Abstract
AIM: To determine whether a communication instrument provided to patients prior to their primary care physician (PCP) visit initiates a conversation with their PCP about colorectal cancer screening (CRC-S), impacting screening referral rates in fully insured and underinsured patients.
METHODS: A prospective randomized control study was performed at a single academic center outpatient internal medicine (IRMC, underinsured) and family medicine (FMRC, insured) resident clinics prior to scheduled visits. In the intervention group, a pamphlet about the benefit of CRC-S and a reminder card were given to patients before the scheduled visit for prompting of CRC-S referral by their PCP. The main outcome measured was frequency of CRC-S referral in each clinic after intervention.
RESULTS: In the IRMC, 148 patients participated, a control group of 72 patients (40F and 32M) and 76 patients (48F and 28M) in the intervention group. Referrals for CRC-S occurred in 45/72 (63%) of control vs 70/76 (92%) in the intervention group (P ≤ 0.001). In the FMRC, 126 patients participated, 66 (39F:27M) control and 60 (33F:27M) in the intervention group. CRC-S referrals occurred in 47/66 (71%) of controls vs 56/60 (98%) in the intervention group (P ≤ 0.001).
CONCLUSION: Patient initiated physician prompting produced a significant referral increase for CRC-S in underinsured and insured patient populations. Additional investigation aimed at increasing CRC-S acceptance is warranted.
Keywords: Colon cancer, Screening, Primary care, Physician patient relationship, Referral
Core tip: Colon cancer screening only performed in approximately 60% of Americans over 50 years old. Inadequate communication between patient and physician is a significant obstacle to obtaining appropriate screening, especially in the underinsured population. Patient initiated prompting of their primary care physician for colorectal cancer screening with colonoscopy increased referrals in both underinsured and insured patient groups.
INTRODUCTION
In spite of the available evidence suggesting effectiveness of colorectal cancer screening (CRC-S), approximately 50% of the United States population over 50 years old has not had CRC-S[1]. According to the National Cancer Institute, in 2009 the estimated new cases of colon cancer and rectal cancer in United States were 106100 and 40870 respectively. The estimated death of these combined cancers was 49920 (www.cancer.gov). Several studies have been conducted to understand the barriers for colorectal screening[2]. Inadequate communication between the primary care physician (PCP) and patient, including lack of a physician’s recommendation for testing and patients unawareness were found to be important barriers[2-4]. Other investigators have shown colonoscopy as a safe and feasible primary screening test[5]. In addition, studies have also shown that in average risk patients, colonoscopy screening found 0.5%-1.0% have colon cancers and 5%-10% have advanced neoplasia that can be removed during the screening[5-9]. Providing educational material and a method for the patient to express interest in CRC-S to their PCP could increase referral for this screening. The aim of our study was to determine if patient initiated prompting of their PCP for CRC-S would increase referrals in both underinsured and insured patients.
MATERIALS AND METHODS
From November 2008 to November 2010, all patients seen in Family Medicine Resident Clinic (FMRC, insured) and Internal Medicine Resident Clinic (IMRC, underinsured) waiting areas were screened for CRC-S eligibility. Those patients meeting criteria for screening but never having been screened previously were considered eligible for the study. Eligible patients were assigned randomly to either a control or intervention group. Intervention consisted of a pamphlet describing the benefit of CRC-S, given to patients prior to their PCP visit and a reminder note about CRC screening to be given to their physician during the encounter. The pamphlet discussed colon cancer incidence, frequency, deaths, prevention, need for screening, risk factors, symptoms, available screening methods with colonoscopy preferred based on ACG guidelines. In order to not reveal the purpose of our study to resident physicians, patients were randomly assigned as control group or intervention group on different clinic days. Since, each resident physician only see patients on one specific day of clinic, and by randomizing patients on the same day will allow the physicians to figure out our study if he received a reminder note on one patient and not the other. A two-page questionnaire was designed to assess the referral patterns and preferred screening method for CRC. Questions on the survey included demographic parameters (age, race, gender, and education level), whether their PCP had referred them for CRC-S, the screening method recommended, whether the participants accepted the screening referral, presence of insurance coverage for CRC-S, and knowledge that CRC could be prevented using screening. Upon completion of the study, all patients in the control group were given the CRC-S pamphlet for use.
The primary outcome was to determine if patient-initiated prompting for CRC-S of their primary care physicians increased CRC-S referrals. We wanted to determine if a communication instrument provided to patients initiated a conversation with their primary care physicians about CRC screening, especially via colonoscopy. The secondary outcome was to determine whether differences exist in regard to patient-physician communication patterns about screening among residents and faculty in the general internal medicine and family practice clinics. We were also interested in the method of CRC-S given to the patients and the overall acceptance rates for CRC-S among patients.
Statistical analysis
The minimum sample size required to detect a referral frequency difference of 25% after patient initiated prompting was calculated using a confidence level of 95% and confidence interval of 5%. The sample size needed for each group was 52 patients. Differences between groups were analyzed using the unpaired Student’s t-test for normally distributed data or the Mann-Whitney U test for skewed data. The χ2 test was used for comparisons of categorical variables. Multivariate analysis using stepwise logistic regression was performed to identify independent factors associated with CRC-S referral. All statistical analysis was done using SAS software (v 9.1.3, SAS Institute, Cary, NC). All statistical tests were carried out at an alpha of 0.05.
RESULTS
A total of 274 patients were included from both clinic sites in the present investigation. One hundred forty eight (148) patients were seen in the IMRC and 126 were seen in the FRMC (Figure 1). Among the IRMC patients, 72 (40F:32M) were in the control group and 76 (48F:28M) in the intervention group. In the FRMC patients, 66 (39F:27M) were in the control group and 60 (33F:27M) in the intervention group. No differences were observed in baseline parameters of control or intervention groups from either of the 2 clinics (Table 1). Patient initiated prompting of PCP (intervention) resulted in a significant referral increase for CRC-S in both underinsured and insured patient populations. In the IMRC, 63% in the control group (45/72) got referrals for CRC-S vs 92% in the intervention group (70/76, P ≤ 0.001, Figure 2A). In the FMRC, 47/66 (71%) in the control group were referred for CRC-S vs 56/60 (98%) in the intervention group (P ≤ 0.001, Figure 2B).
Figure 1.

Patient distribution in both clinics between intervention and control groups. A: Internal medicine resident clinic (underinsured); B: Family medicine resident clinic (insured).
Table 1.
Patients characteristics
| Characteristics |
IMRC |
P value |
FMRC |
P value | ||
| Control group | Intervention group | Control group | Intervention group | |||
| Number of patients | 72 | 76 | NS | 66 | 60 | NS |
| Median age (range), yr | 54 (51-64) | 56 (49-70) | 55 (48-68) | 54 (47-66) | ||
| Sex | ||||||
| Male | 32 | 28 | 27 | 27 | ||
| Female | 40 | 48 | 39 | 33 | ||
| Ethnicity | ||||||
| Non-hispanic white | 35 | 45 | 30 | 32 | ||
| African American | 26 | 24 | 25 | 19 | ||
| Others | 9 | 9 | 11 | 9 | ||
| Health Insurance | ||||||
| Yes | 12 | 19 | 66 | 60 | ||
| No | 60 | 57 | 0 | 0 | ||
| Education | ||||||
| < High school graduate | 12 | 25 | 7 | 5 | ||
| High school graduate | 54 | 41 | 29 | 31 | ||
| College graduate | 6 | 10 | 30 | 24 | ||
| Past medical history | ||||||
| Hypertension | 56 | 60 | 51 | 37 | ||
| Diabetes mellitus | 31 | 26 | 25 | 21 | ||
| Heart disease | 4 | 7 | 5 | 5 | ||
| Liver disease | 6 | 6 | 5 | 3 | ||
| None | 12 | 6 | 3 | 9 | ||
| Alarm symptoms | ||||||
| Yes | 20 | 33 | 28 | 26 | ||
| No | 52 | 43 | 38 | 34 | ||
| Family history of CRC | ||||||
| Yes | 11 | 4 | 12 | 7 | ||
| No | 61 | 72 | 54 | 52 | ||
| Had a colonoscopy | ||||||
| Yes | 6 | 11 | 9 | 8 | ||
| No | 66 | 65 | 57 | 52 | ||
| Knowledge of CRC recommendations | ||||||
| Yes | 14 | 26 | 36 | 38 | ||
| No | 58 | 50 | 30 | 22 | ||
| Know colonoscopy prevents CRC | ||||||
| Yes | 35 | 46 | 42 | 42 | ||
| No | 37 | 30 | 24 | 18 | ||
CRC: Colorectal cancer; IMRC: Internal medicine resident clinic; FMRC: Family medicine resident clinic.
Figure 2.
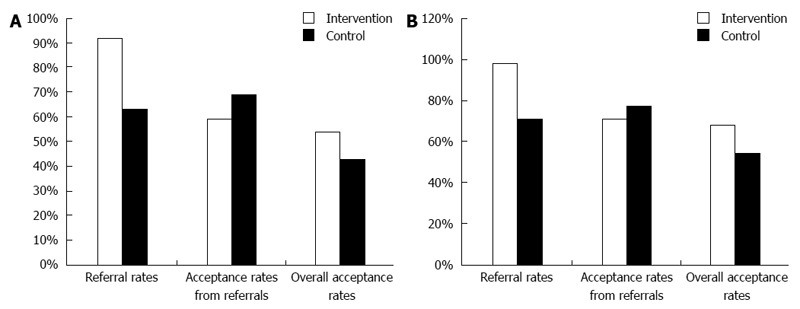
Patterns of referral and acceptance. A: In internal medicine resident clinic (underinsured patients); B: Family medicine resident clinic (Insured patients).
No difference was seen in referral acceptance between the 2 clinics. Among those who got referrals for CRC-S in the IMRC, 31/45 (69%) in the control group vs 41/70 (59%) in the intervention group accepted the referrals, (P = NS, Figure 2A). In patients from FMRC who were referred for CRC-S, 36/47 (77%) in the control group vs 41/56 (73%) in the intervention group accepted the referral, (P = NS, Figure 2B). In univariate analysis, factors related CRC-S referrals were having insurance (60% vs 46%, P = 0.045), male gender (38% vs 54%, P = 0.027), knowledge of CRC recommendations (46% vs 26%, P = 0.0085) and patients initiated promoting of PCP (intervention) (58% vs 18%, P < 0.0001). On multivariate logistic regression analysis, male gender (OR = 0.49, 95%CI: 0.26-0.93, P = 0.03) and patient initiated promoting the PCP (OR = 6.3, 95%CI: 2.9-13.2, P < 0.0001) were identified as independent predictors (Table 2).
Table 2.
Univariate and multivariate analysis of factors impacting colon cancer screening referral n (%)
| Offered CRC screening (n = 210) | Not offered CRC screening (n = 54) | P value | |
| Age, mean ± SD | 55 ± 4 | 55 ± 4 | 0.810 |
| White race | 116 (55) | 26 (48) | 0.350 |
| Male sex | 83 (38) | 31 (54) | 0.027 |
| Higher education | 57 (26) | 13 (23) | 0.590 |
| Insured | 131 (60) | 26 (46) | 0.045 |
| Limiting medical problems | 23 (11) | 5 (8) | 0.680 |
| Symptomatic | 91 (42) | 16 (28) | 0.056 |
| Family history | 23 (11) | 11 (19) | 0.076 |
| Knowledge of CRC recommendations | 99 (46) | 15 (26) | 0.0085 |
| Received pamphlet | 126 (58) | 10 (18) | < 0.0001 |
| Family medicine providers | 102 (47) | 24 (42) | 0.510 |
CRC: Colorectal cancer.
All patients referred for CRC-S were offered colonoscopy as the only screening method. Patients were not advised of any other CRC-S method after declining colonoscopy. Overall, 37% of participants in the IMRC and 35% in the FRMC declined CRC-S recommended by the physicians. The primary issue influencing patients’ decision to defer CRC-S referral was financial difficulty. Bowel preparation fear, procedure related complications, unsure of colonoscopy benefit, and concern of finding cancer were other, less frequent reasons for not accepting CRC-S referral (Figure 3).
Figure 3.
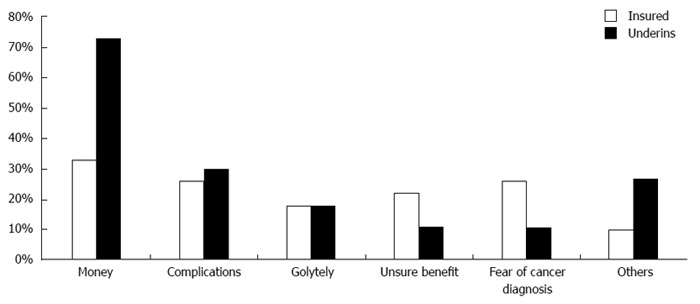
Factors resulting in declining referral between insured and underinsured patients. Underins: Underinsured patients.
DISCUSSION
Colorectal cancer is the fourth most common cancer diagnosed and second leading cause of cancer related death in the United States[1]. Early stage detection of colorectal cancer has a survival rate of around 80%[1]. Despite the proven efficacy of colorectal cancer screening, only about 50% of eligible patients in the United States are currently being screened[1]. Effective interventions as attempts to increase the referral for CRC-S are lacking. Studies have identified that a lack of communication between physicians and patients was the most common factor resulting in inadequate referrals for CRC-S[2-4]. However, few studies focus on the patient as a factor that contributes to this issue. The primary outcome of our study was to determine if patient initiated prompting of their PCP for CRC-S would increase referrals in both underinsured and insured patients. Increasing patient awareness combined with PCP prompting by patients about CRC-S resulted in increased referral rates.
Among the intervention groups in both clinics, ethnicity did not appear to impact the frequency of patient prompting of physician for CRC-S (data not shown). It is well known that African Americans do not get CRC-S as frequently as non-Hispanic whites[10]. This intervention may help narrow the CRC-S disparity observed, improving long term outcome from this disease.
Multiple barriers to colorectal cancer screening referral by PCPs have been identified in the literature[11-15]. The present study reveals another method where PCPs can be reminded of patient interest in CRC-S and provide appropriate referral for the procedure. This type of intervention using patient prompting of their PCP could decrease the burden on the PCP to remember appropriate CRC-S recommendations, resulting in an increased screening rate overall.
Referral rates after intervention were found to be increased in both clinic populations but acceptance rates after referral were less in both intervention groups, unexpectedly. This resulted in lower overall acceptance rates for both clinics and was not significantly different between intervention or control groups. Multiple factors have been identified which contribute to a reduced acceptance rate for CRC-S[16]. In our study, multiple issues were evident. First, college education was more prevalent in patients with medical insurance coverage and more of these individuals were aware of current CRC-S literature than underinsured patients. However, this did not impact whether CRC screening was offered. Secondly, we observed a higher acceptance rate, in insured patients, for CRC-S offered by their primary physicians compared to the underinsured which has been reported by previous investigators[17-19]. Finally, acceptance rate for CRC-S was increased in patients with alarm symptoms compared to asymptomatic patients in both control and intervention groups. The most common limiting factor influenced patient’s decision to refuse CRC screening was financial affordability in both underinsured (72%) and insured populations (36%) even though significantly lower in the insured population. Procedure complications, bowel preparation concerns, colonoscopy benefit uncertainty, and fear of finding cancer were other less common reasons for not accepting referrals.
A limitation to the present study is not using other screening methods available if colonoscopy is declined. As colonoscopy was considered the test of choice and other methods, if positive, result in colonoscopy referral, use of alternative screening tools appeared redundant to the investigators. However, some individuals may prefer colonoscopy only following a positive result from another screening tool and should be considered in larger scale investigations.
CRC-S referrals significantly increased with patient initiated prompting of physicians for such screening. Larger investigations, using this method, directed towards increasing acceptance of CRC-S are warranted.
COMMENTS
Background
Despite the available evidence suggesting the effectiveness of colorectal screening (CRC-S), almost half of the United States population over 50 years has not been tested. According to the National Cancer Institute, in 2009 the estimated new cases of colon cancer and rectal cancer in United States were 106100 and 40870 respectively.
Research frontiers
Effective interventions to increase patient referrals for CRC-S are lacking. Studies have identified that a lack of communication between physicians and patients was the most common factor resulting in inadequate referrals for CRC-S.
Innovations and breakthroughs
As colonoscopy was considered the test of choice and other methods, if positive, result in colonoscopy referral, use of alternative screening tools appeared redundant to the investigators.
Peer review
This is a well constructed study, of high clinical significance. It seems that it is sufficiently powered to detect pre-specified 25% difference in referral frequency, but in my opinion this sample size is not sufficiently enough to portray independent predictors resulting in declining referral between insured and underinsured patients.
Footnotes
P- Reviewers: Kirshtein B, Lakatos PL, Leitman M, Sgourakis G, Tsujikawa T, Vieth M S- Editor: Gou SX L- Editor: A E- Editor: Wang CH
References
- 1.Shapiro JA, Seeff LC, Thompson TD, Nadel MR, Klabunde CN, Vernon SW. Colorectal cancer test use from the 2005 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev. 2008;17:1623–1630. doi: 10.1158/1055-9965.EPI-07-2838. [DOI] [PubMed] [Google Scholar]
- 2.American Cancer Society. Colorectal cancer facts and figures. Accessed 29 October 2013. Available from: http://www.cancer.org/research/cancerfactsstatistics/colorectal-cancer-facts-figures.
- 3.Berkowitz Z, Hawkins NA, Peipins LA, White MC, Nadel MR. Beliefs, risk perceptions, and gaps in knowledge as barriers to colorectal cancer screening in older adults. J Am Geriatr Soc. 2008;56:307–314. doi: 10.1111/j.1532-5415.2007.01547.x. [DOI] [PubMed] [Google Scholar]
- 4.Klabunde CN, Vernon SW, Nadel MR, Breen N, Seeff LC, Brown ML. Barriers to colorectal cancer screening: a comparison of reports from primary care physicians and average-risk adults. Med Care. 2005;43:939–944. doi: 10.1097/01.mlr.0000173599.67470.ba. [DOI] [PubMed] [Google Scholar]
- 5.Lieberman DA. Clinical practice. Screening for colorectal cancer. N Engl J Med. 2009;361:1179–1187. doi: 10.1056/NEJMcp0902176. [DOI] [PubMed] [Google Scholar]
- 6.Lieberman DA, Weiss DG, Bond JH, Ahnen DJ, Garewal H, Chejfec G. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. Veterans Affairs Cooperative Study Group 380. N Engl J Med. 2000;343:162–168. doi: 10.1056/NEJM200007203430301. [DOI] [PubMed] [Google Scholar]
- 7.Schoenfeld P, Cash B, Flood A, Dobhan R, Eastone J, Coyle W, Kikendall JW, Kim HM, Weiss DG, Emory T, et al. Colonoscopic screening of average-risk women for colorectal neoplasia. N Engl J Med. 2005;352:2061–2068. doi: 10.1056/NEJMoa042990. [DOI] [PubMed] [Google Scholar]
- 8.Imperiale TF, Wagner DR, Lin CY, Larkin GN, Rogge JD, Ransohoff DF. Risk of advanced proximal neoplasms in asymptomatic adults according to the distal colorectal findings. N Engl J Med. 2000;343:169–174. doi: 10.1056/NEJM200007203430302. [DOI] [PubMed] [Google Scholar]
- 9.Regula J, Rupinski M, Kraszewska E, Polkowski M, Pachlewski J, Orlowska J, Nowacki MP, Butruk E. Colonoscopy in colorectal-cancer screening for detection of advanced neoplasia. N Engl J Med. 2006;355:1863–1872. doi: 10.1056/NEJMoa054967. [DOI] [PubMed] [Google Scholar]
- 10.Shokar NK, Carlson CA, Weller SC. Factors associated with racial/ethnic differences in colorectal cancer screening. J Am Board Fam Med. 2008;21:414–426. doi: 10.3122/jabfm.2008.05.070266. [DOI] [PubMed] [Google Scholar]
- 11.Hawley ST, Levin B, Vernon SW. Colorectal cancer screening by primary care physicians in two medical care organizations. Cancer Detect Prev. 2001;25:309–318. [PubMed] [Google Scholar]
- 12.Cooper GS, Fortinsky RH, Hapke R, Landefeld CS. Factors associated with the use of flexible sigmoidoscopy as a screening test for the detection of colorectal carcinoma by primary care physicians. Cancer. 1998;82:1476–1481. [PubMed] [Google Scholar]
- 13.Vernon SW. Participation in colorectal cancer screening: a review. J Natl Cancer Inst. 1997;89:1406–1422. doi: 10.1093/jnci/89.19.1406. [DOI] [PubMed] [Google Scholar]
- 14.Dulai GS, Farmer MM, Ganz PA, Bernaards CA, Qi K, Dietrich AJ, Bastani R, Belman MJ, Kahn KL. Primary care provider perceptions of barriers to and facilitators of colorectal cancer screening in a managed care setting. Cancer. 2004;100:1843–1852. doi: 10.1002/cncr.20209. [DOI] [PubMed] [Google Scholar]
- 15.Shokar NK, Nguyen-Oghalai T, Wu H. Factors associated with a physician’s recommendation for colorectal cancer screening in a diverse population. Fam Med. 2009;41:427–433. [PMC free article] [PubMed] [Google Scholar]
- 16.Senore C, Malila N, Minozzi S, Armaroli P. How to enhance physician and public acceptance and utilisation of colon cancer screening recommendations. Best Pract Res Clin Gastroenterol. 2010;24:509–520. doi: 10.1016/j.bpg.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 17.Vlahov D, Ahern J, Vazquez T, Johnson S, Philips LA, Nash D, Mitchell MK, Freeman H. Racial/ethnic differences in screening for colon cancer: report from the New York Cancer Project. Ethn Dis. 2005;15:76–83. [PubMed] [Google Scholar]
- 18.McAlearney AS, Reeves KW, Dickinson SL, Kelly KM, Tatum C, Katz ML, Paskett ED. Racial differences in colorectal cancer screening practices and knowledge within a low-income population. Cancer. 2008;112:391–398. doi: 10.1002/cncr.23156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Green AR, Peters-Lewis A, Percac-Lima S, Betancourt JR, Richter JM, Janairo MP, Gamba GB, Atlas SJ. Barriers to screening colonoscopy for low-income Latino and white patients in an urban community health center. J Gen Intern Med. 2008;23:834–840. doi: 10.1007/s11606-008-0572-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


