Abstract
OBJECTIVES
Dysphagia may develop following antireflux surgery as a consequence of poor esophageal peristaltic reserve. We hypothesized that suboptimal contraction response following multiple rapid swallows (MRS) could be associated with chronic transit symptoms following antireflux surgery.
METHODS
Wet swallow and MRS responses on esophageal high-resolution manometry (HRM) were characterized collectively in the esophageal body (distal contractile integral (DCI)), and individually in each smooth muscle contraction segment (S2 and S3 amplitudes) in 63 patients undergoing antireflux surgery and in 18 healthy controls. Dysphagia was assessed using symptom questionnaires. The MRS/wet swallow ratios were calculated for S2 and S3 peak amplitudes and DCI. MRS responses were compared in patients with and without late postoperative dysphagia following antireflux surgery.
RESULTS
Augmentation of smooth muscle contraction (MRS/wet swallow ratios > 1.0) as measured collectively by DCI was seen in only 11.1% with late postoperative dysphagia, compared with 63.6% in those with no dysphagia and 78.1% in controls (P≤0.02 for each comparison). Similar results were seen with S3 but not S2 peak amplitude ratios. Receiver operating characteristics identified a DCI MRS/wet swallow ratio threshold of 0.85 in segregating patients with late postoperative dysphagia from those with no postoperative dysphagia with a sensitivity of 0.67 and specificity of 0.64.
CONCLUSIONS
Lack of augmentation of smooth muscle contraction following MRS is associated with late postoperative dysphagia following antireflux surgery, suggesting that MRS responses could assess esophageal smooth muscle peristaltic reserve. Further research is warranted to determine if antireflux surgery needs to be tailored to the MRS response.
INTRODUCTION
Provocative maneuvers during esophageal manometry, particularly high-resolution manometry (HRM), are increasingly utilized to uncover subtle motor characteristics. The simplest provocative maneuver is multiple rapid swallows (MRS), where five swallows are administered in rapid sequence (1,2). MRS results in profound inhibition of the esophageal body and lower esophageal sphincter (LES) tone during sequential swallows. After the final swallow in the sequence, there is robust esophageal body contraction and LES tone is regained (Figure 1). Intact neural connections and muscle function are required for an intact MRS response (1). Two broad categories of abnormalities can be seen with multiple rapid swallows: (i) incomplete inhibition wherein contraction fragments are seen during the expected phase of inhibition and (ii) suboptimal contraction wherein there is failure of augmentation of contraction in the sequence following the last swallow of the series (Figure 1). In extreme settings, contraction may fail altogether (2,3). We have previously reported that an abnormal MRS response using these crude measures can be associated with dysphagia after antireflux surgery (2).
Figure 1.

Smooth muscle contraction response to multiple rapid swallows (MRS). A normal response (left panel) consists of profound inhibition of esophageal body peristalsis and lower esophageal sphincter (LES) tone during the repetitive swallows, followed by robust contraction of the smooth muscle esophagus and LES aftercontraction. The right panel depicts absent contraction response, with no smooth muscle contraction evident following multiple swallows.
Low-amplitude distal esophageal contraction, also termed ineffective esophageal motility or weak peristalsis, may not generate enough intraluminal pressure to overcome resistance at the gastroesophageal junction, which can contribute to nonobstructive dysphagia (4,5). The ability to predict the potential for augmentation of esophageal body contraction can be of value to the clinician assessing weak peristalsis, as this would identify retained peristaltic reserve in the esophagus. Identification of patients with such peristaltic reserve would be particularly useful in the evaluation of nonobstructive dysphagia, and in preoperative counseling of postoperative expectations in patients undergoing antireflux surgery. In this context, it would also be beneficial to identify those not at risk for postoperative dysphagia in whom a standard wrap could be performed. However, there are currently no good parameters that can reliably predict esophageal peristaltic reserve.
We hypothesized that a suboptimal contraction response following multiple rapid swallows indicates poor peristaltic reserve, either at a neural or a muscular level, which could be associated with chronic transit symptoms following antireflux surgery. To test this hypothesis, we first characterized MRS response collectively in the esophageal body, and individually in each smooth muscle contraction segment in healthy controls, using HRM software tools. Using this as a yardstick, we determined if MRS responses on preoperative HRM in patients undergoing laparoscopic anti-reflux surgery associated with the persistence of postoperative dysphagia after antireflux surgery.
METHODS
Patients referred for antireflux surgery undergoing preoperative esophageal HRM for assessment of peristaltic function were eligible for enrollment into this study. To qualify for inclusion, subjects had to have documented gastroesophageal reflux disease (GERD; upper endoscopy with erosive esophagitis, Barrett’s esophagus, and/or an abnormal pH study) and one adequately performed MRS sequence on preoperative HRM, consisting of at least four 2-ml water swallows performed in rapid succession, with ≤4-s interval between swallows. Furthermore, patients were required to have completed a preoperative and at least one postoperative symptom questionnaire detailing symptom frequency and severity, and a global symptom score (GSS). Exclusion criteria included surgery for indications other than GERD, prior foregut resections, and unintelligible studies with artifacts limiting evaluation. A cohort of 18 asymptomatic subjects constituted the controls for this study; all underwent esophageal HRM and adequate MRS. This study protocol was approved by the Human Research Protection Office (institutional review board) at Washington University School of Medicine, St Louis, MO. The data and analysis described in this report represent additional analysis of an existing data set from which preliminary conclusions have been previously published (2).
Symptom assessment
All patients completed pre- and postoperative symptom questionnaires. Patients referred to our motility center are uniformly requested to complete this questionnaire, which was developed a priori and validated for use in outcome assessments in patients undergoing esophageal function studies at our institution (6–8). Questionnaires were administered at the initial HRM and repeated at each postoperative follow-up visit with the surgeon (L.M.B.). For this study, only dysphagia was evaluated, and patients with dysphagia as the dominant or presenting clinical symptom were identified. Dysphagia for solids and liquids were scored for severity and frequency on the 5-point Likert scales (0 = none, 4 = frequent, severe), and the product constituted the symptom score. The composite score was the sum of scores for solid and liquid dysphagia and this had to be zero for the designation of “no dysphagia.” Late dysphagia was defined as symptoms persisting beyond or occurring > 3 months after antireflux surgery. Symptomatic patients were evaluated per routine clinical practice with upper endoscopy and endoscopic dilation when appropriate.
Motor assessment
Peak contraction amplitudes were assessed separately in the proximal S2 and distal S3 smooth muscle contraction segments. They were evaluated collectively using the distal contractile integral (DCI) (9). These values were averaged for 10 wet swallows and for the MRS response. MRS response was also evaluated by the presence of abnormal inhibition and/or abnormal contractile response. A designation of abnormal inhibition was made when contraction segments > 3 cm in length at > 30 mm Hg occurred during the course of multiple swallows. A designation of abnormal contractile response was made if S2, S3, or both S2 and S3 failed to form. The MRS/wet swallow ratios were calculated for S2 and S3 peak amplitudes, and for DCI. The MRS response was analyzed and compared in postoperative dysphagia groups, particularly the late dysphagia group.
Surgical technique
Antireflux surgery was performed according to standard technique by a single surgeon to ensure uniformity. A 360-degree fundoplication was performed in all instances, over a 54-French bougie, with three interrupted sutures of 0-polyester suture as per standard technique (2). Therefore, this study cohort only reflects patients with a wet swallow profile deemed adequate for a standard 360-degree fundoplication. In our institution, patients undergo a partial fundoplication if the averaged contraction amplitude is < 30 mm Hg or if peristaltic failure occurs in > 80% of wet swallows; none of the patients in this cohort had these characteristics. MRS responses were not analyzed as part of the routine clinical HRM report, and were therefore not available to the surgeon at the time of antireflux surgery. Patients were followed up at regular intervals; if symptomatic, they were asked to return for an unscheduled follow-up appointment.
Statistical analysis
Data are reported as mean±s.e.m. or median (interquartile range) as appropriate. Intergroup differences were compared using χ2 test or Fisher’s exact test for categorical values and Student’s t-test for continuous values. Means and 95% confidence intervals were calculated from MRS/wet swallow ratios for healthy controls. Proportions of MRS responses within and below the 95% confidence interval range of normal cohort were determined for the antireflux surgery patients. Proportions with augmentation of contraction, defined as the MRS/wet swallow ratios of > 1 for S2, S3, and DCI, were determined. These proportions were compared between early dysphagia, late dysphagia (> 3 mo after antireflux surgery), and no dysphagia, using receiver operating characteristic analysis to identify segregating thresholds. In all instances, a P value of < 0.05 was required for statistical significance.
RESULTS
During the study period, 63 patients (mean age 60.3±1.7 years, 48 female) with an adequate MRS sequence during HRM (range 4–6 swallows, median 5 swallows) underwent antireflux surgery and fulfilled other study inclusion criteria. All subjects had adequate esophageal motor characteristics to sustain a standard Nissen fundoplication; none of the subjects had esophageal outflow obstruction or esophageal body aperistalsis precluding such surgery. Mean wave amplitude in the distal esophagus (average of values at 3, 7, and 11 cm proximal to the LES) was 70.8±3.9 mm Hg. Criteria for major motor disorders were not met by any patient, using published Chicago Classification characteristics. Only 5% had > 50% failed sequences on wet swallows, and none had > 70% failed sequences. In addition, 8 patients (12.7%) had contraction wave abnormalities (double peaked waves) not meeting Chicago Classification characteristics, and 21 (33.3%) had basal end-expiratory LES pressures < 5 mm Hg. The comparison normal cohort consisted of 18 asymptomatic subjects (mean age 28±0.7 years, 9 female); none of these subjects reported any dysphagia and had normal esophageal motor findings.
Dysphagia characteristics were further evaluated in the study population. The mean preoperative composite dysphagia score was 3.2±1.1 and GSS was 3.3±0.3. Preoperative dysphagia was reported by 28 subjects (44.4%, composite dysphagia score 10.6±1.9, GSS 4.5±0.4). Of these, 10 patients had complete resolution of dysphagia after antireflux surgery, and another 6 patients had resolved dysphagia after transiently developing early postoperative dysphagia. Composite dysphagia score improved to 3.5±1.2, and GSS to 2.0±0.4 following antireflux surgery in this subgroup (P<0.05 compared with preoperative scores), suggesting that etiology of preoperative dysphagia was reflux related in most instances. Postoperative dysphagia was further characterized. Early postoperative dysphagia was reported by 34 patients (54.0%, mean 1.2±0.1 months after antireflux surgery) and late dysphagia by 18 patients (28.6%, mean 13.9±1.0 months, range 3.1–25.7 months after antireflux surgery,). Within the late postoperative dysphagia group, 12 (66.7%) also had early postoperative dysphagia, 8 (44.4%) had both preoperative and early postoperative dysphagia, and 4 (22%) had only preoperative dysphagia. Twenty-two patients (34.9%) had no postoperative dysphagia at any point. The prevalence of preoperative dysphagia was significantly associated with postoperative dysphagia (P = 0.0014), but composite preoperative dysphagia score and GSS were similar regardless of whether patients developed late postoperative dysphagia.
MRS parameters were first defined in normal controls, where 180 wet swallows were recorded. Collectively, augmentation of contraction was noted following MRS in all normal controls, and 61.1% had complete and profound inhibition during MRS. On further analysis, S2 and S3 peak amplitudes and DCI augmented after MRS (Table 1). This augmentation was most profound for DCI (mean 52.0% increment) and for S3 peak amplitude (mean 25.1% increment); S2 peak amplitude increased by a mean of only 7.0% (Table 1). The integrated relaxation pressure decreased by a mean of 45.7% because of profound inhibition during MRS. To further quantitate the MRS response, MRS/wet swallow ratios were calculated individually for each subject and then averaged. Physiologically, augmentation of contraction is expected, represented by the MRS/wet swallow ratio of > 1.0. This was collectively achieved for all three measured parameters in the normal control cohort (Table 1). On further analysis of normal controls, the threshold ratio of 1.0 was met by 78.1% for DCI, 88.9% for S2 peak amplitude, and 94.6% for S3 peak amplitude.
Table 1.
MRS parameters in normal controls and patients undergoing antirefl ux surgery
| Wet swallows |
MRS | MRS/wet swallow ratio (95% CI) |
|
|---|---|---|---|
| Normal controls | |||
| S2 peak amplitude (mm Hg) |
97.8±9.8 | 104.6±13 | 1.3 (1.2–1.4) |
| S3 peak amplitude (mm Hg) |
129.9±9.9 | 162.5±16* | 1.5 (1.4–1.7) |
| DCI (mm Hg cm s) | 1,614±295 | 2,454±475* | 1.8 (1.4–2.2) |
| IRP (mm Hg) | 4.6±0.5 | 2.5±0.4* | |
| Antireflux surgery | |||
| S2 peak amplitude (mm Hg) |
79.1±4.3 | 82.4±3.6 | 0.57 (0.4–0.7) |
| S3 peak amplitude (mm Hg) |
108.7±4.9 | 115.6±5.2 | 0.76 (0.6–0.9) |
| DCI (mm Hg cm s) | 1,164±106 | 1,307±125 | 0.98 (0.8–1.2) |
| IRP (mm Hg) | 6.0±0.7 | 4.0±0.7* |
CI, confidence interval; DCI, distal contractile integral; IRP, integrated relaxation pressure; MRS, multiple rapid swallow.
P<0.05 compared with wet swallows.
A total of 630 swallows were evaluated in patients undergoing antireflux surgery. Of these, peristaltic sequences were detected in 83.2% of wet swallows and 73.0% of post-MRS sequences. This translated into a crude MRS contractile response in 43 patients (68.3%) with at least some contractile activity in the smooth muscle esophagus, and 46 (73.0%) demonstrated complete inhibition of contraction during the multiple swallows. Peristaltic responses were further analyzed in patients undergoing antireflux surgery within parameters reported above in normal controls. Esophageal body wet swallow parameters were lower than that seen in normal controls (Table 1). Collectively, mean increment in S2 peak amplitude was 4.2%, S3 peak amplitude 6.3%, and DCI 12.3%, the latter two significantly lower than that recorded in normal controls. These findings reflect a trend toward hypomotility in the GERD population undergoing antireflux surgery. Relaxation of the LES, however, remained profound, with a 33.3% decline in integrated relaxation pressure during MRS. In contrast to the normal cohort, mean MRS/wet swallow ratios were uniformly < 1 (Figure 2) in all three esophageal body parameters analyzed.
Figure 2.

Analysis of multiple rapid swallow (MRS) responses in the smooth muscle esophagus. MRS/wet swallow ratios individually for second (S2) and third (S3) smooth muscle contraction segments, and collectively using distal contractile integral (DCI). Averaged ratios (solid lines) were consistently < 1.0 for all three parameters. Ratios were separately averaged for patients with and without late postoperative dysphagia, depicted as dashed and dotted lines, respectively.
A normal contractile response (within 95% confidence intervals of the normal response) was seen for S2 peak amplitude in 14.2%, S3 peak amplitude in 11.1%, and DCI in 22.2% in patients undergoing antireflux surgery (Figure 3). When augmentation of the esophageal body contractile response, defined as the MRS/wet swallow ratio of > 1, was evaluated, DCI augmented the best, with 29 (46.0%) demonstrating augmentation. S3 peak amplitude similarly augmented in 39.7%, and S2 peak amplitude augmented in 27.0% (Figure 3). As a group, these proportions were significantly lower than in normal controls. Contractile responses were further segregated by timing of postoperative dysphagia after antireflux surgery, and compared with normal controls (Table 2). Using a threshold > 1.0, only 11.1%, 11.1%, and 16.7% of patients with late dysphagia demonstrated a normal DCI, S2, or S3 ratio > 1.0, respectively. These proportions were much lower than those with no dysphagia or even early dysphagia. These differences were statistically significant across all the groups, and individually significantly different from controls.
Figure 3.
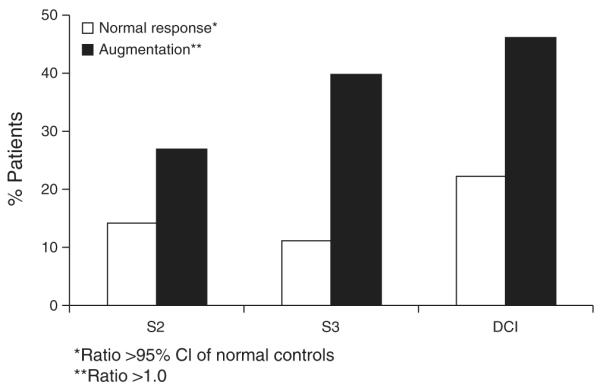
Description of smooth muscle contraction responses after multiple rapid swallows (MRS). Proportions of patients undergoing antireflux surgery with normal responses to MRS, and augmentation of contraction are depicted for each of S2 and S3 peak amplitudes, and distal contractile integral (DCI). Normal response represents MRS/wet swallow ratios within 95% confidence intervals (CIs) of mean values in 18 healthy controls. Augmentation represents MRS/wet swallow ratios of > 1.0. *Ratio >95% CI of normal controls; **ratio >1.0.
Table 2.
MRS responses segregated by timing of dysphagia
| Normal controls* (n=18) | Early dysphagia (n=34) | Late dysphagia (n=18) | No dysphagia (n = 22) | |
|---|---|---|---|---|
| DCI ratio > 1.0 | 78.1% | 44.1% | 11.1% | 63.6%** |
| S2 ratio > 1.0 | 88.9% | 29.4% | 11.1% | 40.9% |
| S3 ratio > 1.0 | 94.6% | 44.1% | 16.7% | 50.0%** |
DCI, distal contractile integral; MRS, multiple rapid swallow.
P≤0.002 compared with patient groups.
P≤0.02 across patient groups.
Receiver operating characteristic analysis was used to establish the best DCI, S2, and S3 ratio thresholds to segregate subjects with no dysphagia from those with late dysphagia (Figure 4). This identified DCI ratio threshold of 0.85, S2 peak amplitude ratio threshold of 0.57, and S3 peak amplitude ratio threshold of 0.75 as segregating thresholds. Area under the curve for receiver operating characteristic curves was 0.7 for each analysis, suggesting that the discriminating power was borderline. The performance characteristics were modest at best, likely reflecting the small sample size; positive predictive values were 0.42–0.44 and negative predictive values 0.83–0.87, suggesting that a normal threshold ratio could be more useful clinically than an abnormal value.
Figure 4.

Receiver operating characteristic (ROC) analysis determined thresholds for segregation of patients with late postoperative dysphagia from those without. Identified distal contractile integral (DCI), S2 peak amplitude, and S3 peak amplitude ratio thresholds (arrows) with corresponding performance characteristics are shown in each panel. Sens, sensitivity; Spec, specificity.
DISCUSSION
In this study, we report that although the MRS response is generally abnormal in GERD patients requiring antireflux surgery, lack of augmentation of smooth muscle contraction in the post-MRS sequence is significantly more prevalent in patients who develop late postoperative dysphagia. We utilized HRM software tools to first quantitate the MRS response in healthy controls, and then compared patient MRS responses with these normal values to determine proportions with abnormal responses. Our study is the first to suggest an outcome benefit from provocative maneuvers during esophageal manometry. These results could improve confidence in recommending a standard antireflux surgical procedure in patients who augment esophageal body contraction following MRS. Preoperative identification of patients at risk for late postoperative dysphagia could augment patient selection and help better counsel patients before antireflux surgery. Finally, our results suggest that a contraction response following MRS could be a better indicator of esophageal body peristaltic reserve than that seen after routine wet swallows during esophageal manometry.
As a provocative technique, MRS takes advantage of what is known about esophageal physiology to interrogate esophageal neural connections and muscle response (1). During a typical swallow, the wave of inhibition along the length of the esophagus (deglutitive inhibition) transitions into a contraction sequence, provided neural circuitry is intact, and the muscle is able to generate a contraction response (10). Normal responses to MRS, therefore, require intact neural pathways and an appropriate esophageal muscle response to stimulation. Central and peripheral mechanisms are responsible for the period of inhibition; central activation of vagal fibers leads to inhibition of the entire esophagus, whereas peripherally, myenteric inhibitory neurons release nitric oxide, inhibiting smooth muscle contraction (10). Following the wave of inhibition, cholinergically mediated deglutitive excitation results in contraction. During MRS, there is augmented inhibition of the esophageal body and LES during repetitive swallows, followed by robust esophageal body and LES contraction after the last swallow of the sequence (1,6). Our report characterizes MRS response using DCI that takes into account the duration, length, and amplitude of the contraction segments, and therefore accurately depicts vigor of contraction in the smooth muscle esophagus. Using these modern HRM software tools, MRS response was first characterized in a normal cohort of asymptomatic subjects, which serves to establish a relevant reference for future comparisons. Normal MRS responses have been previously reported using conventional line tracings, and our findings are similar to earlier studies (1). The additional information gleaned from the use of HRM are that peak contraction amplitudes in the two smooth muscle segments can be assessed separately, and that DCI provides a better overall picture than contraction amplitudes. We report that the DCI augments almost twofold in normal controls. There is a dichotomy in augmentation of the two smooth muscle contraction segments, with the nitric oxide-predominant S3 segment augmenting much more than the cholinergically driven S2. Although the exact physiology is not completely clear, this finding supports the current hypothesis of accumulation of nitric oxide and its derivatives during the period of inhibition during MRS, perhaps contributing to the augmented S3 and LES after contraction response (in addition to posthyperpolarization rebound cholinergic-mediated contraction) following MRS (6). We acknowledge the younger age of our controls, and it is unknown if the normal MRS response decays with age. We were unable to recruit normal controls on no medications, with no comorbidities and no symptoms in older age groups, which were our standards for the normal cohort. In other comparisons in the past, younger GERD patients had esophageal hypomotility patterns similar to older GERD patients, and both were significantly different from these normal controls (11). Hence, we believe our normal cohort is relevant for the current comparisons.
The most striking finding in our report is the very high association of a suboptimal DCI response with late postoperative dysphagia after antireflux surgery. Although patient factors could have confounded this finding, we took exceptional care to ascertain that the MRS portion of the study was not analyzed or reported as part of the clinical report so as not to influence surgical technique; furthermore, a single surgeon’s practice was interrogated to ensure uniform surgical technique. Patients with esophageal aperistalsis or extreme hypomotility (≥80% failure of peristalsis) were not included in order to avoid surgical bias toward a partial fundoplication; in fact, only 5% had > 50% failed sequences. In further analyzing our findings, inhibition during MRS remained intact in the esophageal body and LES in these patients with suboptimal DCI and late postoperative dysphagia, suggesting that the contractile defect is not within the inhibitory pathways. We speculate that inadequate neural excitatory input or an intrinsic muscular defect/inability of the muscle to generate an adequate muscle response is a potential mechanism. However, our study was not designed to determine whether the inadequate peristaltic reserve demonstrated in individuals with late postoperative dysphagia was a consequence of a neural or a muscular defect.
Other provocative maneuvers such as the use of more viscous material like apple sauce, solid bolus swallows, free water drinking, and test meals have been proposed as tools to uncover abnormalities of esophageal motor function (12,13). Although our study did not utilize these additional maneuvers, there will probably be additional information that can be obtained with judicious use of further provocative measures. The advantages of wet swallow MRS include ease of standardization of the procedure for the operator, performance within a relatively short period of time, patient tolerance, and easy interpretation. As antireflux surgery increases the LES pressure mechanically, MRS may be able to distinguish those patients who are able to augment esophageal smooth muscle contraction in response to a relative distal esophageal outflow obstruction from those who are not.
Our study has a few limitations. Although we identified 63 patients with preoperative HRM who had undergone symptom evaluation, the numbers of patients in each dysphagia group were small, thus limiting stratification of dysphagia severity and of MRS responses. The cohort was not consecutive, as not all patients completed HRM studies with adequate MRS sequences; patients were also required to have symptom details and follow-up for inclusion. Nevertheless, all patients operated by the same surgeon (L.M.B.) who completed all inclusion criteria over a 36-month period were included in this review. The mechanisms underlying preoperative dysphagia in 28 patients are likely multifactorial, and subtle structural lesions and ongoing reflux disease could have contributed to these symptoms in addition to motor abnormalities associated with reflux disease, as the dysphagia improved dramatically following antireflux surgery. We acknowledge that controlling for other factors determining postoperative dysphagia (wrap dysfunction, length of wrap, twisting and herniation of the wrap, surgeon experience, and variation in the length of follow-up) would have further enhanced our results, but these could not be evaluated in this retrospective report. The small number of patients in each of the dysphagia groups further limits conclusions that can be drawn about mechanisms underlying abnormal MRS responses. More importantly, many questions remain about the MRS technique and its analysis. For example, the reproducibility of MRS and the value of repeated MRS sequences remain unclear. Finally, patient factors and technical performance of MRS limit this maneuver, and not all patients can perform the MRS procedure adequately. For these reasons, at this stage it would be fair to say that further research is needed to augment and reproduce our results in a larger sample.
Despite these limitations, our study has several implications. Patients undergoing antireflux surgery often have a manometric study to exclude achalasia and its variants (2,14). This study lends additional support to the use of preoperative manometry for patients undergoing antireflux surgery (14). MRS used in conjunction with the standard 10 wet swallows may serve as a tool to uncover otherwise undetected abnormalities in esophageal motor function that may only emerge postoperatively. Future studies with larger numbers of patients will be necessary to fully interrogate the MRS response in patients with underlying motor abnormalities. In addition, our characterization of MRS response in healthy, asymptomatic individuals contributes to the limited knowledge of the definition of a normal MRS response (1) and serves as a platform for future evaluation of MRS response in HRM.
In conclusion, MRS as a provocative maneuver may assess esophageal peristaltic reserve in the esophageal body, and may have particular value in hypomotility states in the esophageal body. Information obtained from MRS during HRM can be used to counsel patients regarding expectations of postoperative transit symptoms after antireflux surgery. We anticipate this will have maximum value in those with borderline weak peristalsis on wet swallows and a robust MRS response, where confidence in full fundoplication could be enhanced. Further research is warranted to reproduce our results, and to determine if antireflux needs to be tailored to the MRS response.
Study Highlights.
WHAT IS CURRENT KNOWLEDGE
 Esophageal body and lower esophageal sphincter (LES) are inhibited during multiple rapid swallows (MRS), followed by augmented contraction.
Esophageal body and lower esophageal sphincter (LES) are inhibited during multiple rapid swallows (MRS), followed by augmented contraction. Some patients with weak wet swallow responses augment contraction following MRS.
Some patients with weak wet swallow responses augment contraction following MRS. There is no information about MRS responses in patients undergoing antireflux surgery.
There is no information about MRS responses in patients undergoing antireflux surgery.
WHAT IS NEW HERE
 Esophageal body contraction as measured by distal contractile integral (DCI) augments twofold with MRS.
Esophageal body contraction as measured by distal contractile integral (DCI) augments twofold with MRS. Gastroesophageal reflux disease (GERD) patients undergoing antireflux surgery have suboptimal MRS responses.
Gastroesophageal reflux disease (GERD) patients undergoing antireflux surgery have suboptimal MRS responses. Patients with late postoperative dysphagia following anti-reflux surgery are highly likely to have an abnormal MRS response.
Patients with late postoperative dysphagia following anti-reflux surgery are highly likely to have an abnormal MRS response.
Acknowledgments
Financial support: None.
Footnotes
CONFLICT OF INTEREST Guarantor of the article: C. Prakash Gyawali, MD, MRCP.
Specific author contributions: A.S.: study concept, data collection and analysis, manuscript preparation, and critical review; N.S.: study concept, data collection, and critical review of manuscript; J.D.: data collection and analysis, critical review of manuscript; V.K.: study concept, data analysis, and critical review of manuscript; L.M.B.: study concept, critical review of manuscript; C.P.G.: study concept, data analysis, manuscript preparation, and critical review.
Potential competing interests: None.
Presented in preliminary form at the annual meeting of the American Gastroenterological Association, San Diego, 2012.
REFERENCES
- 1.Fornari F, Bravi I, Penagini R, et al. Multiple rapid swallowing: a complementary test during standard oesophageal manometry. Neurogastroenterol Motil. 2009;21:718–e741. doi: 10.1111/j.1365-2982.2009.01273.x. [DOI] [PubMed] [Google Scholar]
- 2.Stoikes N, Drapekin J, Kushnir V, et al. The value of multiple rapid swallows during preoperative esophageal manometry before laparoscopic antireflux surgery. Surg Endosc. 2012;26:3401–7. doi: 10.1007/s00464-012-2350-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sifrim D, Jafari J. Deglutitive inhibition, latency between swallow and esophageal contractions and primary esophageal motor disorders. J Neurogastroenterol Motil. 2012;18:6–12. doi: 10.5056/jnm.2012.18.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roman S, Lin Z, Kwiatek MA, et al. Weak peristalsis in esophageal pressure topography: classification and association with dysphagia. Am J Gastroenterol. 2011;106:349–56. doi: 10.1038/ajg.2010.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xiao Y, Kahrilas PJ, Kwasny MJ, et al. High-resolution manometry correlates of ineffective esophageal motility. Am J Gastroenterol. 2012;107:1647–54. doi: 10.1038/ajg.2012.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reidel WL, Clouse RE. Variations in clinical presentation of patients with esophageal contraction abnormalities. Dig Dis Sci. 1985;30:1065–71. doi: 10.1007/BF01315604. [DOI] [PubMed] [Google Scholar]
- 7.Porter RF, Gyawali CP. Botulinum toxin injection in dysphagia syndromes with preserved esophageal peristalsis and incomplete lower esophageal sphincter relaxation. Neurogastroenterol Motil. 2011;23:139–44. e127–138. doi: 10.1111/j.1365-2982.2010.01604.x. [DOI] [PubMed] [Google Scholar]
- 8.Gyawali CP, Kushnir VM. High-resolution manometric characteristics help differentiate types of distal esophageal obstruction in patients with peristalsis. Neurogastroenterol Motil. 2011;23:502–e197. doi: 10.1111/j.1365-2982.2011.01672.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pandolfino JE, Ghosh SK, Rice J, et al. Classifying esophageal motility by pressure topography characteristics: a study of 400 patients and 75 controls. Am J Gastroenterol. 2008;103:27–37. doi: 10.1111/j.1572-0241.2007.01532.x. [DOI] [PubMed] [Google Scholar]
- 10.Sifrim D, Janssens J, Vantrappen G. A wave of inhibition precedes primary peristaltic contractions in the human esophagus. Gastroenterology. 1992;103:876–82. doi: 10.1016/0016-5085(92)90020-y. [DOI] [PubMed] [Google Scholar]
- 11.Porter RF, Kumar N, Drapekin JE, et al. Fragmented esophageal smooth muscle contraction segments on high resolution manometry: a marker of esophageal hypomotility. Neurogastroenterol Motil. 2012;24:763–8. e353. doi: 10.1111/j.1365-2982.2012.01930.x. [DOI] [PubMed] [Google Scholar]
- 12.Basseri B, Pimentel M, Shaye OA, et al. Apple sauce improves detection of esophageal motor dysfunction during high-resolution manometry evaluation of dysphagia. Dig Dis Sci. 2010;56:1723–8. doi: 10.1007/s10620-010-1513-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gyawali CP, Bredenoord AJ, Conklin JL, et al. Evaluation of esophageal motor function in clinical practice. Neurogastroenterol Motil. 2013;25:99–133. doi: 10.1111/nmo.12071. [DOI] [PubMed] [Google Scholar]
- 14.Chan WW, Haroian LR, Gyawali CP. Value of preoperative esophageal function studies before laparoscopic antireflux surgery. Surg Endosc. 2011;25:2943–9. doi: 10.1007/s00464-011-1646-9. [DOI] [PubMed] [Google Scholar]


