Abstract
Background
Children have better outcomes after out-of-hospital cardiac arrest (OHCA) than adults. However, little is known about the difference in outcomes between children and adults after OHCA due to drowning.
Objectives
The aim of this study is to assess the outcome after OHCA due to drowning between children and adults. Our hypothesis is that outcomes after OHCA due to drowning would be in better among children (<18 years old) compared with adults (≥18 years old).
Method
This prospective population-based, observational study included all emergency medical service-treated OHCA due to drowning in Osaka, Japan, between 1999 and 2010 (excluding 2004). Outcomes were evaluated between younger children (0–4 years old), older children (5–17 years old), and adults (≥18 years old). Major outcome measures were one-month survival and neurologically favorable one-month survival defined as cerebral performance category 1 or 2. Multivariate logistic regression analyses were used to account for potential confounders.
Results
During the study period, 66,716 OHCAs were documented, and resuscitation was attempted for 62,048 patients (1300 children [2%] and 60,748 adults [98%]). Among these OHCAs, 1737 (3% of OHCAs) were due to drowning (36 younger children [2%], 32 older children [2%], and 1669 adults [96%]). The odds of one-month survival were significantly higher for younger children (28% [10/36]; adjusted odds ratio [AOR], 20.20 [95% confidence interval {CI} 7.45–54.78]) and older children (9% [3/32]; AOR, 4.47 [95% CI 1.04–19.27]) when compared with adults (2% [28/1669]). However, younger children (6% [2/36]; AOR, 5.23 [95% CI 0.52–51.73]) and older children (3% [1/32]; AOR, 2.53 [95% CI 0.19–34.07]) did not have a higher odds of neurologically favorable outcome than adult s (1% [11/1669]).
Conclusion
In this large OHCA registry, children had better one-month survival rates after OHCA due to drowning compared with adults. Most survivors in all groups had unfavorable neurological outcomes.
Keywords: Out-of-hospital cardiac arrest, Drowning, Children, Adults
1. Introduction
Drowning is the third leading preventable cause of unintentional injury death worldwide, accounting for 0.7% of all deaths.1,2 Approximately 390,000 people in the world die from drowning and children < 5 years old have the highest drowning mortality rate.1 In Japan, almost 7000 people die from drowning annually and drowning is the second most common cause of injury deaths.3
Pediatric out-of-hospital cardiac arrests (OHCA) are more often due to respiratory causes rather than cardiac causes.4–6 Recently, several studies have shown that children are more likely to survive OHCA compared with adults.4,5,7 However, little is known about the differences in the outcomes between children and adults based on the type of OHCAs such as the non-cardiac etiology of drowning. Children with OHCA due to drowning might have better outcomes compared to adults because of unique age-dependent protective physiologic mechanisms such as the diving reflex and/or because of greater likelihood that children’s drowning would be witnessed.8–11
The Utstein Osaka Project, launched in 1998, is a large prospective population-based cohort study of OHCA in Osaka Prefecture, Japan, which covers approximately 8.8 million residents with 1.4 million children (<18 years old).5 From 1999 to 2010, there were approximately 1700 emergency medical service (EMS) treated OHCAs due to drowning. The aim of this study is to describe the characteristics and outcomes among these children and adults with OHCA due to drowning. We hypothesized that pediatric OHCA due to drowning would result in better outcome than adult OHCA.
2. Methods
2.1. Study design, setting, population in Osaka
This observational study enrolled all patients who suffered an OHCA due to drowning, were treated by EMS, and were transported to medical institutions in Osaka Prefecture from January 1, 1999 to December 31, 2010. If a patient had an OHCA due to drowning but had a pulse at EMS arrival, they were excluded because these patients were not treated by EMS. OHCA patients in 2004 were excluded from analysis because of differences in data collected that year which preclude appropriate comparisons. Osaka has an area of 1892 km2 including both urban and rural communities. The population of Osaka was 8,817,166, and 1,452,489 (16%) were < 18 years old in 2005.5,12 Cardiac arrest was defined as the cessation of cardiac mechanical activity confirmed by the absence of signs of circulation.13 In this cardiac arrest database, a witnessed cardiac arrest refers to one that is observed by another person. The arrest was presumed to be of cardiac etiology unless it was documented to be caused by trauma, drowning, drug overdose, foreign body asphyxia, exsanguination, or any other non-cardiac causes according to the Utstein-style international guidelines.13 These diagnoses were clinically determined by the physician in charge in collaboration with the EMS rescuers. The annual mean river water temperature is 17.2 °C and it ranges from 0.3 °C in winter to 37.0 °C in summer.14 The research protocol was approved by the institutional review board of Osaka University with the assent of the EMS authorities of the local governments in Osaka Prefecture.
2.2. Emergency medical service systems in Osaka
In Osaka Prefecture, there were 35 fire stations with emergency dispatch centers. The EMS system is operated by the local fire stations. The free telephone emergency number 119 is used to call for an ambulance from anywhere in Japan. Emergency services are provided 24 h each day, and are single-tiered in 33 stations and two-tiered in two stations. A two-tiered station uses medics followed by physicians. The most highly trained pre-hospital emergency care providers are the Emergency Life-Saving Technicians (ELSTs), who are authorized to insert an intravenous line and an adjunct airway, and to use a semi-automated external defibrillator for OHCA patients. Specially trained ELSTs were permitted to provide tracheal intubation for adults after July 2004 and to administer intravenous epinephrine for adults after April 2006.15 However, they were not permitted to provide tracheal intubation or intravenous epinephrine for children. The use of automated external defibrillator by citizens was legally approved in July 2004. All EMS providers performed and taught cardiopulmonary resuscitation (CPR) according to the Japanese CPR Guidelines which were based on the 2000 American Heart Association (AHA) Guidelines until September 2006, following which they used the 2005 AHA and the 2005 European Resuscitation Council (ERC) Guidelines.16–19 Do-not-resuscitate orders or living wills are not generally accepted in Japan and EMS providers are not permitted to terminate resuscitation in the field. Therefore, all patients with OHCA who were treated by EMS personnel were transported to a hospital and registered in this study. Details of the EMS system in Osaka were described previously.5,12,20
2.3. Data collection and quality control
Data were prospectively collected using a form that included all core data recommended in the Utstein-style reporting guidelines for cardiac arrests including age, gender, witness by EMS personnel or bystanders, first documented rhythm, location of the arrest, activity of daily living before the arrest, time-course of resuscitation, type of bystander-initiated CPR, return of spontaneous circulation (ROSC), hospital admission, one-month survival, and neurological status one-month after the event.13,21 A series of EMS times were recorded automatically at the dispatch center including: call receipt, vehicle arrival at the scene, contact with patient, initiation of CPR, defibrillation by EMS, and hospital arrival. The initiation of bystander CPR was obtained by EMS interview with the bystander before leaving the scene. Both bystander-initiated chest compression-only CPR and conventional CPR with compressions and rescue breathing were considered as bystander CPR. The time of defibrillation was recorded in the semi-automated defibrillator. Defibrillators were synchronized with the clock at their dispatch center, as were other relevant EMS time devices (e.g., clocks, watches).
The data form was filled out by the EMS personnel, transferred to the Information Center for Emergency Medical Services of Osaka, and then checked by the investigators. The EMS personnel collaborate with supervising physician for abstraction of Utstein elements. If the data sheet was incomplete, the relevant EMS personnel were contacted and questioned, and the data sheet was completed. All survivors were followed for up to one-month after the event by the EMS personnel and investigators with the cooperation of the Osaka Medical Association and relevant local medical institutions.
2.4. Study endpoints
The major endpoints were one-month survival and favorable neurological outcome one-month after cardiac arrest, prospectively defined as CPC 1 or 2. Neurological outcome was assessed by the Glasgow–Pittsburgh cerebral performance category (CPC) scale. The CPC 1 is good performance; CPC 2, moderate disability; CPC 3, severe cerebral disability; CPC 4, coma/vegetative state; and CPC 5, death.13,21 Secondary outcome measures included ROSC and hospital admission.
2.5. Statistical analysis
Patient characteristics and outcomes were evaluated between younger children (0–4 years old), older children (5–17 years old), and adults (≥18 years old) suffering OHCA due to drowning. Continuous variables were evaluated by Kruskal–Wallis test and categorical variables by chi-square test or Fisher’s exact test. Multiple logistic regression analysis was used to control for covariates potentially confounding the relationship between age groups and outcomes. Potential confounding factors based on biological plausibility and previous studies were included in the multivariable analysis. A priori confounders introduced into the regression model were age, gender, location of arrests, activity of daily living before arrests, witnessed status, bystander CPR status, first documented rhythm, and time interval from call to the initiation of CPR by EMS personnel. Odds ratios (ORs) and their 95% confidence intervals (CIs) were calculated. All of the tests were 2-tailed and a p value of <0.05 was considered statistically significant. All statistical analyses were performed using SPSS statistical package ver19.0J (SPSS, IBM Corporation).
3. Results
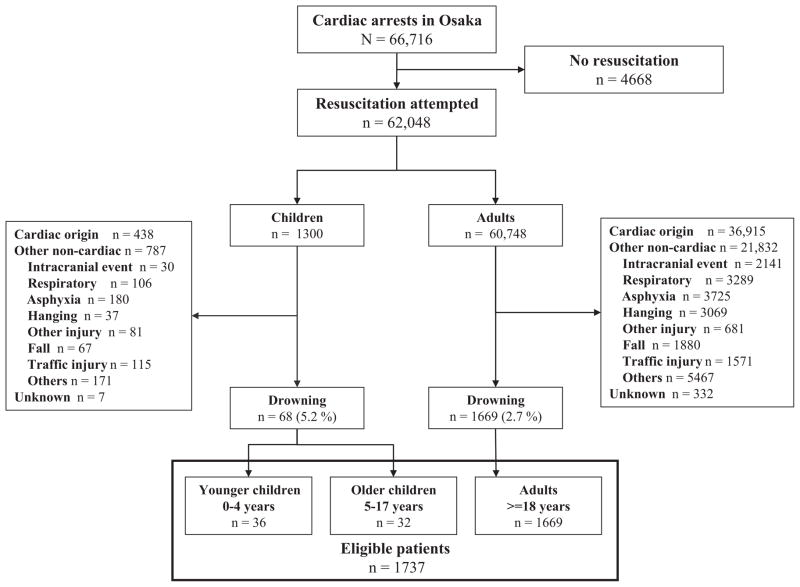
Fig. 1 shows an overview of the study patients based on an abridged Utstein template. During these 11 years, a total of 66,716 OHCAs were documented and resuscitation was attempted by EMS in 62,048. Among 1300 pediatric OHCA victims, 68 (5.2%) had the cause of drowning, 438 (33.6%) cardiac origin, 787 (60.5%) other non-cardiac origin, and 7 (0.5%) unknown origin, respectively. Of 68 pediatric drowning victims, 36 were younger children (0–4 years) and 32 were older children (5–17 years). Among 60,748 adult victims, 1669 (2.7%) had the cause of drowning, 36915 (60.7%) cardiac origin, 21832 (35.9%) other non-cardiac origin, and 332 (0.5%) unknown origin, respectively. A total of 1737 were eligible patients for our analyses. We could not obtain data on one-month survival and neurologic outcome for one adult in these eligible victims.
Fig. 1.
Overview of EMS-treated cardiac arrests with an abridged Utstein template from January 1, 1999 to December 31.
The characteristics of the patients with OHCA due to drowning are presented in Table 1. The median age in younger children, older children, and adults were 2, 11, and 77 years, respectively. The proportion of males was higher among children than adults. Older children with OHCA due to drowning were less likely to have their arrests at home, and both younger and older children were more likely to receive bystander CPR. The proportions of witnessed, ventricular fibrillation as first documented rhythm, and good activity of daily living before arrests were not different between children and adults. The time intervals from call to EMS contact with patients and from call to CPR by EMS and to hospital arrival were longer for older children than other age groups.
Table 1.
Patient and EMS chracteristics of out-of-hospital cardiac arrest due to drowning by age group.
| Total | Younger children | Older children | Adults | p value | |
|---|---|---|---|---|---|
| 0–4 years | 5–17 years | ≥18 years | |||
| (N = 1737) | (N = 36) | (N = 32) | (N = 1669) | ||
| Age, year, median (IQR) | 76 (65–84) | 2 (1–2) | 11 (6–14) | 77 (67–84) | <0.001 |
| Male, n (%) | 867 (49.9) | 24 (66.7) | 28 (87.5) | 815 (48.8) | <0.001 |
| Witnessed, n (%) | 138 (7.9) | 3 (8.3) | 6 (18.8) | 129 (7.7) | 0.073 |
| VF as first documented rhythm, n (%) | 29 (1.7) | 0 (0) | 1 (3.1) | 28 (1.7) | 0.477 |
| Homes, n (%) | 1150 (66.2) | 28 (77.8) | 9 (28.1) | 1113 (66.7) | <0.001 |
| Good activity of daily living before arrests, n (%) | 1399 (80.5) | 33 (91.7) | 29 (90.6) | 1337 (80.1) | 0.077 |
| Bystander-initiated CPR, n (%) | |||||
| No CPR | 1035 (59.6) | 18 (50.0) | 16 (50.0) | 1001 (60.0) | |
| Compresion-only CPR | 349 (20.1) | 1 (2.8) | 5 (15.6) | 343 (20.6) | |
| Conventional CPR | 336 (19.3) | 17 (47.2) | 9 (28.1) | 310 (18.6) | |
| Call to contact with patients (EMS response time), min, median (IQR) | 7 (5–9) | 7 (5–8) | 9 (6–21) | 7 (5–9) | 0.012 |
| Call to CPR by EMS personnel, min, median (IQR) | 8 (6–10) | 7 (5–8) | 9 (6–21) | 8 (6–10) | 0.007 |
| Call to hospital arrival, min, median (IQR) | 26 (20–31) | 22 (17–31) | 32 (26–39) | 26 (20–31) | 0.001 |
EMS indicates emergency medical service; CPR, cardiopulmonary resuscitation; VF, ventricular fibrillation; IQR, interquartile range.
Outcomes from OHCA due to drowning are shown in Table 2. When comparing younger children, older children, and adults, rates of ROSC (52.8% vs. 28.1% vs. 15.4%, p < 0.001), survival to hospital admission (52.8% vs. 28.1% vs. 12.5%, p < 0.001), one-month survival (27.8% vs. 9.4% vs. 1.7%, p < 0.001), and neurologically favorable outcome (5.6% vs. 3.1% vs. 0.7%, p = 0.015) significantly differed. Younger children were more likely to achieve ROSC and survive to hospital admission than older children (p = 0.039), but there was no difference in one-month survival (p = 0.054) or neurologically favorable outcome (p = 1.000).
Table 2.
Outcomes from out-of-hospital cardiac arrest due to drowning by age agroup.
| Total | Younger children | Older children | Adults | p value | |
|---|---|---|---|---|---|
| 0–4 years | 5–17 years | ≥18 years | |||
| (N = 1737) | (N = 36) | (N = 32) | (N = 1669) | ||
| ROSC, n (%) | 285 (16.4) | 19 (52.8) | 9 (28.1) | 257 (15.4) | <0.001 |
| Hospital admission, n (%) | 236 (13.6) | 19 (52.8) | 9 (28.1) | 208 (12.5) | <0.001 |
| One-month survival, n (%) | 41 (2.4) | 10 (27.8) | 3 (9.4) | 28 (1.7) | <0.001 |
| Neurologically favorable outcome, n (%) | 14 (0.8) | 2 (5.6) | 1 (3.1) | 11 (0.7) | 0.015 |
ROSC indicates return of spontaneous circulation.
Table 3 shows factors contributing to both one-month survival and neurologically favorable one-month survival. Compared to adults, after controlling for a priori and other potential confounders, the odds of one-month survival was significantly higher for younger children (adjusted ORs, 20.20 [95% CI 7.45–54.78]) and older children (adjusted ORs, 4.47 [95% CI 1.04–19.27]). There was no a difference in adjusted odds of one-month survival beween older and younger children (p = 0.546). After adjustment for potentially confounding factors, there was no difference in one-month favorable neurological outcome between adults and younger children (adjusted ORs, 5.23 [95% CI 0.52–51.73]) and adults and older children (2.53 [0.19–34.07]). Witnessed status was significantly associated with one-month survival and favorable neurologic outcome, whereas initial rhythm of ventricular fibrillation was only associated with favorable neurologic outcome.
Table 3.
Factors contributing to outcomes from out-of-hospital cardiac arrest due to drowning by age group.
| One-month survival
|
Neurologically favorable one-month survival
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted OR | (95% CI) | Adjusted OR | (95% CI) | Unadjusted OR | (95% CI) | Adjusted OR | (95% CI) | |
| Age group | ||||||||
| Younger children (0–4 years) | 22.54 | (9.93–51.15) | 20.20 | (7.45–54.78) | 8.86 | (1.89–41.52) | 5.23 | (0.53–51.73) |
| Older children (5–17 years) | 6.06 | (1.74–21.08) | 4.47 | (1.04–19.27) | 4.86 | (0.61–38.81) | 2.53 | (0.19–34.07) |
| Adults (≥18 years) | Reference | Reference | Reference | Reference | ||||
| Male | 1.76 | (0.92–3.34) | 1.23 | (0.58–2.62) | 1.81 | (0.60–5.42) | 1.05 | (0.26–4.26) |
| Witnessed | 7.38 | (3.81–14.30) | 6.50 | (2.81–15.02) | 16.33 | (5.58–47.77) | 11.80 | (2.84–49.08) |
| VF as first documented rhythm | 5.47 | (1.58–18.91) | 2.90 | (0.59–14.33) | 19.41 | (5.05–74.65) | 11.38 | (1.83–70.76) |
| Homes | 0.35 | (0.19–0.66) | 0.42 | (0.19–0.96) | 0.14 | (0.04–0.49) | 0.26 | (0.05–1.22) |
| Good activity of daily living | 1.00 | (0.46–2.18) | 1.33 | (0.50–3.51) | 0.89 | (0.25–3.19) | 1.33 | (0.23–7.64) |
| Bystander-initiated CPR | ||||||||
| No CPR | Reference | Reference | Reference | Reference | ||||
| Chest compression-only CPR | 0.37 | (0.11–1.22) | 0.57 | (0.16–2.00) | 0.37 | (0.05–2.96) | 0.51 | (0.05–4.97) |
| Conventional CPR with rescue breathing | 1.83 | (0.94–3.58) | 1.87 | (0.83–4.20) | 1.94 | (0.63–5.96) | 2.35 | (0.52–10.62) |
| Call to CPR by EMS (for 1-min increase in time) | 1.01 | (0.97–1.05) | 0.97 | (0.92–1.02) | 1.00 | (0.92–1.08) | 0.87 | (0.73–1.03) |
VF indicates ventricular fibrillation; CPR, cardiopulmonary resuscitation; EMS, emergency medical service; OR, odds ratio; CI, confidence interval.
4. Discussion
From this large prospective registry of OHCAs, we report the epidemiology and outcomes of OHCA due to drowning in children and adults from January 1999 through December 2010. Among 62,048 patients who suffered a cardiac arrest at EMS arrival and were treated by EMS, drowning was the cause in 1737 (3%) and most of the drowning victims were adults (1669 vs. 68). Children were much more likely to survive to one-month after OHCA due to drowning than adults. Disappointingly, only 34% (14/41) of the survivors had favorable neurological outcomes at one-month. For both children and adults, outcomes were better when the arrest was witnessed22 and the initial rhythm was ventricular fibrillation. Thus, early rhythm detection may improve outcomes for selected drowning OHCA victims.
In the Utstein Osaka registry of OHCA, drowning is a relatively uncommon cause of OHCA. Nevertheless, 1737 OHCAs due to drowning over 12 years is a major public health problem in Osaka. For example, drowning-associated OHCA is the fourth leading cause of death among all injury patients for adults and third leading cause for children in Japan.23 In addition, this database likely underestimates the good outcomes following OHCAs due to drowning because it excludes patients who attained ROSC prior to EMS arrival. Experimental and clinical studies show that the patients who have prompt bystander CPR often have ROSC prior to EMS arrival, and that these patients are the ones most likely to have excellent long-term neurological outcomes.24–30
In our study, survival outcomes are much better among children than adults with 28% (10/36) of younger children and 9% (3/32) of older children surviving one-month post-cardiac arrest vs. 2% of adults (28/1669). Previous studies have also showed that children suffering from OHCAs had better outcomes than adults,4,5,7 but our large database allows us to specifically address the outcomes after drowning-associated OHCAs.
Why was the survival rate so much higher among children? Children with OHCA due to drowning might have better outcomes because of unique age-dependent protective physiologic mechanisms such as the diving reflex.2,8–11 In addition, we speculated that children’s better drowning-associated OHCA outcomes were related to more pediatric drowning-associated OHCAs being witnessed, thereby providing a greater opportunity for effective bystander CPR to be performed. Although the raw numbers are consistent with these expectations, we were not able to demonstrate statistically significant differences. Importantly, children were more likely to receive bystander CPR (especially conventional CPR with rescue breathing). The advantage of conventional CPR with rescue breathing for OHCA of non-cardiac origin has been previously reported.2,6 We also speculate that perhaps other co-morbidities contributed to worse outcomes among adults, including underlying coronary artery disease.31 We also speculate that medical care providers may have been more aggressive in maintaining potential life-sustaining interventions for children compared with adults. This speculation is supported in part by our data that 77% (10/13) of the children who survived for one-month had unfavorable neurological outcomes compared with 61% of adults (17/28).
The overall outcomes after OHCA due to drowning were poor. Less than 1% survived with favorable neurological outcome at one-month post-arrest. The outcomes in this study were worse than those in previous OHCA drowning reports from other countries,32,33 and outcomes from non-drowning witnessed adult OHCA in Osaka (3.4% neurological favorable outcome).34 Factors that may have contributed to worse outcomes in this study could be the older age of this cohort, the high frequency of arrests were at home, the frequency of unwitnessed by bystanders, the high frequency of compression-only CPR and that EMS was not allowed to stop CPR.32,33,35–37 Note that in Japan, older people often have a tradition of taking a deep hot bath alone daily. This practice is known to be associated with bathing syncope, especially among the elderly, and may contribute to the relatively higher frequency OHCA due to drowning among adults in Japan, and the relatively poor outcome.38–40
Although VF was the first documented rhythm in < 2% of these drowning-associated OHCAs, it is important to note that the odds of survival with favorable neurological outcome was much higher when VF was the first documented rhythm. Because VF is so uncommon as the initial rhythm in OHCA due to drowning2,32,33, providers may focus on chest compressions and rescue breathing, and may only consider rhythm detection later during the resuscitative efforts. However, cardiopulmonary resuscitation without defibrillation is futile for patients in VF, and outcomes from VF are very sensitive to the time-to-defibrillation.18 Therefore, when able, providers should include early rhythm detection and prompt defibrillation for VF.
This observational study has some inherent limitations. First, we obtained data on OHCA patients based on the Utstein reporting template for cardiac arrest13,21 rather than the Utstein template for drowning because this is a cardiac arrest study.41 Second, our data do not address prehospital factors such as drowning duration, time, and water temparature as well as in-hospital factors such as body core temperature and blood pH, as recommended in the Utstein reporting guidelines for drowning. In preceding studies, the effectiveness of advanced life support treatments such as cardiopulmonary bypass42 and extra-corporeal membrane oxygenation43 for OHCA due to drowning has been discussed, but these data were not available for this study. Third, favorable neurological outcome was based on the Cerebral Performance Scale rather than more detailed functional neurological assessments. Finally, as with all epidemiological studies, data integrity, validity, and ascertainment are potential limitations. The use of uniform data collection based on Ustsein-style guidelines for reportiong cardiac arrest, population-based design and large sample size was intended to mimimize these potential sourses of bias.
5. Conclusions
From a large registry of OHCA in Osaka, we report the epidemiology and outcomes of OHCA due to drowning among children and adults. Survival one-month post-cardiac arrest was more common among children compared with adults. However, most survivors in all groups had unfavorable neurological outcomes. Thus, major public health initiatives to prevent drowning deserve a high priority.
Acknowledgments
We are grateful to Hiroshi Morita, Masanao Kobayashi, Hiroshi Tamai and Naohisa Kawamura for the support. We are grateful to Naoki Shimizu, Kunio Ohta and the other members of Japanese Pediatric Resuscitation Study (PResS) group for the advice and expertise. We greatly appreciate Hisashi Ikeuchi, Hidekazu Yukioka, Hisashi Sugimoto, Toshifumi Uejima, Kikushi Katsurada, Masafumi Kishimoto, Chizuka Shiokawa, Akihiko Hirakawa, Tokihiko Yamamoto, Hiroshi Rinka, Kentaro Kajino, Yasuo Ohishi, Ryusuke Kawaguchi, Kazuhisa Okuda, Hiroyuki Yokoyama, Tomohiko Sakai, Kayo Tanigawa, Sumito Hayashida, Yasuyuki Matsui, Kenichi Matsumura, and the other members of the Utstein Osaka Project for their contribution in organization, coordination, and oversight as steering committee. We are also deeply indebted to the all of the EMS personnel and concerned physicians in Osaka Prefecture, and the Osaka Medical Association for their indispensable cooperation and support.
Footnotes
A Spanish translated version of the abstract of this article appears as Appendix in the final online version at http://dx.doi.org/10.1016/j.resuscitation.2012.08.336.
Conflict of interest
There are no conflicts of interest to declare.
Role of funding source
None.
References
- 1. [accessed October 2012];World Health Organization Drowning Fact Sheet No. 347. 2012 Available at: http://www.who.int/mediacentre/factsheets/fs347/en/index.html.
- 2.Szpilman D, Bierens JJ, Handley AJ, Orlowski JP. Drowning. N Engl J Med. 2012;366:2102–10. doi: 10.1056/NEJMra1013317. [DOI] [PubMed] [Google Scholar]
- 3.Ikeda K, Nadaoka Y, Kamiya N. Precise analysis of accidental deaths in Japan. Ann Rep Tokyo Metr Inst Pub Health. 2010;61:373–9. [in Japanese] [Google Scholar]
- 4.Atkins DL, Everson-Stewart S, Sears GK, et al. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Circulation. 2009;119:1484–91. doi: 10.1161/CIRCULATIONAHA.108.802678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nitta M, Iwami T, Kitamura T, et al. Age-specific differences in outcomes after out-of-hospital cardiac arrests. Pediatrics. 2011;128:e812–20. doi: 10.1542/peds.2010-3886. [DOI] [PubMed] [Google Scholar]
- 6.Kitamura T, Iwami T, Kawamura T, et al. Conventional and chest-compression-only cardiopulmonary resuscitation by bystanders for children who have out-of-hospital cardiac arrests: a prospective, nationwide, population-based cohort study. Lancet. 2010;375:1347–54. doi: 10.1016/S0140-6736(10)60064-5. [DOI] [PubMed] [Google Scholar]
- 7.Kitamura T, Iwami T, Kawamura T, et al. Nationwide improvements in survival from out-of-hospital cardiac arrest in Japan. Circulation. 2012;126:2834–43. doi: 10.1161/CIRCULATIONAHA.112.109496. [DOI] [PubMed] [Google Scholar]
- 8.Orlowski JP. Prognostic factors in pediatric cases of drowning and near-drowning. JACEP. 1979;8:176–9. doi: 10.1016/s0361-1124(79)80121-5. [DOI] [PubMed] [Google Scholar]
- 9.Golden FS, Tipton MJ, Scott RC. Immersion, near-drowning and drowning. Br J Anaesth. 1997;79:214–25. doi: 10.1093/bja/79.2.214. [DOI] [PubMed] [Google Scholar]
- 10.Layon AJ, Modell JH. Drowning: update 2009. Anesthesiology. 2009;110:1390–401. doi: 10.1097/ALN.0b013e3181a4c3b8. [DOI] [PubMed] [Google Scholar]
- 11.Tipton MJ, Golden FS. A proposed decision-making guide for the search, rescue and resuscitation of submersion (head under) victims based on expert opinion. Resuscitation. 2011;82:819–24. doi: 10.1016/j.resuscitation.2011.02.021. [DOI] [PubMed] [Google Scholar]
- 12.Iwami T, Hiraide A, Nakanishi N, et al. Age and sex analyses of out-of-hospital cardiac arrest in Osaka, Japan. Resuscitation. 2003;57:145–52. doi: 10.1016/s0300-9572(03)00035-2. [DOI] [PubMed] [Google Scholar]
- 13.Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries. A statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, Inter American Heart Foundation, Resuscitation Council of Southern Africa) Resuscitation. 2004;63:233–49. doi: 10.1016/j.resuscitation.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 14.Osaka prefectural government office. [Accessed 31.05.13];River water temperature in Osaka. 2008 [in Japanese]. Available at: http://www.pref.osaka.jp/attach/5078/00103345/5-5%20H20.12.1.pdf.
- 15.Tanigawa K, Tanaka K. Emergency medical service systems in Japan: past, present, and future. Resuscitation. 2006;69:365–70. doi: 10.1016/j.resuscitation.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 16.The American Heart Association in Collaboration With the International Liaison Committee on Resuscitation (ILCOR) Guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care: international consensus on science. Circulation. 2000;102:A3–A4. I1–I384. [PubMed] [Google Scholar]
- 17.Proceedings of the 2005 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2005;67:157–341. [PubMed] [Google Scholar]
- 18.ECC Committee, Subcommittees, Task Forces of the American Heart Association. 2005 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2005;112:IV1–203. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 19.European Resuscitation Council. European Resuscitation Council guidelines for resuscitation 2005. Resuscitation. 2005;67(Suppl 1):S1–189. doi: 10.1016/j.resuscitation.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 20.Iwami T, Kawamura T, Hiraide A, et al. Effectiveness of bystander-initiated cardiac-only resuscitation for patients with out-of-hospital cardiac arrest. Circulation. 2007;116:2900–7. doi: 10.1161/CIRCULATIONAHA.107.723411. [DOI] [PubMed] [Google Scholar]
- 21.Cummins RO, Chamberlain DA, Abramson NS, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein Style. A statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation. 1991;84:960–75. doi: 10.1161/01.cir.84.2.960. [DOI] [PubMed] [Google Scholar]
- 22.Youn CS, Choi SP, Yim HW, Park KN. Out-of-hospital cardiac arrest due to drowning: an Utstein Style report of 10 years of experience from St. Mary’s Hospital Resuscitation. 2009;80:778–83. doi: 10.1016/j.resuscitation.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 23.The Ministry of Health Labour and Welfare of Japan. [Accessed 07.01.13];2010 Vital Statistics of Japan. 2013 [in Japanese]. Available at: http://www.mhlw.go.jp/toukei/saikin/hw/jinkou/kakutei10/dl/11h7.pdf.
- 24.Hickey RW, Cohen DM, Strausbaugh S, Dietrich AM. Pediatric patients requiring CPR in the prehospital setting. Ann Emerg Med. 1995;25:495–501. doi: 10.1016/s0196-0644(95)70265-2. [DOI] [PubMed] [Google Scholar]
- 25.Berg RA, Hilwig RW, Kern KB, Babar I, Ewy GA. Simulated mouth-to-mouth ventilation and chest compressions (bystander cardiopulmonary resuscitation) improves outcome in a swine model of prehospital pediatric asphyxial cardiac arrest. Crit Care Med. 1999;27:1893–9. doi: 10.1097/00003246-199909000-00030. [DOI] [PubMed] [Google Scholar]
- 26.Sirbaugh PE, Pepe PE, Shook JE, et al. A prospective, population-based study of the demographics, epidemiology, management, and outcome of out-of-hospital pediatric cardiopulmonary arrest. Ann Emerg Med. 1999;33:174–84. doi: 10.1016/s0196-0644(99)70391-4. [DOI] [PubMed] [Google Scholar]
- 27.Berg RA, Hilwig RW, Kern KB, Ewy GA. “Bystander” chest compressions and assisted ventilation independently improve outcome from piglet asphyxial pulseless “cardiac arrest”. Circulation. 2000;101:1743–8. doi: 10.1161/01.cir.101.14.1743. [DOI] [PubMed] [Google Scholar]
- 28.Venema AM, Groothoff JW, Bierens JJ. The role of bystanders during rescue and resuscitation of drowning victims. Resuscitation. 2010;81:434–9. doi: 10.1016/j.resuscitation.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 29.Suominen PK, Vahatalo R. Neurologic long term outcome after drowning in children. Scand J Trauma Resusc Emerg Med. 2012;20:55. doi: 10.1186/1757-7241-20-55. http://dx.doi.org/10.1186/1757-7241-20-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Topjian AA, Berg RA, Bierens JJ, et al. Brain resuscitation in the drowning victim. Neurocrit Care. 2012;17:441–67. doi: 10.1007/s12028-012-9747-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Claesson A, Druid H, Lindqvist J, Herlitz J. Cardiac disease and probable intent after drowning. Am J Emerg Med. 2013 doi: 10.1016/j.ajem.2013.04.004. (e-pub ahead of print) [DOI] [PubMed] [Google Scholar]
- 32.Claesson A, Svensson L, Silfverstolpe J, Herlitz J. Characteristics and outcome among patients suffering out-of-hospital cardiac arrest due to drowning. Resuscitation. 2008;76:381–7. doi: 10.1016/j.resuscitation.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 33.Grmec S, Strnad M, Podgorsek D. Comparison of the characteristics and outcome among patients suffering from out-of-hospital primary cardiac arrest and drowning victims in cardiac arrest. Int J Emerg Med. 2009;2:7–12. doi: 10.1007/s12245-009-0084-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Iwami T, Nichol G, Hiraide A, et al. Continuous improvements in “chain of survival” increased survival after out-of-hospital cardiac arrests: a large-scale population-based study. Circulation. 2009;119:728–34. doi: 10.1161/CIRCULATIONAHA.108.802058. [DOI] [PubMed] [Google Scholar]
- 35.Quan L, Kinder D. Pediatric submersions: prehospital predictors of outcome. Pediatrics. 1992;90:909–13. [PubMed] [Google Scholar]
- 36.Quan L, Cummings P. Characteristics of drowning by different age groups. Inj Prev J Inter Soc Child Adol Inj Prev. 2003;9:163–8. doi: 10.1136/ip.9.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dyson K, Morgans A, Bray J, Matthews B, Smith K. Drowning related out-of-hospital cardiac arrests: characteristics and outcomes. Resuscitation. 2013 doi: 10.1016/j.resuscitation.2013.01.020. E-pub ahead of print. [DOI] [PubMed] [Google Scholar]
- 38.Nagasawa Y, Komori S, Sato M, et al. Effects of hot bath immersion on autonomic activity and hemodynamics: comparison of the elderly patient and the healthy young. Jpn Circ J. 2001;65:587–92. doi: 10.1253/jcj.65.587. [DOI] [PubMed] [Google Scholar]
- 39.Nishiyama C, Iwami T, Nichol G, et al. Association of out-of-hospital cardiac arrest with prior activity and ambient temperature. Resuscitation. 2011;82:1008–12. doi: 10.1016/j.resuscitation.2011.03.035. [DOI] [PubMed] [Google Scholar]
- 40.Abe H, Kohno R, Oginosawa Y. Reflex syncope during a hot bath as a specific cause of drowning in Japan. J Arrhyth. 2013;29:37–8. [Google Scholar]
- 41.Idris AH, Berg RA, Bierens J, et al. Recommended guidelines for uniform reporting of data from drowning: the “Utstein style”. Resuscitation. 2003;59:45–57. doi: 10.1016/j.resuscitation.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 42.Suominen PK, Vallila NH, Hartikainen LM, et al. Outcome of drowned hypothermic children with cardiac arrest treated with cardiopulmonary bypass. Acta Anaesthesiol Scand. 2010;54:1276–81. doi: 10.1111/j.1399-6576.2010.02307.x. [DOI] [PubMed] [Google Scholar]
- 43.Wanscher M, Agersnap L, Ravn J, et al. Outcome of accidental hypothermia with or without circulatory arrest: experience from the Danish Praesto Fjord boating accident. Resuscitation. 2012;83:1078–84. doi: 10.1016/j.resuscitation.2012.05.009. [DOI] [PubMed] [Google Scholar]