Abstract
Objective To use the rs1229984 variant in the alcohol dehydrogenase 1B gene (ADH1B) as an instrument to investigate the causal role of alcohol in cardiovascular disease.
Design Mendelian randomisation meta-analysis of 56 epidemiological studies.
Participants 261 991 individuals of European descent, including 20 259 coronary heart disease cases and 10 164 stroke events. Data were available on ADH1B rs1229984 variant, alcohol phenotypes, and cardiovascular biomarkers.
Main outcome measures Odds ratio for coronary heart disease and stroke associated with the ADH1B variant in all individuals and by categories of alcohol consumption.
Results Carriers of the A-allele of ADH1B rs1229984 consumed 17.2% fewer units of alcohol per week (95% confidence interval 15.6% to 18.9%), had a lower prevalence of binge drinking (odds ratio 0.78 (95% CI 0.73 to 0.84)), and had higher abstention (odds ratio 1.27 (1.21 to 1.34)) than non-carriers. Rs1229984 A-allele carriers had lower systolic blood pressure (−0.88 (−1.19 to −0.56) mm Hg), interleukin-6 levels (−5.2% (−7.8 to −2.4%)), waist circumference (−0.3 (−0.6 to −0.1) cm), and body mass index (−0.17 (−0.24 to −0.10) kg/m2). Rs1229984 A-allele carriers had lower odds of coronary heart disease (odds ratio 0.90 (0.84 to 0.96)). The protective association of the ADH1B rs1229984 A-allele variant remained the same across all categories of alcohol consumption (P=0.83 for heterogeneity). Although no association of rs1229984 was identified with the combined subtypes of stroke, carriers of the A-allele had lower odds of ischaemic stroke (odds ratio 0.83 (0.72 to 0.95)).
Conclusions Individuals with a genetic variant associated with non-drinking and lower alcohol consumption had a more favourable cardiovascular profile and a reduced risk of coronary heart disease than those without the genetic variant. This suggests that reduction of alcohol consumption, even for light to moderate drinkers, is beneficial for cardiovascular health.
Introduction
Alcohol is the fifth leading risk factor for death and disability accounting for 4% of life years lost due to disease.1 While the harmful effects of alcohol on conditions such as liver cirrhosis, injuries, and cancers of the liver, colorectum, breast, and upper aerodigestive tract have been firmly established,2 uncertainty remains concerning the potential protective effects of light to moderate alcohol consumption on risk of coronary heart disease and stroke.3 4 5 Observational studies have consistently reported that compared with non-drinkers, light to moderate drinking exhibits a reduced cardiovascular risk,6 7 with the lowest risk found at approximately 12-25 British units per week, while heavier and more hazardous drinking is associated with an increased risk, resulting in the well established U shaped association.2 8 However, the apparent cardioprotective effect associated with light to moderate drinking could be explained by an elevated cardiovascular risk from underlying poor health in non-drinkers,9 or confounding by lifestyle or social factors associated with light to moderate drinking.10
The most widely proposed mechanism for this purported cardioprotective effect of alcohol is an increase in high density lipoprotein (HDL) cholesterol.11 However, the causal nature of the association of HDL cholesterol with cardiovascular events is unclear.12 13 Although an HDL cholesterol raising effect of alcohol has been reported in experimental studies,11 the small sample size and short follow-up means existing studies may be prone to bias, undermining their validity.
In the absence of a viable randomised trial to confirm or refute the cardioprotective effect of light to moderate alcohol consumption, an alternative approach is to use a genetic variant that serves as a proxy for alcohol consumption. This approach, known as Mendelian randomisation, avoids some of the key limitations of observational studies, since allocation of genetic variants is random with regard to potential confounders, and genotype is not modified by disease (abolishing reverse causality).14 15 A non-synonymous single nucleotide polymorphism (rs1229984) in the alcohol dehydrogenase 1B gene (ADH1B), which encodes the ADH1B enzyme, which provides the primary pathway of alcohol metabolism,16 has been associated with a flush response to alcohol consumption, lower levels of usual alcohol consumption and blood ethanol levels,17 as well as a lower risk of alcohol dependence among adult drinkers18 19 and adolescents,19 which led to the selection of this single nucleotide polymorphism as a genetic instrument in previous Mendelian randomisation studies that investigated the role of alcohol in high blood pressure and various cancers.20 21 22 23 We present results from an international collaboration that used the ADH1B rs1229984 variant as an instrument to investigate the association of alcohol with cardiovascular biomarkers and events in more than 260 000 individuals.
Methods
Formation of the consortium
Given that the rs1229984 genetic variant is not represented in widely available genotyping platforms such as Illumina-metabochip, Illumina-immunochip, or genome-wide association platforms (with the exception of recent platforms), we initially focused on studies genotyped with the IBC Cardiochip array, which contains this single nucleotide polymorphism (SNP). Through contact with the designer of the Institute for Translational Medicine and Therapeutics (ITMAT) Broad Institute CARe consortium (IBC) CardioChip array (B J Keating,24 coauthor), we contacted all population based studies genotyped on this array. Subsequently, we established contact with a series of genetic study groups with whom we have collaborated in the past and sent them a brief proposal describing the general aims of the study, including de novo genotyping in their studies. A minor subset of studies in European descent population that used this variant in previous publications was also identified and included in the consortium (details available in table S1 in the appendix on bmj.com). In addition, we checked publicly available consortia such as CARDIoGRAMplusC4D (www.cardiogramplusc4d.org) and found the SNP was not included in these consortia.
We incorporated individual participant data from 261 991 participants of European ancestry from 56 studies (see appendix). All participants provided written, informed consent, and ethical approval was granted by local ethics committees for participating studies. Ethical approval for secondary data analysis was granted by the London School of Hygiene & Tropical Medicine ethics committee (application No 5905).
Alcohol traits
The principal alcohol trait was weekly volume of alcohol in British units (1 British unit is equivalent to 0.57 US units or 10 ml (7.9 g) ethanol), which we derived using questionnaire data from each study (table S2 in the appendix). We additionally assessed the overall drinking status (drinkers v non-drinker) of study subjects, the study specific top tertile of alcohol consumption (separately for men and women), and history of binge drinking (for details see supplementary methods 2.1). γ-glutamyltransferase was used as a marker of heavy alcohol consumption.
Clinical outcomes
The primary clinical event was incident and prevalent (including fatal and non-fatal) coronary heart disease. Secondary clinical outcomes were stroke and type 2 diabetes. Stroke included all subtypes and consisted of incident and prevalent (including fatal and non-fatal) cases. In a subsample, information on ischaemic stroke was also available. For type 2 diabetes, we restricted the analysis to prevalent cases with the exception of one nested case-cohort that included incident cases.25 Precise definitions of outcomes for each study are reported in table S3 of the appendix.
Genotype properties
Genotyping platforms, genotype frequencies, Hardy Weinberg equilibrium P values, and call rates (median of 98.8%) for ADH1B rs1229984 (directly genotyped in all studies) are listed in table S1 and figure S1 of the appendix.
Statistical analysis
A standard analysis protocol was applied to each study to produce a consistent dataset. Analyses were conducted using individual participant data in each study and then pooled across studies using meta-analysis. Because of differences in variables collected by each study, not all studies were included in all analyses (fig S2 of appendix). We restricted analyses to individuals of European descent with data for ADH1B rs1229984 genotype, age, sex, and any one of the outcomes of interest. All non-normally distributed continuous variables, including units/week of alcohol, were natural log transformed. For these traits, the mean difference on the logarithmic scale was exponentiated to generate the relative difference and then converted to a percentage difference.
We investigated the shape of the association between alcohol consumption (log units/week) and cardiovascular biomarkers and potential confounders in observational analysis among 131 490 individuals from 28 studies. Statistical details are given in supplementary methods 2.2 of the appendix.
For all genetic analyses, we used a dominant model due to the low prevalence of the rs1229984 A-allele (average carriage of rs1229984 A-alleles: 7%): data from carriers of either one or two rare A-alleles were pooled and compared with individuals homozygous for the G-allele (the reference group). We first quantified the effects of rs1229984 A-allele on alcohol traits as well as on lifestyle and social factors to validate our instrument for alcohol consumption. Then, we studied the associations of the rs1229984 A-allele with cardiovascular biomarkers from several pathways that may mediate the effects of alcohol on cardiovascular events. Finally, we evaluated the effects of the rs1229984 A-allele on coronary heart disease, combined subtypes of stroke (as well as ischaemic stroke separately) and type 2 diabetes.
For continuous traits, means and standard deviations were derived for rs1229984 A-allele carriers and non-carriers. For binary traits, log odds ratios and standard errors were estimated for rs1229984 A-allele carriers versus non-carriers. All effect estimates were calculated within each study and then pooled using fixed (default) and random effects meta-analysis. Between study heterogeneity was quantified using I2.26
If the U shaped association between alcohol consumption and cardiovascular events is real, a comparison of event rates in rs1229984 A-allele carriers (associated with a reduction in alcohol consumption from published studies20) versus non-carriers will vary across broad categories of alcohol consumption. In light to moderate drinkers (>0 to <21 units/week), ADH1B rs1229984 A-allele carriers will be expected to have a higher coronary heart disease event risk, whereas, for heavy drinkers (≥21 units/week) they will be expected to have a lower event risk. Likewise, this stratification by alcohol consumption will also serve to validate the ADH1B rs1229984 A-allele variant as a specific instrument for alcohol consumption, as it is expected that in non-drinkers carriage of the rs1229984 A-allele variant will have no effect on cardiovascular traits or events, or a substantially attenuated effect given the known difficulty in correctly classifying long term non-drinkers from self reported questionnaires.27 Therefore, we repeated the genetic analysis in strata of alcohol intake (none (0 units/week), light to moderate (>0 to <21 units/week), and heavy (≥21 units/week); the strata were selected to represent the U shaped association of alcohol and cardiovascular events from observational studies) and investigated if there was a trend between alcohol categories and the effect of rs1229984 A-allele using meta-regression (see supplementary methods 2.3 of appendix for further details). The same stratified analysis was conducted for potential confounders, to investigate if confounding was reintroduced by stratifying by alcohol.28 For units/week of alcohol consumption (our main alcohol phenotype), we also performed a subgroup analysis according to the type of alcohol questionnaire (according to whether consumption questions asked separately for beverage type (such as beer, wine, spirits) v all beverages combined). Exploratory subgroup analyses were undertaken to assess the impact of study characteristics included sex, mean age, geographical region, Hardy Weinberg equilibrium, genotype platform, year of DNA extraction, and, whether the study contributed to observational analysis.
In order to investigate potential residual confounding by population stratification, we adjusted for principal components derived from IBC CardioChip array24 in studies with available data (see supplementary methods 2.4 for further details). To evaluate confounding by linkage disequilibrium between rs1229984 with single nucleotide polymorphisms associated with cardiovascular risk factors in genome-wide association studies29 that could distort associations of rs1229984, we used the Whitehall-II cohort30 (including both IBC CardioChip24 and MetaboChip31 platforms).
In the current manuscript, we did not conduct an instrumental variable analysis to estimate causal effects since the available methods assume a linear association between the exposure and the outcome, which may not hold for alcohol and cardiovascular disease.
Analyses were conducted in Stata v13.0 (StataCorp, Texas, USA). All P values reported are two sided.
Results
We approached 59 studies, of which 56 were included in this collaboration. Of the three excluded studies, two (INTERHEART and INTERSTROKE) declined to participate because of overlap with existing projects, and a third (CoLaus) was excluded as the rs1229984 genetic variant was not directly genotyped.
Of the 261 991 participants in our analysis, 48% were women, and the mean age per study was 58 years (range 26-75 years) (table S4 of appendix). The median number of alcohol units consumed in each study is shown in table S4. There were 20 259 coronary heart disease events, 10 164 stroke cases (4339 ischaemic strokes) and 14 549 type 2 diabetes cases (table S5). Means and distributions for continuous traits in all studies are presented in tables S6-S8. The observational analysis between alcohol and cardiovascular risk factors is reported in the supplementary results section and figures S2 and S3 of the appendix.
Genetic association analysis
ADH1B and alcohol consumption
Carriers of the rs1229984 A-allele consumed fewer units of alcohol per week (−17.2% units/week (95% confidence interval −18.9% to −15.6%)) and had lower odds of being in the top third of drinking volume (odds ratio 0.70 (0.68 to 0.73)) compared with non-carriers. Rs1229984 A-allele carriers also had lower odds of binge drinking (odds ratio 0.78 (0.73 to 0.84)), increased odds of being self reported abstainers (odds ratio 1.27 (1.21 to 1.34)) and lower levels of γ-glutamyltransferase (−1.8% (−3.4% to −0.3%)) (table 1).
Table 1.
Pooled estimates of association between genetic variant ADH1B rs1229984 (A-allele carriers v non-carriers) and measures of alcohol consumption. (Summary effect estimates are derived from fixed effects meta-analysis)
| Alcohol consumption measure | No of studies, cases/individuals | Effect estimate (95% CI) | P value | I2 value (%) |
|---|---|---|---|---|
| Log transformed data* | % difference | |||
| Intake volume (units/week†) | 46, NA/218 969 | −17.22 (−18.86 to −15.55) | 5.5×10−76 | 64 |
| γ-glutamyltransferase level (U/L) | 15, NA/97 755 | −1.84 (−3.40 to −0.26) | 0.028 | 36 |
| Categorical data | Odds ratio | |||
| Top tertile of alcohol intake | 45, 69 229/222 332 | 0.70 (0.68 to 0.73) | 9.8×10−67 | 60 |
| Binge drinker‡ | 21, 22 198/131 290 | 0.78 (0.73 to 0.84) | 1.4×10−12 | 47 |
| Alcohol abstainer‡ | 32, 24 482/189 854 | 1.27 (1.21 to 1.34) | 2.6×10−19 | 73 |
NA = not applicable.
*Non-normally distributed variables were natural log transformed and mean differences on the log scale were converted to percentage differences.
†Alcohol units in British units; 1 UK unit = 0.57 US units or 10 mL (7.9 g) ethanol.
‡For definitions of binge drinker and alcohol abstainer, see table S2 in appendix.
The association of the rs1229984 A-allele with alcohol volume remained unaltered when stratified by age, gender, geographical region, Hardy Weinberg Equilibrium P value, and whether the alcohol questionnaire used was beverage specific (fig S4 of appendix), or after exclusion of samples with a proportion of A-allele carriers >10% (approximately >5% minor allele frequency; data available on request). A meta-regression analysis of the mean alcohol volume (on the log scale) in rs1229984 A-allele carriers compared with non-carriers that takes into account the uncertainty around the mean suggested a constant proportional effect of the of ADH1B rs1229984 variant on alcohol volume (fig S5). This was also supported by the finding that in our samples the standard deviations for carriers and non-carriers were very similar (fig S6).
ADH1B and cardiovascular biomarkers
Carriers of the rs1229984 A-allele had lower systolic blood pressure (−0.88 (−1.19 to −0.56) mm Hg) compared with non-carriers. Concordant with this, rs1229984 A-allele carriers also had lower odds of hypertension (104 570 cases; odds ratio 0.94 (0.91 to 0.98)). Rs1229984 A-allele carriers had lower levels of interleukin-6 (−5.2% (−7.8% to −2.4%)), C reactive protein (−3.4% (−5.7% to −1.1%)), body mass index (−0.17 (−0.24 to −0.10) kg/m2), and waist circumference (−0.34 (−0.58 to −0.10) cm). Rs1229984 A-allele carriers also had lower non-HDL cholesterol concentrations (−0.03 (−0.05 to −0.01) mmol/L) (table 2).
Table 2.
Pooled estimates of association between genetic variant ADH1B rs1229984 (A-allele carriers v non-carriers) and cardiovascular biomarkers in all participants. (Summary effect estimates are derived from fixed effects meta-analysis and are reported as mean differences unless stated otherwise)
| Biomarker | No of studies, individuals | Effect estimate (95% CI) | P value | I2 value (%) |
|---|---|---|---|---|
| Systolic blood pressure (mm Hg) | 48, 227 559 | −0.88 (−1.19 to −0.56) | 4.1×10−8 | 26 |
| Anthropometric measures: | ||||
| Body mass index (weight (kg)/(height (m)2)) | 51, 232 570 | −0.17 (−0.24 to −0.10) | 3.4×10−6 | 52 |
| Waist circumference (cm) | 42, 140 923 | −0.34 (−0.58 to −0.10) | 6.2×10−3 | 41 |
| Inflammation: | ||||
| Log transformed interleukin 6 (% difference)* | 17, 30 950 | −5.15 (−7.82 to −2.40) | 2.90×10−4 | 33 |
| Log transformed C reactive protein (% difference)* | 42, 124 498 | −3.40 (−5.68 to −1.05) | 4.60×10−3 | 1 |
| Lipids: | ||||
| Non-HDL cholesterol (mmol/L) | 46, 202 794 | −0.03 (−0.05 to −0.01) | 5.10×10−3 | 25 |
| Log transformed triglycerides (% difference)* | 46, 205 824 | 1.61 (0.66 to 2.57) | 8.90×10−4 | 36 |
| HDL cholesterol (mmol/L) | 46, 203 440 | −0.004 (−0.012 to 0.003) | 0.259 | 54 |
*Non-normally distributed variables were natural log transformed and mean differences on the log scale were converted to percentage differences.
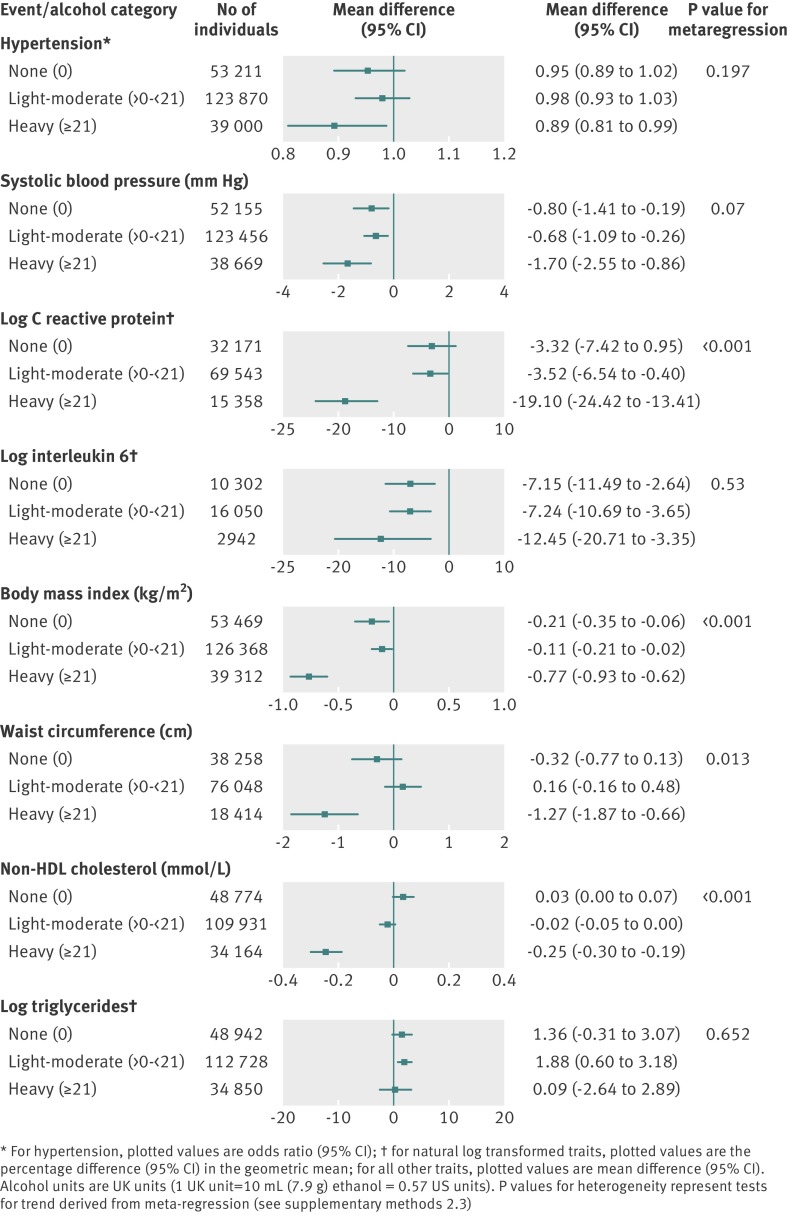
When the effect of the ADH1B rs1229984 A-allele on these cardiovascular traits was stratified by alcohol consumption, a differential effect was observed. Among heavy drinkers (≥21 units/week), carriers of the rs1229984 A-allele, who on average consume 17.2% less alcohol than non-carriers, showed a more pronounced reduction in these cardiovascular traits than that observed in light to moderate drinkers and non-drinkers (fig 1 ). In contrast, the effect of rs1229984 on these cardiovascular traits did not differ systematically according to exploratory subgroup analyses by laboratory procedures or study characteristics (P>0.05 for 52 of 58 comparisons; fig S7 of appendix).
Fig 1 Meta-analysis pooled estimates of the association between ADH1B rs1229984 (A-allele carriers v non-carriers) and cardiovascular disease biomarkers showing association on crude analysis, stratified by alcohol intake
Although we observed that rs1229984 A-allele carriers had higher triglyceride levels (1.6% (0.7% to 2.6%)), this effect was not modified by alcohol categories (fig 1 ).
There was no overall difference between rs1229984 A-allele carriers and non-carriers in HDL cholesterol concentration (−0.004 (−0.012 to 0.003) mmol/L). However, an association between rs1229984 A-allele carriage with HDL cholesterol was observed in the highest category of alcohol consumption, but in the opposite direction to that expected from observational findings (0.04 (0.02 to 0.06) mmol/L; fig S8 of appendix). (That is, the log-linear association of HDL cholesterol with alcohol consumption from observational studies (fig S3) would suggest that a reduction in alcohol consumption, as observed for carriers of the rs1229984 A-allele, should associate with a reduction in HDL cholesterol levels.) In subgroup analysis by laboratory procedures and major study characteristics, we observed that rs1229984 A-allele carriers from northern Europe had lower levels of HDL cholesterol (−0.04 (−0.05 to −0.02) mmol/L). Since this geographical specificity could reflect residual population stratification in samples outside northern Europe, we adjusted for principal components in a subset of individuals not from northern Europe. The unadjusted model for the association between rs1229984 A-allele and HDL cholesterol (0.02 difference in standard deviation (95% confidence interval −0.02 to 0.06)) did not differ from the model adjusted for population structure (0.01 difference in standard deviation (−0.03 to 0.05)) (fig S8). Similar null results were observed for apolipoprotein A1 (table S9 of appendix).
Rs1229984 A-allele carriage was not associated with carotid intima medial thickness, electrocardiographic measures of left ventricular hypertrophy, fibrinogen, von Willebrand factor, factor VII, fasting blood glucose, N-terminal of the prohormone brain natriuretic peptide, or lipoprotein(a) overall (table S9 of appendix). For these traits, similar null results were observed when stratified for alcohol consumption or by other exploratory subgroups (P>0.05 for 47 of 48 comparisons, data available on request), with the exception of fasting glucose and lipoprotein(a), where the strength of association was more pronounced in heavy drinkers compared with other alcohol categories (P values for heterogeneity 0.05 and 0.01, respectively) (fig S9).
ADH1B and lifestyle factors
Carriage of the rs1229984 A-allele was not associated with physical activity, but showed higher odds of ever smoking (odds ratio 1.06 (95% confidence interval 1.02 to 1.09)). However, the association with ever smoking was in the opposite direction to that seen in observational analysis, and no association was observed for other quantitative measures of tobacco exposure such as cigarettes per day, pack years, or cotinine levels. Rs1229984 A-allele carriers showed higher total years in education (0.04 difference in standard deviation (95% confidence interval 0.01 to 0.08)). No differential effect of ADH1B on any of the lifestyle factors was identified on stratifying by alcohol intake (making it unlikely that stratifying by alcohol introduced bias) or by other exploratory subgroups (P>0.05 for all comparisons) (figs S10 and S11 of appendix).
ADH1B and cardiovascular events
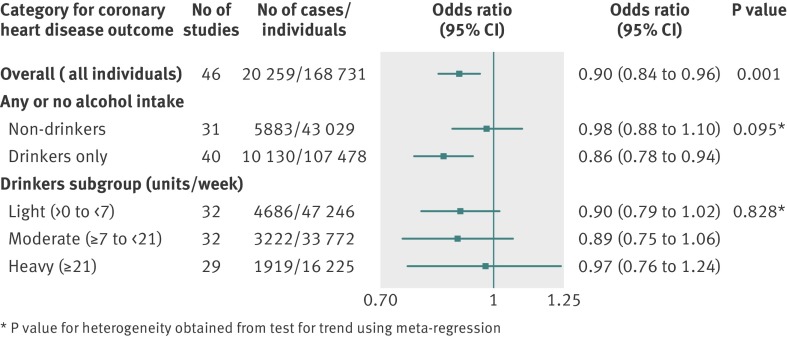
Rs1229984 A-allele carriage showed reduced odds of coronary heart disease (odds ratio 0.90 (95% confidence interval 0.84 to 0.96, I2=17%)) (fig 2 and fig S12 of appendix). In studies with ≥1000 coronary heart disease events (four studies with 8374 coronary heart disease events), the odds ratio for coronary heart disease was 0.81 (0.72 to 0.91, I2=0%) (table S10). When analysis was restricted to non-drinkers the association was null (odds ratio 0.98 (0.88 to 1.10)), while among drinkers (>0 units/week alcohol), carriers of the rs1229984 A-allele had reduced odds of coronary heart disease (odds ratio 0.86 (0.78 to 0.94)). This is consistent with the assumption that the associations ascribed to the ADH1B variant are mainly due to alcohol consumption. Further subdivision of the drinkers category into light (>0 to <7 units/week), moderate (≥7 to <21 units/week), and heavy (≥21 units/week) showed the same protective effect of the variant across all alcohol categories (P value for heterogeneity=0.83; fig 2 ), suggesting that there was no difference between rs1229984 A-allele carriers and non-carriers in coronary heart disease risk across alcohol consumption levels among individuals who drank.
Fig 2 Meta-analysis pooled estimates of the association between ADH1B rs1229984 (A-allele carriers v non-carriers) and coronary heart disease overall, and stratified by alcohol intake
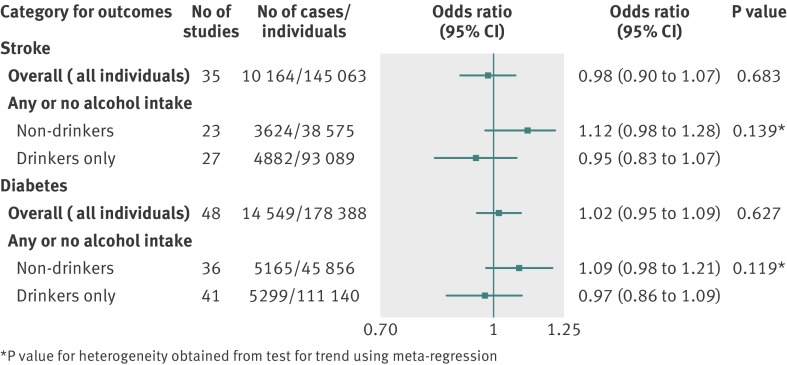
Although there was no association of the rs1229984 A-allele with the combined stroke subtypes (odds ratio 0.98 (0.90 to 1.07)) (fig 3 ), when the analysis was limited to ischaemic stroke subtype, rs1229984 A-allele carriers had lower odds of ischaemic stroke (odds ratio 0.83 (0.72 to 0.95)) (fig S13 of appendix). No association between rs1229984 A-allele with type2 diabetes was observed (odds ratio 1.02 (0.95 to 1.09)) (fig 3 ).
Fig 3 Meta-analysis pooled estimates of the association between ADH1B rs1229984 (A-allele carriers v non-carriers) and stroke (combined subtypes) and type 2 diabetes overall, and stratified by alcohol intake
Random effect estimates for associations of ADH1B with all outcomes were similar to those from fixed effect models (figs S4-14 of appendix).
Adjustment for population structure did not alter the rs1229984 A-allele associations (figs S15-16). The gene variant was not in linkage disequilibrium with previously reported loci from genome-wide association studies for any cardiovascular trait (table S11).
Discussion
Principal findings of study
In this large scale Mendelian randomisation analysis, we showed that carriers of the rs1229984 A-allele had lower levels of alcohol consumption and exhibited lower levels of blood pressure, inflammatory biomarkers, adiposity measures, and non-HDL cholesterol, and reduced odds of developing coronary heart disease, compared with non-carriers of this allele. In contrast to previous observational and experimental studies, our study showed that individuals with a genetic predisposition to consume less alcohol had lower, not higher, odds of developing coronary heart disease regardless of whether they were light, moderate, or heavy drinkers. Moreover, ADH1B genotype was not associated with type 2 diabetes, HDL cholesterol level, or coagulation markers.
The rs1229984 A-allele showed very strong association with non-drinking and amount of alcohol consumed. The fact that our analyses suggested a constant proportional effect of the rs1229984 A-allele on alcohol volume across a wide range of alcohol volume from the included studies supports the notion that social pressure in heavier drinking cultures is unlikely to override the effect of the genetic variant on alcohol consumption.20 It is important to note that the rs1229984 A-allele was a proxy for all types of self reported drinking behaviour including volume, being in the top third of drinkers per study, binge drinking, and abstention, and it also showed association with levels of the liver enzyme γ-glutamyltransferase (an objective marker of heavy alcohol intake). This confirms that rs1229984 was suitable as a non-specific genetic proxy of alcohol consumption in the mendelian randomisation analysis. Our findings are therefore not specific to one particular type of alcohol behaviour, but reflect a combination of different patterns of alcohol exposures, which are nevertheless directionally concordant (that is, the A-allele resulted in lower alcohol consumption).
For the cardiovascular traits that showed association on overall with the rs1229984 A-allele, null or substantially reduced associations were observed in non-drinkers and more pronounced associations in heavy drinkers when compared with light to moderate drinkers. This is as expected under the assumption that the effect of this genetic variant is only explained by exposure to alcohol.
From the U shaped association seen in observational studies, we would expect that for drinkers below the nadir (12-25 units/week), a reduction of 17.2% in alcohol consumption (corresponding to rs1229984 A-allele carriage) would lead to a small increase in the risk of coronary heart disease, whereas for those with alcohol consumption above the nadir, a similar reduction in alcohol consumption would lead to a decrease in coronary heart disease risk. Contrary to these expectations, however, we found that individuals below the nadir with a genetic predisposition to consume less alcohol had lower odds of developing coronary heart disease at all categories of alcohol consumption (fig 2 ), bringing the hypothesised cardioprotective effect of alcohol into question.
Strengths and weaknesses of the study
Major strengths of this international collaboration are the large sample size, availability of detailed alcohol phenotypic data and a comprehensive repertoire of cardiovascular risk factors and major cardiovascular events. The process by which studies were recruited into the collaboration, including mainly unpublished data, means that findings are unlikely to suffer from publication bias. The use of a standardised analytical protocol further increases reliability of the findings.
The lack of association of the ADH1B rs1229984 A-allele with HDL cholesterol levels was unexpected. In principle, failure to detect an association with HDL cholesterol could have arisen from lack of power. However, this is unlikely as rs1229984 was associated with traits (such as C reactive protein or interleukin 6) for which alcohol consumption had a less powerful effect and where the sample size for genetic analysis was several times smaller than for HDL cholesterol (fig S2 of appendix). Our extensive subgroup and in silico analyses also suggested it was unlikely that laboratory technique, type of alcohol questionnaire used in the studies, or confounding by linkage disequilibrium could explain the overall null effect. We did find an association of rs1229984 A-allele carriage with HDL cholesterol in the subset of northern European studies. Although this suggests the lack of association in non-northern European studies may arise from population stratification, adjustment for population structure using principal components analysis did not reveal an association, making this an unlikely explanation.
We also did not identify associations of the rs1229984 A-allele with coagulation markers, type 2 diabetes, and the combined subtypes of stroke. With regard to coagulation markers, these results seem more robust for fibrinogen, as confirmed by subgroup analysis. For factor VII and von Willebrand factor, reduced sample size limited our ability to exclude a small effect.
Although we observed an overall null association of the rs1229984 A-allele with type 2 diabetes and blood glucose concentration, a stratified analysis by alcohol consumption showed that, among heavy drinkers, carriers of the rs1229984 A-allele had lower levels of glucose and a directionally consistent relationship with type 2 diabetes. It is interesting that we did not observe a stronger protective association of coronary heart disease in heavy drinkers for carriers of the ADH1B variant, as we observed for cardiovascular risk factors. This is likely to reflect reduced power due to the low number of coronary heart disease events in the heavy drinking stratum. The relatively small number of stroke events is an important limitation, as well as the use of combined stroke subtypes, which could have obscured some differential associations of alcohol by pathological or aetiological subtype, as suggested by recent overviews from observational studies.7 In this context it is interesting to note than in a subset of studies, we found the rs1229984 A-allele associated with reduced odds of ischaemic stroke, but this requires replication.
One of the advantages of a mendelian randomisation study is that this design is less prone to some of the biases of observational studies. In contrast to observational analyses that have shown associations of alcohol with physical activity and different measures of smoking,32 rs1229984 A-allele was not associated with physical activity or any of the more precise measures of smoking exposure (cigarettes/day, pack years, or cotinine level). However, an association was observed with the binary ever/never smoking trait, but this was in the opposite direction to the association with coronary heart disease and is therefore unlikely to explain the association of rs1229984 A-allele with a reduced risk of coronary heart disease. There was also some evidence for a difference in years of education, and, while the size of the effect was small, this requires further investigation.
Strengths and weaknesses in relation to other studies
Our findings compare with findings from studies in east Asians, using the rs671 genetic variant of the aldehyde dehydrogenase 2 gene (ALDH2), that have also shown associations of alcohol with blood pressure, body mass index, and non-HDL cholesterol levels.21 22 However, the association with coronary heart disease events remains unclear since the association of ALDH2 with coronary heart disease has been analysed only in small studies.21 22 In contrast to our findings, ALDH2 rs671 has shown an association with HDL cholesterol levels in individuals of Asian ancestry.21 In Europeans the ALDH2 rs671 variant is monomorphic and cannot be used for mendelian randomisation, and previous studies have therefore used the ADH1B genotype to investigate the effect of alcohol on cardiovascular disease.20 23 33 34 Our results not only replicate findings of ADH1B on blood pressure and body mass index from smaller data collections, but expand the number of cardiovascular traits and include major vascular events. Given our large sample size, we are able to identify associations with other cardiovascular traits (non-HDL cholesterol, interleukin 6, and C reactive protein), and most notably we are able to detect for the first time an association with coronary heart disease.
One feature in common to both ALDH2 and AHD1B for mendelian randomisation is the use of genetic variants within loci that encode alcohol metabolising enzymes. In both examples, genetic variation results in altered exposure to acetaldehyde, a metabolite of alcohol that causes unpleasant symptoms, thought to be responsible for the different drinking behaviour in individuals who possess the alleles.35 Thus, a simple interpretation of a mendelian randomisation analysis using a genetic variant in an alcohol metabolising enzyme is that it is akin to a long term randomised trial of more versus less alcohol exposure.
Meaning of the study: possible explanations and implications for clinicians and policymakers and other researchers; how your study could promote better decisions
These data show that individuals of European descent with a genetic predisposition to consume less alcohol had a reduced risk of coronary heart disease and ischaemic stroke, and lower levels of several established and emerging risk factors for cardiovascular disease. These findings suggest that reductions of alcohol consumption, even for light to moderate drinkers, may be beneficial for cardiovascular health. Our results therefore challenge the concept of a cardioprotective effect associated with light to moderate alcohol consumption reported in observational studies and suggest that this effect may have been due to residual confounding or selection bias.
Unanswered questions and future research
Although the association of the ADH1B variant with coronary heart disease is compatible with being null in non-drinkers and a more pronounced association is seen in drinkers, future access to large scale population studies such as UK Biobank and China Kadoorie Biobank Study will help to minimise potential measurement error in alcohol exposure and provide sufficiently large numbers of coronary heart disease events to enable replication of our findings, in particular the analysis stratified by alcohol status, but will also allow a more detailed examination of stroke subtypes.
What is already known on this topic
Observational studies suggest that consuming alcohol in heavy amounts is deleterious for cardiovascular health, whereas light to moderate consumption may be protective
However, findings for light to moderate drinkers could be due to unaccounted bias
What this study adds
Use of a genetic approach in an analysis of over 260 000 participants showed that carriers of a variant in the alcohol dehydrogenase 1B gene (ADH1B) associated with less alcohol consumption were found to have a reduced risk of coronary heart disease, and this was maintained at all levels of alcohol consumption
Under the principles of mendelian randomisation, these findings suggest that reduction of alcohol consumption, even for light to moderate drinkers, is beneficial for cardiovascular health
Members of the InterAct Consortium and IMPROVE study group are listed in the supplementary appendix.
We thank Dr Kieran McCaul (Western Australian Centre for Health & Ageing, Centre for Medical Research, University of Western Australia, Perth, Western Australia, Australia) for help with analysis of the Health in Men Study (HIMS) cohort.
Contributors: All coauthors satisfy the recommendations outlined in the ICMJE Recommendations 2013. All coauthors provided substantial contributions to the conception or design of the work or acquisition, analysis, or interpretation of data for the work, and helped with drafting the work or revising it critically for important intellectual content. All coauthors approve this version of the manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. MVH, CED, and JPC are guarantors for the study, had full access to all of the data in the study, and take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding of individuals
Dr Michael V. Holmes is funded by a UK Medical Research Council (MRC) population health scientist fellowship (G0802432). Dr Abbas Dehghan is supported by NWO grant (veni, 916.12.154) and the EUR Fellowship. Dr James Meschia receives support from a Clinical Investigator grant from the Mayo Foundation for Medical Education and Research. Prof Mika Kivimaki was supported by the Medical Research Council; the British Heart Foundation; the Economic and Social Research Council; the National Heart Lung and Blood Institute (NHLBI: HL36310); and the National Institute on Aging (AG13196), US, NIH. Prof. Dr. J. W. Jukema is an Established Clinical Investigator of the Netherlands Heart Foundation (grant 2001 D 032). Dr Owen Ross is funded by the James and Ester King Foundation and the Florida State Department of Health, the American Heart Association and the Myron and Jane Hanley Award in Stroke research. Prof Sir Michael Marmot is supported by a Medical Research Council Professorship. Dr Johan Sundstrom is supported by the Swedish Heart-Lung Foundation (grant 20041151), the Swedish Research Council (grant 2007-5942). Dr. Alex Reiner was supported by a contract HHSN268200900009C from the NIH National Heart Lung and Blood Institute. Dr James Y. Dai was supported by a R01 grant from the National Heart Lung and Blood Institute (HL 114901). Prof Hugh Watkins and Prof Martin Farrall are members of the Oxford British Heart Foundation (BHF) Centre of Research Excellence. Dr Daniel Swerdlow was supported by a MRC doctoral training award, and acknowledges support of the UCL MBPhD programme. Prof Frank Dudbridge is supported by a MRC grant (G1000718). Dr Jaroslav Hubacek was supported by MH CZ - DRO („Institute for Clinical and Experimental Medicine - IKEM, IN 00023001“). Dr Richard Silverwood is supported by the UK Economic and Social Research Council (NCRM Pathways node, ES/I025561/2). Professor Steve E. Humphries is supported by the British Heart Foundation (PG/2008/008). Prof Kuh, Prof Hardy and Dr Wong were supported by the Medical Research Council (MC_UU_12019/1). Dr Folkert W. Asselbergs is supported by National Institute of Health Research University College London Hospitals Biomedical Research Centre and Netherlands Heart Foundation (2014T001). Dr. Jorgenson is supported by the National Institute on Alcohol Abuse and Alcoholism (NIAAA: AA021223-01). Ajna Hamidovic was funded by MD Scientist Fellowship in Genetic Medicine (Northwestern Memorial Foundation) and the National Research Service Award F32DA024920 (NIH/NIDA; Ajna Hamidovic). Dr. Spring’s work is supported by NIH HL075451. This work was supported in part by BHF Programme Grant RG/10/12/28456. Professors Lawlor and Davey Smith and Dr Zuccolo work in a research unit that receives funding from the UK Medical Research Council (MC_UU_12013/1 and MC_UU_12013/5). Dr. Buxbaum’s research is supported in part by P20MD006899 awarded by the National Institute on Minority Health and Health Disparities of the National Institutes of Health. Professors Aroon D. Hingorani and Juan P Casas are supported by the National Institute of Health Research University College London Hospitals Biomedical Research Centre.
Funding of studies
ALSPAC: We are extremely grateful to all of the families who took part in this study, the midwives for recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses. The research leading to the specific results from ALSPAC in this paper received funding from the Wellcome Trust (WT088806 and WT087997MA). The UK Medical Research Council and Wellcome Trust (092731), together with the University of Bristol, provide core support for the ALSPAC study. ARIC: The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C), R01HL087641, R01HL59367 and R01HL086694; National Human Genome Research Institute contract U01HG004402; and National Institutes of Health contract HHSN268200625226C. The authors thank the staff and participants of the ARIC study for their important contributions. Infrastructure was partly supported by Grant Number UL1RR025005, a component of the National Institutes of Health and NIH Roadmap for Medical Research; BWHHS: The British Women’s Heart and Health Study has been supported by funding from the British Heart Foundation (BHF) (grant PG/09/022) and the UK Department of Health Policy Research Programme (England) (grant 0090049). The BWHHS HumanCVD data were funded by the BHF (PG/07/131/24254); We thank all BWHHS participants, the general practitioners and their staff who have supported data collection since the study inception; BRHS: The British Regional Heart Study has been supported by programme grant funding from the British Heart Foundation (RG/08/013/25942); CARe: wishes to acknowledge the support of the National Heart, Lung and Blood Institute and the contributions of the research institutions, study investigators, field staff, and study participants in creating this resource for biomedical research (NHLBI contract number HHSN268200960009C); CARDIA: CARDIA is supported by contracts N01-HC-48047, N01-HC-48048, N01-HC-48049, N01-HC-48050 and N01-HC-95095 from the National Heart, Lung, and Blood Institute/National Institutes of Health; CFS: The Cleveland Family Study (CFS) was supported by grant HL46380 from the National Heart, Lung, and Blood Institute (NHLBI); CGPS: This study was supported by Herlev Hospital, Copenhagen University Hospital, The Copenhagen County Research Fund, and The Danish Medical Research Council; CHS: This research was supported by contracts HHSN268201200036C, HHSN268200800007C, N01 HC55222, N01HC85079, N01HC85080, N01HC85081, N01HC85082, N01HC85083, N01HC85086, N01HC65226, and grant HL080295 from the National Heart, Lung, and Blood Institute (NHLBI), with additional contribution from the National Institute of Neurological Disorders and Stroke (NINDS). Additional support was provided by AG023629 from the National Institute on Aging (NIA). A full list of principal CHS investigators and institutions can be found at CHS-NHLBI.org; Cyprus: The Cyprus Study has been supported by the Cyprus Cardiovascular Disease Educational and Research Trust (CCDERT) and Joint Cyprus Research Promotion Foundation, Ministry of Health and Cyprus Heart Foundation grant No 41/5PE as well as Research Promotion Foundation grants (PENEK 05/04 and YGEIA 04/06); EAS: The EAS was funded by the British Heart Foundation (Programme Grant RG/98002); ELSA: Samples from the English Longitudinal Study of Ageing (ELSA) DNA Repository (EDNAR), received support under a grant (AG1764406S1) awarded by the National Institute on Ageing (NIA). ELSA was developed by a team of researchers based at the National Centre for Social Research, University College London and the Institute of Fiscal Studies. The data were collected by the National Centre for Social Research.; EPIC InterAct: We thank all EPIC participants and staff for their contribution to the study. We thank staff from the Technical, Field Epidemiology and Data Functional Group Teams of the MRC Epidemiology Unit in Cambridge, UK, for carrying out sample preparation, DNA provision and quality control, genotyping and data-handling work. The InterAct study received funding from the European Union (Integrated Project LSHM-CT-2006-037197 in the Framework Programme 6 of the European Community); EPIC Netherlands: We thank Statistics Netherlands and Netherlands Cancer Registry (NKR) for follow-up data on cancer, cardiovascular disease, vital status and causes of death. Supported by the European Commission: Public Health and Consumer Protection Directorate 1993-2004; Research Directorate-General 2005; Dutch Ministry of Public Health, Welfare and Sports; Netherlands Cancer Registry; LK Research Funds; Dutch Prevention Funds; Dutch Zorg Onderzoek Nederland; and World Cancer Research Fund (The Netherlands) (to the European Prospective Investigation into Cancer and Nutrition-Netherlands study). The EPIC-NL study was funded by ‘Europe against Cancer’ Programme of the European Commission (SANCO), Dutch Ministry of Public Health, Welfare and Sports (VWS), Netherlands Cancer Registry (NKR), LK Research Funds, Dutch Prevention Funds, Dutch Cancer Society; ZonMW the Netherlands Organisation for Health Research and Development, World Cancer Research Fund (WCRF) (The Netherlands). Genotyping was funded by IOP Genomics grant IGE05012 from Agentschap NL; EPIC Norfolk: We thank all study participants and the general practitioners and the EPIC-Norfolk study team for their helpful input. The EPIC-Norfolk study is supported by programme grants from the Medical Research Council and Cancer Research UK; EPIC Potsdam: The recruitment phase of the EPIC-Potsdam Study was supported by the Federal Ministry of Science, Germany (01 EA 9401), and the European Union (SOC 95201408 05F02). The follow-up was supported by the German Cancer Aid (70-2488-Ha I) and the European Community (SOC 98200769 05F02). The present study was supported by the Federal Ministry of Education and Research (0312750B). Mercodia provided the oxLDL kits free of charge. JS and AFHP were supported by German Research Federal Ministry (BMBF), JS was supported by a Heisenberg-Professorship (SP716/1-1) and clinical research groups of the German Research Foundation (DFG; KFO192/1 and 218/1). JS, AFHP and MM were also supported by a graduate school of the DFG (GK1208); EPIC Turin: The EPIC Turin study is funded by grants from the Associazione Italiana per le Ricerche sul Cancro, Italy and grants from the Compagnia di San Paolo, Turin, Italy; FHS: The Framingham Heart Study began in 1948 with the recruitment of an original cohort of 5,209 men and women (mean age 44 years; 55 percent women). In 1971 a second generation of study participants was enrolled; this cohort consisted of 5,124 children and spouses of children of the original cohort. The mean age of the offspring cohort was 37 years; 52 percent were women. A third generation cohort of 4,095 children of offspring cohort participants (mean age 40 years; 53 percent women) was enrolled beginning in 2002. At each clinic visit, a medical history was obtained with a focus on cardiovascular content, and participants underwent a physical examination including measurement of height and weight from which BMI was calculated; HAPIEE: This study was supported by Wellcome Trust ‘Determinants of Cardiovascular Diseases in Eastern Europe: A multi-centre cohort study’ [grants 064947/Z/01/Z; and 081081/Z/06/Z]; the MacArthur Foundation ‘MacArthur Initiative on Social Upheaval and Health’ [grant 712058]; the National Institute on Ageing ‘Health disparities and aging in societies in transition (the HAPIEE study)’ [grant 1R01 AG23522]; and a project from the Ministry of Health, Czech Republic, for the development of the research organization No. 00023001 (IKEM, Prague, Czech Republic). We would like to thank researchers, interviewers and participants in Novosibirsk, Krakow, Kaunas, Havířov/Karviná, Jihlava, Ústí nad Labem, Liberec, Hradec Králové, and Kromĕříz.; HIMS: National Health and Medical Research Council (NHMRC) project grants 279408, 379600, 403963, 513823 and 634492; HPFS/NHS: We would like to thank Hardeep Ranu and Pati Soule from the DF/HCC Genotyping Core for genotyping and data management. This study was supported by research grants HL35464, CA55075, CA87969, AA11181, and HL34594 from the National Institute of Health, Bethesda; M.D; IMPROVE: This study was supported by the European Commission (Contract number: QLG1- CT- 2002- 00896), Ministero della Salute Ricerca Corrente, Italy, the Swedish Heart-Lung Foundation, the Swedish Research Council (projects 8691 and 0593), the Foundation for Strategic Research, the Stockholm County Council (project 562183), the Foundation for Strategic Research, the Academy of Finland (Grant #110413) and the British Heart Foundation (RG2008/014). None of the aforementioned funding organizations or sponsors has had a specific role in design or conduct of the study, collection, management, analysis, or interpretation of the data, or preparation, review, or approval of the manuscript; Inter99: The Inter99 study was supported by the Danish Medical Research Council, the Danish Centre for Evaluation and Health Technology Assessment, Copenhagen County, the Danish Heart Foundation, the Danish Pharmaceutical Association, the Health Insurance Foundation, the Augustinus Foundation, the Ib Henriksens foundation and the Beckett Foundation. The present study was further supported by the Danish Diabetes Association (grant No. 32, December 2005) and the Health Insurance Foundation (grant No. 2010 B 131); ISGS/SWISS: ISGS (Grant Number R01 42733) and SWISS (R01 NS39987) were funded by grants from the National Institute of Neurological Disorders and Stroke (US); Izhevsk: The Izhevsk Family Studies was funded by a UK Wellcome Trust programme grant (078557); MDC: This work was supported by the Swedish Medical Research Council; by the Swedish Heart and Lung Foundation; by the Medical Faculty of Lund University, Malmo University Hospital; by the Albert Pahlsson Research Foundation; by the Crafoord foundation; by the Ernhold Lundstroms Research Foundation, the Region Skane; by the Hulda and Conrad Mossfelt Foundation; by the King Gustaf V and Queen Victoria Foundation; by the Lennart Hanssons Memorial Fund; and by the Marianne and Marcus Wallenberg Foundation. Genotyping was supported by the British Heart Foundation (grant number CH/98001 to A.F.D., RG/07/005/23633 to A.F.D., S.P.); MESA: The Multi-Ethnic Study of Atherosclerosis Study (MESA) is a multicenter prospective cohort study initiated to study the development of subclinical cardiovascular disease. A total of 6814 women and men between the age of 45 and 84 year were recruited for the first examination between 2000 and 2002. Participants were recruited in six US cities (Baltimore, MD; Chicago, IL; Forsyth County, NC; Los Angeles County, CA; Northern Manhattan, NY; and St. Paul, MN). This study was approved by the institutional review boards of each study site, and written informed consent was obtained from all participants. This cohort was genotyped as part of the National Heart Lung and Blood Institute’s (NHLBI) Candidate Gene Association Resource (CARe) (Musunuru, K., Lettre, G., Young, T., Farlow, D.N., Pirruccello, J.P., Ejebe, K.G., Keating, B.J., Yang, Q., Chen, M.H., Lapchyk, N. et al. Candidate gene association resource (CARe): design, methods, and proof of concept. Circ. Cardiovasc. Genet, 3, 267-275.); MRC 1958BC: Dr Sue Ring and Dr Wendy McArdle (University of Bristol) and Mr Jon Johnson (Centre for Longitudinal Studies, Institute of Education, London) are thanked for help with data linkage. The study was supported by the Academy of Finland (12926) and the Medical Research Council (MRC G0601653 and SALVE/PrevMedsyn). The Medical Research Council funded the 2002-2004 clinical follow-up of the 1958 birth cohort (grant G0000934). This research used resources provided by the Type 1 Diabetes Genetics Consortium, a collaborative clinical study sponsored by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institute of Allergy and Infectious Diseases, National Human Genome Research Institute, National Institute of Child Health and Human Development, and Juvenile Diabetes Research Foundation International (JDRF) and supported by U01 DK062418. This study makes use of data generated by the Wellcome Trust Case-Control Consortium. A full list of investigators who contributed to generation of the data is available from the Wellcome Trust Case-Control Consortium website(www.wtccc.org.uk). Funding for the project was provided by the Wellcome Trust under award 076113. Work at the Centre for Paediatric Epidemiology and Biostatistics benefits from funding support from the MRC in its capacity as the MRC Centre of Epidemiology for Child Health. Research at the University College London Institute of Child Health and Great Ormond Street Hospital for Children NHS Trust benefits from R&D funding received from the NHS Executive; MRC NSHD: Supported by Medical Research Council -- MC_UU_12019/1. We are very grateful to the members of this birth cohort for their continuing interest and participation in the study. We would like to acknowledge the Swallow group, UCL, who performed the DNA extractions; NHANES III: The findings and conclusions in this report are those of the author(s) and do not necessarily represent the views of the Centers for Disease Control and Prevention; NORDIL: This work was supported by the British Heart Foundation (grant number CH/98001 to A.F.D., RG/07/005/23633 to A.F.D., S.P.) and a Special Project, for genotyping of the Swedish extremes from the NORDIL and MDC cohorts; and by Pharmacia. We thank Professor Thomas Hedner (Department of Clinical Pharmacology, Sahlgrenska Academy, Gotheburg, Sweden) and Professor Sverre Kjeldsen (Ullevaal University Hospital, University of Oslo, Oslo, Norway), who are investigators of the NORDIL study. Professor Kjeldsen is also an investigator of the ASCOT trial; NPHS II: NPHS-II was supported by the British Medical Research Council, the US National Institutes of Health (grant NHLBI 33014), and Du Pont Pharma, Wilmington, Delaware; Portuguese stroke: Instituto Nacional de Saude Doutor Ricardo Jorge; PREVEND: PREVEND genetics is supported by the Dutch Kidney Foundation (Grant E033), The Netherlands organisation for health research and development (ZonMw grant 90.700.441), and the Dutch Inter University Cardiology Institute Netherlands (ICIN); PROCARDIS: PROCARDIS was supported by the EU FP7 Program (LSHM‐CT‐2007‐037273), AstraZeneca, the British Heart Foundation, the Oxford BHF Centre of Research Excellence, the Wellcome Trust core award (090532/Z/09/Z), the Swedish Research Council, the Knut and Alice Wallenberg Foundation, the Swedish Heart‐Lung Foundation, the Torsten and Ragnar Söderberg Foundation, the Strategic Cardiovascular Program of Karolinska Institutet and Stockholm County Council, the Foundation for Strategic Research and the Stockholm County Council (560283); PROSPER: The PROSPER study was supported by an investigator initiated grant obtained from Bristol-Myers Squibb and by grants from the Interuniversity Cardiology Institute of the Netherlands (ICIN) and the Durrer Center for Cardiogenetic Research both Institutes of the Netherlands Royal Academy of Arts and Sciences (KNAW), the Netherlands Heart Foundation, the Center for Medical Systems Biology (CMSB), a center of excellence approved by the Netherlands Genomics Initiative/Netherlands Organisation for Scientific Research (NWO), the Netherlands Consortium for Healthy Ageing (NCHA). The research leading to these results has received funding from the European Union’s Seventh Framework Programme (FP7/2007-2013) under grant agreement n° HEALTH-F2-2009-223004 and by the Netherlands Genomics Initiative (Netherlands Consortium for Healthy Aging grant 050-060-810); Rotterdam: The Rotterdam Study is supported by the Erasmus Medical Center and Erasmus University Rotterdam; the Netherlands Organization for Scientific Research (NWO); the Netherlands Organization for Health Research and Development (ZonMw); the Research Institute for Diseases in the Elderly (RIDE); the Netherlands Heart Foundation; the Ministry of Education, Culture and Science; the Ministry of Health Welfare and Sports; the European Commission; and the Municipality of Rotterdam. Support for genotyping was provided by the Netherlands Organisation of Scientific Research NWO Investments (nr. 175.010.2005.011, 911-03-012), the Research Institute for Diseases in the Elderly (014-93-015; RIDE2), the Netherlands Genomics Initiative (NGI)/Netherlands Consortium for Healthy Aging (NCHA) project nr. 050-060-810; SMART: SMART GENETICS was financially supported by BBMRI-NL, a Research Infrastructure financed by the Dutch government (NWO 184.021.007); TPT: TPT was funded by the Medical Research Council, the British Heart Foundation, DuPont Pharma and Bayer Corporation; UCP: The UCP study was funded by Veni grant Organization for Scientific Research (NWO), Grant no. 2001.064 Netherlands Heart Foundation (NHS), and TI Pharma Grant T6-101 Mondriaan. The department of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences, has received unrestricted research funding from the Netherlands Organisation for Health Research and Development (ZonMW), the Dutch Health Care Insurance Board (CVZ), the Royal Dutch Pharmacists Association (KNMP), the private-public funded Top Institute Pharma (www.tipharma.nl, includes co-funding from universities, government, and industry), the EU Innovative Medicines Initiative (IMI), EU 7th Framework Program (FP7), the Dutch Medicines Evaluation Board, the Dutch Ministry of Health and industry (including GlaxoSmithKline, Pfizer, and others); Whitehall II: The Whitehall II study and Mika Kivimaki were supported by the Medical Research Council; the British Heart Foundation; the Economic and Social Research Council; the National Heart Lung and Blood Institute (NHLBI: HL36310); and the National Institute on Aging (AG13196), US, NIH; WHI: The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201100003C, HHSN268201100004C, and HHSN271201100004C. A listing of WHI investigators can be found at https://cleo.whi.org/researchers/Documents%20%20Write%20a%20Paper/WHI%20Investigator%20Short%20List.pdf.
Statement of independence from funders: All researchers acted independently of study funders. The study funders played no role in study design and the collection, analysis, and interpretation of data and the writing of the article and the decision to submit it for publication. None of the funders influenced the data analysis or interpretation of results. The comments made in this paper are those of the authors and not necessarily those of any funders.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: Prof Whittaker is 90% employed by GlaxoSmithKline and own shares in GlaxoSmithKline. All other coauthors report no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Data sharing statement: No additional data available
Transparency declaration: The lead authors, MVH, CED, and JPC (the manuscript’s guarantors) affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Cite this as: BMJ 2014;349:g4164
Related links
bmj.com/archive
Web Extra. Supplementary appendix supplied by the author
References
- 1.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rehm J, Baliunas D, Borges GL, Graham K, Irving H, Kehoe T, et al. The relation between different dimensions of alcohol consumption and burden of disease: an overview. Addiction 2010;105:817-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freiberg MS, Samet JH. Alcohol and coronary heart disease: the answer awaits a randomized controlled trial. Circulation 2005;112:1379-81. [DOI] [PubMed] [Google Scholar]
- 4.O’Keefe JH, Bybee KA, Lavie CJ. Alcohol and cardiovascular health: the razor-sharp double-edged sword. J Am Coll Cardiol 2007;50:1009-14. [DOI] [PubMed] [Google Scholar]
- 5.Hansel B, Thomas F, Pannier B, Bean K, Kontush A, Chapman MJ, et al. Relationship between alcohol intake, health and social status and cardiovascular risk factors in the Urban Paris-Ile-de-France Cohort: is the cardioprotective action of alcohol a myth? Eur J Clin Nutr 2010;64:561-8. [DOI] [PubMed] [Google Scholar]
- 6.Corrao G, Rubbiati L, Bagnardi V, Zambon A, Poikolainen K. Alcohol and coronary heart disease: a meta-analysis. Addiction 2000;95:1505-23. [DOI] [PubMed] [Google Scholar]
- 7.Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 2011;342:d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boffetta P, Garfinkel L. Alcohol drinking and mortality among men enrolled in an American Cancer Society prospective study. Epidemiology 1990;1:342-8. [DOI] [PubMed] [Google Scholar]
- 9.Shaper AG, Wannamethee G, Walker M. Alcohol and mortality in British men: explaining the U-shaped curve. Lancet 1988;2:1267-73. [DOI] [PubMed] [Google Scholar]
- 10.Jackson R, Broad J, Connor J, Wells S. Alcohol and ischaemic heart disease: probably no free lunch. Lancet 2005;366:1911-2. [DOI] [PubMed] [Google Scholar]
- 11.Brien SE, Ronksley PE, Turner BJ, Mukamal KJ, Ghali WA. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ 2011;342:d636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Briel M, Ferreira-Gonzalez I, You JJ, Karanicolas PJ, Akl EA, Wu P, et al. Association between change in high density lipoprotein cholesterol and cardiovascular disease morbidity and mortality: systematic review and meta-regression analysis. BMJ 2009;338:b92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwartz GG, Olsson AG, Abt M, Ballantyne CM, Barter PJ, Brumm J, et al. Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med 2012;367:2089-99. [DOI] [PubMed] [Google Scholar]
- 14.Hingorani A, Humphries S. Nature’s randomised trials. Lancet 2005;366:1906-8. [DOI] [PubMed] [Google Scholar]
- 15.Davey Smith G, Ebrahim S. ‘Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol 2003;32:1-22. [DOI] [PubMed] [Google Scholar]
- 16.Edenberg HJ. The genetics of alcohol metabolism: role of alcohol dehydrogenase and aldehyde dehydrogenase variants. Alcohol Res Health 2007;30:5-13. [PMC free article] [PubMed] [Google Scholar]
- 17.Yokoyama A, Yokoyama T, Mizukami T, Matsui T, Kimura M, Matsushita S, et al. Blood ethanol levels of nonabstinent Japanese alcoholic men in the morning after drinking and their ADH1B and ALDH2 genotypes. Alcohol Alcoholism 2013. 10.1093/alcalc/agt136. [DOI] [PubMed] [Google Scholar]
- 18.Macgregor S, Lind PA, Bucholz KK, Hansell NK, Madden PA, Richter MM, et al. Associations of ADH and ALDH2 gene variation with self report alcohol reactions, consumption and dependence: an integrated analysis. Hum Molecular Genetics 2009;18:580-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bierut LJ, Goate AM, Breslau N, Johnson EO, Bertelsen S, Fox L, et al. ADH1B is associated with alcohol dependence and alcohol consumption in populations of European and African ancestry. Molecular Psychiatry 2012;17:445-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lawlor DA, Nordestgaard BG, Benn M, Zuccolo L, Tybjaerg-Hansen A, Davey Smith G. Exploring causal associations between alcohol and coronary heart disease risk factors: findings from a Mendelian randomization study in the Copenhagen General Population Study. Eur Heart J 2013;34:2519-28. [DOI] [PubMed] [Google Scholar]
- 21.Kato N, Takeuchi F, Tabara Y, Kelly TN, Go MJ, Sim X, et al. Meta-analysis of genome-wide association studies identifies common variants associated with blood pressure variation in east Asians. Nature Genetics 2011;43:531-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen L, Davey Smith G, Harbord RM, Lewis SJ. Alcohol intake and blood pressure: a systematic review implementing a Mendelian randomization approach. PLoS Med 2008;5:e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Drogan D, Sheldrick AJ, Schutze M, Knuppel S, Andersohn F, di Giuseppe R, et al. Alcohol consumption, genetic variants in alcohol deydrogenases, and risk of cardiovascular diseases: a prospective study and meta-analysis. PloS One 2012;7:e32176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Keating BJ, Tischfield S, Murray SS, Bhangale T, Price TS, Glessner JT, et al. Concept, design and implementation of a cardiovascular gene-centric 50 k SNP array for large-scale genomic association studies. PloS One 2008;3:e3583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.InterAct Consortium, Langenberg C, Sharp S, Forouhi NG, Franks PW, Schulze MB, et al. Design and cohort description of the InterAct Project: an examination of the interaction of genetic and lifestyle factors on the incidence of type 2 diabetes in the EPIC Study. Diabetologia 2011;54:2272-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Del Boca FK, Darkes J. The validity of self-reports of alcohol consumption: state of the science and challenges for research. Addiction 2003;98(suppl 2):1-12. [DOI] [PubMed] [Google Scholar]
- 28.Glymour MM, Tchetgen EJ, Robins JM. Credible Mendelian randomization studies: approaches for evaluating the instrumental variable assumptions. AmJ Epidemiol 2012;175:332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hindorff LA, MacArthur J, Morales J, Junkins HA, Hall PN, Klemm AK, et al. A catalog of published genome-wide association studies. National Human Genome Research Institute. www.genome.gov/gwastudies (accessed Feb 2013).
- 30.Marmot MG, Davey Smith G, Stansfeld S, Patel C, North F, Head J, et al. Health inequalities among British civil servants: the Whitehall II study. Lancet 1991;337:1387-93. [DOI] [PubMed] [Google Scholar]
- 31.Voight BF, Kang HM, Ding J, Palmer CD, Sidore C, Chines PS, et al. The metabochip, a custom genotyping array for genetic studies of metabolic, cardiovascular, and anthropometric traits. PLoS Gen 2012;8:e1002793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Room R. Smoking and drinking as complementary behaviours. Biomed Pharmacother 2004;58:111-5. [DOI] [PubMed] [Google Scholar]
- 33.Tolstrup JS, Gronbaek M, Nordestgaard BG. Alcohol intake, myocardial infarction, biochemical risk factors, and alcohol dehydrogenase genotypes. Circ Cardiovasc Genet 2009;2:507-14. [DOI] [PubMed] [Google Scholar]
- 34.Husemoen LL, Jorgensen T, Borch-Johnsen K, Hansen T, Pedersen O, Linneberg A. The association of alcohol and alcohol metabolizing gene variants with diabetes and coronary heart disease risk factors in a white population. PLoS One 2010;5:e11735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Quertemont E, Didone V. Role of acetaldehyde in mediating the pharmacological and behavioral effects of alcohol. Alcohol Res Health 2006;29:258-65. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.