Abstract
Background
The diagnosis of blunt abdominal trauma can be challenging and resource intensive. Observation with serial clinical assessments plays a major role in the evaluation of these patients, but the time required for intra-abdominal injury to become clinically apparent is unknown. The purpose of this study was to determine the amount of time required for an intra-abdominal injury to become clinically apparent after blunt abdominal trauma via physical examination or commonly followed clinical values.
Methods
A retrospective review of patients who sustained blunt trauma resulting in intra-abdominal injury between June 2010 and June 2012 at a Level 1 academic trauma center was performed. Patient demographics, injuries, and the amount of time from emergency department admission to sign or symptom development and subsequent diagnosis were recorded. All diagnoses were made by computed tomography or at the time of surgery. Patient transfers from other hospitals were excluded.
Results
Of 3,574 blunt trauma patients admitted to the hospital, 285 (8%) experienced intra-abdominal injuries. The mean (SD) age was 36(17) years, the majority were male (194 patients, 68%) and the mean (SD) Injury Severity Score (ISS) was 21 (14). The mean (SD) time from admission to diagnosis via computed tomography or surgery was 74 (55) minutes. Eighty patients (28%) required either surgery (78 patients, 17%) or radiographic embolization (2 patients, 0.7%) for their injury. All patients who required intervention demonstrated a sign or symptom of their intra-abdominal injury within 60 minutes of arrival, although two patients were intervened upon in a delayed fashion. All patients with a blunt intra-abdominal injury manifested a clinical sign or symptom of their intra-abdominal injury, resulting in their diagnosis within 8 hours 25 minutes of arrival to the hospital.
Conclusion
All diagnosed intra-abdominal injuries from blunt trauma manifested clinical signs or symptoms that could prompt imaging or intervention, leading to their diagnosis within 8 hours 25 minutes of arrival to the hospital. All patients who required an intervention for their injury manifested a sign or symptom of their injury within 60 minutes of arrival.
Level of Evidence
Therapeutic study, level IV Epidemiologic study, level III.
Keywords: Blunt trauma, intra-abdominal injury, 8 hours, 60 minutes, clinically apparent
The accurate and timely diagnosis of blunt intra-abdominal injury (IAI) is a common dilemma. The accuracy of physical examination has been questioned by multiple previous studies,1,2 while others have suggested that the optimal method of diagnosis is via serial examination by an experienced trauma surgeon.3,4 Unfortunately, these studies do not define the period that is needed for IAIs to become clinically apparent.
Differing periods of observation both in the emergency department and as an inpatient have been proposed in the literature to identify clinically relevant injuries after trauma.5–8 The largest study by Poletti et al. arbitrarily used a 23-hour period of observation and, in retrospect, identified a missed injury rate of just 0.5%, suggesting that this is not warranted in all trauma patients. However, we could find no data in the literature that described the time frame necessary for an IAI to manifest itself. The period of observation chosen by previous studies was determined solely by expert opinion. This duration, if known, could be used to define the optimal period of observation required to identify clinically significant injuries following blunt abdominal trauma.
The purpose of this study was to determine the length of time necessary for an IAI to become apparent after blunt abdominal trauma based on commonly followed clinical findings. Our hypothesis is that an IAI in a patient after blunt trauma will become clinically evident via a commonly followed sign or symptom within 12 hours of presentation to the hospital.
Patients and Methods
The Denver Health Medical Center (DHMC) Trauma Registry was queried for all blunt trauma patients with an IAI from June 2010 to June 2012. DHMC is a state-cerified and American College of Surgeons-verified level I regional trauma center and an intergral teaching facitlity of the University of Colorado School of Medicine. These records were reviewed for general patient demographics, mechanism of injury, Injury Severity Score (ISS), timing and results of initial and subsequent physical examinations, Focused Abdominal Sonogram for Trauma (FAST) results, complete blood count and urinalysis, imaging and operative intervention for the abdominal injury, and overall survival. Patient transfers from other facilities were excluded.
At DHMC, all trauma patients immeditiatly undergo full physical assessment as per the Advanced Trauma and Life Support protocol.9 Bedsides FAST, cervical-spine, chest, and pelvis x-rays are performed when indicated, and an initial laboratory panel is drawn, which includes a complete blood cell (CBC) count, basic metabolic panel, and coagulation studies. Blunt abdominal trauma patients who are mentally intact (Glasgow Coma Scale [GCS] score of 15 and oriented to person, place, and time) with an initially normal physical examination finding, a negative FAST result, and normal laboratory results do not undergo initial computed tomography (CT) and are observed in the emergency department. This common practice of observation includes serial physical and FAST examinations as well as a repeat CBC count at 8 hours to 12 hours after arrival.10 However, this practice has varied in the past and can be altered at the trauma surgeon's discretion.3,8,11
The amount of time required for an IAI to manifest was defined as the time from emergency department arrival to the first documentation of a sign or symptom commonly associated with IAIs (Table 1). For ease of categorization, these were arbitrarily prioritized based on the authors' experience as follows: (1) vital signs; (2) unevaluable patient (intubated and sedated or GCS < 15 who is not oriented, intoxicated, or combatative); (3) abdominal examination findings such as peritonitis, significant pain, abrasions, or a seat belt sign; (4) other concerning examination findings commonly associated with an IAI including lower chest wall, flank, or lumbar spine tenderness; (6) positive FAST result with stable vital signs; (7) distracting or severe associated injuries, for example, pelvic, femur, spinal, multiple lower rib fractures, or multiple long bone fractures; (8) unexplained, altered white blood cell count, hemoglobin, gross hematuria, or microscopic red blood cell count greater than 100 cells/mL; and (9) high-energy mechanism or attending discretion (when no other indicator was identified before imaging or intervention).2,8,12–19 When two or more clinical indicators were apparent at the same time, the higher priority sign or symptom was recorded as the prompting sign or symptom. All diagnoses were made by CT or surgery. The University of Colorado Multi-Institutional Review Board approved this study (COMIRB #13-0244).
Table 1. Definition of Signs or Symptoms Prompting the Diagnosis.
| Vital signs | Hypotension (SBP < 90 mm Hg) or delayed tachycardia |
| Unevaluable patient | Intubated and sedated, altered mental status |
| Abdominal examination findings | Abdominal pain, peritonitis or significant tenderness, seat belt sign, significant abrasions |
| Other examination findings | Flank, spine, pelvic, lower chest wall tenderness |
| Distracting injuries | Pelvic or femur fractures, multiple long bone fractures, multiple lower rib fractures, sternal fracture |
| Unexplained abnormal laboratory values | CBC count, UA |
| Severe mechanism | When none of the above identified before diagnosis |
Patients with a GCS score of less than 15 were considered to have an altered mental status. CBC count was considered abnormal with when either the white blood cell count or hemoglobin was out of the normal range. UA was considered abnormal if there was evidence of hematuria.
SBP, systolic blood pressure; UA, urinalysis.
Results
During a 2-year period 3,574 blunt trauma patients were admitted to the DHMC, and 285 (8%) were diagnosed with IAIs. Of those 285 patients with an IAI, the mean (SD) age was 36 (17) years, the majority was male (68%), and the mean (SD) ISS was 21 (14). The most common mechanism of injury was a motor vehicle collision in 127 patients (45%), followed by motorcycle crashes (40 patients, 14%), and auto pedestrian collisions (41 patients, 14%) (Table 2). The majority of the injuries included isolated liver or spleen injuries (139 patients, 49%), followed by patients with multiple solid organ injuries (60 patients, 21%). Just 9 patients (3.2%) experienced isolated hollow viscus injuries, although an additional 14 patients (5.0%) had concomitant solid organ injuries, for a total of 25 hollow viscus injuries (8.8%) (Table 3).
Table 2. Mechanisms of Injury.
| Mechanism | Patients (n = 285), n (%) |
|---|---|
| Motor vehicle crash | 127 (45) |
| Motorcycle crash | 40 (14) |
| Auto pedestrian collision | 41 (14) |
| Falls | 27 (9.5) |
| Bicycle crash | 18 (6.3) |
| Assault | 17 (6.0) |
| Sports/all-terrain vehicle/miscellaneous | 15 (5.3) |
The most common mechanism in patients diagnosed with an IAI was motor vehicle crashes.
Table 3. Distribution of IAIs and Interventions.
| Injury | Patients | Patients Requiring Intervention, n (%) |
|---|---|---|
| Multiple IAIs | 74 | 31 (42) |
| Isolated liver injury | 70 | 10 (14) |
| Isolated spleen injury | 69 | 12 (17) |
| Isolated genitourinary | 33 | 15(45) |
| Isolated hollow viscus | 9 | 6 (6.7) |
| Other | 30 | 6 (20) |
| Total | 285 | 80 (28) |
Fourteen of the patients with multiple IAIs included both hollow viscus and solid organs; the remaining 60 experienced multiple solid organ injuries. “Other” injuries included retroperitoneal and/or vascular injuries.
Of the 285 patients with IAIs diagnosed at our facility, 52(18%) underwent immediate CT or intervention because they were deemed unevaluable owing to altered mental status or endotracheal intubation with sedation. The remaining 233 patients (82%) exhibited specific clinical abnormalities prompting CT or intervention, resulting in the diagnosis (and management in the case of surgery) of their injury (Fig. 1). The two patients (0.7%) who were found to have a severe mechanism as an indication for diagnosis were involved in high-speed (>55 mph) motor vehicle accidents with significant vehicular damage and/or a death at the scene; both patients also exhibited a sign or symptom of their injury within 6 hours of arrival.
Figure 1.
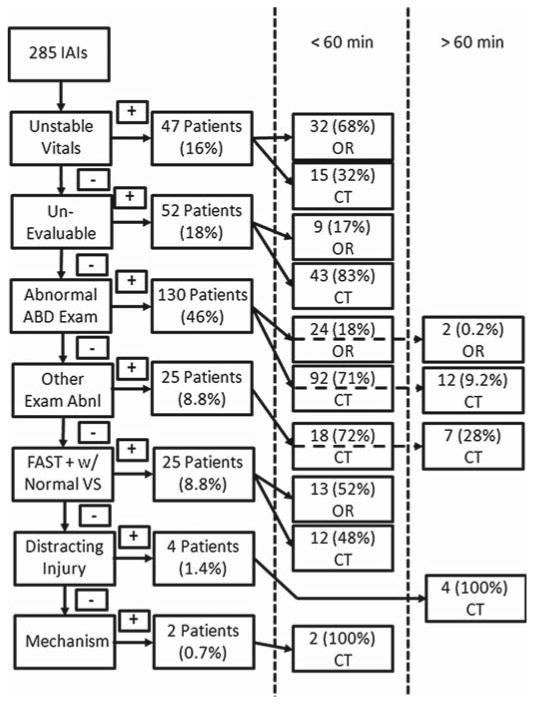
The pathway to diagnosis after blunt abdominal trauma. Unstable vitals are considered to be a systolic blood pressure less than 90 mmHg and/or new or delayed onset tachycardia of greater than 100 beats per minute. Unevaluable patients are those with a CCS score of less than 15 and/or clinical intoxication or combativeness. Abnormal abdominal examination findings included peritonitis, significant tenderness, or a seat belt sign. Other examination abnormalities indicative of an IAI included significant lower chest wall, flank, or lumbar spine tenderness. Distracting injuries include multiple lower rib fractures, pelvic fractures, or long bone fractures. A severe mechanism includes motor vehicle collisions at faster than 55 mph or a death at the scene. ABD, abdominal; Abnl, abnormal; OR, operating room; IR, interventional radiology.
Of the 285 patients with an IAI, 80 (28%) required either surgery (78 patients, 17%) or radiographic embolization (2 patients, 0.7%) for their injury (Table 3 and 4). Of these 80 patients, 78 (98%) proceeded directly to the operating room or radiology suite within 1 hour of arrival. Two patients underwent a delay in the diagnosis and subsequent intervention owing to initial inappropriate triage as nontrauma. However, both demonstrated signs or symptoms of their injury within 1 hour of arrival. Despite the delay, neither patient experienced additional complications following exploration for their hollow viscus or splenic injury.
Table 4. Signs or Symptoms Leading to the Diagnosis via Imaging or Intervention.
| Clinical Indicator | Total (n = 285) | Intervention for Abdominal Injury (n = 80) |
|---|---|---|
| Vital signs | 47 | 32 |
| Unevaluable | 52 | 9 |
| Abdominal examination | 130 | 26 |
| Other examination | 25 | 0 |
| FAST+ (hemodynamically normal) | 25 | 13 |
| Distracting injury | 4 | 0 |
| Mechanism | 2 | 0 |
The majority of patients had an abnormal physical examination finding, which prompted the diagnosis in both groups. Patients included in the FAST+ group all demonstrated at least one quadrant with free fluid on the FAST examination but had normal vitals.
Two hundred sixty patients (91%) were diagnosed within this first 60 minutes of arrival, while the remaining 25 patients underwent serial examinations and a repeat CBC count 6 hours to 12 hours after arrival, resulting in their diagnosis. All 285 patients demonstrated a sign or symptom prompting diagnosis by either CT or intervention within 8 hours 25 minutes of arrival, with a mean (SD) time to diagnosis of 74 (55) minutes (Fig. 2). All patients with an IAI that required an intervention demonstrated a sign or symptom of their injury within 60 minutes of arrival.
Figure 2.
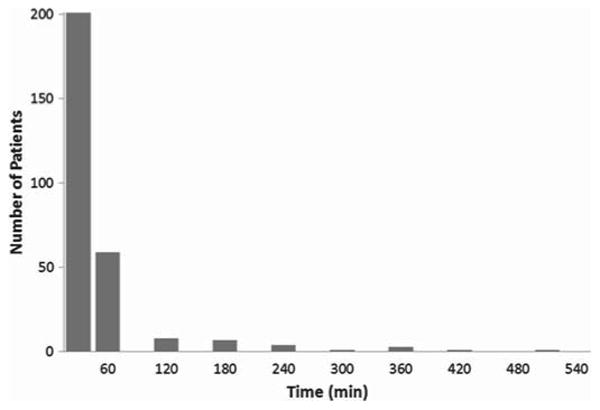
The number of patients diagnosed at 30-minute intervals after arrival. The majority of patients were diagnosed within 60 minutes of arrival by physical examination alone, although one patient required 8 hours 25 minutes to manifest symptoms of their injury.
Discussion
We reviewed our experience with more than 3,500 blunt trauma admissions, resulting in 285 IAIs diagnosed at our facility during a 2-year period to determine the length of time required for patients with IAIs to manifest via commonly measured clinical variables. Interestingly, all patients who ultimately required an intervention for their IAI developed a clinical sign or symptom within 1 hour of arrival to the hospital. For the entire population, all patients with blunt IAIs demonstrated a sign or symptom of their injury within 8 hours 25 minutes of arrival to the DHMC.
A consistent, evidence-based duration for serial clinical assessments or a time course for the clinical presentation of IAIs is lacking. Differing periods of observation have been proposed to reasonably exclude additional traumatic injuries.5–8 Direct comparison of these studies is challenging because each apply a different management algorithm. An earlier study from our institution by Kendall et al. most closely follows our current system and found that just 6% of blunt trauma patients required admission with an IAI rate of 0.4% after observation for a median 9.5 hours in the emergency department. Our study differs from this and previous studies in that we are not evaluating a blunt abdominal trauma protocol. Rather, we sought to define the time interval required for known IAIs to manifest themselves through commonly followed clinical signs or symptoms. This information can then be used to determine the optimal duration for observation of patients after blunt abdominal trauma.
Our study is not without limitations. The retrospective identification of specific clinical variables prompting the imaging or intervention is prone to error because there is no way to confirm the actual indication or constellation of signs and symptoms considered by the bedside clinician. In addition, the hierarchy of clinical signs and symptoms was designed for ease of categorization based on the authors' experience but may not be applicable in all situations. The specific signs and symptoms we evaluated are supported by the literature.2,12–15 While the intent of this study does not include the evalution of our blunt abdominal trauma protocol, it is impossible to describe the natural course of an IAI without chronicling our management algorithm. Thus, more or less frequent examinations, laboratory evaluations, or imaging may have resulted in more efficient or cost-effective management of these patients and warrant further study.
Conclusion
Of the 3,574 blunt trauma patients admitted to the DHMC during the 2-year study period, all diagnosed IAIs exhibited clinical signs or symptoms that could prompt imaging or intervention within 8 hours 25 minutes of arrival to the hospital. All patients who required intervention for their IAI demonstrated a clinical sign or symptom of their injury within 60 minutes of arrival. These periods should be considered when establishing protocols for the management of blunt abdominal trauma.
Footnotes
Authorship: E.L.J. and R.T.S. designed this study. E.L.J, R.T.S., and T.S.J. collected the data, and all authors contributed to the data analysis and interpretation. E.L.J., R.T.S., and T.S.J. prepared the manuscript, which was critically reviewed by D.D.B., C.C.B., J.L.J., G.J.J., C.C.B., and E.E.M.
Disclosure: The authors declare no conflicts of interest.
References
- 1.Rodriguez A, DuPriest RW, Jr, Shatney CH. Recognition of intraabdominal injury in blunt trauma victims. A prospective study comparing physical examination with peritoneal lavage. Am Surg. 1982;48(9):457–459. [PubMed] [Google Scholar]
- 2.Schurink GW, Bode PJ, van Luijt PA, van Vugt AB. The value of physical examination in the diagnosis of patients with blunt abdominal trauma: a retrospective study. Injury. 1997;28(4):261–265. doi: 10.1016/s0020-1383(97)00007-7. [DOI] [PubMed] [Google Scholar]
- 3.McAnena OJ, Moore EE, Marx JA. Initial evaluation of the patient with blunt abdominal trauma. Surg Clin North Am. 1990;70(3):495–515. doi: 10.1016/s0039-6109(16)45126-1. [DOI] [PubMed] [Google Scholar]
- 4.Hoff WS, Holevar M, Nagy KK, Patterson L, Young JS, Arrillaga A, Najarian MP, Valenziano CP, Eastern Association for the Surgery of Trauma Practice management guidelines for the evaluation of blunt abdominal trauma: the EAST practice management guidelines work group. J Trauma. 2002;53(3):602–615. doi: 10.1097/00005373-200209000-00038. [DOI] [PubMed] [Google Scholar]
- 5.Cowell VL, Ciraulo D, Gabram S, Lawrence D, Cortes V, Edwards T, Jacobs L. Trauma 24-hour observation critical path. J Trauma. 1998;45(1):147–150. doi: 10.1097/00005373-199807000-00030. [DOI] [PubMed] [Google Scholar]
- 6.Poletti PA, Mirvis SE, Shanmuganathan K, Takada T, Killeen KL, Perlmutter D, Hahn J, Mermillod B. Blunt abdominal trauma patients: can organ injury be excluded without performing computed tomography? J Trauma. 2004;57(5):1072–1081. doi: 10.1097/01.ta.0000092680.73274.e1. [DOI] [PubMed] [Google Scholar]
- 7.Stephan PJ, McCarley MC, O'Keefe GE, Minei JP. 23-Hour observation solely for identification of missed injuries after trauma: is it justified? J Trauma. 2002;53(5):895–900. doi: 10.1097/00005373-200211000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Kendall JL, Kestler AM, Whitaker KT, Adkisson MM, Haukoos JS. Blunt abdominal trauma patients are at very low risk for intra-abdominal injury after emergency department observation. West J Emerg Med. 2011;12(4):496–504. doi: 10.5811/westjem.2010.11.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American College of Surgeons. Advanced Trauma Life Support Program for Physicians: ATLS. 8th. Chicago, IL: American College of Surgeons; 2008. [Google Scholar]
- 10.Harris HW, Morabito DJ, Mackersie RC, Halvorsen RA, Schecter WP. Leukocytosis and free fluid are important indicators of isolated intestinal injury after blunt trauma. J Trauma. 1999;46:656–659. doi: 10.1097/00005373-199904000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Branney SW, Moore EE, Cantrill SV, Burch JM, Terry SJ. Ultrasound based key clinical pathway reduces the use of hospital resources for the evaluation of blunt abdominal trauma. J Trauma. 1997;42:1086–1090. doi: 10.1097/00005373-199706000-00017. [DOI] [PubMed] [Google Scholar]
- 12.Mackersie RC, Tiwary AD, Shackford SR, Hoyt DB. Intra-abdominal injury following blunt trauma: identifying the high-risk patient using objective risk factors. Arch Surg. 1989;124:809–813. doi: 10.1001/archsurg.1989.01410070063013. [DOI] [PubMed] [Google Scholar]
- 13.Soderstrom CA, McArdle DQ, Ducker TB, Militello PR. The diagnosis of intra-abdominal injury in patients with cervical cord trauma. J Trauma. 1983;23(12):1061–1065. doi: 10.1097/00005373-198312000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Grieshop NA, Jacobson LE, Gomez GA, Thompson CT, Solotkin KC. Selective use of computed tomography and diagnostic peritoneal lavage in blunt abdominal trauma. J Trauma. 1995;38(5):727–731. doi: 10.1097/00005373-199505000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Chandler CF, Lane JS, Waxman KS. Seatbelt sign following blunt trauma is associated with increased incidence of abdominal injury. Am Surg. 1997;63(10):885–888. [PubMed] [Google Scholar]
- 16.Beck D, Marley R, Salvator A, Muakkassa F. Prospective study of the clinical predictors of a positive abdominal computed tomography in blunt trauma patients. J Trauma. 2004;57(2):296–300. doi: 10.1097/01.ta.0000130612.60661.c3. [DOI] [PubMed] [Google Scholar]
- 17.Griffin XL, Pullinger R. Are diagnostic peritoneal lavage or focused abdominal sonography for trauma safe screening investigations for hemodynamically stable patients after blunt abdominal trauma? A review of the literature. J Trauma. 2007;62(3):779–784. doi: 10.1097/01.ta.0000250493.58701.ad. [DOI] [PubMed] [Google Scholar]
- 18.Gad MA, Saber A, Farrag S, Shams ME, Ellabban GM. Incidence, patterns, and factors predicting mortality of abdominal injuries in trauma patients. N Am J Med Sci. 2012;4(3):129–134. doi: 10.4103/1947-2714.93889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burney RE, Mueller GL, Coon WW, Thomas EJ, Mackenzie JR. Diagnosis of isolated small bowel injury following blunt abdominal trauma. Ann Emerg Med. 1983;12:71–74. doi: 10.1016/s0196-0644(83)80374-6. [DOI] [PubMed] [Google Scholar]


