Abstract
Novel strategies are required to control mosquitoes and the pathogens they transmit. One attractive approach involves maternally inherited endosymbiotic Wolbachia bacteria. After artificial infection with Wolbachia, many mosquitoes become refractory to infection and transmission of diverse pathogens. We evaluated the effects of Wolbachia (wAlbB strain) on infection, dissemination and transmission of West Nile virus (WNV) in the naturally uninfected mosquito Culex tarsalis, which is an important WNV vector in North America. After inoculation into adult female mosquitoes, Wolbachia reached high titers and disseminated widely to numerous tissues including the head, thoracic flight muscles, fat body and ovarian follicles. Contrary to other systems, Wolbachia did not inhibit WNV in this mosquito. Rather, WNV infection rate was significantly higher in Wolbachia-infected mosquitoes compared to controls. Quantitative PCR of selected innate immune genes indicated that REL1 (the activator of the antiviral Toll immune pathway) was down regulated in Wolbachia-infected relative to control mosquitoes. This is the first observation of Wolbachia-induced enhancement of a human pathogen in mosquitoes, suggesting that caution should be applied before releasing Wolbachia-infected insects as part of a vector-borne disease control program.
Author Summary
Current methods to control mosquitoes and the pathogens they transmit are ineffective, partly due to insecticide and drug resistance. One novel control method involves exploiting naturally occurring Wolbachia bacteria in insects. Wolbachia are bacterial symbionts that are attractive candidates for mosquito-borne disease control due to their ability to inhibit pathogens infecting humans. Additionally, Wolbachia affects insect reproduction to facilitate its own transmission to offspring, which has been exploited to establish the bacterium in naturally uninfected field populations. Most Wolbachia pathogen control research has focused on Aedes and Anopheles mosquitoes, but Culex mosquitoes also transmit pathogens that affect human health. We evaluated impacts of Wolbachia infection on West Nile virus (WNV) in the naturally uninfected mosquito Culex tarsalis. Wolbachia was able to efficiently establish infection in Cx. tarsalis but contrary to other studies, Wolbachia enhanced rather than inhibited WNV infection. Enhancement occurred in conjunction with suppression of mosquito anti-viral immune gene expression. This study indicates that Wolbachia control strategies to disrupt WNV via pathogen interference may not be feasible in Cx. tarsalis, and that caution should be used when releasing Wolbachia infected mosquitoes to control human vector-borne diseases.
Introduction
Efforts to control vector-borne pathogens have been hindered by evolution of insecticide resistance and failing drug therapies. Evidence suggests bed nets and indoor residual spraying with insecticides are losing efficacy in developing countries [1], [2]. To improve the sustainability and efficacy of control efforts, alternative vector control strategies are being considered, including methods that suppress the pathogen instead of the vector [3], [4]. Wolbachia are a genus of maternally-inherited bacterial endosymbionts that naturally occur in numerous arthropod taxa [5]. Wolbachia can inhibit viruses and parasites in fruit flies and mosquitoes [6]–[11] and influence reproduction of their host to facilitate spread through populations [12]. Mosquito-borne disease management programs that use Wolbachia are currently under investigation [13]. In field trials in Australia, Wolbachia reached fixation in naturally uninfected populations of Aedes aegypti [11] and the DENV blocking phenotype has been maintained [14], but the impacts of Wolbachia on reducing the incidence of disease are yet to be investigated.
Pathogen interference conferred by Wolbachia depends on various factors, including Wolbachia strain, pathogen type, infection type (natural versus artificial) and host and is not a guarantee [7], [15], [16]. For example, Wolbachia increases Plasmodium berghei, P. yoelii and P. gallinaceum oocyst loads in Anopheles gambiae, An. stephensi, and Aedes fluviatilis, respectively [17]–[19], and P. relictum sporozoite prevalence in Culex pipiens [20]. These Wolbachia-mediated pathogen enhancement studies suggest that careful examination of Wolbachia is required, since the bacterium influences insect-pathogen interactions in ways that may negatively impact pathogen control efforts.
Few studies have investigated the effect of Wolbachia on pathogen transmission by Culex mosquitoes, despite the fact they transmit viruses impacting human health [9], [21], [22]. Culex tarsalis is a mosquito species associated with agriculture and urban areas in the western United States [23] and is highly competent for West Nile virus (WNV), St. Louis encephalitis virus (SLEV) and western equine encephalitis virus (WEEV) [24]–[26]. Cx. tarsalis are naturally uninfected with Wolbachia [27]. We established Wolbachia infections in this mosquito by intrathoracic injection of purified symbionts into adult females, characterized the extent of the infection by fluorescence in situ hybridization and quantitative PCR, and assessed the ability for Wolbachia to block WNV infection, dissemination and transmission at multiple time points. We found that, in contrast to other systems, Wolbachia infection enhanced WNV infection rates 7 days post-blood feeding. This is the first observation of Wolbachia-induced enhancement of a human pathogen in mosquitoes and suggests that caution should be applied before using Wolbachia as part of a vector-borne disease control program.
Methods
Ethics statement
Mosquitoes were maintained on commercially available bovine blood using a membrane feeder. WNV infection experiments were performed under biosafety-level 3 (BSL3) and arthropod-containment level 3 (ACL3) conditions.
Mosquitoes, Wolbachia, and West Nile virus
The Cx. tarsalis YOLO strain was used for experiments. The colony was originally established from Yolo County, CA in 2009. Mosquitoes were reared and maintained at 27°C±1°C, 16∶8 hour light∶dark diurnal cycle at approximately 45% relative humidity in 30×30×30 cm cages. The wAlbB Wolbachia strain was purified from An. gambiae Sua5B cells according to published protocols [28]. Viability and density of the bacteria was assessed using the Live/Dead BacLight Kit (Invitrogen) and a hemocytometer. The experiment was replicated twice; wAlbB concentrations were: replicate one, 5.3×109 bacteria/mL; replicate two, 1.3×1011 bacteria/mL. Two- to four-day-old adult female Cx. tarsalis were anesthetized with CO2 and intrathoracically (IT) injected with approximately 0.1 uL of either wAlbB or Schneider's insect media (Sigma Aldrich) as a control. Mosquitoes were provided with 10% sucrose ad libitum and maintained at 27°C in a growth chamber. WNV strain WN02-1956 (GenBank: AY590222) was originally isolated in African green monkey kidney (Vero) cells from an infected American crow in New York in 2003 [29] and amplified in Aedes albopictus cells (C6/36) to a final titer of 5.0×109 PFU/ml. WNV was added to 5 mL defibrinated bovine blood (Hema-Resource & Supply, Aurora, OR) with 2.5% sucrose solution. Replicate titers were: replicate one, 8.0×107 PFU/mL; replicate two, 3.0×107 PFU/mL. Seven days post Wolbachia injection mosquitoes were fed a WNV infectious blood meal via Hemotek membrane feeding system (Discovery Workshops, Accrington, UK) for approximately one hour. Partially- or non-blood fed females were excluded from the analysis.
Fluorescence in situ hybridization (FISH) and microscopy
To characterize Wolbachia infections in Cx. tarsalis tissues, we performed fluorescence in situ hybridization (FISH) on mosquitoes at 12 dpi according to published protocols [10] with slight modifications. Briefly, mosquitoes were fixed in acetone, embedded in paraffin wax and sectioned with a microtome. Slides were dewaxed with three successive xylene washes for 5 minutes, followed by two 5-minute washes with 100% ethanol and one wash in 95% ethanol before treatment with alcoholic hydrogen peroxide (6% H2O2 in 80% ethanol) for 3 days to minimize autofluorescence. Sectioned tissues were hybridized overnight in 1 ml of hybridization buffer (50% formamide, 5× SSC, 200 g/liter dextran sulfate, 250 mg/liter poly(A), 250 mg/liter salmon sperm DNA, 250 mg/liter tRNA, 0.1 M dithiothreitol [DTT], 0.5× Denhardt's solution) with Wolbachia specific probes W1 and W2 labeled with a 5-prime rhodamine fluorophore [30]. After hybridization, tissues were successively washed three times in 1× SSC, 10 mM DTT and three times in 0.5× SSC, 10 mM DTT. Slides were mounted with SlowFade Gold antifade reagent (Invitrogen) and counterstained with DAPI (Roche). Images were captured with a LSM 510 META confocal microscope (Zeiss) and epifluorescent BX40 microscope (Olympus). Images were processed using LSM image browsers (Zeiss) and Photoshop 7.0 (Adobe) software. No-probe, competition probe and RNAse treatment controls were conducted (Figure S1).
Vector competence for WNV
Virus infection and transmission assays were performed as described at 7 and 14 days post blood feeding [31]–[33]. Female mosquitoes were anesthetized with triethylamine (Sigma, St. Louis, MO), legs from each mosquito were removed and placed separately in 1 mL mosquito diluent (MD: 20% heat-inactivated fetal bovine serum [FBS] in Dulbecco's phosphate-buffered saline, 50 ug/mL penicillin/streptomycin, 50 ug/mL gentamicin and 2.5 ug/mL fungizone). The proboscis of each mosquito was positioned in a tapered capillary tube containing 10 uL of a 1∶1 solution of 50% sucrose and FBS to induce salivation. After 30 minutes, the contents were expelled into 0.3 mL MD and bodies were placed individually into 1 mL MD. Mosquito body, legs and salivary secretion samples were stored at −70°C until tested for WNV presence and Wolbachia titers. Mosquito bodies and legs were homogenized for 30 seconds utilizing Qiagen Tissue Lyser at 24 cycles/second, followed by clarification via centrifugation for one minute. Mosquito samples were tested for WNV infectious particles by plaque assay on Vero cells [34]. Infection was defined as the proportion of mosquitoes with WNV positive bodies. Dissemination and transmission were defined as the proportion of infected mosquitoes with WNV positive legs and salivary secretions, respectively. Proportions were compared using Fisher's exact test. The experiment was replicated twice.
Quantitative real-time PCR (qPCR) of Wolbachia density
To evaluate Wolbachia density in individual mosquitoes from vector competence experiments, DNA was extracted using DNeasy Blood and Tissue kits (Qiagen) and used as template for qPCR on a Rotor Gene Q (Qiagen) with the SYBR green PCR kit (Qiagen). Wolbachia DNA was amplified with primers Alb-GF and Alb-GR [35] and was normalized to the Cx. tarsalis actin gene [36] (Table 1). Wolbachia to host genome ratios were calculated using Qgene [37]. PCRs were performed in duplicate. Comparisons of Wolbachia titers between treatments were analyzed using Mann-Whitney U test.
Table 1. Primers used for qPCR.
| Primer | Sequence 5′-3′ | Reference |
| REL1-F | GCGACTTTGGCATCAAGCTC | This study |
| REL1-R | GTTCGACCGGAGCGTAGTAG | |
| REL2-F | GTCGAGATGGCCAAAACGATG | This study |
| REL2-R | ACTCACTCATATTGTTGATGGCATT | |
| CACTUS-F | GACCTGTGCAAGAGTCTGCT | This study |
| CACTUS-R | ACGTATCACCATCGTCGTTC | |
| DEFENSIN-F | TTGTTTGCTTCGTTGCTCTTT | This study |
| DEFENSIN-R | ATCTCCTACACCGAACCCACT | |
| DIPTERICIN-F | CCCAGCGCTGCTTACTT | This study |
| DIPTERICIN-R | CATCATCCAGGCCGAGAAC | |
| ALB-GF | GGTTTTGCTTATCAAGCAAAAG | [35] |
| ALB-GR | GCGCTGTAAAGAACGTTGATC | |
| ACTIN-F | GACTACCTGATGAAGATCCTGAC | [36] |
| ACTIN-R | GCACAGCTTTTCCTTGATGTCGC |
Cx. tarsalis immune gene expression in response to Wolbachia
To explore Wolbachia effects on mosquito immune gene expression, one- to four- day old adult female Cx. tarsalis were anesthetized with CO2 and injected as described above with Wolbachia (wAlbB) or Schneider's insect media as control. Mosquitoes were provided with 10% sucrose ad libitum and maintained at 27°C in a growth chamber. At 7 dpi, mosquitoes were blood fed on bovine blood via glass membrane feeder. At 2 dpf, five mosquitoes per treatment were harvested and RNA extracted using RNeasy mini kits (Qiagen). Extracted RNA was DNase treated (Ambion #AM1906) and converted to cDNA using Superscript III with random hexamers (Invitrogen #18080-51) according to the manufacturers' protocols. qPCRs were performed using the Rotor Gene Q (Qiagen) and SYBR Green qPCR kit (Qiagen) according to the manufacturer's protocol. Five target immune genes in the Toll and IMD innate immune pathways (REL1, REL2, cactus, defensin and diptericin) were selected, primers designed based on homologous genes in the Anopheles gambiae, Aedes aegypti and Culex pipiens genomes and normalized to host actin (Table 1). Gene expression was analyzed by calculating ratios of target to host gene and tested for significance using Mann-Whitney U test. All qPCRs were technically replicated twice.
Results
Fluorescence in situ hybridization (FISH)
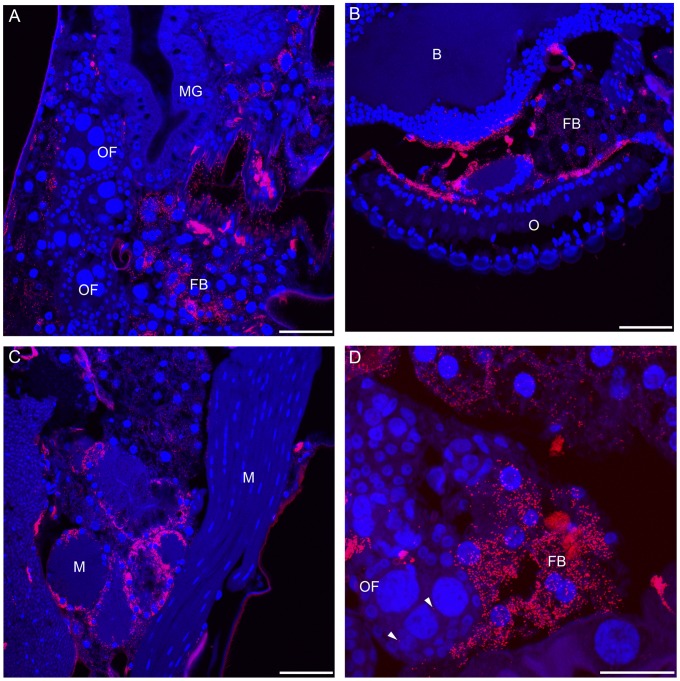
Using fluorescence in situ hybridization, we observed that wAlbB establishes an infection in both somatic and germline tissue in Cx. tarsalis 12 days post injection. Wolbachia disseminated to various tissues including the head, proboscis, thoracic flight muscles, fat body and ovarian follicles (Figure 1). Cx. tarsalis appeared heavily infected, suggesting that adult microinjection is an effective method to experimentally infect this mosquito species.
Figure 1. Fluorescence in situ hybridization of Wolbachia infection in Cx. tarsalis mosquitoes 12 days post injection.
Confocal microscopy of sectioned mosquitoes shows Wolbachia infection in diverse tissues after adult microinjection. A. Wolbachia localized in the abdomen of Cx. tarsalis. B. Wolbachia infection disseminated to the head and nervous tissue. C. Wolbachia is present in the muscular tissue of the mosquito. D. Wolbachia infection within and surrounding the ovarian follicles. Arrowheads denote infection within the ovarian follicle. The scale bar represents 50 um. OF; ovarian follicle, MG; midgut, FB; fat body, M; muscle, B; brain, O; omnitidia. Red = Wolbachia; Blue = mosquito DNA.
Vector competence for WNV
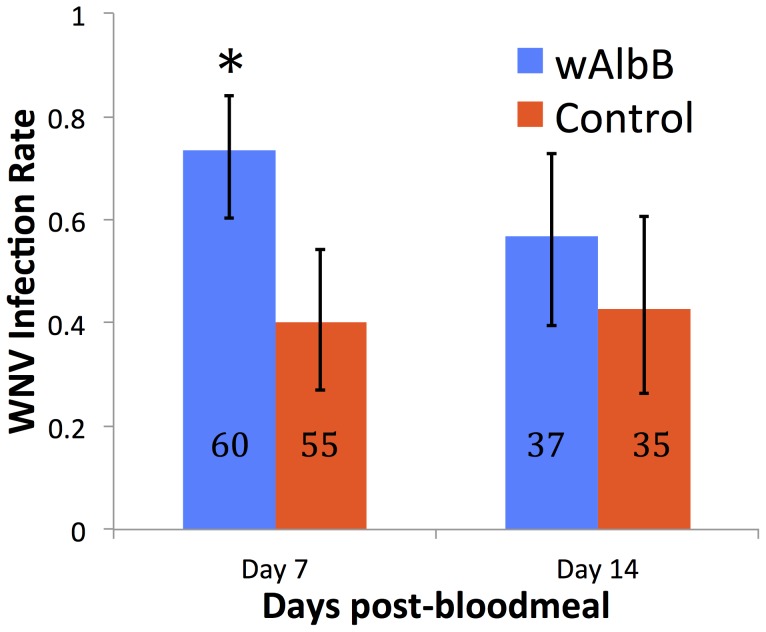
We evaluated the vector competence of Wolbachia-infected and uninfected Cx. tarsalis for WNV in mosquito bodies, legs and salivary secretions to determine infection, dissemination and transmission rates, respectively. Replicate results were similar, and results from pooled replicates or analysis of individual replicates were identical, so the pooled analysis is presented for clarity; results from individual replicates are available as Table S1. wAlbB-infected Cx. tarsalis displayed significantly higher WNV infection rates 7 days post-feeding (dpf) (P = 0.04). A similar but non-significant trend was observed 14 dpf (Figure 2). If mosquitoes were infected, virus dissemination and transmission rates did not differ statistically (Table S1).
Figure 2. Effect of wAlbB infection status on WNV probability of infection in Cx. tarsalis.
wAlbB infection significantly increases WNV infection 7 days post-bloodmeal. Asterisk denotes statistical significance (P = 0.04). N denotes sample size. Error bars represent 95% binomial confidence intervals.
Quantitative real-time PCR (qPCR) of Wolbachia density
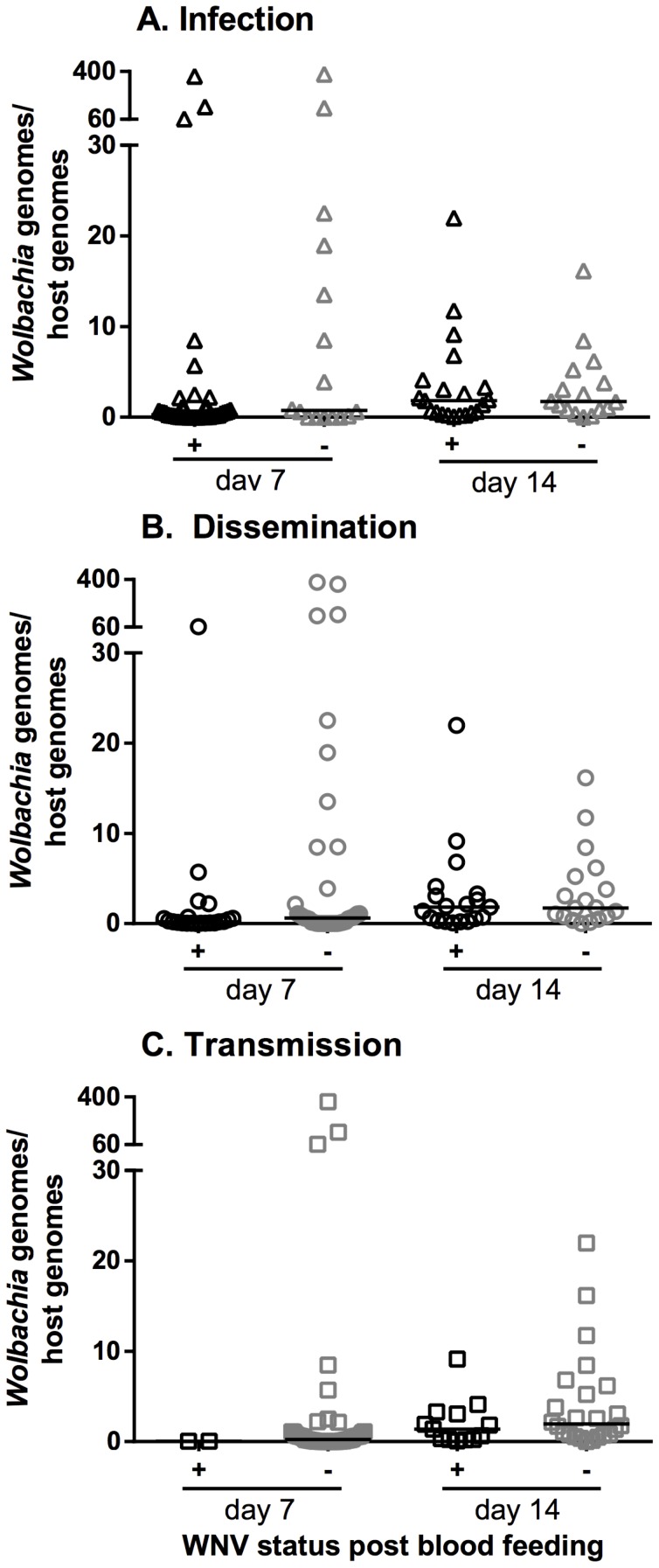
To determine if there was a Wolbachia density effect on WNV phenotype, qPCR was used to compare Wolbachia titers in mosquitoes either positive or negative WNV. Wolbachia titers in WNV-infected versus uninfected Cx. tarsalis did not differ statistically; similarly, no significant titer differences were found in individuals that disseminated versus non-disseminated or transmitted vs. non-transmitted (Figure 3).
Figure 3. Comparison of WNV infection status and Wolbachia titers in Cx. tarsalis.
Wolbachia titers in mosquito bodies were compared between WNV positive (black symbols) or negative (gray symbols) bodies, legs and salivary secretions. (A) Infection, (B) Dissemination, and (C) Transmission.
Cx. tarsalis immune gene expression in response to Wolbachia
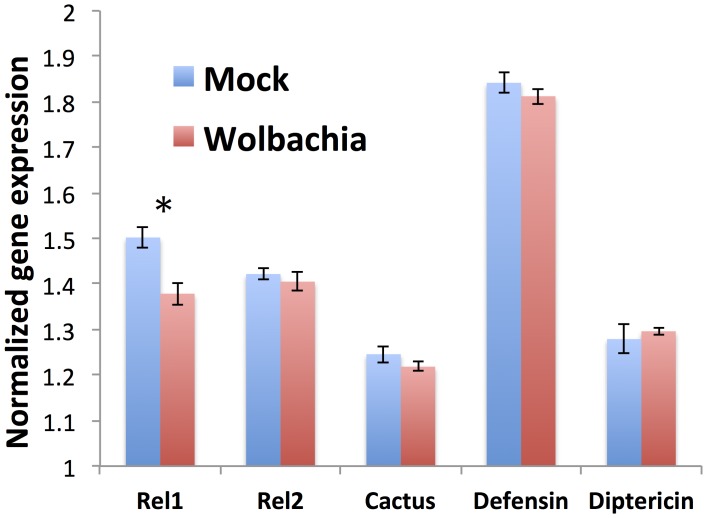
To elucidate the mechanism behind Wolbachia mediated WNV infection enhancement in Cx. tarsalis, we evaluated mosquito immune gene expression in response to Wolbachia using qPCR. Unlike other systems [38]–[40], Wolbachia did not induce a significant immune response in Cx. tarsalis females compared to the control. In contrast, REL1 (the NF kappa B activator of the antiviral Toll pathway) was significantly reduced in Wolbachia-infected mosquitoes compared to controls (one-tailed P = 0.008) (Figure 4).
Figure 4. Cx. tarsalis immune gene expression in response to Wolbachia infection.
Expression for each gene was normalized to the S7 gene. Cx. tarsalis females were injected with Wolbachia or media as control, blood fed 7 days post-injection and harvested 2 dpf to assess expression of five key immune genes. N = 5 per gene. REL1 expression in Wolbachia injected mosquitoes is significantly higher compared to control (one-tailed P = 0.008; asterisk). Error bars represent standard errors.
Discussion
Caveats of this study
It should be noted that these experiments were performed with mosquitoes transiently infected in the somatic tissues with Wolbachia, rather than a stable maternally inherited infection. It remains to be seen whether a stable wAlbB infection will enhance WNV in a similar way. Wolbachia density in mosquito somatic tissues (as opposed to germline) was found to explain differences in virus infection in Aedes mosquitoes [41]. Thus, it seems likely that if stable infection in Cx. tarsalis has a similar somatic tissue distribution to a transient infection it may induce a similar virus enhancement phenotype. However, this must be tested empirically. It is also unknown whether virus enhancement is limited to WNV or occurs more broadly. Finally, we tested a single Wolbachia strain, and it is unknown whether virus enhancement is specific to wAlbB or occurs with diverse Wolbachia strains.
Previous studies have shown that pathogen suppression by Wolbachia has the potential to be a novel method for controlling vector-borne diseases [4], [42]–[44]. Not all mosquito species are naturally infected with Wolbachia, but non-infected species may support infection once introduced and these novel infections often effectively inhibit various pathogens [5], [45]. Our experiments indicate that following adult microinjection, Wolbachia is capable of establishing both somatic and germline infection in Cx. tarsalis but does not inhibit WNV infection, dissemination or transmission. In contrast with other studies showing pathogen inhibition by Wolbachia, our data suggest that Wolbachia may in fact increase WNV infection rates in Cx. tarsalis, particularly at early time points. Increased early infection has the potential to shorten the extrinsic incubation period of the pathogen, which can dramatically increase the reproductive rate of the virus [19]. It has become increasingly clear that Wolbachia does not always suppress pathogens in insects [46]. For example, the cereal crop pest Spodoptera exempta is more susceptible to nucleopolydrovirus mortality in the presence of Wolbachia [47]. In the mosquitoes An. gambiae An. stephensi, Ae. fluviatilis and Cx. pipiens, Wolbachia enhances Plasmodium berghei, P. yoelii, P. gallinaceum and P. relictum, respectively [17]–[20]. Enhancement may be dependent on the host-Wolbachia strain-pathogen system of interest, as Wolbachia strains that block one pathogen yet enhance another have been documented [9], [17]. Wolbachia-mediated pathogen enhancement may be a common yet often ignored phenomenon, which merits attention when designing Wolbachia-based strategies for disease control [46].
Intracellular infection with bacteria may alter the cellular environment in multiple ways, including bacterial manipulation to avoid host immune defenses [48]. Though the exact Wolbachia-mediated inhibition mechanism is unknown, studies have suggested that Wolbachia indirectly modulates mosquito immunity [40], [49]. Wolbachia can activate the Toll pathway, stimulating a cascade of events that have been correlated with inhibition of dengue and Plasmodium in mosquitoes [39], [50], [51]. In contrast, in Cx. tarsalis, wAlbB infection significantly downregulated REL1 (the activator of the Toll pathway), suggesting that in this system Wolbachia may down regulate antiviral Toll-based immunity leading to increased virus infection. However, while statistically significant, this decrease in REL1 expression was modest, and further study is required to determine the precise mechanism of Wolbachia-based WNV enhancement in this system.
To our knowledge this is first study showing Wolbachia can potentially enhance a vector-borne pathogen that causes human disease. Our results, combined with other Wolbachia enhancement studies [17]–[20], [46]–[47], suggest that field deployment of Wolbachia-infected mosquitoes should proceed with caution. Wolbachia effects on all potential pathogens in the study area should be determined. Additionally, several studies have shown that Wolbachia is capable of horizontal transfer to other insect species which could have unforeseen effects on non-target insects [52]–[54]. A lack of understanding of Wolbachia-pathogen-mosquito interactions could impact efficacy of disease control programs. Cx. tarsalis is a competent vector for many human pathogens, and further studies that assess alternative Wolbachia strains and viruses in Cx. tarsalis may elucidate the importance of host background on pathogen interference phenotypes in this medically important mosquito species.
Supporting Information
FISH controls. Red: Wolbachia , Blue: mosquito DNA, Green: background fluorescence. Top row: positive ( w AlbB) control.
(PDF)
Results from individual vector competence replicates.
(PDF)
Acknowledgments
We thank the Wadsworth Center Tissue Culture Core facility for providing Vero and C636 cells; and William Reisen for providing mosquitoes used to establish the Cx. tarsalis colony. We are grateful to Anne Payne and Rhiannon Barry for technical assistance. We thank the Ross Confocal Microscopy Facility for confocal microscope access and John Gibas for assistance with confocal microscopy.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. Data from individual replicates available as Supporting Table 1.
Funding Statement
This research was funded by NIH grants R01AI067371, R21AI070178 and R21AI111175 to JLR. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Moiroux N, Gomez MB, Pennetier C, Elanga E, Djènontin A, et al. (2012) Changes in Anopheles funestus biting behavior following universal coverage of long-lasting insecticidal nets in Benin. J Infect Dis 206: 1622–1629 10.1093/infdis/jis565 [DOI] [PubMed] [Google Scholar]
- 2. Syed Z, Leal WS (2008) Mosquitoes smell and avoid the insect repellent DEET. Proc Natl Acad Sci 105: 13598–13603 10.1073/pnas.0805312105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Read AF, Lynch PA, Thomas MB (2009) How to make evolution-proof insecticides for malaria control. PLoS Biol 7: e1000058 10.1371/journal.pbio.1000058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ricci I, Damiani C, Rossi P, Capone A, Scuppa P, et al. (2011) Mosquito symbioses: from basic research to the paratransgenic control of mosquito-borne diseases. J Appl Entomol 135: 487–493 10.1111/j.1439-0418.2011.01613.x [DOI] [Google Scholar]
- 5. Hilgenboecker K, Hammerstein P, Schlattmann P, Telschow A, Werren JH (2008) How many species are infected with Wolbachia?–A statistical analysis of current data. FEMS Microbiol Lett 281: 215–220 10.1111/j.1574-6968.2008.01110.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hedges LM, Brownlie JC, O'Neill SL, Johnson KN (2008) Wolbachia and virus protection in insects. Science 322: 702 10.1126/science.1162418 [DOI] [PubMed] [Google Scholar]
- 7. Teixeira L, Ferreira A, Ashburner M (2008) The bacterial symbiont Wolbachia induces resistance to RNA viral infections in Drosophila melanogaster . PLoS Biol 6: e1000002 10.1371/journal.pbio.1000002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Van den Hurk AF, Hall-Mendelin S, Pyke AT, Frentiu FD, McElroy K, et al. (2012) Impact of Wolbachia on infection with chikungunya and yellow fever viruses in the mosquito vector Aedes aegypti . PLoS Negl Trop Dis 6: e1892 10.1371/journal.pntd.0001892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Glaser RL, Meola MA (2010) The native Wolbachia endosymbionts of Drosophila melanogaster and Culex quinquefasciatus increase host resistance to West Nile virus infection. PLoS One 5: e11977 10.1371/journal.pone.0011977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hughes GL, Koga R, Xue P, Fukatsu T, Rasgon JL (2011) Wolbachia infections are virulent and inhibit the human malaria parasite Plasmodium falciparum in Anopheles gambiae . PLoS Pathog 7: e1002043 10.1371/journal.ppat.1002043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hoffmann AA, Montgomery BL, Popovici J, Iturbe-Ormaetxe I, Johnson PH, et al. (2011) Successful establishment of Wolbachia in Aedes populations to suppress dengue transmission. Nature 476: 454–457 10.1038/nature10356 [DOI] [PubMed] [Google Scholar]
- 12. Werren JH (1997) Biology of Wolbachia . Annu Rev Entomol 42: 587–609 10.1146/annurev.ento.42.1.587 [DOI] [PubMed] [Google Scholar]
- 13. Bourtzis K, Dobson SL, Xi Z, Rasgon JL, Calvitti M, et al. (2014) Harnessing mosquito-Wolbachia symbiosis for vector and disease control. Acta Trop 132 Suppl: S150–63 10.1016/j.actatropica.2013.11.004 [DOI] [PubMed] [Google Scholar]
- 14. Frentiu FD, Zakir T, Walker T, Popovici J, Pyke AT, et al. (2014) Limited dengue virus replication in field-collected Aedes aegypti mosquitoes infected with Wolbachia . PLoS Negl Trop Dis 8: e2688 10.1371/journal.pntd.0002688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Osborne SE, Leong YS, O'Neill SL, Johnson KN (2009) Variation in antiviral protection mediated by different Wolbachia strains in Drosophila simulans . PLoS Pathog 5: e1000656 10.1371/journal.ppat.1000656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hussain M, Lu G, Torres S, Edmonds JH, Kay BH, et al. (2013) Effect of Wolbachia on replication of West Nile virus in a mosquito cell line and adult mosquitoes. J Virol 87: 851–858 10.1128/JVI.01837-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hughes GL, Vega-Rodriguez J, Xue P, Rasgon JL (2012) Wolbachia strain wAlbB enhances infection by the rodent malaria parasite Plasmodium berghei in Anopheles gambiae mosquitoes. Appl Environ Microbiol 78: 1491–1495 10.1128/AEM.06751-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Baton LA, Pacidônio EC, Gonçalves DDS, Moreira LA (2013) wFlu: Characterization and evaluation of a native Wolbachia from the mosquito Aedes fluviatilis as a potential vector control agent. PLoS One 8: e59619 10.1371/journal.pone.0059619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Murdock CC, Blanford S, Hughes GL, Rasgon JL, Thomas MB (2014) Temperature alters Plasmodium blocking by Wolbachia . Sci Rep 4: 3932 10.1038/srep03932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zélé F, Nicot A, Berthomieu A, Weill M, Duron O, et al. (2014) Wolbachia increases susceptibility to Plasmodium infection in a natural system. Proc R Soc 281 10.1098/rspb.2013.2837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Reisen WK, Fang Y, Martinez VM (2005) Avian host and mosquito (Diptera: Culicidae) vector competence determine the efficiency of West Nile and St. Louis encephalitis virus transmission. J Med Entomol 42: 367–375 10.1603/0022-2585(2005)0420367:AHAMDC2.0.CO2 [DOI] [PubMed] [Google Scholar]
- 22. Cupp EW, Tennessen KJ, Oldland WK, Hassan HK, Hill GE, et al. (2004) Mosquito and arbovirus activity during 1997–2002 in a wetland in northeastern Mississippi. J Med Entomol 41: 495–501 10.1603/0022-2585-41.3.495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bohart RM and Washino R (1978) Mosquitoes of California. Berkeley: University of California Press. [Google Scholar]
- 24. Meyer RP, Hardy JL, Presser SB (1983) Comparative vector competence of Culex tarsalis and Culex quinquefasciatus from the Coachella, Imperial, and San Joaquin Valleys of California for St. Louis encephalitis virus. Am J Trop Med Hyg 32: 305–311. [DOI] [PubMed] [Google Scholar]
- 25. Hammon W, Reeves W (1943) Laboratory transmission of western equine encephalomyelitis virus by mosquitoes of the genera Culex and Culiseta . J Exp Med 78: 425–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Goddard LB, Roth AE, Reisen WK, Scott TW (2002) Vector competence of California mosquitoes for West Nile virus. Emerg Infect Dis 8: 1385–1391 10.3201/eid0812.020536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rasgon JL, Scott TW (2004) An initial survey for Wolbachia (Rickettsiales: Rickettsiaceae) infections in selected California mosquitoes (Diptera: Culicidae). J Med Entomol 41: 255–257 10.1603/0022-2585-41.2.255 [DOI] [PubMed] [Google Scholar]
- 28. Rasgon JL, Gamston CE, Ren X (2006) Survival of Wolbachia pipientis in cell-free medium. Appl Environ Microbiol 72: 6934–6937 10.1128/AEM.01673-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ebel GD, Carricaburu J, Young D, Bernard KA, Kramer LD (2004) Genetic and phenotypic variation of West Nile virus in New York, 2000–2003. Am J Trop Med Hyg 71: 493–500. [PubMed] [Google Scholar]
- 30. Heddi A, Grenier A, Khatchadourian C, Charles H, Nardon P (1999) Four intracellular genomes direct weevil biology: nuclear, mitochondrial, principal endosymbiont, and Wolbachia. Proc Natl Acad Sci 96: 6814–6819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Aitken T (1977) An in vitro feeding technique for artifically demonstrating virus transmission by mosquitoes. Mosq News 37: 130–133. [Google Scholar]
- 32. Dodson BL, Kramer LD, Rasgon JL (2012) Effects of larval rearing temperature on immature development and West Nile virus vector competence of Culex tarsalis . Parasit Vectors 5: 199 10.1186/1756-3305-5-199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Dodson BL, Kramer LD, Rasgon JL (2011) Larval nutritional stress does not affect vector competence for West Nile virus (WNV) in Culex tarsalis . Vector Borne Zoonotic Dis 11: 1493–1497 10.1089/vbz.2011.0662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Payne AF, Binduga-Gajewska I, Kauffman EB, Kramer LD (2006) Quantitation of flaviviruses by fluorescent focus assay. J Virol Methods 134: 183–189 10.1016/j.jviromet.2006.01.003 [DOI] [PubMed] [Google Scholar]
- 35. Hughes GL, Pike AD, Xue P, Rasgon JL (2012) Invasion of Wolbachia into Anopheles and other insect germlines in an ex vivo organ culture system. PLoS One 7: e36277 10.1371/journal.pone.0036277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Provost-Javier KN, Chen S, Rasgon JL (2010) Vitellogenin gene expression in autogenous Culex tarsalis . Insect Mol Biol 19: 423–429 10.1111/j.1365-2583.2010.00999.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Joehanes R, Nelson JC (2008) QGene 4.0, an extensible Java QTL-analysis platform. Bioinformatics 24: 2788–2789 10.1093/bioinformatics/btn523 [DOI] [PubMed] [Google Scholar]
- 38. Kambris Z, Cook PE, Phuc HK, Sinkins SP (2009) Immune activation by life-shortening Wolbachia and reduced filarial competence in mosquitoes. Science 326: 134–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kambris Z, Blagborough AM, Pinto SB, Blagrove MSC, Godfray HCJ, et al. (2010) Wolbachia stimulates immune gene expression and inhibits Plasmodium development in Anopheles gambiae . PLoS Pathog 6: e1001143 10.1371/journal.ppat.1001143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hughes GL, Ren X, Ramirez JL, Sakamoto JM, Bailey J a, et al. (2011) Wolbachia infections in Anopheles gambiae cells: transcriptomic characterization of a novel host-symbiont interaction. PLoS Pathog 7: e1001296 10.1371/journal.ppat.1001296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lu P, Bian G, Pan X, Xi Z (2012) Wolbachia induces density-dependent inhibition to dengue virus in mosquito cells. PLoS Negl Trop Dis 6: e1754 10.1371/journal.pntd.0001754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Iturbe-Ormaetxe I, Walker T, O'Neill SL (2011) Wolbachia and the biological control of mosquito-borne disease. EMBO Rep 12: 508–518 10.1038/embor.2011.84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Walker T, Moreira LA (2011) Can Wolbachia be used to control malaria? Mem Inst Oswaldo Cruz 106: 212–217. [DOI] [PubMed] [Google Scholar]
- 44. Riehle MA, Moreira CK, Lampe D, Lauzon C, Jacobs-Lorena M (2007) Using bacteria to express and display anti-Plasmodium molecules in the mosquito midgut. Int J Parasitol 37: 595–603 10.1016/j.ijpara.2006.12.002 [DOI] [PubMed] [Google Scholar]
- 45. Hughes GL, Rasgon JL (2013) Transinfection: a method to investigate Wolbachia-host interactions and control arthropod-borne disease. Insect Mol Biol 10.1111/imb.12066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hughes GL, Rivero A, Rasgon JL (2014) Wolbachia can enhance Plasmodium infection in mosquitoes: Implications for malaria control? PLoS Pathog In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Graham RI, Grzywacz D, Mushobozi WL, Wilson K (2012) Wolbachia in a major African crop pest increases susceptibility to viral disease rather than protects. Ecol Lett 15: 993–1000 10.1111/j.1461-0248.2012.01820.x [DOI] [PubMed] [Google Scholar]
- 48. Finlay BB, McFadden G (2006) Anti-immunology: evasion of the host immune system by bacterial and viral pathogens. Cell 124: 767–782 10.1016/j.cell.2006.01.034 [DOI] [PubMed] [Google Scholar]
- 49. Siozios S, Sapountzis P, Ioannidis P, Bourtzis K (2008) Wolbachia symbiosis and insect immune response. Insect Sci 15: 89–100 10.1111/j.1744-7917.2008.00189.x [DOI] [Google Scholar]
- 50. Pan X, Zhou G, Wu J, Bian G, Lu P, et al. (2011) Wolbachia induces reactive oxygen species (ROS)-dependent activation of the Toll pathway to control dengue virus in the mosquito Aedes aegypti . Proc Natl Acad Sci U S A 109: E23–31 10.1073/pnas.1116932108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Xi Z, Ramirez JL, Dimopoulos G (2008) The Aedes aegypti Toll pathway controls dengue virus infection. PLoS Pathog 4: e1000098 10.1371/journal.ppat.1000098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Le Clec'h W, Chevalier FD, Genty L, Bertaux J, Bouchon D, et al. (2013) Cannibalism and predation as paths for horizontal passage of Wolbachia between terrestrial isopods. PLoS One 8: e60232 10.1371/journal.pone.0060232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Vavre F, Fleury F, Lepetit D, Fouillet P, Boulétreau M (1999) Phylogenetic evidence for horizontal transmission of Wolbachia in host-parasitoid associations. Mol Biol Evol 16: 1711–1723. [DOI] [PubMed] [Google Scholar]
- 54. Heath BD, Butcher RD, Whitfield WG, Hubbard SF (1999) Horizontal transfer of Wolbachia between phylogenetically distant insect species by a naturally occurring mechanism. Curr Biol 9: 313–316. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
FISH controls. Red: Wolbachia , Blue: mosquito DNA, Green: background fluorescence. Top row: positive ( w AlbB) control.
(PDF)
Results from individual vector competence replicates.
(PDF)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. Data from individual replicates available as Supporting Table 1.