| Male | 37.5 | 14.0 | 28.2 | 33.9 | 15.7 | 24.1 |
| 35–49 | 47.6 | 15.2 | 30.0 | 43.9 | 16.7 | 24.6 |
| 50–64 | 37.4 | 18.7 | 30.0 | 31.5 | 23.6 | 22.4 |
| 65+ | 29.1 | 26.8 | 17.0 | 19.5 | 30.1 | 12.9 |
| Female | 4.8 | 1.2 | 28.3 | 3.8 | 1.5 | 25.2 |
| 35–49 | 5.9 | 1.1 | 33.0 | 4.8 | 1.7 | 29.5 |
| 50–64 | 1.6 | 1.0 | 25.8 | 2.0 | 1.1 | 21.5 |
| 65+ | 1.9 | 1.0 | 13.8 | 1.3 | 1.0 | 13.2 |
*Source: Adult Smoking Behavior Survey in Taiwan.
†Percentage of non-smokers who are exposed to SHS in the home or at the workplace.
CS, current smoker; FS, former smoker; SHS, secondhand smoke.
Table 3.
Total deaths, SAM and SAYPLL by cause of death and gender among adults aged 35 and older: Taiwan, 2010
| Cause of death | Male |
Female |
||||
|---|---|---|---|---|---|---|
| Death* | SAM | SAYPLL | Death* | SAM | SAYPLL | |
| Smoking-related death | 49 563 | 13 744 | 252 954 | 28 390 | 615 | 12 244 |
| Cancers | ||||||
| Lip/oral cavity/pharynx | 2705 | 1135 | 29 214 | 338 | 0 | 0 |
| Oesophagus | 1455 | 715 | 17 356 | 106 | 24 | 493 |
| Stomach | 1440 | 310 | 5102 | 808 | 0 | 0 |
| Rectum | 827 | 250 | 4397 | 522 | 0 | 0 |
| Liver/gallbladder/bile ducts | 5663 | 920 | 19 031 | 2516 | 181 | 3682 |
| Lung | 5388 | 2198 | 34 801 | 2724 | 129 | 2988 |
| Cervix uteri | 0 | 0 | 0 | 687 | 72 | 2010 |
| Cardiovascular diseases | ||||||
| Rheumatic HD | 45 | 0 | 0 | 76 | 11 | 212 |
| Ischaemic HD | 4921 | 1467 | 23 279 | 2862 | 124 | 1802 |
| Cardiac arrest and other HD | 4141 | 816 | 14 119 | 3200 | 0 | 0 |
| Cerebrovascular disease | 5910 | 1225 | 19 805 | 4142 | 0 | 0 |
| Respiratory diseases | ||||||
| Chronic bronchitis | 104 | 47 | 518 | 62 | 0 | 0 |
| Asthma | 261 | 0 | 0 | 242 | 24 | 366 |
| Chronic airway obstruction | 3254 | 1253 | 12 928 | 908 | 0 | 0 |
| Digestive system diseases | ||||||
| Peptic ulcer, GI haemorrhage | 361 | 160 | 2350 | 190 | 51 | 689 |
| Liver cirrhosis | 3367 | 1065 | 28 538 | 1388 | 0 | 0 |
| Other diseases | ||||||
| Diabetes mellitus | 4043 | 689 | 11 477 | 4139 | 0 | 0 |
| Kidney disease | 2071 | 677 | 9831 | 2001 | 0 | 0 |
| Accidents | 3604 | 817 | 20 207 | 1479 | 0 | 0 |
| SHS-associated death | 613 | 9768 | 583 | 9799 | ||
| Lung cancer | 5388 | 131 | 2078 | 2724 | 117 | 2584 |
| Ischaemic HD | 4921 | 104 | 1652 | 2862 | 86 | 1222 |
| Cerebrovascular disease | 5910 | 353 | 5677 | 4142 | 354 | 5603 |
| Asthma | 261 | 25 | 361 | 242 | 27 | 390 |
| Total† | 49 563 | 14 357 | 262 722 | 28 390 | 1198 | 22 043 |
*Number of deaths among people aged ≥35 regardless of their smoking and SHS exposure status.
†Total deaths from 19 smoking-related diseases which overlap with the four SHS-associated diseases.
GI, gastrointestinal; HD, heart disease; SAM, smoking and SHS-attributable mortality; SAYPLL, smoking and SHS-attributable years of potential life lost; SHS, secondhand smoke.
Table 4 shows the total direct and indirect costs attributed to smoking and SHS exposure by gender, age and disease. The total economic costs of smoking and SHS exposure in 2010 amounted to US$1670 million, including US$828 million (50%) in direct costs, US$820 million (49%) in indirect mortality costs and US$22 million (1%) in indirect morbidity costs. The share of the total costs was greater from active smoking (92%) than SHS exposure (8%), and greater for men (92%) than women (8%). The total economic costs averaged US$72/Taiwanese aged 0+ and US$718/adult smoker aged 35+. Based on Taiwan's total cigarette consumption of 1894 million packs in 2010, the total economic costs averaged US$0.88/pack, about 43% the 2010 average retail price of cigarettes (NT$65 or US$2.05).12
Table 4.
Total economic costs of smoking and SHS exposure by component of costs, gender, age and disease for adults aged 35 and older: Taiwan, 2010 (unit: US$1000)
| Direct costs |
Indirect costs |
Total economic costs | ||||
|---|---|---|---|---|---|---|
| Inpatient | Outpatient | Subtotal | Morbidity cost | Mortality cost | ||
| Smoking | 268 941 | 473 003 | 741 943 | 18 669 | 782 595 | 1 543 208 |
| SHS exposure | 39 179 | 46 894 | 86 073 | 3407 | 36 968 | 126 448 |
| Male | 274 288 | 467 438 | 741 726 | 18 932 | 782 515 | 1 543 173 |
| Female | 33 832 | 52 458 | 86 290 | 3144 | 37 049 | 126 484 |
| 35–49 | 61 319 | 114 908 | 176 228 | 10 797 | 472 607 | 659 631 |
| 50–64 | 106 579 | 204 427 | 311 006 | 9601 | 269 320 | 589 927 |
| 65+ | 140 222 | 200 561 | 340 783 | 1678 | 77 637 | 420 098 |
| Lung cancer | 21 191 | 31 552 | 52 743 | 1249 | 86 729 | 140 721 |
| Ischaemic HD | 66 157 | 38 128 | 104 285 | 1615 | 62 728 | 168 628 |
| Cerebrovascular disease | 46 055 | 48 275 | 94 330 | 2943 | 71 882 | 169 155 |
| Other diseases* | 174 717 | 401 942 | 576 659 | 16 270 | 598 225 | 1 191 152 |
| Total | 308 120 | 519 896 | 828 016 | 22 076 | 819 564 | 1 669 656 |
Exchange rate of the NT$ against US$1=31.642 in 2010.
*‘Other’ includes all the other smoking or SHS-related diseases.
HD, heart disease; SHS, secondhand smoke.
Of the US$828 million in direct healthcare costs, US$104 million was spent for treating ischaemic heart disease, US$94 million for stroke and US$53 million for lung cancer. Outpatient expenditures amounted to US$520 million (63%) while inpatient expenditures were US$308 million (37%). Among the US$22 million in indirect morbidity costs, US$18.7 million was due to active smoking and US$3.4 million was due to SHS exposure. The US$820 million in mortality costs averaged US$52 688/death among the 15 555 premature deaths caused by smoking or SHS exposure.
Sensitivity analysis
Table 5 shows that if the prevalence rates of smoking and SHS exposure in 2010 had remained at the same levels as in 2008, the toll of active and passive smoking-attributable losses would have been greater by an additional 1540 deaths and US$107 million in total economic cost. If the prevalence rates of smoking and SHS exposure were at the mean values of the 2009 and 2010 levels, there would have additional 883 deaths and US$59 million loss in total economic cost.
Table 5.
Sensitivity analysis of SAM and smoking and SHS-attributable direct healthcare costs and total economic costs: Taiwan, 2010
| SAM |
Direct costs |
Total economic costs |
||||
|---|---|---|---|---|---|---|
| N | Percentage of all deaths* | Amount (US$ million) | Percentage of NHE | Amount (US$ million) | Percentage of GDP | |
| Main analysis | 15 555 | 10.75 | 828 | 3.38 | 1670 | 0.39 |
| Sensitive analysis | ||||||
| Smoking and SHS exposure prevalence | ||||||
| Assume the levels in 2008 | 17 095 | 11.81 | 894 | 3.65 | 1777 | 0.41 |
| Assume the mean levels in 2008 and 2010 | 16 438 | 11.36 | 865 | 3.53 | 1729 | 0.40 |
| Growth rate in productivity | ||||||
| Assume 6% instead of 4% | 15 555 | 10.75 | 828 | 3.38 | 1847 | 0.43 |
| RR | ||||||
| Assume RRs for former smokers=1 | 11 140 | 7.88 | 629 | 2.57 | 1323 | 0.31 |
| Assume published RRs in the USA† | 22 513 | 15.56 | 1042 | 4.25 | 2175 | 0.51 |
Exchange rate of the NT$ against US$=31.642 in 2010.
*In 2010, the number of all-cause deaths among people aged ≥0 was 144 709.
†See table 12.1 in the 2014 US Surgeon General Report.25
GDP, gross domestic product (US$430.1 billion in 2010); NHE, national personal healthcare expenditure (US$24.5 billion in 2010); RR, relative risk; SAM, smoking and SHS-attributable mortality; SHS, secondhand smoke.
If we assumed that the annual growth rate of productivity was 6% instead of 4%, total economic costs would be US$177 million higher. If we used the RR values for those smoking-related diseases reported by the widely cited American study,24 25 our estimates of active and passive smoking-attributable premature deaths and total economic costs would increase by 6958 deaths and US$505 million.
Discussion
The direct costs of smoking and SHS exposure in Taiwan amounted to US$828 million and accounted for 3.4% of Taiwan's personal healthcare expenditures in 2010. Smoking and SHS exposure also led to 15 555 premature deaths, 284 765 YPLLs, US$820 million in indirect costs of productivity losses due to premature deaths and US$22 million in indirect costs of time lost from work due to tobacco-related illness. These costs totalled US$1670 million, representing 0.4% of Taiwan's GDP and averaging about US$720/adult smoker.
The proportion of the total costs of smoking and SHS exposure to GDP in Taiwan is smaller than those estimated for other East Asian countries, such as 0.7% for China23 and 0.6–0.8% for South Korea.26 One possible explanation is because of relatively lower smoking rates in Taiwan. Another explanation may be the underestimation of our direct cost estimates which were based on the NHI claims database. The NHI database only includes health expenditures paid by the NHI, but not copayments or out-of-pocket payments that were spent on non-NHI covered health services such as orthodontics, long-term care and nursing home care. In 2010, the NHI expenditures only comprised 57% of Taiwan's personal health expenditures.27 Furthermore, due to limited data accessibility, we only included the NHI spending on inpatient care and Western medicine outpatient care. Other NHI covered health services such as Chinese medicine outpatient care accounted for 16% of the NHI expenditures in 2010.27 If copayments, out-of-pocket and other NHI covered health expenditures are counted, our direct cost estimate could be considerably larger than US$828 million.
Our estimated total costs of smoking and SHS exposure are very likely to be underestimated for several other reasons. First, we only included 19 diseases in the analyses of smoking-attributable costs. Smoking also causes many other diseases such as aortic aneurysm, atherosclerosis, pneumonia, influenza, hip fractures, rheumatoid arthritis, periodontitis, nuclear cataract and tuberculosis.25 Because the RRs of these diseases for Taiwanese smokers were not available in public sources, we did not include them in our analyses. Without considering these diseases, our assessments almost certainly underestimate the true costs of smoking. Second, we did not include children and young adults under age 35 in the analyses of SHS-attributable costs. SHS exposure has been causally linked to adverse health effects on infants and children, including low birth weight, sudden infant death syndrome, middle ear disease, chronic respiratory symptoms, asthma and attention deficit hyperactivity disorder.25 28 Third, we measured SHS exposure based on self-reported exposure in the home and workplace during the last week, but did not consider exposure that may have occurred in other public places or at an earlier time. It has been shown that self-reported SHS exposure greatly underestimates actual exposure assessed by the biomarker such as cotinine level.29 Therefore, our estimated SHS-attributable costs are most likely to be underestimated. Fourth, in estimating indirect morbidity costs, we did not count the opportunity costs of relatives or informal caregivers who took care of patients with smoking-related diseases, productivity losses due to smoking-caused disability other than inpatient days and transportation expenses incurred during inpatient and outpatient visits for the treatment of smoking-related diseases.23
A previous study by Yang et al8 also included the same 19 smoking-related diseases and used the same data source for RRs. They estimated that active smoking caused 233 223 YPLLs and US$467 million (after converting into 2010 constant dollars) in excess healthcare costs for 2001. Our corresponding estimates for 2010 are 265 198 years and US$742 million. Even though adult smoking prevalence declined significantly during 2001−2010,5 our 2010 estimates are larger than the 2001 estimates. One explanation is that Yang et al8 assumed the disease-specific RRF equal to 1, which implies former smokers have the same risk of death or illness as never-smokers. This assumption would lead to underestimation of the SAD and healthcare costs in 2001. Another explanation is that the total number of deaths from the 19 smoking-related diseases increased from 75 003 to 77 953 deaths and Taiwan's personal health expenditures rose by almost 40% in real term between 2001 and 2010.13 27
This study indicates that Taiwan's NHI spent US$828 million—6% of their budget—in 2010 to cover the excess healthcare expenditures caused by smoking and SHS exposure. These costs were borne by all Taiwan residents including never-smokers who paid for insurance premiums. Increasing cigarette taxes will help to offset the external costs of smoking imposed by smokers on others.
Tobacco control programmes are costly. In 2009, the government of Taiwan spent US$15.7 million (or NT$520 million based on the 2009 exchange rate of NT$33.049 against US$1) on tobacco control programmes.30 However, the benefits of tobacco control programmes are substantially larger. Several recent studies have shown that the 2009 Act in Taiwan was associated with a reduction in adolescent smoking31 and SHS exposure,7 and an increase in adult cessation rates.32 Assuming a half of the reduction in adult smoking prevalence and SHS exposure during 2008−2010 was driven by the 2009 Act, our sensitivity analysis results show that there was a saving in avoided smoking and SHS attributable financial losses by US$59 million a year in 2010 alone.
This study makes several contributions. First, our results indicated that the SHS-attributable medical costs, indirect morbidity costs and indirect mortality costs among adults aged ≥35 were not negligible—equalling 12%, 18% and 5% of the levels of the active smoking-attributable direct medical costs, indirect morbidity costs and indirect mortality costs, respectively. Thus, not including the impact of SHS exposure would underestimate the true burden of smoking. Second, we developed an interpolation approach to measure the disease-specific RRF in Taiwan to count smoking-attributable costs for former smokers. Smokers often quit smoking because they had developed smoking-related illness. Although the risks of heart attack and stroke fall quickly within the first 5 years after quitting,33 the risks of other tobacco-related diseases take a longer time to reverse after quitting. Therefore, assuming the RRF equal to 1 would certainly underestimate the costs of smoking when the prevalence of former smokers, especially recent quitters, is high.
This study is subject to some limitations. We used the RR of death as a proxy for the RR of healthcare utilisation and expenditures to estimate the direct cost of smoking because of data limitation. Also, our measure for disease-specific RRF was based on the assumption that the ratio between the excess risk for former smokers and the excess risk for current smokers is the same for any disease-specific death and all-cause death. To test the validity of this, we applied this approach to the widely cited American RR data which consist of disease-specific and all-cause RRs for current and former smokers and are available in the internet-based SAMMEC software.24 We found that our derived RRF follow a consistent pattern with the actual RRF across diseases. Nevertheless, epidemiological research is needed to more accurately quantify the disease-specific RRF in Taiwan. Finally, we obtained the RRs from previous epidemiological studies which followed up the vital status of two cohorts, established prior to 1992, until 2000.16 17 Owing to the changes in smoking behaviour over time, the cohort of smokers today is likely different from the cohort 20 years ago; therefore, these RR data may not reflect the true RRs of smokers in 2010. Indeed, the 2014 US Surgeon General's Report has shown that today's cigarette smokers—men and women—have a much higher risk for lung cancer and chronic obstructive pulmonary disease than smokers in the past.
Despite the limitations that certainly lead to underestimation of our estimated total economic costs of smoking and SHS exposure, we found that smoking still imposes a huge financial burden on Taiwanese society even though smoking prevalence and SHS exposure in Taiwan have declined in recent years. Thus, sustained tobacco control efforts to encourage people to quit smoking, prevent smoking uptake by children and young adults and protect all people from SHS exposure are needed.
Supplementary Material
Acknowledgments
The authors are grateful for the comments provided by Drs Kung-Yee Liang, Teh-wei Hu, Kenneth E Warner and Frank J Chaloupka.
Footnotes
Contributors: H-YS laid out the analytical framework, supervised all the steps of data analysis and revised the manuscript critically for important intellectual content. Y-WW drafted the manuscript particularly on the method parts and helped to review and interpret the results. L-CC helped obtain all the data and conducted the analyses for this study. Y-WT conceptualised the research idea, obtained the funding, drafted the manuscript and helped interpret the results. All authors reviewed and approved the final manuscript.
Funding: This study was funded by Health Promotion Administration, Ministry of Health and Welfare, Taiwan (grant CCY 10009-102).
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Campaign for Tobacco-Free Kids. The global cigarette industry. June 2013. http://global.tobaccofreekids.org/files/pdfs/en/Global_Cigarette_Industry_pdf.pdf (accessed 1 Mar 2014).
- 2.Katanoda K, Jiang Y, Park S, et al. Tobacco control challenges in East Asia: proposals for change in the world's largest epidemic region. Tob Control 2014;23:359–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Report on the global tobacco epidemic, 2008: the MPOWER package. Geneva, 2008 [Google Scholar]
- 4.Wen CP, Cheng TY, Eriksen MP, et al. The impact of the cigarette market opening in Taiwan. Tob Control 2005;14(Suppl 1):i4–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ministry of Health and Welfare, Taiwan. 2012 Taiwan tobacco control annual report. Executive Yuan, Taipei: Health Promotion Administration, 2013 [Google Scholar]
- 6.World Health Organization. Framework convention on tobacco control. Geneva, 2003 [Google Scholar]
- 7.Tsai YW, Chang LC, Sung HY, et al. The impact of smoke-free legislation on reducing exposure to secondhand smoke: differences across gender and socioeconomic groups. Tob Control. Published Online First: 6 September 2013. doi:10.1136/tobaccocontrol-2013-051004 [DOI] [PubMed] [Google Scholar]
- 8.Yang MC, Fann CY, Wen CP, et al. Smoking attributable medical expenditures, years of potential life lost, and the cost of premature death in Taiwan. Tob Control 2005;14(Suppl 1):i62–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chung CW, Wang JD, Yu CF, et al. Lifetime medical expenditure and life expectancy lost attributable to smoking through major smoking related diseases in Taiwan. Tob Control 2007;16:394–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sung HY, Max W, Gajalakshmi V, et al. eds Economics of tobacco toolkit: assessment of the economic costs of smoking. Geneva: World Health Organization, 2011 [Google Scholar]
- 11.Lilienfeld DE, Stolley PD. Foundations of epidemiology. 3rd edn New York, USA: Oxford University Press, 1994 [Google Scholar]
- 12.Ministry of Interior, Taiwan. 2012 Statistical yearbook of interior. Executive Yuan, Department of Statistics, 2013. http://sowf.moi.gov.tw/stat/year/list.htm (accessed 15 Aug 2013). [Google Scholar]
- 13.Ministry of Health and Welfare, Taiwan. 2010 Statistics of causes of death. Executive Yuan. http://www.mohw.gov.tw/EN/Ministry/Statistic.aspx?f_list_no=474&fod_list_no=3480 (accessed 13 Jun 2013).
- 14.Ministry of the Interior, Taiwan. 2010 Abridged life table in Taiwan. Executive Yuan. http://sowf.moi.gov.tw/stat/english/elife/elist.htm (accessed 14 Apr 2013).
- 15.Directorate-General of Budget, Accounting and Statistics, Taiwan. 2010 Report on the Manpower Utilization Survey. Executive Yuan. http://www.dgbas.gov.tw/lp.asp?ctNode=4987&CtUnit=1183&BaseDSD=7 (accessed 15 May 2013).
- 16.Wen CP, Tsai SP, Chen CJ, et al. Smoking attributable mortality for Taiwan and its projection to 2020 under different smoking scenarios. Tob Control 2005;14(Suppl 1):i76–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wen CP, Tsai SP, Chen CJ, et al. The mortality risks of smokers in Taiwan: part I: cause-specific mortality. Prev Med 2004;39:528–35 [DOI] [PubMed] [Google Scholar]
- 18.California Environmental Protection Agency. Proposed identification of environmental tobacco smoke as a toxic air contaminant. Sacramento, CA: California Environmental Protection Agency, Office of Environmental Health Hazard Assessment, 2005 [Google Scholar]
- 19.Öberg M, Jaakkola MS, Woodward A, et al. Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. Lancet 2011;377:139–46 [DOI] [PubMed] [Google Scholar]
- 20.Öberg M, Jaakkola MS, Prüss-Üstün A, et al. Second-hand smoke: assessing the environmental burden of disease at national and local levels. Geneva: World Health Organization, 2010. (WHO Environmental Burden of Disease Series, No. 18). [Google Scholar]
- 21.Max W, Sung HY, Shi Y. Deaths from secondhand smoke exposure in the United States: economic implications. Am J Public Health 2012;102:2173–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Max W, Rice DP, Sung HY, et al. Valuing human life: estimating the present value of lifetime earnings. http://repositories.cdlib.org/ctcre/esarm/PVLE2000 (accessed 8 May 2013).
- 23.Yang L, Sung HY, Mao Z, et al. Economic costs attributable to smoking in China: update and an 8-year comparison, 2000-2008. Tob Control 2011;20:266–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Adult SAMMEC: smoking-attributable mortality, morbidity, and economic costs. (Online software). Atlanta, GA: Centers for Disease Control and Prevention; https://apps.nccd.cdc.gov/sammec/show_esaf_data.asp (accessed 8 May 2013). [Google Scholar]
- 25.US Department of Health and Human Services. The health consequences of smoking: 50 years of progress. A report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014 [Google Scholar]
- 26.Kang HY, Kim HJ, Park TK, et al. Economic burden of smoking in Korea. Tob Control 2003;12:37–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ministry of Health and Welfare, Taiwan. 2010 National Health Expenditure. Executive Yuan, 2011 [Google Scholar]
- 28.Max W, Sung HY, Shi Y. Attention deficit hyperactivity disorder among children exposed to secondhand smoke: a logistic regression analysis of secondary data. Int J Nurs Stud 2012;50:797–806 [DOI] [PubMed] [Google Scholar]
- 29.Max W, Sung HY, Shi Y. Who is exposed to secondhand smoke? Self-reported and serum cotinine measured exposure in the US, 1999-2006. Int J Environ Res Public Health 2009;6:1633–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chiou S. Smoking cessation services and tobacco control [in Chinese]. Taipei, Taiwan: Health Promotion Administration, Ministry of Health and Welfare, R.O.C. (Taiwan), 2012. http://www.tma.tw/se_dis/42.asp (accessed 21 May 2014). [Google Scholar]
- 31.Huang SL, Lin IF, Chen CY, et al. Impact of tobacco control policies on adolescent smoking: findings from the global youth tobacco survey in Taiwan. Addiction 2013;108:1829–35 [DOI] [PubMed] [Google Scholar]
- 32.Chang FC, Sung HY, Zhu SH, et al. Impact of the 2009 Taiwan tobacco hazards prevention act on smoking cessation. Addiction 2014;109:140–6 [DOI] [PubMed] [Google Scholar]
- 33.US Department of Health and Human Services. How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease. A report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2010. http://www.surgeongeneral.gov/library/reports/tobaccosmoke/ (accessed 11 Nov 2013). [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


