Abstract
Background
Sub-anesthetic ketamine infusions may benefit a variety of psychiatric disorders, including addiction. Though ketamine engenders transient alterations in consciousness, it is not known whether these alterations influence efficacy. This analysis evaluates the mystical-type effects of ketamine, which may have therapeutic potential according to prior research, and assesses whether these effects mediate improvements in dependence-related deficits, 24 h postinfusion.
Methods
Eight cocaine dependent individuals completed this double-blind, randomized, inpatient study. Three counter-balanced infusions separated by 48 h were received: lorazepam (2 mg) and two doses of ketamine (0.41 mg/kg and 0.71 mg/kg, with the former dose always preceding the latter). Infusions were followed within 15 min by measures of dissociation (Clinician Administered Dissociative Symptoms Scale: CADSS) and mystical-type effects (adapted from Hood's Mysticism Scale: HMS). At baseline and 24 h postinfusion, participants underwent assessments of motivation to stop cocaine (University of Rhode Island Change Assessment) and cue-induced craving (by visual analogue scale for cocaine craving during cue exposure).
Results
Ketamine led to significantly greater acute mystical-type effects (by HMS) relative to the active control lorazepam; ketamine 0.71 mg/kg was associated with significantly higher HMS scores than was the 0.41 mg/kg dose. HMS score, but not CADSS score, was found to mediate the effect of ketamine on motivation to quit cocaine 24 h postinfusion.
Conclusions
These findings suggest that psychological mechanisms may be involved in some of the anti-addiction benefits resulting from ketamine. Future research can evaluate whether the psychoactive effects of ketamine influence improvements in larger samples.
Keywords: Cocaine, Dependence, Ketamine, Mystical experience
1. Introduction
A single sub-anesthetic infusion of ketamine (0.5 mg/kg over 40 min intravenously, IV) has been found to rapidly improve depressive symptoms, with benefits peaking at 24 h postinfusion (when active metabolites are at negligible serum levels) and generally subsiding by 72 h (Mathew et al., 2012; Skolnick et al., 2009; Zarate et al., 2006). This unique response has been attributed to enhanced neuroplasticity via various downstream effects (Li et al., 2010; Maeng et al., 2008), improved prefrontal glutamate homeostasis (Salvadore et al., 2009), and sustained attenuations in default mode network connectivity and activity (Scheidegger et al., 2012). Ketamine may address dependence-related deficits through comparable mechanisms. We previously reported that ketamine improves low motivation to quit and cue-induced craving in non-depressed cocaine dependent volunteers (Dakwar et al., 2013).
An intriguing but unexplored question is whether the psychoactive effects of ketamine influence its efficacy through psychological mechanisms. At the therapeutic doses studied to date, ketamine elicits an array of psychoactive effects, which tend to resolve entirely within 30 min postinfusion (Perry et al., 2007). These effects include dissociative phenomena, as well as alterations in consciousness similar to those engendered by serotonergic hallucinogens (Perry et al., 2007; Vollenweider and Kometer, 2010). The latter effects may be particularly relevant to therapeutic mechanism. Recent research suggests that the 5HT-2A agonist psilocybin occasions altered states of enduring personal importance and possible benefit in healthy volunteers (Griffiths et al., 2006, 2008).
These experiences were similar to mystical states that might spontaneously emerge over the normal course of life, and which are imbued with sacred, spiritual, or existential significance (Griffiths et al., 2006; Hoffer, 1970; Miller and C'de Baca, 2001).
The role of mystical states in robust clinical improvement has been frequently noted in the literature on recovery, with individuals reporting that efforts toward abstinence were promoted by experiences with mystical characteristics (Miller and C'de Baca, 2001; Miller, 2004). It is, therefore, possible that the improvements in cocaine users we reported previously were influenced by ketamine-induced mystical-type phenomena. This analysis examines the mystical-type effects of the ketamine infusions administered previously (Dakwar et al., 2013) and investigates whether these phenomena mediate ketamine efficacy, 24 h postin-fusion. We predict that ketamine infusions dose-dependently promote transient mystical-type effects, assessed with items from a widely used mystical experience scale (Hood, 1975; Hood et al., 2001). Further, we predict that the intensity of the mystical experience, but not of dissociative phenomena, serves to mediate the effects of the initial ketamine dose (0.41 mg/kg over 52 min) on motivation to quit cocaine and cue-induced craving.
2. Methods
2.1. Participants
Eight cocaine dependent individuals not seeking treatment or abstinence, actively using free-base (“crack”) cocaine, and describing a history of cue-induced craving underwent psychiatric screening, including a Structured Clinical Interview for the Diagnostic Statistical Manual, 4th edition (DSM-IV SCID), as well as a medical evaluation. All participants were in good health, had no history of ketamine use, and denied past or current psychiatric disorders other than substance use disorders. Participants were hospitalized for 9 days, and were abstinent on days 1 through 3 before being randomized to one of three infusion orders. Our Institutional Review Board approved all procedures.
2.2. Infusions
Three 52-min infusions (2-min bolus followed by 50 min infusion) separated by 48 h were administered in a randomized double-blind manner to each participant: ketamine 0.41 mg/kg (K1) or 0.71 mg/kg (K2) (0.11 mg/kg over 2 min followed by 0.3 mg/kg or 0.6 mg/kg slow-drip over 50 min, respectively) or lorazepam 2 mg (LZP) (saline bolus over 2 min followed by 2 mg slow-drip over 50 min). There were three possible orders: K1, K2, LZP; LZP, K1, K2; and K1, LZP, K2. K1 always preceded K2 for safety reasons.
Participants were monitored for 2 h after the infusion ended, and were interviewed 20 min and 1 h post-infusion, with special attention given to persistent symptomatology that might merit concern, such as sedation, psychosis or dissociation.
2.3. Assessments
Assessments of motivation to quit cocaine and cue-induced craving occurred at baseline and at 24 h post-infusion. Motivation to quit cocaine was assessed using the University of Rhode Island Change Assessment (URICA), a 32-item questionnaire validated to ascertain readiness for change in cocaine users (DiClemente and Hughes, 1990; Siegal et al., 2001). Cue-induced craving was ascertained by summing serial (every 3 min) visual analogue scale (VAS) assessments of craving over 15 min of cocaine cue exposure.
2.4. Mystical-type effects
Acute mystical-type effects were assessed with items from the Hood's Mysticism Scale (HMS; Hood, 1975; Hood et al., 2001). The questionnaire was modified for the purposes of this study. First, the verb tense of items was changed to focus on infusion-related phenomena rather than on lifetime experience (Maclean et al., 2012). Second, the questionnaire was shortened. To reduce redundancy and facilitate administration, negative items were removed (e.g., I did not experience a perfectly peaceful state), while each of the eight dimensions, and all three factors (Hood, 1975; Hood et al., 2001), were represented by at least one item, leaving nine items (see Table 1).
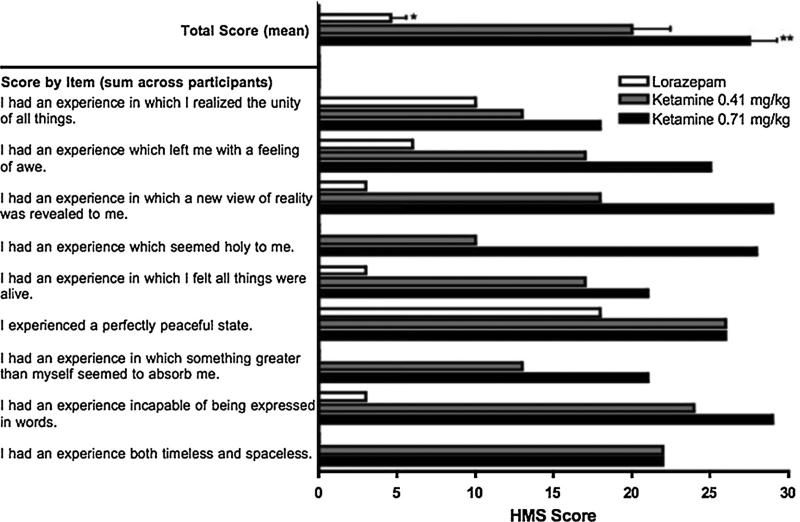
Table 1.
Mean hood mystical experience scale (HMS) Score for each infusion condition by total score and item score (n = 8). For total score, bars represent mean score, and error bars represent standard errors of the mean (SEM); median values are available in Findings. For item scores, bars represent sum values across participants. Scoring for each item was based on a 5-point scale: 0 = definitely not true of my experience; 1 = probably not true; 2 = undecided; 3 = probably true; 4 = definitely true. HMS score associated with lorazepam (LZP) was significantly different from both ketamine 0.41 mg/kg (K1) and ketamine 0.71 mg/kg (K2), * p = 0.012. HMS scores associated with K1 and K2 were also significantly different, ** p = 0.027.
|
Items were administered within 15 min of infusion termination alongside other measures, including a VAS of drug liking, Clinician Administered Dissociative Symptoms Scale (CADSS), and four items pertaining to psychosis from the Brief Psychiatric Rating Scale. Scoring was consistent with the 5-point HMS scale, and HMS scores were calculated as the total sum (maximum possible score = 36).
2.5. Statistics
To evaluate whether ketamine led to mystical-type effects, HMS scores were compared by Friedman's 2-way analyses of variance (ANOVA) (medication (LZP, K1, K2) by order (three possible orders)) and paired Bonferroni-corrected Wilcoxon signed-rank tests. Non-parametric tests were used because of small sample sizes (n = 8), with 2-tailed α = 0.05.
Because we have previously shown that K1 (0.41 mg/kg) led to a significant ~60% change from preceding values for both primary outcomes (craving VAS and URICA), while the efficacy of K2 (always received after K1) could not be fully evaluated due to order and carry-over effects (Dakwar et al., 2013), analyses of HMS or CADSS scores as mediators were conducted with data from K1 relative to LZP only.
Four mediation analyses were conducted using the approach proposed by Baron and Kenny (1986). One set of analyses tested CADSS score as a mediator, with URICA or sum VAS alternately designated as dependent variables, and another tested HMS score as a mediator. Mediation was supported if the mediator remained a significant predictor when controlling for infusion condition, and if infusion condition ceased to be a significant predictor when controlling for the mediator (Baron and Kenny, 1986). Because multiple comparisons were tested, α was adjusted to 0.0125 to minimize Type I error.
3. Results
3.1. Participants
Eight adult participants with high mean baseline cocaine use (22 use days in 4 weeks, at $158.83 per use day) completed the study (see Dakwar et al., 2013 for other participant characteristics). All participants tolerated study procedures without adverse events, including unexpected psychiatric disturbances and initiation of ketamine or benzodiazepine misuse.
3.2. Mystical-type effects
All psychoactive effects, including dissociative and mystical-type phenomena, resolved within 20 min postinfusion. Both doses of ketamine led to significant elevations in HMS score relative to lorazepam (LZP vs. K1, median 4 vs. 22; LZP vs. K2, median 4 vs. 30; p = 0.012; mean values and standard errors of the mean are shown in Fig. 1). Additionally, K2 led to significantly greater mystical-type effects by HMS compared to K1 (30 vs. 22, p = 0.027). The test for order effects was not significant. A linear regression testing for correlations between HMS and CADSS scores for K1 was non-significant (R2 = 0.261, p = 0.12).
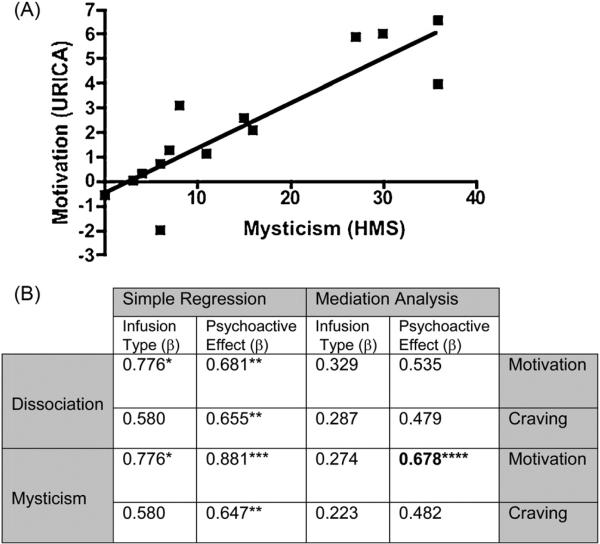
Fig. 1.
(A) Regression plot assessing correlation between mystical experience and change in motivation to quit and (B) β values calculated from simple regressions and mediation analyses with respect to change in dependent variables (motivation to quit and cue-induced craving) for ketamine-induced dissociation (CADSS score) or mysticism (HMS score), as well as infusion type (lorazepam vs. ketamine). The correlation between mystical experience and change in motivation to quit is represented in (A), and remained significant when controlling for infusion type (lorazepam vs. ketamine 0.41 mg/kg), β = 0.678, p = 0.005. The relationship between HMS score and motivation to quit was the only association to remain significant after mediation analyses were performed (B). This suggests that mystical-type phenomena might mediate the effect of ketamine on motivation enhancement. * p = 0.001, ** p = 0.012, *** p < 0.001, **** p = 0.005.
3.3. Mediation
The only analysis to fulfill the criteria for mediation was that testing the mediating role of HMS score with respect to URICA score (adjusted R2 for the total model = 0.775, p < 0.005). Infusion condition also ceased to be significant when controlling for HMS score (β = 0.776 in an uncontrolled regression, p < 0.001; β = 0.274 after controlling for HMS score, p = 0.19; Fig. 1).
4. Discussion
Two main findings emerged from this study. The first is that sub-anesthetic ketamine significantly and dose-dependently generated mystical-type phenomena. Second, the intensity of these transient effects was found to mediate (at 24 h postinfusion) the therapeutic effect of ketamine on motivation to quit cocaine, but not on cue-induced craving. These results indicate that the mystical-type effects of ketamine may influence its efficacy, and suggest a psychological mechanism by which ketamine might exert certain benefits.
While the dissociative effects of ketamine have been well characterized (Perry et al., 2007), its mystical-type effects have not. A single previous study (Lofwall et al., 2006) had examined the mystical-type effects of ketamine (by the intramuscular, IM, route), and found that it did not significantly generate mystical phenomena relative to placebo. Our data suggest that pharmacologically elicited mystical states may be dose-dependent, as has also been shown with psilocybin (Griffiths et al., 2006, 2008). Thus, the lack of observed effect in the previous study might be attributed to the reduced bioavailability of ketamine by the IM route compared to IV (Clements et al., 1982) as well as the low doses administered (0.2 mg/kg and 0.4 mg/kg; Lofwall et al., 2006).
The finding that HMS score was found to influence the effect of ketamine on motivation to quit is consistent with the hypothesis, first proposed by James (1907) more than a century ago, that mystical experience might be psychologically beneficial. According to James and more recent psychologists, mystical experience may impact most directly on the existential dimensions of personhood, such as moral values, self-identity, and purpose (James, 1907; Miller and C'de Baca, 2001; Miller, 2004). This may explain why HMS score was correlated so robustly with motivation to quit, which implicates many of these dimensions (Miller and C'de Baca, 2001; Miller, 2004). It also provides a rationale for the failure of HMS score to mediate improvements in cue-induced craving, a deficit only partly influenced by the perspectival shifts (Wilson et al., 2004) that might result from mystical-type phenomena. Important vulnerabilities that ostensibly involve an existential dimension, and which have responded robustly to ketamine previously, include such depressive symptoms as hopelessness, guilt, and suicidality (Mathew et al., 2012; Price et al., 2009; Skolnick et al., 2009; Zarate et al., 2006).
This study also suggests that a framework aimed at harnessing the therapeutic potential of these psychoactive effects may optimize efficacy, at least for certain vulnerabilities. Ketamine Psychedelic Therapy (KPT), for example, incorporates 1 or 2 sessions of ketamine-facilitated existential reappraisal into an existential psychotherapy, and preliminary controlled trials suggest that it effectively promotes long-term abstinence in alcohol or opioid dependent individuals (Krupitsky and Grinenko, 1997; Krupitsky et al., 2002). The approach of KPT, as of other therapies aimed at the pharmacological production of a transformative experience, is predicated on two notions: that the quality of the experience is crucial to efficacy, and that efficacy is enhanced by patient preparation and the treatment context (Hoffer, 1970; Johnson et al., 2008; Vollenweider and Kometer, 2010). Some research has aimed to clarify how various factors might shape psychoactive responses to other agents (Studerus et al., 2011, 2012), but this has not been studied for ketamine. Our findings suggest that by adequately screening and preparing individuals, administering infusions under controlled conditions, and providing postinfusion support, investigators can effectively minimize the risks of ketamine, such as its abuse liability and behavioral toxicity (Dakwar et al., 2013), while also allowing for its possibly beneficial psychoactive effects to safely emerge.
An important limitation is that we cannot conclusively determine from these preliminary results whether mystical-type effects constitute a true mediator or whether they are simply a marker of potency or efficacy. Two findings, however, lend support to the hypothesis of mediation. First, we failed to find a significant correlation between HMS and CADSS scores in individuals receiving K1, suggesting that HMS score did not reflect general psychoactive potency for that dose (though this should be interpreted conservatively in light of a small sample). Similarly, mystical-type effects were not found to mediate general efficacy, even as the improvements in cue-induced craving and motivation to quit were comparable in magnitude (Dakwar et al., 2013). These results, taken together, suggest that a discrete set of psychoactive effects, as ascertained by the HMS, served to influence a particular category of improvements. Larger, adequately powered studies are needed to confirm this hypothesis.
Other limitations also reflect the preliminary nature of this study. The sample was small and homogenous. Factors that might impact on the effects of ketamine were not explored, such as a family history of alcoholism or serum levels (Mathew et al., 2012; Petrakis et al., 2004). In addition, the study was not designed to test how mystical-type effects might mediate drug use reductions in follow-up, because there was no control group that did not receive ketamine. Finally, though the basic dimensions of the HMS were retained, shortening the questionnaire may have impacted on our capacity to obtain more nuanced information on psychoactive effects, particularly when comparing the two ketamine dosages.
Despite these limitations, this analysis demonstrates that sub-anesthetic ketamine engenders mystical-type effects in a dose-dependent fashion, and that these transient effects may mediate improvements in motivation to quit cocaine, 24 h postinfusion. Future research can evaluate whether mystical-type effects influence the therapeutic effects of ketamine in larger clinical samples. Researchers can also consider evaluating whether ketamine efficacy is improved by utilizing a clinical framework aimed at enhancing and consolidating the apparent psychological benefits emerging from its psychoactive effects.
Acknowledgments
Role of funding sources: The authors thank the National Institutes of Health for supporting this study with the following grants: MH081870, DA022412, DA031771, DA035472, DA009236, and DA007294.
Drs. Dakwar, Hart, Levin, and Nunes also acknowledge the support of Columbia College of Physicians and Surgeons, and the New York State Psychiatric Institute. Dr. Mathew is supported by the Brown Foundation, Inc., and the Michael E. DeBakey VA Medical Center, Houston, TX.
Footnotes
Author disclosures
Contributors: ED devised the study, obtained funding for it, and wrote the manuscript. ED, CH, and FL carried out study procedures. CA, CH, FL, SM, and EN edited and revised the manuscript. All authors contributed to and approved the final manuscript.
Conflict of interest
Dr. Mathew has been named as an inventor on a pending use-patent of ketamine for the treatment of depression. Dr. Mathew has relinquished his claim to any royalties and will not benefit financially if ketamine were approved for this use. Dr. Mathew has received consulting fees or research support from AstraZeneca, Bristol-Myers Squibb, Naurex, Noven, Roche Pharmaceuticals, and Takeda. The other authors have no conflicts to report.
References
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic and statistical considerations. J. Pers. Soc. Psychol. 1986;51:173–182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Clements JA, Nimmo WS, Grant IS. Bioavailability, pharmacokinetics, and analgesic activity of ketamine in humans. J. Pharm. Sci. 1982;71:539–542. doi: 10.1002/jps.2600710516. [DOI] [PubMed] [Google Scholar]
- Dakwar E, Levin FR, Foltin RW, Nunes EV, Hart CL. The effects of subanesthetic ketamine infusions on motivation to quit and cue-induced craving in cocaine-dependent research volunteers. Biol. Psych. 2013 Sep 11; doi: 10.1016/j.biopsych.2013.08.009. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiClemente CC, Hughes SO. Stages of change profiles in outpatient alcoholism treatment. J. Subst. Abuse. 1990;2:217–235. doi: 10.1016/s0899-3289(05)80057-4. [DOI] [PubMed] [Google Scholar]
- Griffiths RR, Richards W, Johnson M, McCann U, Jesse R. Mystical-type experiences occasioned by psilocybin mediate the attribution of personal meaning and spiritual significance 14 months later. J. Psychopharmacol. 2008;22:621–632. doi: 10.1177/0269881108094300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths RR, Richards WA, McCann U, Jesse R. Psilocybin can occasion mystical-type experiences having substantial and sustained personal meaning and spiritual significance. Psychopharmacology. 2006;187:268–283. doi: 10.1007/s00213-006-0457-5. discussion 284–292. [DOI] [PubMed] [Google Scholar]
- Hoffer A. Therapeutic uses. In: Aaronson B, Osmond H, editors. Psychedelics: The Uses and Implications of Hallucinogenic Drugs. Hogarth Press; London: 1970. pp. 357–366. [Google Scholar]
- Hood RW. The construction and preliminary validation of a measure of reported mystical experience. J. Sci. Study Relig. 1975;14:29–41. [Google Scholar]
- Hood RW, Ghorbani N, Watson PJ, Ghramaleki AF, Bing MN, Davison HK, Morris RJ, Williamson WP. Dimensions of the mysticism scale: confirming the three-factor structure in the United States and Iran. J. Sci. Study Relig. 2001;40:691–705. [Google Scholar]
- James W. The Varieties of Religious Experience: A Study in Human Nature. Oxford World's Classics; Oxford: 1907. [Google Scholar]
- Johnson M, Richards W, Griffiths R. Human hallucinogen research: guidelines for safety. J. Psychopharmacol. 2008;22:603–620. doi: 10.1177/0269881108093587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krupitsky E, Burakov A, Romanova T, Dunaevsky I, Strassman R, Grinenko A. Ketamine psychotherapy for heroin addiction: immediate effects and two-year follow-up. J. Subst. Abuse Treat. 2002;23:273–283. doi: 10.1016/s0740-5472(02)00275-1. [DOI] [PubMed] [Google Scholar]
- Krupitsky E, Grinenko AY. Ketamine psychedelic therapy (KPT): a review of the results of ten years of research. J. Psychoactive Drugs. 1997;29:165–183. doi: 10.1080/02791072.1997.10400185. [DOI] [PubMed] [Google Scholar]
- Li N, Lee B, Liu RJ, Banasr M, Dwyer JM, Iwata M, Li XY, Aghajanian G, Duman RS. mTOR-dependent synapse formation underlies the rapid antidepressant effects of NMDA antagonists. Science. 2010;20:959–964. doi: 10.1126/science.1190287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lofwall MR, Griffiths RR, Mintzer MZ. Cognitive and subjective acute dose effects of intramuscular ketamine in healthy adults. Exp. Clin. Psychopharmacol. 2006;14:439–449. doi: 10.1037/1064-1297.14.4.439. [DOI] [PubMed] [Google Scholar]
- Maclean KA, Leoutsakos JM, Johnson MW, Griffiths RR. Factor analysis of the Mystical Experience Questionnaire: a study of experiences occasioned by the hallucinogen psilocybin. J. Sci. Study Relig. 2012;51:721–737. doi: 10.1111/j.1468-5906.2012.01685.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maeng S, Zarate CA, Jr., Du J, Schloesser RJ, McCammon J, Chen G, Manji HK. Cellular mechanisms underlying the antidepressant effects of ketamine: role of alpha-amino-3-hydroxy-5-methylisoxazole-4-proprionic acid receptors. Biol. Psychiatry. 2008;63:349–352. doi: 10.1016/j.biopsych.2007.05.028. [DOI] [PubMed] [Google Scholar]
- Mathew SJ, Shah A, Lapidus K, Clark C, Jarun N, Ostermeyer B, Murrough JW. Ketamine for treatment-resistant unipolar depression: current evidence. CNS Drugs. 2012;26:189–204. doi: 10.2165/11599770-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, C'de Baca J. Quantum Change: When Epiphanies and Sudden Insights Transform Ordinary Lives. Guilford; New York, NY.: 2001. [Google Scholar]
- Miller WR. The phenomenon of quantum change. J. Clin. Psychol. 2004;5:453–460. doi: 10.1002/jclp.20000. [DOI] [PubMed] [Google Scholar]
- Perry EB, Cramer JA, Cho HS, Petrakis IL, Karper LP, Genovese A, O'Donnell E, Krystal JH, D'Souza DC. Psychiatric safety of ketamine in psychopharmacology research. Psychopharmacology. 2007;192:253–260. doi: 10.1007/s00213-007-0706-2. [DOI] [PubMed] [Google Scholar]
- Petrakis IL, Limoncelli D, Gueorguieva R, Jatlow P, Boutros NN, Trevisan L, Gelernter J, Krystal JH. Altered NMDA glutamate receptor antagonist response in individuals with a family vulnerability to alcoholism. Am. J. Psychiatry. 2004;161:1776–1782. doi: 10.1176/ajp.161.10.1776. [DOI] [PubMed] [Google Scholar]
- Price RB, Nock MK, Charney DS, Mathew SJ. Effects of intravenous ketamine on explicit and implicit measures of suicidality in treatment-resistant depression. Biol. Psychiatry. 2009;66:522–526. doi: 10.1016/j.biopsych.2009.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvadore G, Cornwell BR, Colon-Rosario V, Coppola R, Grillon C, Zarate CA, Manji HK. Increased anterior cingulate cortical activity in response to fearful faces: a neurophysiological biomarker that predicts rapid antidepressant response to ketamine. Biol. Psychiatry. 2009;65:289–295. doi: 10.1016/j.biopsych.2008.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheidegger M, Walter M, Lehmann M, Metzger C, Grimm S, Boeker H, Boesiger P, Henning A, Seifritz E. Ketamine decreases resting state functional network connectivity in healthy subjects: implications for antidepressant drug action. PLoS One. 2012;7:e44799. doi: 10.1371/journal.pone.0044799. http://dx.doi.org/10.1371/journal.pone.0044799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegal HA, Li L, Rapp RC, Saha P. Measuring readiness for change among crack cocaine users: a descriptive analysis. Subst. Use Misuse. 2001;36:687–700. doi: 10.1081/ja-100104085. [DOI] [PubMed] [Google Scholar]
- Skolnick P, Popik P, Trullas P. Glutamate-based antidepressants: 20 years on. Trends Pharmacol. Sci. 2009;30:563–569. doi: 10.1016/j.tips.2009.09.002. [DOI] [PubMed] [Google Scholar]
- Studerus E, Gamma A, Kometer M, Vollenweider FX. Prediction of psilocybin response in healthy volunteers. PloS One. 2012;7:e30800. doi: 10.1371/journal.pone.0030800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Studerus E, Kometer M, Hasler F, Vollenweider FX. Acute, subacute and long-term subjective effects of psilocybin in healthy humans: a pooled analysis of experimental studies. J. Psychopharmacol. 2011;25:1434–1452. doi: 10.1177/0269881110382466. [DOI] [PubMed] [Google Scholar]
- Vollenweider FX, Kometer M. The neurobiology of psychedelic drugs: implications for the treatment of mood disorders. Nat. Rev. Neurosci. 2010;11:642–651. doi: 10.1038/nrn2884. [DOI] [PubMed] [Google Scholar]
- Wilson SJ, Sayette MA, Fiez JA. Prefrontal responses to drug cues: a neurocognitive analysis. Nat. Neurosci. 2004;7:211–214. doi: 10.1038/nn1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarate CA, Singh JB, Carlson BP, Brutsche NE, Ameli R, Luckenbaugh DA, Charney DS, Manji HK. A randomized trial of an N-methyl-d-aspartate antagonist in treatment-resistant depression. Arch. Gen. Psychiatry. 2006;63:856–864. doi: 10.1001/archpsyc.63.8.856. [DOI] [PubMed] [Google Scholar]