Abstract
Objective
The authors quantitatively examined differences in psychiatric residents’ and attending physicians’ communication profiles and voice tones.
Methods
Audiotaped recordings of 49 resident–patient and 35 attending–patient medication-management appointments at four ambulatory sites were analyzed with the Roter Interaction Analysis System (RIAS). Nonparametric tests were used to compare differences in proportions of speech devoted to relationship-building, activating, and partnering in decision-making processes, and data-gathering/counseling/patient education. Differences in affect expressed by psychiatrists’ voice tones were also examined.
Results
Residents’ visits were twice as long as Attendings’ visits (28.2 versus 14.1 minutes), and residents devoted a significantly greater proportion of their talk to relationship-building (23% versus 20%) and activating/partnering (36% versus 28%) aspects of communication, whereas Attendings devoted a greater proportion to biomedically-related data-gathering/counseling/ patient education (31% versus 20%). Analysis of voice tones revealed that residents were perceived as sounding significantly friendlier and more sympathetic, versus Attendings, who were rated as sounding more dominant and rushed.
Conclusion
These findings show distinct communication profiles and voice-tone differences. Future psychiatric communication research should address the influence of appointment length, psychiatrist/patient characteristics, and other potential confounders on psychiatrist–patient communication.
The development of communication skills is central to the training and professional development of psychiatric residents. In order to inform psychiatric education and the development of training models, it is important to thoroughly examine the communication characteristics of Attending and Resident physicians. Although many studies have examined isolated aspects of psychosocial attitudes and interpersonal styles, there have been no studies to our knowledge that have compared psychiatry residents to attendings via systematic analysis of both the content and context of communication. Such information has the potential to inform targets for intervention strategies and identify trends in the development of professional styles.
Communication skills are at the fore of psychiatric training. The Accreditation Council for Graduate Medical Education (ACGME) highlights interpersonal communication skills as one of six core areas of clinical competence (1). The American Board of Psychiatry and Neurology (ABPN) defines interpersonal and communications skills to be of the “highest importance … worthy of constant assessment from residency training and all through practice” (2). These competencies highlight communication skills with both patients and the healthcare team. Since much of clinical training consists of interpersonal and mentor relationships, it is easy to picture how faculty–mentor and resident–peer communication practices can have a great impact on the psychiatry trainee (3–5).
This study quantitatively analyzed audiotaped medication-management appointments. We compared and contrasted the communication skills used by postgraduate year (PGY) 3 and 4 psychiatry residents and attendings in order to gain a better understanding of psychiatrist communication profiles.
Overview of Communication: The Impact of Medical Training
There is a large body of literature on physician–patient communication, but relatively few systematic studies in psychiatric communication (6). Positive physician attitudes and communication skills identified by previous work include better interpretation of nonverbal cues (7), stronger therapeutic alliance (8), emphasis on patient beliefs and expectations (9), and query of psychosocial issues (10). These positive skills have been shown to relate to higher patient and physician satisfaction, improved medication and appointment compliance, and improved outcomes, such as shorter recovery time and decreased use of pain medications (11). Surprisingly, studies looking at the communication skills of medical students have largely shown negative effects of increased years of training. As compared with preclinical medical students, students closer to graduation have been shown to have more negative attitudes toward the medical profession (12), poorer interviewing skills (13, 14), greater physician-centered/ paternalistic attitudes (15, 16), and decreased empathy (17). Studies have shown similar findings in residents, such as high paternalism (16), frequent interruptions of patient speech (18), failure to recognize emotional distress (10), and inaccurate interpretation of patients’ desired level of decision-making control (19). Studies comparing residents and attendings have been mixed, with attendings exhibiting greater paternalistic attitudes, eliciting less patient input, and covering fewer patient-education topics than residents (16, 20), but also demonstrating less cynicism, more idealism, and higher aptitude in information-gathering and patient-education (3, 21–23).
The above literature paints a mixed picture of the impact of medical training on communication, with higher medical training relating to improvements in certain domains, particularly data-gathering and patient-education skills, but declines in others, specifically, rapport-building skills and shared medical decision-making. Shedding light on these opposing trends, Roter and Larson make a distinction between innate aspects of communication (i.e., relationship-building, patient-activation, and partnership) versus those communication practices acquired through medical education (i.e., data-gathering, patient-education, and counseling) (24). As one progresses through training, therefore, one would expect to show improvement in acquired skills, potentially at the sacrifice of more innate, empathetic practices. Within the psychiatric interview, this might be reflected by an increasing focus on data-gathering, patient-education, and counseling, and a decreasing emphasis on relationship-building and partnership.
We recently completed a cross-sectional study of psychiatrist communication with depression patients in medication-management appointments. Using data from the parent study, we quantitatively analyzed audiotaped recordings of medication-management appointments to characterize psychiatry attending and resident communication profiles. We hypothesized the following:
Residents spend a significantly greater proportion of their talk on relationship-building, activating, and partnering in treatment decisions with patients in medication-management appointments than do attendings.
Attendings spend a significantly greater proportion of their talk on data-gathering, counseling, and patient-education with patients in medication-management appointments than do residents.
Residents’ vocal tones are perceived more positively (i.e., as more interested, friendly, responsive, sympathetic, respectful, and interactive) than attendings’.
Method
Data for this study were acquired from an NIMH funded study (K23 MH071520) that quantitatively analyzed audiotaped psychiatric interviews to examine the impact of psychiatrist communication on patient satisfaction and appointment adherence. This pilot study reports the findings specific to Resident and Attending communication practices.
Our sites were three community psychiatric clinics and one academic research clinic, located in western Pennsylvania. This study was approved by the University of Pittsburgh Institutional Review Board. Data were collected from 2005 to 2008.
Physician participants were recruited from medical staff meetings or through individual meetings with the parent study’s primary investigator (MC). Psychiatrists also received informational brochures about the study. A total of 52 psychiatrists were approached, with 41 (78.8%) consenting to participate, and a total of 24 (46.2%) recorded. Of the 17 consenting psychiatrists not included, 5 provided inaudible recordings that could not be used for analysis, and the remainder encountered difficulties with patient recruitment; 10 of the 11 psychiatrists who refused to participate cited no reasons for refusal, and 1 reported anxiety with being recorded. Patients were assigned to psychiatrists as per usual-care protocols at the four sites. Patient participants were recruited on the day of their second, third, fourth, or fifth clinic appointment. The first appointment was not chosen, so as to allow the patient time to assess satisfaction with services before their study participation. Patients and psychiatrists were given a complete description of the study, including the study’s purpose, after which written informed consent was obtained. Psychiatrists received no compensation for participation in this study. Patients were compensated $10 for participation.
The study sample included a total of 84 patients (49 Resident and 35 Attending patients), 16 psychiatry Residents (PGY-3 and PGY-4), and 8 psychiatry Attendings (3 faculty, 5 staff). The patient sample comprised 69 women and 15 men, with 58.3% of patients being African American. Attendings’ patients’ average age was 43.5 years, versus 46.5 years for Residents’ patients. Psychiatrist demographic characteristics are summarized in Table 1. Our Residents’ sample had a higher proportion of women, greater racial/ethnic diversity, and fewer international medical graduates, as compared with our Attendings’ sample, closely mirroring demographic trends in recent national census data of psychiatry residents (25).
TABLE 1.
Physician Demographic Characteristics
| Attendings | n | % | Residents | n | % |
|---|---|---|---|---|---|
| Gender | Gender | ||||
| Male | 6 | 75.0 | Male | 9 | 56.2 |
| Female | 2 | 25.0 | Female | 7 | 43.7 |
| Race | Race | ||||
| White | 7 | 87.5 | White | 10 | 62.5 |
| Black | 0 | Black | 2 | 12.5 | |
| Asian | 1 | 12.5 | Asian | 4 | 25.0 |
| IMG Status | IMG Status | ||||
| IMG | 2 | 25.0 | IMG | 1 | 6.7 |
| Non-IMG | 6 | 75.0 | Non-IMG | 14 | 93.3 |
| Mean | Range | Mean | Range | ||
| Age, years | 46.5 | 35–60 | Age, years | 31.4 | 27–37 |
| Appointment length, min. | 14.1 | 4.2–29.8 | Appointment length, min. | 28.2 | 9.9–60.3 |
| Recordings per provider | 4.4 | 2–11 | Recordings per provider | 3.1 | 1–7 |
| Years post-residency | 11.8 | 1.5–28.0 |
IMG: international medical-school graduate.
The Roter Interaction Analysis System (RIAS)
This study used the RIAS for quantitative analysis of audiotaped recordings. The RIAS is a well-validated communication measurement instrument used extensively in other medical disciplines, including internal medicine, pediatrics, surgery, nursing, and dentistry (24). The RIAS uses professional coders to categorize physician or patient statements, the smallest unit of speech representing a complete thought, into 1 or more of the 41 specific RIAS communication categories. This process allows for the quantitative analysis of speech and the systematic description of communication profiles.
We used three composite categories of the RIAS for this study: 1) biomedical and psychosocial task-focused communication; 2) relationship-building; and 3) activation and partnership (25). Biomedical and psychosocial task-focused communication includes data-gathering, patient-education, and counseling. Relationship-building talk is responsive to patient needs and concerns and includes the affective aspects of communication, such as empathy, and shows of encouragement or criticism, to name a few. Activation and partnership talk encourages patient participation, patient decision-making, and helps the patient navigate the medical interview (e.g., orienting the patient to shifts in conversations, requests for more information, and queries about patient opinion and understanding). Pearson correlation coefficients for interrater agreement on high frequency (>2 statements per recording) categories of psychiatrist talk ranged from 0.847 to 0.967. Lower reliability was found on the low-frequency (≤2 statements per recording) categories of negativity (0.359) and orientation (0.369). To compare Attendings and Residents within each RIAS communication category, we analyzed proportions of provider statements. We did this by dividing provider statements per RIAS category by total provider statements. This strategy for comparing provider groups is commonly used in the communication literature (26–28). Although this strategy does not completely address differences in appointment length or pauses, it does exclude patient talk within the appointment and focuses analyses on provider communication.
By analyzing directly from audiotapes rather than transcripts, the RIAS is able to capture the tonal qualities of speech via Global Affect Ratings. These ratings are not based on specific statements or content, but aim to describe the overall emotional impression of provider talk. Global Affect Ratings are divided into Positive (e.g., warmth, empathy) and Negative (e.g., dominance, nervousness) affect ratings. Each item is 6-point Likert-scaled (No Affect to High Affect), with ratings of 3 or 4 considered average. To determine ratings, trained RIAS coders assign lower or higher numbers to reflect psychiatrists’ levels of affect specific to each category. The interrater agreement of Global Affect Ratings ranged from 80% to 100%. RIAS coders were blinded to physician status and to the purpose of the parent study.
Descriptive statistics, including measures of central tendency (e.g., means, medians) and dispersion (e.g., standard deviations, ranges), were computed for continuous data. Frequency distributions were estimated for categorical data. To identify differences between Residents and Attendings, we did chi-square tests with ordinal data and Wilcoxon rank-sum tests with continuous data. We used the nonparametric Wilcoxon rank-sum test because normal distribution could not be assumed because of the small sample size.
Results
Psychiatrist demographics, as noted, are summarized in Table 1. Psychiatry residents had significantly longer appointment times than those of attendings (mean 28.2 versus 14.1 minutes; z = −5.50; p<0.001). Differences were also seen between Resident and Attending patient groups, with Residents treating significantly more African American/non-white patients (40 versus 25; χ2=23.86; p<0.001) and patients with significantly lower educational background (χ2=4.75; p=0.029). Attendings saw significantly more patients with personality disorders (χ2=6.10; p=0.019). There were no significant differences in other diagnostic categories (i.e., major depressive disorder, other depressive disorders, PTSD, anxiety disorders, and psychotic disorders).
Table 2 summarizes the communication categories used by Residents and Attendings. To test our first hypothesis, that residents’ talk is more affective and collaborative than that of Attendings, we analyzed the RIAS composites of Relationship-Building and Activation/Partnership. Our findings support this hypothesis, showing that Activation/ Partnership talk comprised 36% of the total number of Residents’ statements, as compared with 28% of Attendings’ (p=0.002). Examining the subcategories of Activation/Partnership talk, Residents engaged in significantly more facilitation talk (31% versus 24%; p=0.007). Residents’ talk was also characterized by a significantly greater proportion of positive affective talk (16% versus 13%; p=0.007), emotional rapport (7% versus 5%; p=0.017), and total Relationship-Building talk (23% versus 20%; p=0.006). Importantly, the majority of Resident communication in medication-management appointments comprised Relationship-Building and Activation/Partnership talk (59%), versus Attendings’ (48%; p<0.001; Figure 1).
TABLE 2.
Summary of Communication Categories Used in Medication-Management Appointments
| Communication Category | Residents
|
Attendings
|
|||||
|---|---|---|---|---|---|---|---|
| Median | Range | % | Median | Range | % | z-score | |
| Biomedical Talk | 62 | 17–165 | 20 | 41 | 13–90 | 32 | 3.51** |
| Data-gathering | 18 | 2–50 | 6 | 12. | 2–45 | 10 | 2.86** |
| Education and counseling | 41 | 9–115 | 14 | 29. | 7–60 | 22 | 2.94** |
| Psychosocial Talk | 61 | 21–158 | 20 | 26 | 5–97 | 20 | 0.04 |
| Data-gathering | 31 | 7–91 | 11 | 15. | 2–46 | 10 | −0.57 |
| Education and counseling | 24 | 1–126 | 9 | 11 | 0–63 | 10 | 0.35 |
| Relationship-Building | 69 | 33–182 | 23 | 28 | 3–70 | 20 | −2.72** |
| Positive rapport-building | 44 | 21–119 | 16 | 18 | 2–62 | 13 | −2.67** |
| Negative rapport-building | 0 | 0–8 | 0 | 0–1 | −2.08* | ||
| Emotional rapport-building | 21 | 4–75 | 7 | 9 | 0–27 | 5 | −2.38* |
| Social rapport-building | 0 | 0–9 | 0 | 0–14 | 1 | 0.49 | |
| Activation and Partnership | 94 | 35–434 | 36 | 38 | 9–114 | 28 | −3.07** |
| Facilitation | 85 | 27–399 | 31 | 31 | 6–110 | 24 | −2.72** |
| Procedural | 11 | 1–69 | 5 | 4 | 0–20 | 4 | −1.49 |
Proportion calculation: number of provider statements in RIAS category/total number of provider statements. Proportions were calculated for each RIAS category in each patient–psychiatrist recording. Percentages shown represent the average of these proportions.
z-score by Wilcoxon rank-sum test; describes differences in talk percentages according to resident vs. attending status.
p<0.05.
p <0.01.
FIGURE 1. Summary of Composite Communication Categories Used in Medication-Management Appointments.
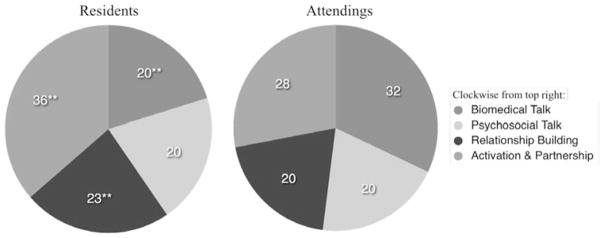
Proportion: number of provider statements in Roter Interaction Analysis System/total number of provider statements.
**p <0.01.
Testing our second hypothesis, that Attendings spend significantly more time on the task-related elements of communication than did Residents, we analyzed the categories of Biomedical and Psychosocial talk. Our hypothesis was partially supported. Attendings engaged in a significantly greater proportion of total Biomedical task-focused talk (32% versus 20%; p<0.001), and in the Biomedical subcategories of data-gathering (10% versus 6%; p=0.004) and Education/Counseling (22% versus 14%; p=0.003). Contrary to our expectations, there were no significant differences between Residents’ and Attendings’ total Psychosocial talk or the Psychosocial subcategories. Consistent with our hypothesis, the majority of Attendings’ talk comprised task-focused communication (data-gathering, patient-education, and counseling) in the Biomedical and Psychosocial categories (52%), as compared with Residents’ (41%; p<0.001; Figure 1).
Chi-square analysis supported our hypotheses with respect to Residents’ and Attendings’ RIAS Global Affect Ratings (results not shown). Residents had more positive Global Affect Ratings than Attendings, with Residents conveying more friendliness/warmth (χ2=8.83; p=0.032) and sympathy/empathy (χ2=17.74; p=0.005). Attendings, on the other hand, significantly conveyed more hurried and rushed (χ2=15.13; p=0.004) and dominant and assertive affects (χ2=8.81; p=0.032) than residents.
Discussion
With the growing influence of managed care dramatically changing the orientation of the psychiatric appointment, psychiatrists’ dominant role is medication-management (6, 29). Our study sought to explore how Resident and Attending physicians execute the balancing act between data-gathering and patient-oriented communication within medication-management appointments.
To our knowledge, this is the first study to quantitatively evaluate Resident and Attending psychiatrist communication profiles in medication-management appointments. We found distinct differences. Residents spend significantly more time with their patients—twice as much—and devote a significantly greater proportion of talk to Relationship-Building and Activation/Partnership than Attendings (59% versus 48%). Attendings engaged in significantly greater task-based communication (52% versus 41%), particularly Biomedical talk (32% versus 20%). Roter and Hall describe patient-centered communication as talk that works to build a therapeutic relationship, facilitate patient input, and activate the patient to shared decision-making (11). Our findings suggest that psychiatry Resident communication is predominantly patient-centered (59%), whereas the slight majority of Attendings’ communication is task-focused (52%; Figure 1). These findings mirror those of studies on primary-care communication (30, 31). Roter and Larson showed that the greatest proportion of primary-care Attendings’ communication, when consulting during a resident visit, was spent on task-focused, Biomedical talk, as compared with the Residents’ communication, which was characterized as reflecting more social rapport, reassurance, and empathy (30).
Previous work has shown that physicians with predominantly biomedically task-focused communication styles can potentially be perceived by patients as verbally dominant and preoccupied with the administrative tasks of the medical visit (11). Work by Hall (32) has shown that, whereas Biomedical talk (particularly certain types of patient-education) is related to greater patient adherence with treatment recommendations, it is also associated with perceptions of physician paternalism and lower patient and physician satisfaction. Conversely, patient-centered communication has been associated with greater patient and physician satisfaction and even certain positive health-related outcomes (32). Consistent with the above findings, our sample of Attendings with a biomedically task-focused communication profile conveyed significantly more dominant affect, whereas Residents with a more patient-centered communication style conveyed significantly friendlier and more empathetic affect.
Residents’ communication profiles may reflect the recent evolution toward teaching patient-centered clinical competencies and communication skills, influenced by a movement toward outcomes-based educational standards (1), key consensus statements on doctor–patient talk (33, 34), and critical reviews on teaching medical communication (35). Alternatively, medical expertise, differing roles, and levels of perceived medical liability by attendings and resident physicians may play a role. Residents may use less task-related communication because of relative inexperience in engaging patients in certain biomedically-related topics. In addition to their roles as clinicians, residents are trainees and may incorporate communication strategies aimed at enhancing their learning. With relatively fewer responsibilities, residents may perceive more flexibility in their medication-management appointments that cultivates longer appointment times and a patient-centered style. Attendings, on the other hand, may perceive greater medical liability than residents, and may attempt to control this risk by devoting a greater proportion of their talk to task-related communication at the sacrifice of patient-centered elements. Attendings may be subject to different time pressures and efficiency expectations, which may explain why attendings were perceived as sounding more hurried/rushed and dominant/assertive.
Future work should seek to clarify the evolution of professional development through longitudinal studies tracking communication skills from early training to post-residency practice. These studies, augmented by surveys of physician attitudes and qualitative interviews, could help identify critical times for communication interventions. Future studies should identify the salient communication practices, with respect to patient and physician outcomes, that must be targeted by these interventions. Communication studies can be time-consuming and challenging with respect to recruitment and the numerous patient (e.g., attitudes toward treatment, stigma, explanatory models of mental illness, race/ethnicity, temperament), physician (e.g., attitudes toward medication-management appointments, type of psychotherapy orientation, age, racial/ethnic biases), organizational (e.g., financing, appointment scheduling, productivity standards), and other factors that potentially affect the psychiatrist–patient interaction. Future studies should consider recruitment and data-gathering methods that allow for more uniform conditions and study populations to decrease the potential for such confounders, while at the same time maintaining generalizability to the challenges of real-world practice conditions. Such work has the potential to affect psychiatrist–patient, mentor, and peer relationships that comprise the interpersonal education of future psychiatrists.
This pilot study has a few limitations. This is a small-sample study that performs secondary analysis of data from a parent study, which was designed to examine related but distinct questions concerning psychiatrist–patient communication. As a result, the parent study was not designed to recruit a uniform number of residents and attendings from each of our four sites, nor designed to standardize appointment duration or the number of recordings by each psychiatrist-participant. Of note, we found no significant correlation between number of recordings per attending and the number of years post-residency. Differences in appointment time may contribute substantially to the tone and content of a medical interview. Although our analysis used proportions of provider talk to attempt to adjust for appointment length, appointment duration may influence psychiatrist communication choices and vocal tones in important ways. The impact of demographic differences, particularly gender, between residents and attendings, was not examined in this study, and so potentially serve as confounders. The intricacies of communication analysis are also complicated by the influence that organizational factors, such as patient volume and time constraints, and patient/ psychiatrist characteristics, such as race and sociocultural discordance, have on doctor–patient talk (11). Also, care should be taken in viewing our study’s results because, although statistically significant, observed communication differences were small. Despite these limitations, our pilot study provides a foundation for analyzing, understanding, and conceptualizing differences in psychiatrist communication profiles in medication-management appointments with the potential to inform future research and interventions.
Conclusion
To our knowledge, this is the first study to systematically and quantitatively characterize the distinct differences in psychiatry residents’ and attendings’ communication profiles. The challenge to residency training programs is to use quantitative, systematic methods to assess the professional development of psychiatrist communication and the factors that influence this development. The challenges to future researchers are to determine the impact of these distinct communication differences on patient as well as psychiatrist outcomes, such as medication and appointment adherence, appointment and job satisfaction, and psychiatrist skills and productivity, with the end-goal being communication interventions that improve service delivery and the physician’s learning experience.
Acknowledgments
The authors thank the patients and physicians who graciously shared their experiences in our study.
Funding for this study was provided by the NIMH Research Fellowship for Medical Students (MH05431813, K23 MH071520), the Advanced Center for Interventions and Services Research on Late-Life Mood Disorders (P30MH71944), and the Commonwealth of Pennsylvania Department of Health.
Footnotes
The findings reported in this manuscript have been presented as a poster presentation at the Western Psychiatric Institute and Clinic Research Day in Pittsburgh, PA on June 4, 2009.
References
- 1.Beresin E, Mellman L. Competencies in psychiatry: the new, outcomes-based approach to medical training and education. Harvard Rev Psychiatry. 2002;10:185–191. doi: 10.1080/10673220216219. [DOI] [PubMed] [Google Scholar]
- 2.Ebert MH. A Report of the American Board of Psychiatry & Neurology, Inc. Washington, DC: American Psychiatric Publishing; 2003. Interpersonal and communications skills core competencies, in Core Competencies for Psychiatric Practice: What Clinicians Need to Know; p. 87. [Google Scholar]
- 3.Light D. The sociological calendar: an analytic tool for field-work applied to medical and psychiatric training. Am J Sociol. 1975;80:1145–1164. doi: 10.1086/225948. [DOI] [PubMed] [Google Scholar]
- 4.Hafferty FW. Beyond curriculum reform: confronting medicine’s hidden curriculum. Acad Med. 1998;73:403–407. doi: 10.1097/00001888-199804000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Hook KM, Pfeiffer CA. Impact of a new curriculum on medical students’ interpersonal and interviewing skills. Med Educ. 2007;41:154–159. doi: 10.1111/j.1365-2929.2006.02680.x. [DOI] [PubMed] [Google Scholar]
- 6.Cruz M, Pincus HA. Research on the influence that communication in psychiatric encounter has on treatment. Psychiatr Serv. 2002;53:1253–1265. doi: 10.1176/appi.ps.53.10.1253. [DOI] [PubMed] [Google Scholar]
- 7.DiMatteo MR, Taranta A, Friedman HS, et al. Predicting patient satisfaction from physicians’ nonverbal communication skills. Med Care. 1980;18:376–387. doi: 10.1097/00005650-198004000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Blatt SJ, Sanislow CA, Zuroff DC. Characteristics of effective therapists: further analyses of data from the National Institute of Mental Health Treatment of Depression Collaborative Research Program. J Consult Clin Psychol. 1996;64:1276–1284. doi: 10.1037//0022-006x.64.6.1276. [DOI] [PubMed] [Google Scholar]
- 9.Korsch BM, Gozzi EK, Francis V. Gaps in doctor–patient communication, I: doctor–patient interaction and patient satisfaction. Pediatrics. 1968;42:855–871. [PubMed] [Google Scholar]
- 10.Wissow LS, Roter D, Larson SM, et al. Mechanisms behind the failure of residents’ longitudinal primary care to promote disclosure and discussion of psychosocial issues. Arch Pediatr Adolesc Med. 2002;156:685–692. doi: 10.1001/archpedi.156.7.685. [DOI] [PubMed] [Google Scholar]
- 11.Roter D, Hall JA. Improving Communication in Medical Visits. 2. Westport, CT: Praeger; 2006. Doctors Talking with Patients/Patients Talking with Doctors. [Google Scholar]
- 12.Woloschuk W, Harasym PH, Temple W. Attitude change during medical school: a cohort study. Med Educ. 2004;38:522–534. doi: 10.1046/j.1365-2929.2004.01820.x. [DOI] [PubMed] [Google Scholar]
- 13.Helfer RE. An objective comparison of the pediatric interviewing skills of freshman and senior medical students. Pediatrics. 1970;45:623–627. [PubMed] [Google Scholar]
- 14.Pfeiffer C, Madray H, Ardolino A, et al. The rise and fall of students’ skill in obtaining a medical history. Med Educ. 1998;32:283–288. doi: 10.1046/j.1365-2923.1998.00222.x. [DOI] [PubMed] [Google Scholar]
- 15.Haidet P, Dains JE, Paterniti DA, et al. Medical student attitudes toward the doctor–patient relationship. Med Educ. 2002;46:568–574. doi: 10.1046/j.1365-2923.2002.01233.x. [DOI] [PubMed] [Google Scholar]
- 16.Beisecker AE, Murden RA, Moore WP, et al. Attitudes of medical students and primary-care physicians regarding input of older and younger patients in medical decisions. Med Care. 1996;34:126–137. doi: 10.1097/00005650-199602000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Hojat M, Vengare MJ, Maxwell K, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84:1182–1191. doi: 10.1097/ACM.0b013e3181b17e55. [DOI] [PubMed] [Google Scholar]
- 18.Rhoades DR, McFarland KF, Finch WH, et al. Speaking and interruptions during primary-care office visits. Fam Med. 2001;33:528–532. [PubMed] [Google Scholar]
- 19.McKeown RE, Reininger BM, Martin M, et al. Shared decision making: views of first-year residents and clinic patients. Acad Med. 2002;77:438–445. doi: 10.1097/00001888-200205000-00020. [DOI] [PubMed] [Google Scholar]
- 20.Kerns JW, Krist AH, Woolf SH, et al. Patient perceptions of how physicians communicate during prostate cancer screening discussions: a comparison of residents and faculty. Family Med. 2008;40:181–187. [PubMed] [Google Scholar]
- 21.Sloan DA, Donnelly MB, Johnson SB, et al. Assessing surgical residents’ and medical students’ interpersonal skills. J Surg Res. 1994;57:613–618. doi: 10.1006/jsre.1994.1190. [DOI] [PubMed] [Google Scholar]
- 22.Langewitz WA, Eich P, Kiss A, et al. Improving communication skills: a randomized, controlled, behaviorally-oriented intervention study for residents in internal medicine. Psychosom Med. 1998;60:268–276. doi: 10.1097/00006842-199805000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Testerman JK, Morton KR, Loo LK, et al. The natural history of cynicism in physicians. Acad Med. 1996;71:S43–S45. doi: 10.1097/00001888-199610000-00040. [DOI] [PubMed] [Google Scholar]
- 24.Roter D, Larson S. The Roter Interaction Analysis System (RIAS): utility and flexibility for analysis of medical interactions. Patient Educ Couns. 2002;46:243–251. doi: 10.1016/s0738-3991(02)00012-5. [DOI] [PubMed] [Google Scholar]
- 25.Hales DJ, Delanoche N. Resident census: characteristics and distribution of psychiatry residents in the US. Washington, D.C: American Psychiatric Association: Office of Education; 2008–2009. [Google Scholar]
- 26.Roter DL, Hall JA, Katz NR. Patient–physician communication: a descriptive summary of the literature. Patient Educ Couns. 1988;12:99–119. [Google Scholar]
- 27.Isikawa H, Roter DL, Yamazaki Y, et al. Physician–elderly patient-companion communication and roles of companions in Japanese geriatric encounters. Soc Science Med. 2005;60:2307–2320. doi: 10.1016/j.socscimed.2004.08.071. [DOI] [PubMed] [Google Scholar]
- 28.Bensing JM, Roter DL, Hulsman RL. Communication patterns of primary-care physicians in the United States and The Netherlands. J Gen Intern Med. 2003;18:335–342. doi: 10.1046/j.1525-1497.2003.10735.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mojtabai R, Olfson M. National trends in psychotherapy by office-based psychiatrists. Arch Gen Psychiatry. 2008;65:962–970. doi: 10.1001/archpsyc.65.8.962. [DOI] [PubMed] [Google Scholar]
- 30.Roter DL, Larson S. The relationship between residents’ and attending physicians’ communication during primary-care visits: an illustrative use of the Roter Interaction Analysis System. Health Commun. 2001;13:33–48. doi: 10.1207/S15327027HC1301_04. [DOI] [PubMed] [Google Scholar]
- 31.Roter DL, Stewart M, Putnam SM, et al. Communication patterns of primary-care physicians. JAMA. 1997;277:350–356. [PubMed] [Google Scholar]
- 32.Hall J, Roter D, Katz N. Meta-analysis of correlates of provider behavior in medical encounters. Med Care. 1988;26:657–675. doi: 10.1097/00005650-198807000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Makoul G. Essential elements of communication in medical encounters: the Kalamazoo consensus statement. Acad Med. 2001;76:390–393. doi: 10.1097/00001888-200104000-00021. [DOI] [PubMed] [Google Scholar]
- 34.Simpson M, Buckman R, Stewart M, et al. Doctor–patient communication: The Toronto Consensus Statement. BMJ. 1991;303:1385–1387. doi: 10.1136/bmj.303.6814.1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sanson-Fisher RW, Fairbairn S, Maguire P. Teaching skills in communication to medical students: a critical review of the methodology. Med Educ. 1981;15:33–37. doi: 10.1111/j.1365-2923.1981.tb02312.x. [DOI] [PubMed] [Google Scholar]


