Abstract
Background
Since lateral tibial slope (LTS) affects the amount of anterior tibial translation and anterior cruciate ligament (ACL) strain during a dynamic maneuver, accurate measurements of lateral tibial slope may be beneficial in screening individuals at a higher risk for ACL injury. Methods for measuring LTS on magnetic resonance imaging scans of the proximal tibia include the midpoint and circle methods. There are no current studies that have validated different LTS measurements methods using a proximal tibia magnetic resonance imaging scan.
Hypothesis
We tested the null hypotheses that (1) LTS measurements were independent of the length of tibia imaged using the midpoint method, and (2) LTS measurements calculated from different methods (‘midpoint’, ‘circle’, and ‘full tibia’) would not differ significantly.
Study Design
Descriptive Laboratory Study
Methods
Blinded observers measured LTS from 3-Tesla 3D magnetic resonance images from 40 size-matched donors according to one circle method and three midpoint methods. Outcomes were then compared to the full tibial anatomical axis (line connecting the center of two circles fit within the proximal and distal tibia) in 11 donors. Bonferroni-correct paired t-tests (p < 0.005 significant) were used to compare the five methods.
Results
The circle and full tibia methods had the lowest inter- and intra-observer variability, while the midpoint method with 10 cm tibia was the most variable. The midpoint method with 10cm and 15 cm proximal tibia closely resembled LTS measurements with the full tibia anatomic axis. The circle method, while repeatable, provided smaller numerical LTS measurements than the full tibia and midpoint methods.
Conclusions
While LTS measurements using the midpoint method can resemble measurements made using the full tibia, the reliability of the midpoint method depends on the length of proximal tibia used. The circle method may be the preferred method for future studies since it was the most repeatable method and is independent of proximal tibia length.
Clinical Relevance
LTS measurements vary depending on the method utilized.
Keywords: tibial slope, tibial anatomical axis, magnetic resonance imaging, image analysis, anterior cruciate ligament
INTRODUCTION
Clinical measurements of posterior tibial slope are important for understanding anterior cruciate ligament (ACL) injury mechanisms. ACL-injured individuals have a greater posterior tibial slope than healthy controls2, 3, 8, 9, 12, 19-23. Posterior tibial slope is commonly measured in both the lateral and medial compartments of the tibial plateau. ACL-injured individuals have a greater lateral tibial slope than medial tibial slope8, 21 and the difference between these two slopes may influence dynamic landing knee biomechanics14, 19. Previous studies have validated different radiographic methods for measuring posterior tibial slope4. No significant difference exists between radiographs, computed tomography, and magnetic resonance imaging (MRI)24. Recent work has focused on MRI2, 8, 10, 11, 13, 19, 21, 22. We are unaware of any studies that compare the different MRI methods for measuring lateral tibial slope. A recent review article has highlighted the need to validate lateral tibial slope measurements with magnetic resonance imaging, especially against a gold standard, because tibial slope measurements are becoming more important in understanding ACL injury mechanisms25.
Tibial slope is commonly defined as the angle between a line fit to the posterior-inferior surface of the tibial plateau and a tibial anatomic reference line3. The proposed MRI methods for measuring lateral tibial slope use a reference line by measuring the tibial proximal anatomical axis (TPAA) using either the “midpoint method”2, 7, 8, which connects the midpoints of two anteroposterior tibial lines within the proximal end of the tibia, or the “circle method”10, 11, 13, which connects the center of two circles within the proximal tibia (Figure 1). This study validates those different methods for measuring lateral tibial slope. Due to the concavity of the posterior tibial cortex and the presence of the tibial tuberosity, the midpoint method may be affected by proximal tibial bone length within the scan. Furthermore, the relationship between lateral tibial slope measurements using the midpoint method, circle method, and a control method utilizing the full tibia is unknown.
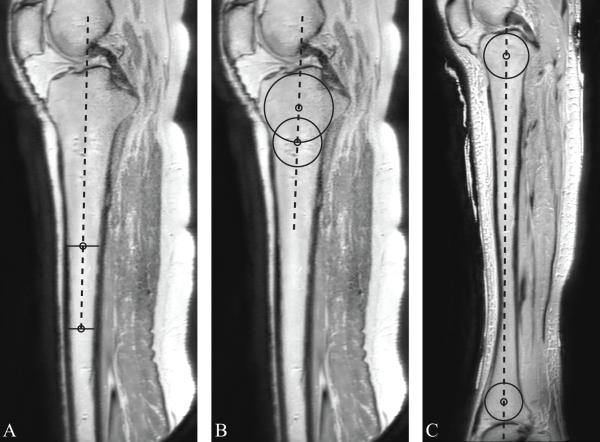
Figure 1.
The tibial longitudinal axis (dashed lines) was defined using (a) the midpoint method (distal line: 15 cm), (b) the circle method, and (c) the full tibia method. The specifics for each method are outlined in the Materials and Methods section.
The objective of this study was to compare MRI methods of measuring lateral tibial slope with the midpoint method and the circle method, validating these measurements against an MR scan of the full tibia. Our null hypotheses were (1) lateral tibial slope measurements using the midpoint method will not be affected by the length of tibia in the image; (2) lateral tibial slope measurements will not differ between the midpoint method and the circle method; and (3) a new method using the full tibial anatomic axis will not result in different lateral tibial slope measurements than methods which only utilize the proximal end of the tibia.
MATERIALS AND METHODS
Forty cadaveric lower extremities from 22 female and 7 male height- and weight-matched donors (mean (SD) age: 59(14) yrs; height: 169(11) cm; weight: 70(7) kg) were acquired from the University of Michigan Anatomical Donations Program and the Anatomy Gift Registry (Hanover, MD). They were MR scanned prior to their use in an in vitro experiment (not reported here). All forty lower extremities underwent 3-Tesla MRI scans where a minimum of 20 cm of proximal tibia captured within the image set (3T Phillips Scanner, T2-weighted 3D-PE sequence; field of view: 290 mm; slice thickness: 0.7 mm). In addition, 11 of the 40 lower extremities underwent an additional scan that acquired the entire length of the tibia within the scan (same image sequence except field of view: 400 mm). The lateral tibial slope measurements were performed using the OsiriX software package (v3.9, open source, www.osirix-viewer.com). The 3D multi-planar reconstruction mode was utilized to ensure that the three imaging planes lay on the proper sagittal, axial, and coronal planes of the tibia. Two blinded observers measured lateral tibial slope with five different techniques.
To standardize the scan slices within each observation, the slices corresponding to the central axis and lateral tibial plateau were the same for all methods. The central axis was defined according to the methods of Hudek et al.10, 11: the slice where the tibial attachment of the posterior cruciate ligament was present, the intercondylar eminence was visible, and the anterior and posterior tibial cortices were concave. Lateral tibial plateau measurements were performed at the center of articulation7, 8, where a line was fit to the plateau’s subchondral bone line from the most anterior-proximal point to the most posterior point (Figure 2). All lateral tibial slope measurements were defined as the angle between this lateral tibial plateau line and a line perpendicular to the tibial longitudinal axis.
Figure 2.
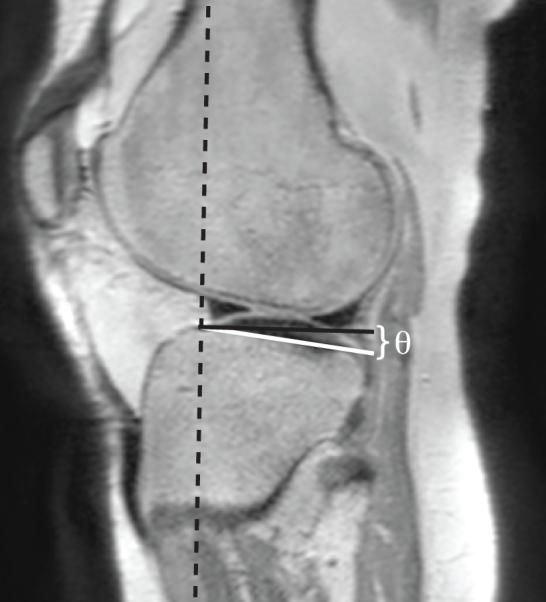
Lateral tibial slope is measured at the center of articulation on the lateral tibial plateau. The tibial proximal anatomic axis (dashed black line), defined by the midpoint method with 15 cm (Fig. 1A), is superimposed on the image. Lateral tibial slope is the angulation (θ) between a line fit to the subchondral bone line (white line) and a line perpendicular to the tibial proximal anatomic axis (black line).
Three methods were used to measure the tibial anatomical axis on the central axis image. The midpoint method, developed by Hashemi et al.7, 8, involved drawing two lines (5 cm apart) that connected the anterior and posterior cortices of the tibia (Figure 1(a)). The midpoints of these two lines were connected, defining the TPAA. The measurement was performed at three locations on the proximal tibia, with the most distal anteroposterior line located 20 cm, 15 cm, and 10 cm from the knee joint line. Secondly, the circle method, introduced by Hudek et al.10, 11, involved drawing two circles within the proximal tibial (Figure 1(b)). The proximal circle was fit within the proximal, anterior, and posterior cortical borders. The center of the distal circle was positioned on the perimeter of the proximal circle, and was fit within the anterior and posterior cortices. A line connecting the center of these two circles defined the TPAA. Finally, a second scan that captured the entire tibia was collected for 11 specimens within the subset. Using the same central axis image, a method similar to the circle method was utilized to fit a circle within the proximal tibia (connecting the anterior, proximal, and distal cortical borders) and the distal tibia (connecting the anterior, distal, and posterior cortical borders) (Figure 1(c)). The center of these two circles was connected to define the full tibial anatomical axis.
Paired two-sided t-tests, with a Bonferroni corrected significance level of p < 0.005 (calculated as alpha level/number of observations = 0.05 / 10), were used to compare lateral tibial slope using (a) the midpoint method using three different lengths of tibia, (b) the circle method, and (c) the full-tibia method. Inter- and intra-observer reliability was examined using intra-class coefficients (ICC), where ICC values greater than 0.9 were considered excellent and values between 0.8 and 0.9 were considered good, as well as typical error calculations with associated 95% confidence intervals. The first blinded observer performed two sets of measurements on all 40 lower extremities with a minimum of one week between observations with a random specimen order. The second observer was blinded to the results of the first observer, and performed the same measurements as the first observer on a random subset of 15 knees (five of which contained the full tibia scan). All analyses were performed in SPSS 19 (IBM Corp., Armonk, NY).
RESULTS
The most repeatable measurement techniques for lateral tibial slope were the circle method and the full tibia method, while the midpoint method using 10 cm of proximal tibia was the least repeatable method (Table 1). Overall, the results of this study showed excellent intra-observer reliability and good-to-excellent inter-observer reliability.
Table 1.
Intra-observer and inter-observer reliability for all five lateral tibial slope measurement methods.
| Intra-observer | Inter-observer | |||
|---|---|---|---|---|
|
|
||||
| Typical Error | ICC | Typical Error | ICC | |
| Midpoint method, 20 cm | ± 0.92° (CI 0.75° - 1.18°) | 0.92 | ± 0.86° (CI 0.44° - 0.99°) | 0.85 |
| Midpoint method, 15 cm | ± 1.08° (CI 0.89° - 1.39°) | 0.9 | ± 0.85° (CI 0.43° - 0.97°) | 0.87 |
| Midpoint method, 10 cm | ± 1.18° (CI 0.97° - 1.52°) | 0.89 | ± 1.08° (CI 0.55° - 1.23°) | 0.79 |
| Circle method | ± 0.84° (CI 0.69° - 1.08°) | 0.92 | ± 0.75° (CI 0.38° - 0.86°) | 0.93 |
| Full tibia method | ± 0.64° (CI 0.53° - 0.83°) | 0.91 | ± 0.89° (CI 0.45° - 1.01°) | 0.85 |
Abbreviations: ICC: Intra-class coefficients; CI: 95% confidence intervals
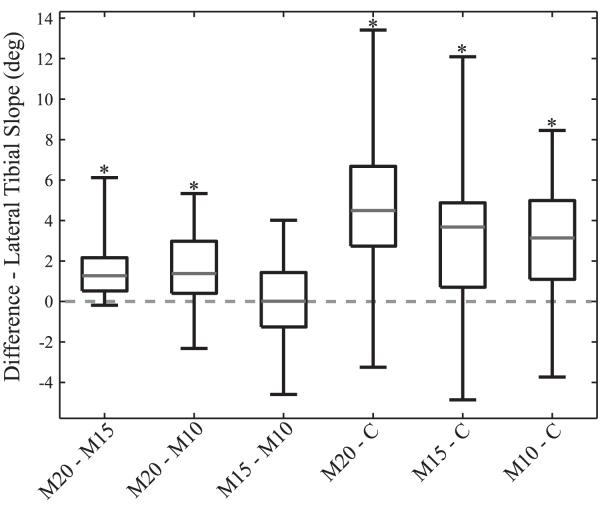
Using proximal tibia scans from 40 donor lower extremities, we found lateral tibial slope measurements using the midpoint method were dependent on the length of proximal tibia, as shown by the significantly difference in lateral tibial slope when 20 cm (mean ± SD: 10.0 ± 3.3 deg) and 15 cm (8.4 ± 3.4 deg) of proximal tibia were used (p < 0.001), as well as 20 cm and 10 cm (8.3 ± 3.7 deg) (Figure 3; p < 0.001). However, there was no significant difference in lateral tibial slope with the midpoint method when 15 cm and 10 cm of proximal tibia were used (p = 0.687). The circle method (5.3 ± 3.1 deg) produced smaller lateral tibial slope measurements than the midpoint method, regardless of the amount of proximal tibial used (Figure 3; p < 0.001 for 20 cm, 15 cm, and 10 cm).
Figure 3.
The box plots compare the difference in lateral tibial slope measurements for 40 knees using the circle method (C) and the midpoint method with 20 cm (M20), 15 cm (M15), and 10 cm (M10) of proximal tibia. Central mark indicates the median value, edges of box indicate 25% and 75% quartiles, and the whiskers indicate the maximum and minimum values. In this figure, the asterisk denotes a significant difference at p < 0.005.
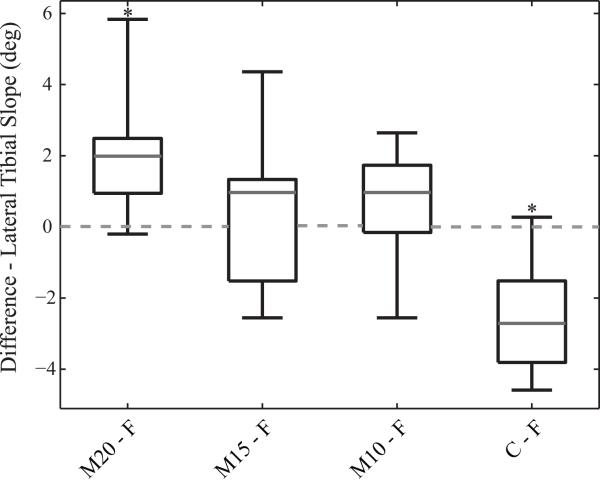
Using full tibia scans from a subset of 11 knees in this study, the full tibia method (6.9 ± 2.2 deg) was significantly different from the circle method (p < 0.001) and the midpoint method when 20 cm of proximal tibia was used (p = 0.003) (Figure 4). The midpoint method using either 15 cm (p = 0.474) or 10 cm (p = 0.225) of proximal tibia provided the closest representation of lateral tibial slope using the full tibia.
Figure 4.
Box plots of the differences in lateral tibial slope for 11 knees as measured with the full-tibia method (F) method with methods utilizing only the proximal tibia: the circle method (C) and the midpoint method (M20, M15, and M10). Central mark indicates the median value, edges of box indicate 25% and 75% quartiles, and the whiskers indicate the maximum and minimum values. In this figure, the asterisk denotes a significant difference at p < 0.005.
DISCUSSION
Differences in lateral tibial slope measurements in clinical research studies may be due to the lack of agreement between measurement methods25. The proximal tibia shows a small range of variation in lateral tibial slope (0° – 14° with the midpoint method8), making accurate measurements most important for clinical assessments. The results show that lateral tibial slope measurements using the midpoint method are affected by the proximal tibial bone length used in the measurement. Secondly, different methods for defining the TPAA with MRI will produce different lateral tibial slope measurements. Furthermore, the midpoint method with 10 cm or 15 cm of proximal tibia closely resembled lateral tibial slope measurements with the full tibia anatomic axis in a subset of 11 knees. Overall, the circle method is the most consistent method for assessing lateral tibial slope with MRI using the proximal tibia.
Reliable clinical measurements of posterior tibial slope are important for understanding ACL injury. An increased posterior tibial slope has been retrospectively linked with a greater ACL injury risk2, 3, 8, 9, 12, 19-23. Furthermore, an increased posterior tibial slope has been linked to greater peak ACL strain during a dynamic landing13, 15, as well as greater anterior tibial translation6, 17, 18 and acceleration15. An increased lateral tibial slope relative to the medial tibial slope can influence dynamic landing biomechanics by coupling knee abduction with internal tibial rotation14, 16, 19. These studies emphasize the importance of accurate, repeatable measurements of posterior tibial slope for clinical interventions.
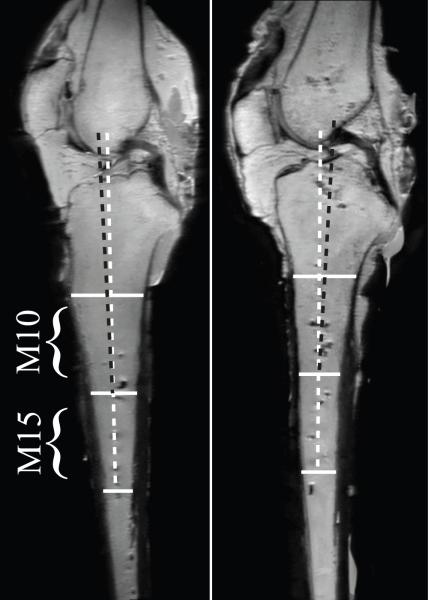
Due to the concave shape of the posterior tibial cortex, the midpoint method is affected by the length of proximal tibia within the MR image, as well as the spacing between the proximal and distal anteroposterior lines. The spacing between the proximal and distal lines was constant in this study, while the amount of tibia used for the measurement was varied, with the distal line positioned 20 cm, 15 cm, and 10 cm from the knee joint line. This controlled approach allowed more consistent measurements than previous work that did not control for tibial length7, 8. While there was no significant difference between 10 cm and 15 cm of proximal tibia using the midpoint method, the data shows that there was as much or more variability between these measurements and 20 cm of proximal tibia (Figure 3). The presence of both positive and negative values with the midpoint method when comparing 10 cm and 15 cm of proximal tibia may be due to the tibial tuberosity shifting the TPAA more anteriorly with the 10 cm midpoint method in some knees (Figure 5). While a standardized method for determining the central axis image was utilized in order to remove subjective errors between observers, there appears to be potential for inter- and intra-observer errors as the midpoint method is used more proximally. Despite the authors’ best efforts to standardize the measurement, there exists the potential for a slightly rotated scan, leading to the presence of the tibial tuberosity (Figure 5). Based on the inter- and intra-reliability measurements (Table 1), this error appears to be exclusive to the midpoint method and did not affect lateral tibial slope measurements with the circle method. The authors speculate that the circle method is not affected because the distal circle lies proximal to the tibial tuberosity.
Figure 5.
The tibial tuberosity can affect tibial slope measurements with the midpoint method, especially with the M10 measurement. The left image shows the tibial tuberosity better than the image on the right (at the level of the proximal anteroposterior line for the M10 measurement). This anatomical detail will affect the ability to perform the M10 measurement, as the tibial tuberosity will shift the tibial proximal anatomic axis (white dashed line) more anteriorly.
If future ACL injury prevention interventions involve morphological screening, it is important to recognize that lateral tibial slope measurements are method-dependent. The circle method will result in a lateral tibial slope measurement that is significantly smaller than that with the midpoint method. This finding is consistent with the results of studies that found the average lateral tibial slope in healthy females was 5.4 deg with the circle method11 but 7.0 deg with the midpoint method8. An average lateral tibial slope of 8.4 degrees measured with the midpoint method has been implicated in females sustaining an ACL injury8. Based on these results, a lateral tibial slope closer to 5.3 degrees using the circle method would have a greater ACL injury risk, based on the mean difference (3.1 degrees) between the midpoint method using 15 cm of proximal tibia and the circle method.
This is the first study to consider the full tibial anatomical axis when utilizing MRI for measuring lateral tibial slope. The tibial shaft axis has been evaluated with radiographs1, 4, 5 or manual measurements26. This study differs slightly by defining full tibial anatomic axis from the proximal and distal tibia, rather than the tibial shaft. It appears that the midpoint method, specifically with 15 cm or 10 cm of proximal tibia, is a better representation of the full tibial anatomical axis than the circle method (Figure 4). Despite this finding, the circle method is still an excellent choice for measuring lateral tibial slope when comparing knee-coil MR images with varying visibility of the proximal tibia. The circle method also had the best inter- and intra-observer reliability statistics (Table 1).
The strengths of this study are the use of two blinded observers for making multiple measurements of lateral tibial slope, the good to excellent ICC values for inter- and intra-observations of each method, and the introduction of a full tibial anatomical axis method for measuring posterior tibial slope. The limitations of this study are unlikely to affect the overall findings. Since these measurements are subjective to the individual observer, we accounted for these differences by reporting the inter-observer and intra-observer reliability. The inter-observer reliability was only performed on a random sample of 15 knees, but we are encouraged by the strong inter-observer reliability reported. Only 11 of the 40 donors had the additional full tibia scan performed. The donors were acquired for a separate in vitro study that focused on the knee joint, so the ankle joint was not always harvested. Despite the smaller sample size of 11 donors, the authors do not believe the full tibia method results, when compared to the circle method or midpoint method using 10 cm or 15 cm of proximal tibia, were underpowered. The authors recognize that the significant difference in LTS measurements between the full tibia method and midpoint method with 20 cm of proximal tibia only achieved 64% power. Due to the numerous observations, we used a Bonferroni correction to limit the potential for type II error and to conserve study power.
The method we utilized for measuring the full tibial anatomic axis was similar to the circle method proposed for the proximal tibia. While a method similar to the midpoint method could have been utilized, we felt that adjusting the circle method for the full-tibia method gave the best representation of the bone’s anatomical axis in the sagittal plane. The selection of the central axis image differed slightly from the method described by Hashemi et al.7, 8 in order to have consistency between the different methods of determining the tibial longitudinal axis. While this study has focused on measuring lateral tibial slope using the subchondral bone line, the slopes of the meniscus10 and articular cartilage may not resemble the subchondral bone line and could influence dynamic knee mechanics. All of these images were acquired from cadaver lower extremities, and some of the knees imaged had the soft tissue distal of the knee joint removed in preparation for a separate in vitro testing protocol.
We conclude that MRI measurements of lateral tibial slope are method-dependent, and there are advantages and disadvantages of each method. The authors recommend the use of the circle method when evaluating lateral tibial slope with a proximal tibia MR image. The circle method had the highest repeatability and is independent of proximal tibia length. However, lateral tibial slope measurements using the circle method were consistently lower than with the full tibia, and this should be taken into account by future researchers. While the midpoint method with 15 cm or 10 cm of proximal tibia produced lateral tibial slope measurements that resembled results with the full tibia method, the authors caution that future studies using the midpoint method should ensure that a consistent length of proximal tibia is utilized.
ACKNOWLEDMENTS
We acknowledge the assistance of Dr. Catherine Brandon and Mrs. Suzan Lowe with imaging, Mr. Christopher J. Bush and Dr. Youkeun Oh with image analysis, and Ms. Ashley Brower with specimen procurement. This study was supported with funding from PHS grant R01 AR054821 and an NDSEG Fellowship (to D.B.L.). The authors have no professional or financial conflicts of interest to report.
Footnotes
Present Address: Rehabilitation Institute of Chicago Sensory Motor Performance Program 345 E Superior St., Room 1401 Chicago, IL 60611
REFERENCES
- 1.Billings A, Scott DF, Camargo MP, Hofmann AA. High tibial osteotomy with a calibrated osteotomy guide, rigid internal fixation, and early motion. Long-term follow-up. J Bone Joint Surg Am. 2000;82(1):70–79. doi: 10.2106/00004623-200001000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Bisson LJ, Gurske-DePerio J. Axial and sagittal knee geometry as a risk factor for noncontact anterior cruciate ligament tear: a case-control study. Arthroscopy. 2010;26(7):901–906. doi: 10.1016/j.arthro.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 3.Brandon ML, Haynes PT, Bonamo JR, Flynn MI, Barrett GR, Sherman MF. The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy. 2006;22(8):894–899. doi: 10.1016/j.arthro.2006.04.098. [DOI] [PubMed] [Google Scholar]
- 4.Brazier J, Migaud H, Gougeon F, Cotten A, Fontaine C, Duquennoy A. Evaluation of methods for radiographic measurement of the tibial slope. A study of 83 healthy knees. Rev Chir Orthop Reparatrice Appar Mot. 1996;82(3):195–200. [PubMed] [Google Scholar]
- 5.Chiu KY, Zhang SD, Zhang GH. Posterior slope of tibial plateau in Chinese. J Arthroplasty. 2000;15(2):224–227. doi: 10.1016/s0883-5403(00)90330-9. [DOI] [PubMed] [Google Scholar]
- 6.Dejour H, Bonnin M. Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg Br. 1994;76(5):745–749. [PubMed] [Google Scholar]
- 7.Hashemi J, Chandrashekar N, Gill B, et al. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg Am. 2008;90(12):2724–2734. doi: 10.2106/JBJS.G.01358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hashemi J, Chandrashekar N, Mansouri H, et al. Shallow medial tibial plateau and steep medial and lateral tibial slopes: new risk factors for anterior cruciate ligament injuries. Am J Sports Med. 2010;38(1):54–62. doi: 10.1177/0363546509349055. [DOI] [PubMed] [Google Scholar]
- 9.Hohmann E, Bryant A, Reaburn P, Tetsworth K. Is there a correlation between posterior tibial slope and non-contact anterior cruciate ligament injuries? Knee Surg Sports Traumatol Arthrosc. 2011;19(Suppl 1):S109–114. doi: 10.1007/s00167-011-1547-4. [DOI] [PubMed] [Google Scholar]
- 10.Hudek R, Fuchs B, Regenfelder F, Koch PP. Is noncontact ACL injury associated with the posterior tibial and meniscal slope? Clin Orthop Relat Res. 2011;469(8):2377–2384. doi: 10.1007/s11999-011-1802-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hudek R, Schmutz S, Regenfelder F, Fuchs B, Koch PP. Novel measurement technique of the tibial slope on conventional MRI. Clin Orthop Relat Res. 2009;467(8):2066–2072. doi: 10.1007/s11999-009-0711-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kostogiannis I, Sward P, Neuman P, Friden T, Roos H. The influence of posterior-inferior tibial slope in ACL injury. Knee Surg Sports Traumatol Arthrosc. 2011;19(4):592–597. doi: 10.1007/s00167-010-1295-x. [DOI] [PubMed] [Google Scholar]
- 13.Lipps DB, Oh YK, Ashton-Miller JA, Wojtys EM. Morphologic characteristics help explain the gender difference in peak anterior cruciate ligament strain during a simulated pivot landing. Am J Sports Med. 2012;40(1):32–40. doi: 10.1177/0363546511422325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McLean SG, Lucey SM, Rohrer S, Brandon C. Knee joint anatomy predicts high-risk in vivo dynamic landing knee biomechanics. Clin Biomech (Bristol, Avon) 2010;25(8):781–788. doi: 10.1016/j.clinbiomech.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 15.McLean SG, Oh YK, Palmer ML, et al. The relationship between anterior tibial acceleration, tibial slope, and ACL strain during a simulated jump landing task. J Bone Joint Surg Am. 2011;93(14):1310–1317. doi: 10.2106/JBJS.J.00259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oh YK, Lipps DB, Ashton-Miller JA, Wojtys EM. What Strains the Anterior Cruciate Ligament During a Pivot Landing? Am J Sports Med. 2012 doi: 10.1177/0363546511432544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shao Q, MacLeod TD, Manal K, Buchanan TS. Estimation of ligament loading and anterior tibial translation in healthy and ACL-deficient knees during gait and the influence of increasing tibial slope using EMG-driven approach. Ann Biomed Eng. 2011;39(1):110–121. doi: 10.1007/s10439-010-0131-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shelburne KB, Kim HJ, Sterett WI, Pandy MG. Effect of posterior tibial slope on knee biomechanics during functional activity. J Orthop Res. 2011;29(2):223–231. doi: 10.1002/jor.21242. [DOI] [PubMed] [Google Scholar]
- 19.Simon RA, Everhart JS, Nagaraja HN, Chaudhari AM. A case-control study of anterior cruciate ligament volume, tibial plateau slopes and intercondylar notch dimensions in ACL-injured knees. J Biomech. 2010;43(9):1702–1707. doi: 10.1016/j.jbiomech.2010.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sonnery-Cottet B, Archbold P, Cucurulo T, et al. The influence of the tibial slope and the size of the intercondylar notch on rupture of the anterior cruciate ligament. J Bone Joint Surg Br. 2011;93(11):1475–1478. doi: 10.1302/0301-620X.93B11.26905. [DOI] [PubMed] [Google Scholar]
- 21.Stijak L, Herzog RF, Schai P. Is there an influence of the tibial slope of the lateral condyle on the ACL lesion? A case-control study. Knee Surg Sports Traumatol Arthrosc. 2008;16(2):112–117. doi: 10.1007/s00167-007-0438-1. [DOI] [PubMed] [Google Scholar]
- 22.Terauchi M, Hatayama K, Yanagisawa S, Saito K, Takagishi K. Sagittal alignment of the knee and its relationship to noncontact anterior cruciate ligament injuries. Am J Sports Med. 2011;39(5):1090–1094. doi: 10.1177/0363546510393305. [DOI] [PubMed] [Google Scholar]
- 23.Todd MS, Lalliss S, Garcia E, DeBerardino TM, Cameron KL. The relationship between posterior tibial slope and anterior cruciate ligament injuries. Am J Sports Med. 2010;38(1):63–67. doi: 10.1177/0363546509343198. [DOI] [PubMed] [Google Scholar]
- 24.Utzschneider S, Goettinger M, Weber P, et al. Development and validation of a new method for the radiologic measurement of the tibial slope. Knee Surg Sports Traumatol Arthrosc. 2011;19(10):1643–1648. doi: 10.1007/s00167-011-1414-3. [DOI] [PubMed] [Google Scholar]
- 25.Wordeman SC, Quatman CE, Kaeding CC, Hewett TE. In Vivo Evidence for Tibial Plateau Slope as a Risk Factor for Anterior Cruciate Ligament Injury: A Systematic Review and Meta-analysis. Am J Sports Med. 2012 Apr 26; doi: 10.1177/0363546512442307. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yoshioka Y, Siu DW, Scudamore RA, Cooke TD. Tibial anatomy and functional axes. J Orthop Res. 1989;7(1):132–137. doi: 10.1002/jor.1100070118. [DOI] [PubMed] [Google Scholar]