Abstract
Objective
Diphenhydramine is an H1 histamine antagonist that is commonly used for allergic reactions, colds and cough, and as a sleep aid. In addition to anticholinergic and antihistaminergic effects, sodium channel blockade becomes evident following diphenhydramine overdose. While seizures may occur following overdose of a diphenhydramine, status epilepticus is distinctly uncommon. We report a case with both status epilepticus and wide-complex dysrhythmias following an intentional diphenhydramine overdose.
Case report
A 36-year-old woman with a medical history of hypothyroidism on levothyroxine was brought to the emergency department with active seizures by emergency medical services after what was later determined to be a diphenhydramine overdose. One hour after an argument with her husband he found her lethargic in a locked room. Initial vital signs were: blood pressure, 90/55 mmHg; heart rate, 160 beats/min; respiratory rate 18 breaths/min; room air oxygen saturation, 99%; temperature, 99.8°F; rapid point-of-care glucose, 130 mg/dL. The generalized seizures continued for duration of 30 min, despite the intravenous administration of 8 mg of lorazepam. The patient underwent endotracheal intubation and a propofol infusion terminated her seizures. An electrocardiogram after the status was terminated which revealed a wide-complex tachycardia with QRS duration of 127 ms. The QRS narrowed after 200 mEq of intravenous sodium bicarbonate was administrated. The patient was neurologically intact upon extubation on hospital day 2. The serum diphenhydramine concentration drawn on arrival to the ED was 1200 ng/mL (9–120 ng/ mL); a tricyclic screen was negative.
Discussion
While seizures and sodium channel blockade are recognized complications of diphenhydramine toxicity, reported cases of status epilepticus from diphenhydramine overdose are rare. Elements of the patient’s presentation were similar to a tricyclic overdose and management required aggressive control of her seizures, sodium bicarbonate therapy, and recognizing that physostigmine was contraindicated due to wide complex tachycardia.
Conclusions
Diphenhydramine overdose may cause status epilepticus and wide-complex tachycardia. Management should focus on antidotal therapy with sodium bicarbonate and supportive neurological management with appropriate anticonvulsants and airway protection if clinically indicated.
Keywords: Heart, CNS/psychological, Other
Introduction
Diphenhydramine, an H1 histamine receptor antagonist, is commonly used for allergic reactions and found in a variety of cold medication preparations and sleep aid products.1 According to one survey, diphenhydramine is the sixth most commonly used medication in the USA.2 Antihistamines, in particular, diphenhydramine are frequently involved in suicide attempts, likely due to their over-the-counter accessibility. Diphenhydramine is also implicated either in isolation or in combination with other medications in fatal poisonings.3,4
Diphenhydramine is a member of the ethanolamine class of antihistamine, which as a class exhibit sedative and anticholinergic properties. Diphenhydramine is rapidly absorbed and distributed, which accounts for its relatively rapid onset of action.3 Early symptoms can range from neuroexcitation to sedation or somnolence.5
Diphenhydramine overdose may mimic that of a tricyclic antidepressant. In addition to anticholinergic toxicity, patients with diphenhydramine overdose may also manifest cardiotoxicity, such as wide complex tachycardia, and neurotoxicity, including sedation and seizures. We report a case of status epilepticus and a wide-complex tachycardia following intentional diphenhydramine overdose. While up to 10% of cases of status epilepticus presenting to the emergency department (ED) may result from drug toxicity,6 a search of the literature suggests that status epilepticus from diphenhydramine overdose is uncommon.
Case report
A 33-year-old woman weighing 47 kg was brought to the ED by emergency medical services (EMS) with active seizures. Her medical history included hypothyroidism for which she was prescribed levothyroxine. According to EMS personnel, the patient reportedly was in her normal state of health approximately 2 h prior to her presentation. After an argument with her husband, she locked herself in her room. About an hour later the husband went to check on the patient where she was found lethargic and minimally responsive. EMS did not find any pill bottles or unusual objects on scene. While the patient was being transported to the, ED she developed a generalized tonic-clonic seizure that terminated within 1–2 min without any pharmacologic intervention, but recurred on arrival to the ED.
On presentation to the ED, the patient was minimally responsive to pain. Vital signs were as follows: blood pressure, 90/55 mmHg; heart rate, 160 beats/min; respiratory rate, 18 breaths/min; room air oxygen saturation, 99%; temperature, 99.8°F; rapid point-of-care glucose, 130 mg/dL. Her heart and lung examinations were unremarkable. The abdomen was soft, and bowel sounds were normal. The general neurologic examination did not reveal any focal findings. She did have spontaneous tonic-clonic movement. The rest of the neurologic examination could not be performed due to continuous seizures. Her generalized seizures consisted of diffuse tonic-clonic movements in 1–2 min periods that were recurrent with no noticeable refractory period. The patient was given intravenous lorazepam at a dose of 2 mg repeated twice, and then 4 mg for a total of 8 mg in the 30-min time period with no apparent effect. At this time, with the inability to control her seizures and concern for possible aspiration, the patient underwent endotracheal intubation facilitated with 100 mg of succinylcholine and 100 mg of propofol. The patient’s seizure terminated with the propofol and did not recur even well after the effects of succinylcholine wore off. Aside from serial examination, the patient did not undergo any formal seizure monitoring while in the ED. Approximately 5 h post-ingestion, a nasogastric tube was placed and 60 g of activated charcoal was administrated. Physostigmine was not given due to the active seizures as well as widen QRS complex which is a contraindication.
During the management of her prolonged seizure, the patient was attached to a cardiac monitor, which revealed a rate of 170 beats/min with a QRS interval of 127 ms (Fig. 1). The patient initially received sodium bicarbonate [8.4% (1 mEq/mL)] in one dose of 50 mL and another of 150 mL for a total of 200 mL (200 mEq) with narrowing of the QRS complex duration to 120 ms. This was followed by another 200 mL (200 mEq) of sodium bicarbonate with a repeat ECG as seen in Fig. 2. Three 50-mL ampules of sodium bicarbonate were placed in 1 L of 5% dextrose in water (D5W) and an infusion was initiated at a rate of 250 mL/h and was continued for 24 hours with serial ECGs that remained similar to (Fig. 2) with a narrow QRS complex.
Fig. 1.
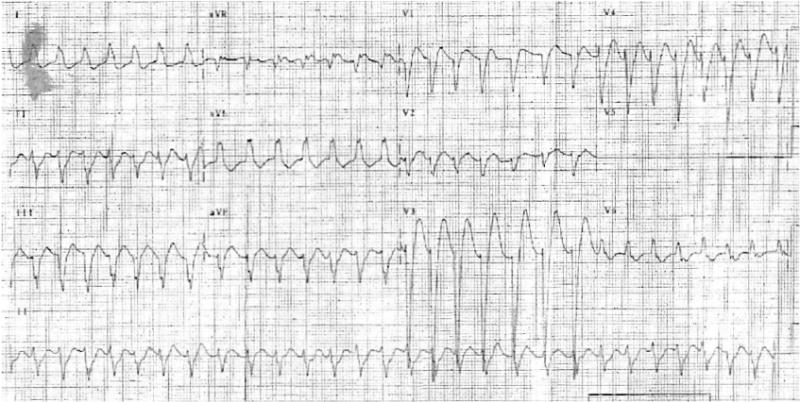
Patient’s ECG on arrival to the ED with a QRS duration of 127 ms.
Fig. 2.
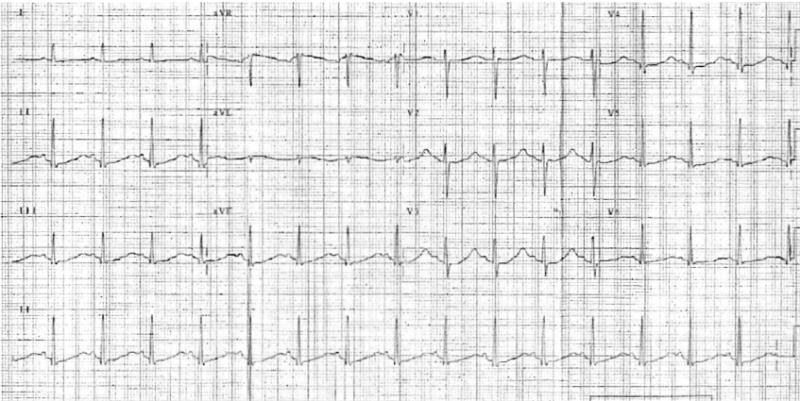
Narrowing of the QRS complex after administration of sodium bicarbonate.
The initial laboratory data obtained upon arrival revealed a hematocrit of 33%; a hemoglobin of 10 g/dL; and a white blood cell count (WBC) of 14 000/mm3. ABG values immediately after intubation were: pH, 7.5; PCO2, 27 mm Hg; PO2, 225 mm Hg. The platelet count and international normalized ratio (INR) were normal.
The electrolyte analysis revealed sodium, 140 mEq/L; potassium, 3.5 mEq/L; chloride, 101 mEq/L; bicarbonate, 10 mEq/L; blood urea nitrogen (BUN), 12 mg/dL; creatinine 0.9 mg/dL, and glucose, 130 mg/dL. The creatine phosphokinase (345 IU/L), lactic dehydrogenase (35 IU/L), and aspartate aminotransferase (35 IU/L) were normal. Salicylates and acetaminophen concentrations were negative. A non-contrast computed tomography of the head was normal. A tricyclic antidepressant screen of the blood was negative. At a later date her diphenhydramine concentration, drawn on ED arrival, returned as 1200 ng/mL (therapeutic: 9–120 ng/mL).
The patient was admitted to the intensive care unit for further management. By the next day, she regained consciousness and remained in normal sinus rhythm with a narrow QRS after the discontinuation of the sodium bicarbonate infusion. She was extubated and stated that she had taken an overdose of diphenhydramine in a gesture of anger due to the dispute with her husband. This was also confirmed by the husband who later arrived with an empty bottle of diphenhydramine although the exact amount ingested was not known. It was later confirmed that the patient has no other history such as ethanol use, prior seizure disorder, and was not noted to use herbals or any other medications.
Discussion
Diphenhydramine is classified as a H1 receptor antagonist chemically described within the ethanolamine group that also includes doxylamine. Diphenhydramine toxicity typically manifests with some degree of both central and peripheral anticholinergic toxicity.5 The effects of diphenhydramine toxicity on the central nervous system often display a wide range of findings such as somnolence, decreased alertness, and diminished reaction times. Other central nervous system effects in overdose can include hallucinations, delirium, and seizures.5
One retrospective study noted that diphenhydramine was a leading cause of drug-induced seizures in the USA.6 An experimental animal study demonstrated that diphenhydramine-induced convulsions are dose-dependant.7 The mechanism of action is thought to be related to the histamine receptor. Agonism at the histamine receptor is thought to mediate an anticonvulsant effect. The epileptogenic activity of first generation antihistamines are antagonized by histidine, but not physostigmine.7 While seizures are commonly reported in patients with diphenhydramine overdoses, most seizures are typically short-lived and often respond to benzodiazepines.8 Status epilepticus, however, is distinctly uncommon from isolated diphenhydramine overdose.
In addition to its anticholinergic effect, overdoses of diphenhydramine can result in cardiotoxicity. Sodium channel blockade is best described as a Vaughan-Williams type IA antidysrhythmic effect, similar to that of tricyclic antidepressants.9 The findings on an ECG that can occur with a diphenhydramine overdose are similar to those with a TCA overdose, including prolongation of the QRS interval (>100 ms), an R wave in AVR, S waves in leads I and AVL indicating right axis change, and sinus tachycardia.10 The mechanism behind these effects is blockade of the fast-closing myocardial sodium channels. This blockade prolongs phase 0 of cellular depolarization. The right side of the cardiac conduction system appears more susceptible to sodium channel blockade and is responsible for the right axis change seen on ECG.10,11 Although not formally studied in experimental models, based on its mechanism of action, cardiotoxicity would most likely respond to hypertonic sodium bicarbonate. In fact, there are reports of successful use of sodium bicarbonate to treat cardiotoxicity from diphenhydramine overdoses.12,13
Like many sodium channel blocking drugs, diphenhydramine also weakly blocks the delayed rectifier potassium channel which delays repolarization. There are also reports of QT prolongation and polymorphic ventricular tachycardia following overdose.14,15 This provides a substrate in which polymorphic ventricular tachycardia can occur. Treatment of torsades often consists of intravenous magnesium as well as over-driving pacing.14,15
Management of patients with diphenhydramine toxicity should focus primarily on supportive care with careful attention to both the cardiovascular and neurologic status. Diphenhydramine cardiotoxicity should be evaluated with an ECG to observe for signs of sodium channel blockade and treated with hypertonic sodium bicarbonate when the QRS is significantly prolonged. While seizures are often short-lived and typically do not require any treatment, benzodiazepines should be first-line treatment for prolonged seizures. Status epilepticus refractory to benzodiazepines and other antiepileptic agents should be managed with an intravenous anesthetic compounds, such as thiopental or propofol. A unique mechanism of action of propofol in the treatment of refractory seizure is the interaction with the N-methyl D-aspartate receptor as well as γ-aminobutyric acid receptors. Their use is clearly advocated for the treatment of generalized convulsive status epilepticus. And finally if this approach is unsuccessful then the use of an inhalation anesthetic may be required.16 It is important to realize that both barbiturates and propofol can cause respiratory depression and endotracheal intubation may be required. If neuromuscular blockade is needed to facilitate intubation, only a short-acting paralytic should be used to allow repeated neurologic examinations as well as to monitor for seizures with an EEG.
One of the limitations of this case report may include that there may have been other co-ingestions involved which may have contributed to the patient’s development of status epilepticus such as isoniazid or extended-release bupropion which are well known to also cause status epilepticus. However, given that combination of wide-complex tachycardia and seizures along with confirmatory concentrations of diphenhydramine and negative tricyclic screen, this is less likely. Another limitation is whether propofol terminated the patient’s seizures as the patient was also given a dose of a neuromuscular junction blocker which would terminate the peripheral manifestation, although would only last 5–8 min.
Conclusion
This case illustrates the complications of a large diphenhydramine overdose. While supportive care remains the cornerstone of treatment, special attention should focus on the potential neurologic and cardiac complications.
References
- 1.Jumbelic MI, Hanzlick R, Cohle S. Alkylamine antihistamine toxicity and review of Pediatric Toxicology Registry of the National Association of Medical Examiners. Report 4: Alkylamines. Am J Forensic Med Pathol. 1997;18:65–69. doi: 10.1097/00000433-199703000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population of the United States: the Slone survey. JAMA. 2002;287:337–344. doi: 10.1001/jama.287.3.337. [DOI] [PubMed] [Google Scholar]
- 3.Pragst F, Herre S, Bakdash A. Poisonings with diphenhydramine – a survey of 68 clinical and 55 death cases. Forensic Sci Int. 2006;161:189–197. doi: 10.1016/j.forsciint.2006.01.019. [DOI] [PubMed] [Google Scholar]
- 4.Krenzelok EP, Anderson GM, Mirick M. Massive diphenhydramine overdose resulting in death. Ann Emerg Med. 1982;11:212–213. doi: 10.1016/s0196-0644(82)80501-5. [DOI] [PubMed] [Google Scholar]
- 5.Koppel C, Ibe K, Tenczer J. Clinical symptomatology of diphenhydramine overdose: an evaluation of 136 cases. J Toxicol Clin Toxicol. 1987;25:53–70. doi: 10.3109/15563658708992613. [DOI] [PubMed] [Google Scholar]
- 6.Alldredge BK, Lowenstein DH, Simon RP. Seizures associated recreational drug abuse. Neurology. 1989;39:1037–1039. doi: 10.1212/wnl.39.8.1037. [DOI] [PubMed] [Google Scholar]
- 7.Kamei C, Ohuchi M, Sugimoto Y, Okuma C. Mechanism responsible for epileptogenic activity by first-generation H1-antagonists in rats. Brain Res. 2000;887:183–186. doi: 10.1016/s0006-8993(00)03041-9. [DOI] [PubMed] [Google Scholar]
- 8.Radovanovic D, Meier PJ, Guirguis M, Lorent JP, Kupferschmidt H. Dose-dependent toxicity of diphenhydramine overdose. Hum Exp Toxicol. 2000;19:489–495. doi: 10.1191/096032700671040438. [DOI] [PubMed] [Google Scholar]
- 9.Kuo CC, Huang RC, Lou BS. Inhibition of Na current by diphenhydramine and other diphenyl compounds: molecular determinants of selective binding to the inactivated channels. Mol Pharmacol. 2000;57:135–143. [PubMed] [Google Scholar]
- 10.Nuemann JT, Bessen HA, Rothstein RJ, Laks MM. Electrocardiographic criteria for tricyclic antidepressant cardiotoxicity. Am J Cardiol. 1986;57:1154–1159. doi: 10.1016/0002-9149(86)90691-0. [DOI] [PubMed] [Google Scholar]
- 11.Zareba W, Moss AJ, Rosero SZ, Hajj-Ali R, Konecki J, Andrews M. Electrocardiographic findings in patients with diphenhydramine overdose. Am J Cardiol. 1977;80:1168–1173. doi: 10.1016/s0002-9149(97)00634-6. [DOI] [PubMed] [Google Scholar]
- 12.Sharma AN, Hexdall AH, Chang EK, Nelson LS, Hoffman RS. Diphenhydramine-induced wide complex dysrhythmia responds to treatment with sodium bicarbonate. Am J Emerg Med. 2003;21:212–215. doi: 10.1016/s0735-6757(02)42248-6. [DOI] [PubMed] [Google Scholar]
- 13.Clark RF, Vance MV. Massive diphenhydramine poisoning resulting in a wide-complex tachycardia: successful treatment with sodium bicarbonate. Ann Emerg Med. 1992;21:318–321. doi: 10.1016/s0196-0644(05)80897-2. [DOI] [PubMed] [Google Scholar]
- 14.Thakur AC, Aslam AK, Aslam AF, Vasavada BC, Sacchi TJ, Khan IA. QT interval prolongation in diphenhydramine toxicity. Int J Cardiol. 2005;98:341–343. doi: 10.1016/j.ijcard.2003.10.051. [DOI] [PubMed] [Google Scholar]
- 15.Joshi AK, Sljpic T, Borghei H, Kowey PR. Case of polymorphic ventricular tachycardia in diphenhydramine poisoning. J Cardiovasc Electrophysiol. 2004;15:591–593. doi: 10.1046/j.1540-8167.2004.03173.x. [DOI] [PubMed] [Google Scholar]
- 16.Rossetti AO, Santoli F. Drug treatment of refractory status epilepticus. Rev Neurol (Paris) 2009;165:373–379. doi: 10.1016/j.neurol.2008.12.003. [DOI] [PubMed] [Google Scholar]


