Abstract
BACKGROUND
Bystander cardiopulmonary resuscitation (CPR) is a crucial therapy for sudden cardiac arrest (SCA), yet rates of bystander CPR are low. This is especially the case for SCA occurring in the home setting, as family members of at-risk patients are often not CPR trained.
OBJECTIVE
To evaluate the feasibility of a novel hospital-based CPR education program targeted to family members of patients at increased risk for SCA.
DESIGN
Prospective, multicenter, cohort study.
SETTING
Inpatient wards at 3 hospitals.
SUBJECTS
Family members of inpatients admitted with cardiac-related diagnoses.
MEASUREMENTS AND RESULTS
Family members were offered CPR training via a proctored video-self instruction (VSI) program. After training, CPR skills and participant perspectives regarding their training experience were assessed. Surveys were conducted one month postdischarge to measure the rate of “secondary training” of other individuals by enrolled family members. At the 3 study sites, 756 subjects were offered CPR instruction; 280 agreed to training and 136 underwent instruction using the VSI program. Of these, 78 of 136 (57%) had no previous CPR training. After training, chest compression performance was generally adequate (mean compression rate 90 ± 26/minute, mean depth 37 ± 12 mm). At 1 month, 57 of 122 (47%) of subjects performed secondary training for friends or family members, with a calculated mean of 2.1 persons trained per kit distributed.
CONCLUSIONS
The hospital setting offers a unique “point of capture” to provide CPR instruction to an important, undertrained population in contact with at-risk individuals.
Patients discharged from the hospital with coronary disease complications experience an increased risk of sudden cardiac arrest (SCA), which afflicts over 200,000 people in the United States each year with an 80% to 90% mortality rate.1–7 Prompt delivery of cardiopulmonary resuscitation (CPR) can triple the probability of survival from SCA, yet less than 25% of SCA victims receive bystander CPR.8 Given that 80% of SCA events occur in the home environment, hospitalization could serve as an important “point of capture” for family instruction in CPR. Prior investigations have suggested conducting conventional CPR training courses before discharge for family members. However, significant barriers exist to this approach, including the requirement for a certified instructor and a large time commitment for standard training.9–12
To address these resource and time barriers, the American Heart Association recently established a video self-instruction (VSI) course in CPR, eliminating the need for an instructor and reducing the time requirement for training to 25 minutes. The course consists of a digital video disc (DVD) and low-cost inflatable mannequin in a self-contained kit.13 Several investigations have shown that CPR performance skills of students after VSI courses are similar to those of students after traditional CPR training programs.14–17 This VSI program presents the unique opportunity for “secondary training,” given that the DVD and mannequin may be shared by primary trainees with family members or friends. This VSI approach has not been evaluated in the hospital setting or with family members of patients at risk for SCA. We sought to test the feasibility of an in-hospital CPR training program using the VSI tool, with the hypothesis that VSI training would be well-accepted by family members of hospitalized patients with known or suspected coronary disease. We further hypothesized that subjects would be able to perform skills adequately and would be motivated to subsequently share the VSI course with others after their family member's hospital discharge.
METHODS
This prospective, multicenter investigation was approved by the University of Pennsylvania Institutional Review Board (IRB) and represents the initial component of an ongoing longitudinal study testing different methods of CPR education in the hospital setting. Enrollment was conducted at 3 hospitals: The Hospital of the University of Pennsylvania (a 700-bed tertiary-care academic medical center), Penn Presbyterian Medical Center (a 300-bed tertiary-care and community hospital) and Pennsylvania Hospital (a 400-bed community hospital).
Recruitment Strategy
Family members of hospitalized patients with known or suspected coronary disease were targeted in this investigation (eg, patients admitted with known myocardial infarction, or patients over 40 years old admitted with chest pain or shortness of breath who had a known history of coronary risk factors). Recruitment took place in the cardiology and telemetry wards of each hospital site by research assistants who were previously CPR trained, but not certified as CPR instructors. Subjects were considered eligible for participation if they were a family member of a current inpatient with known or suspected coronary disease and had not received CPR instruction within the past 2 years. Subjects were excluded if they were under age 18 years, felt unwell, or considered themselves physically unable to undergo CPR training. Eligible individuals were approached using an IRB-approved recruitment script. If the family member declined participation, the research assistant collected the individual's demographic information and reason for nonparticipation.
If the targeted individual expressed willingness to undergo CPR training, the research assistant administered a pretraining questionnaire to obtain demographic information and history of prior CPR instruction. Subjects then underwent the VSI training program in a family consultation room within the hospital unit, proctored by the research assistant. The VSI program contains an instructional DVD that teaches standard CPR (30 compressions: 2 breaths), as well as the importance of recognizing a nonresponsive patient and calling 9-1-1. The training process, including set-up, video review, and practice routinely took less than 45 minutes per subject. Upon completion of the VSI session, subjects were tested in their newly acquired CPR skills using a VSI or a standard CPR-recording mannequin, with CPR data analyzed via commercial software (Skill-Reporter ResuciAnne and Skill-Reporter software, Laerdal Medical Corporation, Wappinger Falls, NY). Compression rate was calculated as compressions per minute, omitting pauses, with video-recorded data abstracted and combined with objective CPR recordings. Subjects then completed a Likert scale semi-quantitative self-assessment to rate their perspectives on the CPR training experience. Subjects were not compensated financially, but were given the VSI kit to bring home with them at no cost, for the opportunity of performing secondary training.
Assessment of Secondary Training
In an effort to determine whether subjects shared the VSI kit with other family members, follow-up telephone contact was made with enrollees approximately 1 month after initial CPR training. Subjects were asked to complete a brief survey that included self-reporting of whether they shared the kit, and if so, how many individuals were trained by the subject (measurement of secondary training, defined as the mean number of people trained for each kit distributed).
Data Analysis and Statistical Calculations
All data, including compiled survey results and CPR quantitative data, were abstracted using a spreadsheet application (Excel, Microsoft Corporation, Redmond, WA). Descriptive statistics were used to compare demographics of enrolled vs. nonenrolled populations, using either student's t-tests for continuous variables or chi square tests for categorical data. Data are presented as mean ± standard deviation (SD), with significance set at an alpha = 0.05.
RESULTS
Subject Characteristics and Demographics
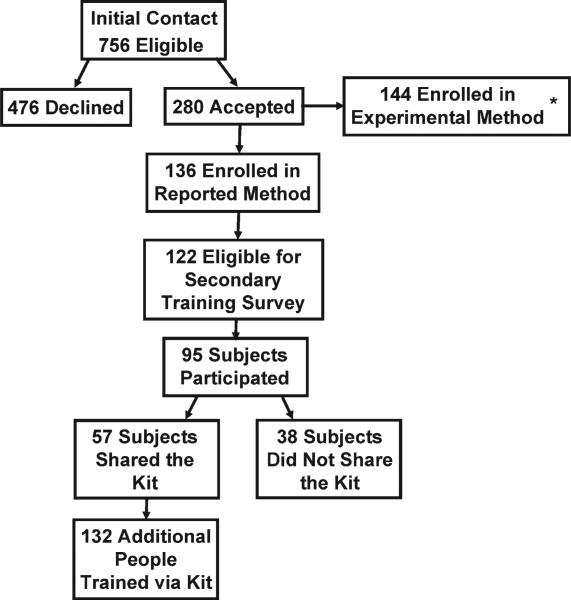
Subjects were recruited at the 3 hospital sites between May 2009 and January 2010. A total of 756 eligible individuals were approached, and 280 accepted enrollment for CPR training, representing a 37% enrollment rate (Figure 1). Of the 280 enrolled, 136 underwent instruction using the VSI training program as described, and 144 were enrolled using an experimental method of VSI training in CPR; this second cohort will be described elsewhere. When comparing the eligible individuals who declined enrollment versus those who accepted (Table 1), no significant differences were observed with regard to age, gender or race (P = NS for each). Common reasons cited for nonparticipation included “lack of interest” or “lack of time” (data not shown).
FIG. 1.
Schematic of experimental design and enrollment. *Denotes experimental CPR arm that will be reported elsewhere.
TABLE 1.
Subject Characteristics
| Enrolled (%) n = 136 | Screened/Not Enrolled (%) n = 476 | |
|---|---|---|
| Age, years | 52 ± 15 | 46 ± 26 |
| Female | 94(69) | 326 (68) |
| Race | ||
| White | 101 (74) | 316 (66) |
| Black | 30(22) | 90 (19) |
| Hispanic | 5(4) | 8(2) |
| Other/no response | 0(0) | 59 (13) |
| Relationship to patient | ||
| Spouse | 49 (36) | 171 (36) |
| Immediate family* | 58(43) | 168 (35) |
| Other | 28(21) | 76 (16) |
| No response | 1 (1) | 61 (13) |
| Highest Education | ||
| Elementary | 1 (1) | 1 (1) |
| Middle school | 1 (1) | 7(1) |
| High school | 46 (34) | 157 (33) |
| Some college/vocation | 36 (26) | 86 (18) |
| College | 30 (22) | 92 (19) |
| Graduate school | 22 (16) | 39 (8) |
| No response | 0(0) | 94(20) |
| Previous CPR training | ||
| No | 78 (57) | |
| Yes: within past 2 years | 0(0) | |
| Yes: within past 2–5 years | 13 (10) | |
| Yes: within past 5–10 years | 5(4) | |
| Yes: more than 10 years ago | 40 (29) |
NOTE: Percentages are rounded to the nearest integer. CPR training history was not assessed among subjects declining enrollment. Abbreviation: CPR, cardiopulmonary resuscitation.
Immediate family denotes sibling, parent or child of patient.
Demographics of the enrolled subject cohort are detailed in Table 1. The mean age of subjects was 52 ± 15, and 94 of 136 (69%) were female. Enrolled subjects represented spouses or immediate family members of the hospitalized patient in 107 of 136 (79%) of cases, and the vast majority, 118 of 136 (87%), had either never received CPR training or had received it over 10 years prior to current enrollment.
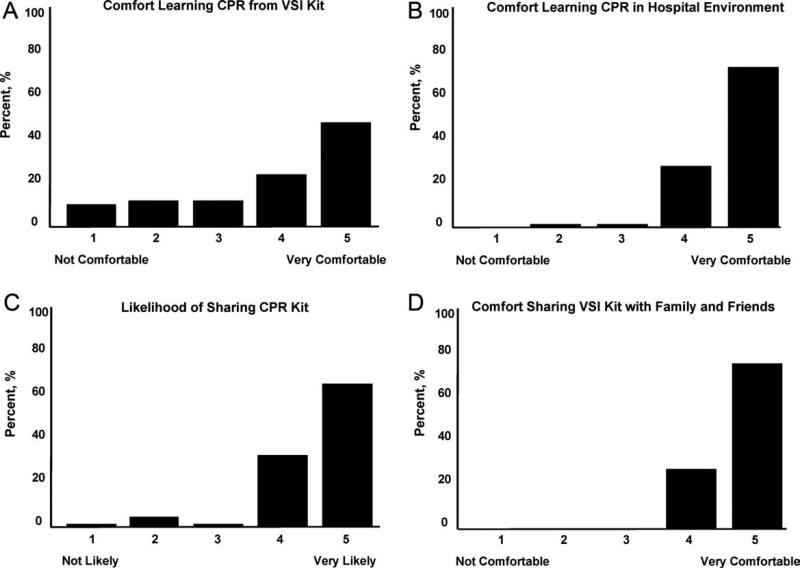
Subject Perspectives
A posttraining survey revealed that most respondents, 101 of 136 (74%) felt comfortable or very comfortable learning CPR from the VSI kit, and 127 of 136 (93%) felt likely or very likely to share the VSI kit (Figure 2).
FIG. 2.
Compiled survey responses from the enrolled subjects immediately after training. Data from 4 questions are shown, each with the Likert scale (1-5) responses as indicated.
Resuscitation Skills Testing
After CPR training, subjects were asked to perform initial resuscitation actions including 2 minutes of CPR on a mannequin (Table 2). A total of 127 subjects completed these trainings, with 25 completing testing using a VSI kit and 102 using a depth-recording mannequin; data from 9 subjects were excluded due to CPR recording technical problems. With regard to performance of initial resuscitation actions, 96 of 127 (76%) of subjects assessed responsiveness, 90 of 127 (71%) checked for breathing and 91 of 127 (72%) signaled the need to call for help. CPR was attempted by 127 of 127 (100%) subjects. The mean chest compression rate was 90 ± 26 per minutes, and mean compression depth was 37 ± 12 mm. The mean ventilation rate was 4 ± 3 per minutes.
TABLE 2.
CPR Skills Assessment After Training (n =127*)
| Resuscitation Basic Skills | Subjects (%) |
|---|---|
| Checked for responsiveness | 96(76) |
| Checked for breathing | 90(71) |
| Called for help | 91 (72) |
| Attempted CPR | 127(100) |
| CPR Characteristics | Mean (SD) |
| Compression rate (n/minute) | 90(26) |
| Compression depth (mm) | 37 (12)† |
| Ventilation rate (n/minute) | 4(3) |
Abbreviations: CPR, cardiopulmonary resuscitation, SD, standrad deviation.
Nine subjects were excluded from calculations due to CPR reporting technical problems.
Depth of compressions calculated from subset of trainees tested on CPR-recording mannequin (n = 102).
Secondary Training
Eligible subjects (n = 122) were surveyed via telephone 1 month after initial training, in which 95 individuals participated (78% response rate of those eligible for follow-up). VSI kits were shared by 57 subjects, with a total of 132 additional individuals receiving VSI-based CPR instruction. This represented a mean of 2.1 (median of 6) people trained per kit shared, with the actual number of people trained ranging from 1 to 15.
DISCUSSION
In the current work, we demonstrated the feasibility of using the hospital environment as a “point of capture” for training family members of at-risk patients in CPR skills. Given that most SCA events occur in the home setting, family member training may hold greater potential for CPR delivery during actual events than training a similar number of younger laypersons at large. Other investigators have identified the focused identification and CPR training of populations at risk of SCA as an important and potentially efficient step to improve survival.10,12,18,19 CPR education of family members before hospital discharge represents a logical extension of other cardiac risk factor-focused health care education and services before patients are discharged home, including delivery of dietary counseling, diabetic teaching, and education regarding cardiac symptoms. To our knowledge, our work represents the first hospital-based, adult, layperson, CPR training program using VSI as an instructional approach.
CPR training via a 25-minute VSI program has been shown to yield CPR performance quality in trainees that is similar to that generated from formal CPR classes that require 3 hours to 4 hours.14–16 While VSI training does not provide CPR certification, it is unlikely that the lack of testing and certification is a barrier to participation for the lay public. Indeed, the removal of the pressures of a formal class and testing may increase interest in CPR training through the VSI method.13,20,21
Several prior investigations have exploited VSI methodology as an outreach tool to teach CPR in various settings. A recent study in Norway used VSI CPR kits as refresher tools for hospital employees.22 Other work has focused on use of VSI implementation in schools.20,21,23 An example of this latter approach was a Danish initiative in which 35,000 VSI kits were distributed to seventh graders.20 Over 15,000 laypersons received “secondary training” at home by the initially trained students, highlighting a key advantage of the VSI kit approach. It has been argued that this secondary training phenomenon is among the reasons the VSI educational approach may offer a cost effective means for targeted family training.13,20,21
While participants in our program were able to adequately perform CPR skills and expressed self-reported motivation and empowerment, it must be acknowledged that many trained laypersons still do not act when confronted with an actual arrest event.8 In addition, CPR quality at the time of actual performance may be variable, attenuating the survival benefit.24–26 However, several population-based observational studies have supported the notion that training more laypersons in CPR translates into improved overall survival rates from cardiac arrest.25,27,28 Further work will be required to follow newly trained, at-risk family members over time to determine if SCA events occur, and if so, whether CPR was initiated.
Limitations
Willingness to undergo CPR training is likely to be confounded by cultural, regional, and educational factors. Therefore, the general applicability of this 3-hospital program to other practice environments remains an open question. In our program, the majority of screened family members still refused participation; however, we did not discern a simple relationship between willingness to participate and age, gender, or race. Furthermore, we utilized paid research assistants as subject recruiters and proctors to the VSI training; from a broader implementation perspective, it would be important to determine whether hospital volunteers or staff could perform the training. In addition, while a VSI training kit currently costs $35 and a conventional CPR course could cost from $150 to $300, a formal cost-effectiveness analysis of VSI training has yet to be performed. Another key limitation is that the secondary training effect was measured by participant self-report, which may be prone to recall bias; however, no specific incentives or penalties were used to encourage over-reporting of secondary training. Finally, in this short-term feasibility study, no direct patient outcomes nor instances of CPR performance were measured.
CONCLUSIONS
In this prospective study of hospital-based CPR training, we have shown that targeted training of families before hospital discharge is feasible, well received by trainees, and has the benefits of secondary training in the home environment, where most SCA events take place. This program could be easily implemented in other hospital or practice settings. Through targeted CPR training programs such as the one described in this investigation, at risk populations that are underre-presented in conventional CPR training classes can be equipped with important life-saving skills. Further work on a larger scale will be required to measure the impact of such programs on patient outcomes.
Acknowledgements
The authors wish to thank Lori Albright, Matthew Buchwald, Laura Ebbeling, Emily Esposito, Lori Ingleton, Kristy Walsh, Benjamin Weisenthal, Julie Xu and Mariana Gonzalez for subject recruitment and data collection assistance.
This work was supported by a Clinical Research Program grant from the American Heart Association. The funding organization had no role in data collection, analysis or drafting of this manuscript. Ms. Leary has received honoraria from Philips Healthcare, pertaining to professional rescuer CPR quality. Dr. Abella has received research funding and honoraria from Philips Healthcare, also pertaining to professional rescuer CPR quality, and in-kind research support from Laerdal Medical Corporation. Drs. Abella and Bobrow have received research funding from Medtronic Foundation, pertaining to improving statewide cardiac arrest monitoring and reporting, and both report being members of the American Heart Association Basic Life Support Subcommittee. Dr. Bobrow has also received funding from the American Heart Association to study ultra-brief CPR video training. Dr. Abella is additionally supported by a Career Development Award from the NIH (K23HL083082) and funding from the Doris Duke Foundation.
Footnotes
Additional Supporting Information may be found in the online version of this article.
References
- 1.Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics–2010 update: a report from the American Heart Association. Circulation. 2010;121(7):e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 2.Nichol G, Thomas E, Callaway CW, et al. Regional variation in outof-hospital cardiac arrest incidence and outcome. JAMA. 2008;300(12):1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huikuri HV, Tapanainen JM, Lindgren K, et al. Prediction of sudden cardiac death after myocardial infarction in the beta-blocking era. J Am Coll Cardiol. 2003;42(4):652–658. doi: 10.1016/s0735-1097(03)00783-6. [DOI] [PubMed] [Google Scholar]
- 4.Solomon SD, Zelenkofske S, McMurray JJ, et al. Sudden death in patients with myocardial infarction and left ventricular dysfunction, heart failure, or both. N Engl J Med. 2005;352(25):2581–2588. doi: 10.1056/NEJMoa043938. [DOI] [PubMed] [Google Scholar]
- 5.Maddox TM, Reid KJ, Rumsfeld JS, Spertus JA. One-year health status outcomes of unstable angina versus myocardial infarction: a prospective, observational cohort study of ACS survivors. BMC Cardiovasc Disord. 2007;7:28. doi: 10.1186/1471-2261-7-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adabag AS, Therneau TM, Gersh BJ, Weston SA, Roger VL. Sudden death after myocardial infarction. JAMA. 2008;300(17):2022–2029. doi: 10.1001/jama.2008.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao L, Wang L, Zhang Y. Elevated admission serum creatinine predicts poor myocardial blood flow and one-year mortality in ST-segment elevation myocardial infarction patients undergoing primary percutaneous coronary intervention. J Invasive Cardiol. 2009;21(10):493–498. [PubMed] [Google Scholar]
- 8.Swor R, Khan I, Domeier R, Honeycutt L, Chu K, Compton S. CPR training and CPR performance: do CPR-trained bystanders perform CPR? Acad Emerg Med. 2006;13(6):596–601. doi: 10.1197/j.aem.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 9.Abella BS, Aufderheide TP, Eigel B, et al. Reducing barriers for implementation of bystander-initiated cardiopulmonary resuscitation: a scientific statement from the American Heart Association for health-care providers, policymakers, and community leaders regarding the effectiveness of cardiopulmonary resuscitation. Circulation. 2008;117(5):704–709. doi: 10.1161/CIRCULATIONAHA.107.188486. [DOI] [PubMed] [Google Scholar]
- 10.Vaillancourt C, Stiell IG, Wells GA. Understanding and improving low bystander CPR rates: a systematic review of the literature. CJEM. 2008;10(1):51–65. doi: 10.1017/s1481803500010010. [DOI] [PubMed] [Google Scholar]
- 11.Brennan RT, Braslow A. Are we training the right people yet? A survey of participants in public cardiopulmonary resuscitation classes. Resuscitation. 1998;37(1):21–25. doi: 10.1016/s0300-9572(98)00026-4. [DOI] [PubMed] [Google Scholar]
- 12.Swor RA, Jackson RE, Compton S, et al. Cardiac arrest in private locations: different strategies are needed to improve outcome. Resuscitation. 2003;58(2):171–176. doi: 10.1016/s0300-9572(03)00118-7. [DOI] [PubMed] [Google Scholar]
- 13.Potts J, Lynch B. The American Heart Association CPR Anytime Program: the potential impact of highly accessible training in cardiopulmonary resuscitation. J Cardiopulm Rehabil. 2006;26(6):346–354. doi: 10.1097/00008483-200611000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Isbye DL, Rasmussen LS, Lippert FK, Rudolph SF, Ringsted CV. Lay-persons may learn basic life support in 24 min using a personal resuscitation manikin. Resuscitation. 2006;69(3):435–442. doi: 10.1016/j.resuscitation.2005.10.027. [DOI] [PubMed] [Google Scholar]
- 15.Roppolo LP, Pepe PE, Campbell L, et al. Prospective, randomized trial of the effectiveness and retention of 30-min layperson training for cardiopulmonary resuscitation and automated external defibrillators: The American Airlines Study. Resuscitation. 2007;74(2):276–285. doi: 10.1016/j.resuscitation.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 16.Lynch B, Einspruch EL, Nichol G, Becker LB, Aufderheide TP, Idris A. Effectiveness of a 30-min CPR self-instruction program for lay responders: a controlled randomized study. Resuscitation. 2005;67(1):31–43. doi: 10.1016/j.resuscitation.2005.04.017. [DOI] [PubMed] [Google Scholar]
- 17.Todd KH, Braslow A, Brennan RT, et al. Randomized, controlled trial of video self-instruction versus traditional CPR training. Ann Emerg Med. 1998;31(3):364–369. doi: 10.1016/s0196-0644(98)70348-8. [DOI] [PubMed] [Google Scholar]
- 18.Swor R, Compton S, Vining F, et al. A randomized controlled trial of chest compression only CPR for older adults-a pilot study. Resuscitation. 2003;58(2):177–185. doi: 10.1016/s0300-9572(03)00123-0. [DOI] [PubMed] [Google Scholar]
- 19.Swor R, Compton S. Estimating cost-effectiveness of mass cardiopulmonary resuscitation training strategies to improve survival from cardiac arrest in private locations. Prehosp Emerg Care. 2004;8(4):420–423. doi: 10.1016/j.prehos.2004.06.012. [DOI] [PubMed] [Google Scholar]
- 20.Isbye DL, Rasmussen LS, Ringsted C, Lippert FK. Disseminating cardiopulmonary resuscitation training by distributing 35,000 personal manikins among school children. Circulation. 2007;116(12):1380–1385. doi: 10.1161/CIRCULATIONAHA.107.710616. [DOI] [PubMed] [Google Scholar]
- 21.Lorem T, Palm A, Wik L. Impact of a self-instruction CPR kit on 7th graders’ and adults’ skills and CPR performance. Resuscitation. 2008;79(1):103–108. doi: 10.1016/j.resuscitation.2008.04.030. [DOI] [PubMed] [Google Scholar]
- 22.Bjørshol CA, Lindner TW, Soreide E, Moen L, Sunde K. Hospital employees improve basic life support skills and confidence with a personal resuscitation manikin and a 24-min video instruction. Resuscitation. 2009;80(8):898–902. doi: 10.1016/j.resuscitation.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 23.Lorem T, Steen PA, Wik L. High school students as ambassadors of CPR--a model for reaching the most appropriate target population? Resuscitation. 2010;81(1):78–81. doi: 10.1016/j.resuscitation.2009.09.030. [DOI] [PubMed] [Google Scholar]
- 24.Gilmore CM, Rea TD, Becker LJ, Eisenberg MS. Three-phase model of cardiac arrest: time-dependent benefit of bystander cardiopulmo-nary resuscitation. Am J Cardiol. 2006;98(4):497–499. doi: 10.1016/j.amjcard.2006.02.055. [DOI] [PubMed] [Google Scholar]
- 25.Rea TD, Stickney RE, Doherty A, Lank P. Performance of chest compressions by laypersons during the Public Access Defibrillation Trial. Resuscitation. 2010;81(3):293–296. doi: 10.1016/j.resuscitation.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 26.Abella BS, Sandbo N, Vassilatos P, et al. Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during in-hospital cardiac arrest. Circulation. 2005;111(4):428–434. doi: 10.1161/01.CIR.0000153811.84257.59. [DOI] [PubMed] [Google Scholar]
- 27.Vadeboncoeur T, Bobrow BJ, Clark L, et al. The Save Hearts in Arizona Registry and Education (SHARE) program: who is performing CPR and where are they doing it? Resuscitation. 2007;75(1):68–75. doi: 10.1016/j.resuscitation.2007.02.015. [DOI] [PubMed] [Google Scholar]
- 28.Herlitz J, Svensson L, Holmberg S, Angquist KA, Young M. Efficacy of bystander CPR: intervention by lay people and by health care professionals. Resuscitation. 2005;66(3):291–295. doi: 10.1016/j.resuscitation.2005.04.003. [DOI] [PubMed] [Google Scholar]