Abstract
Abstract
The outcome of bicondylar tibial plateau fractures treated with either external fixation (35 patients) or internal fixation (24 patients) was reviewed. Outcome measures included the Rasmussen score, clinical complications, development of osteoarthritis and the requirement for total knee replacement (TKR). Twenty-two (92%) anatomical reductions were achieved in the internal fixation group compared to 27 (77%) in the external fixation group. Infective complications were more common in the external fixation group (9 patients, 26%) due to pin tract infection. There were no deep infections in the internal fixation group. The mean Rasmussen score was not significantly different (mean score 32 in external fixation and 29 in internal fixation) between the two groups and the incidence of osteoarthritis was the same in both groups. Four patients in the external fixation group underwent a TKR compared to 5 patients in the internal fixation group. Bicondylar tibial plateau fractures have similar outcomes following external or internal fixation.
Key Words
bicondylar, tibial, plateau, external, internal, fixation, outcome
Introduction
The majority of tibial plateau fractures involve the lateral plateau and the standard method of treatment is internal fixation. Bicondylar fractures are less common but are more difficult to treat due to the complexity of the fracture configuration and the associated soft tissue injury. They are associated with a higher complication rate after internal fixation.
The optimal choice of treatment for bicondylar tibial plateau fractures remains controversial1. Although, in the past, internal fixation has been used commonly, external fixation has become a popular method of treatment in recent years, with a number of publications suggesting that satisfactory results can be obtained 2-4. External fixation is less invasive but achieving accurate anatomical reduction can be difficult. Internal fixation is theoretically better at achieving a more perfect reduction but the risk of soft tissue problems and wound breakdown is higher. Recent studies have shown that the Less Invasive Stabilization System (LISS) plating system provides stable fixation of complex bicondylar tibial plateau fractures allowing early range of knee motion with favourable clinical results 5. However we found no published studies comparing results of these two treatment methods to determine if one method is superior.
The aim of the present study was to compare the outcome of bicondylar tibial plateau fractures treated by external fixation versus internal fixation. In particular, we endeavoured to determine the incidence of symptomatic osteoarthritis and the requirement for late total knee joint replacement.
Materials and Methods
Eighty-two patients with bicondylar tibial plateau fractures were treated surgically from September 1995 to March 2005. Four patients had bilateral bicondylar tibial plateau fractures. Twenty-three patients had incomplete data or were lost to follow-up. Thus study group comprised 58 patients with 59 fractures. Twenty-four (41%) cases had internal fixation and 35 (59%) cases had external fixation as part of their management for bicondylar tibial plateau fractures. Fractures were classified using the AO classification (Table I)6.
Table I: Group C subgroups (AO Classification5). Comparison of Outcomes for Bicondylar Tibial Plateau Fractures Treated Operatively with Internal and External Fixation.
| AO Subgroup | Explanation |
| C1.1 | One condyle slightly displaced |
| C1.2 | One condyle displaced |
| C1.3 | Both condyles displaced |
| C2.1 | Intact wedged fracture |
| C2.2 | Fragmented wedged fracture |
| C2.3 | Complex fracture |
| C3.1 | Lateral plateau multifragmented fracture |
| C3.2 | Medial plateau multifragmented fracture |
| C3.3 | Both lateral and medial multifragmented articular fracture |
For patients who had internal fixation, 21 (84%) had conventional open reduction internal fixation with a standard AO buttress plate and 4 (16%) had fixation with a LISS plate (Figure 1). Following internal fixation, patients were mobilised (non-weight bearing) with crutches for 6 weeks. Partial weight bearing was then commenced, progressing to full weight bearing by 3 months.
Fig. 1: Position after internal fixation with Less Invasive Stabilization System (LISS) plate.

For patients who had external fixation, 23 (64%) had Ilizarov external fixators and 13 (36%) had Hoffman II external fixators with limited internal fixation. External fixators were left in situ for a minimum of 6 weeks. The mean duration of external fixation was 10 weeks (range, 6 – 14 weeks; 95% confidence interval). Patients were kept non-weight bearing while frames were on and were allowed to begin partial weight bearing following frame removal, progressing to fullweight bearing by 3 months. All patients were followed for a minimum of 2 years with radiographs at 3, 6, 12 and 24 months postoperatively.
Pre-operative, post-operative and most recent radiographs (anteroposterior and lateral) for each patient were analysed(Figure 2a and 2b) to assess the anatomical outcome using Rasmussen’s system of grading 7. This rating system evaluates joint depression, condylar widening and varus or valgus angulation. Postoperative reductions with less than 3mm of residual joint depression on anteroposterior or lateral views were considered acceptable. Postoperative reductions with more than 5mm of residual joint depression on anteroposterior or lateral views were rated as poor. Followup radiographs were used to detect post-traumatic osteoarthritis. Osteoarthritis was recorded if there was progressive obliteration of joint space, osteophyte formation and subchondral sclerosis 7. The requirement for total knee joint replacement was recorded. Measurements and observations were taken by one of the authors (JFK). All radiographs were checked for magnification, penetration and exposure before measurements and observations were taken to eliminate magnification errors. All radiographs included in this study were taken by staff members from the same radiology department adhering to local guidelines and the set up for knee radiograph was standardised.
Fig. 2a: Anteroposterior radiographic view of bicondylar plateau fracture after transarticular external fixation and limited internal fixation.

Fig. 2b: Final position after healing.

The databases for the period between September 1995 and March 2005 were collated, matched for variable types and merged using SPSS Version 12.0 statistical software package (SPSS Inc., Chicago, IL) for Windows. Analysis of parametric data was carried out with a Student t-test. Nonparametric data was analysed using Mann-Whitney U-test, the Chi-square test or Fisher’s exact test. Values of p less than 0.05 <0.05) were considered statistically significant.
Results
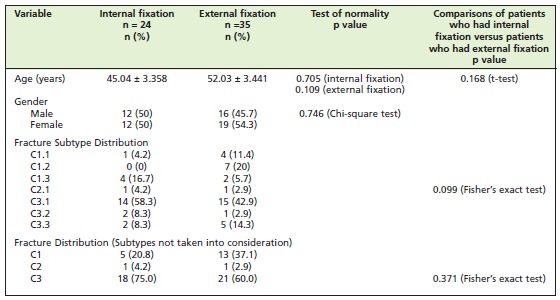
There were no significant differences in age, gender or fracture distribution between patients who had internal fixation and patients who had external fixation (Table II). There was 1 (4%) alcoholic in the internal fixation group but 7 (20%) in the external fixation group. There were no other differences between the 2 groups.
Table II: Summary of pre-operative variables for both groups of patients.
Three patients (13%) had infections after internal fixation (all were superficial infections) and 9 (26%) patients had infections after external fixation. Out of the 9 externally fixated patients, 6 developed a superficial pin tract infection. One patient with a transarticular Ilizarov frame developed septic arthritis. The frame was converted to a below knee configuration and lavage of the joint controlled the infection. Two patients developed deep infection in the proximal tibia.
One case was due to pin tract infection, and the other involved two screws that had been inserted to supplement external fixation. Both cases were controlled with debridement and antibiotic therapy.
Two patients (8%) developed deep vein thrombosis (DVT) after internal fixation, and there were no cases of DVT in the external fixation group. There were no pulmonary emboli in either group. Five cases of compartment syndromes occurred, 3 (14%) in the internal fixation group and 2 (6%) in the external fixation group. These cases occurred within 48 hours of admission and were successfully treated with fasciotomy.
Anatomical outcomes were evaluated using the Rasmussen’s system. Figure 3 shows the postoperative depression after the bicondylar tibial plateau fractures patients had internal fixation and external fixation. Reductions with less than 3mm of residual depression were achieved in 22 (92%) patients of the open reduction internal fixation (ORIF) group and 27 (77%) patients of the external fixation group. Poor reduction with residual joint depression was noted in 2 (8%) patients of the ORIF group and 8 (23%) patients of the external fixation group. These differences did not achieve statistical significance (Mann-Whitney U-test, p = 0.446, Table III). Similarly, condylar widening was not different between the two groups.
Fig. 3: Postoperative depression for internal fixation vs. external fixation.

In patients who had internal fixation, 21 (88%) of them had valgus alignment and 3 (13%) had residual varus alignment. In patients who have external fixation, 31 (89%) were in valgus and 4 (11%) were in varus alignment. Using Rasmussen’s score, the outcome of bicondylar tibial plateau fractures was determined by scoring system. Score 0 denotes the poorest outcome and score 18 denotes the best outcome (Figure 4). The median score in the external fixation group was 28.81 and the median score after internal fixation was 31.73 (p = 0.512, Mann-Whitney U-test (Table III).
Table III: Comparison of outcomes for internal fixation versus external fixation.
| Outcomes | p value | Test |
| Post-operative depression | 0.446 | Mann-Whitney U-test |
| Condylar widening | 0.728 | Mann-Whitney U-test |
| Angulation (valgus/varus) | 0.767 | Mann-Whitney U-test |
| Anatomical end outcome (using Rasmussen’s score) | 0.512 | Mann-Whitney U-test |
| Development of Osteoarthritis | 0.770 | Chi-square test |
| Total knee replacement (TKR) | 0.324 | Chi-square test |
At the time of final follow-up, 7 (29%) patients in the internal fixation group and 9 (26%) patients of the external fixation group showed radiographic evidence of osteoarthritis. Ultimately, 5 (21%) patients of the internal fixation group and 4 (11%) patients of the external fixation group underwent TKR. These slight differences were not significant (Table III).
Discussion
This study evaluated the outcome of two matched groups of patients with bicondylar tibial plateau fractures treated by internal fixation or external fixation at a single centre. Our results suggest that there is no significant difference in the anatomical outcome between the patients treated by internal fixation versus external fixation. The quality of reduction showed a trend towards more anatomical reductions in the internal fixation group but the difference was not statistically significant. Reflecting the severity of the injury, there was a high percentage of osteoarthritic change in both groups but the requirement for TKR for severe symptomatic osteoarthritis was not different between the groups. Patients underwent TKR as clinically indicated and were not limited by financial resources or a long waiting list. The National Health Service provided funding for TKR and the average waiting period was about 18 weeks. Although external fixation is theoretically safer with a lower rate of local surgical complications we did not find significant problems with the internal fixation group 8.
Previous studies on the management of bicondylar tibial plateau fractures have generally reported use of one surgical technique. Although internal fixation has been popular in the past, it is often thought to be associated with a high risk of early wound problems 9. A number of recent studies have indicated that satisfactory results can be achieved with external fixation 2-4. External fixation treatment includes conventional frames and circular fine wire fixators, is a less invasive surgical technique and may minimise the risk of soft tissue complications. However in our series, there were some troublesome pin tract infections and one case of septic arthritis, which is a well-recognised complication associated with external fixation around the knee.
We were unable to demonstrate an advantage of external fixation over internal fixation in the present study. Anatomical results were slightly inferior in internal fixation cases but both groups had a similar incidence of posttraumatic osteoarthritis and requirement for late knee replacement. We found no other large study comparing these two treatment methods for bicondylar plateau fractures. Mallik et al (1992) reported on 10 patients with bicondylar plateau fractures, three of whom had been treated with fine wire external fixation10. The remainder had been treated with internal fixation. They reported no difference in outcome but had a higher rate of infections in the internal fixation group. The numbers in that study were too small to draw firm conclusions about which treatment was the optimum choice.
Newer techniques of external fixation include arthroscopically assisted reduction with percutaneous screw fixation as well as applications of hybrid circular external fixators with or without limited internal fixation. These techniques provide adequate reduction and fixation while limiting the complications associated with traditional ORIF 2,3. The Sheffield Hybrid fixators (SHF) technique minimizes soft tissue dissection and provides superior cancellous bone purchase using beam-loading stabilization for comminuted fractures. Complex bicondylar tibial plateau fractures managed by this technique have good final outcome 11, 12.
Minimally invasive techniques of internal fixation have now become popular. Initial reports of the Less Invasive Surgical Stabilisation (LISS) plate system suggest it can provide stable fixation of complex bicondylar tibial plateau fractures while allowing early range of knee motion with favourable clinical results 3,5,13,14. Biomechanical studies suggest that a unilateral locked screw plate (LSP) is as effective as double plating for prevention of vertical subsidence in a bicondylar tibial plateau fracture model 15.
More limited surgical exposure with a second posteromedial incision has also been reported, resulting in a lower wound complication rate than previously reported16. This technique is a good choice in patients with a large posteriomedial fragment as a component of the bicondylar tibial plateau fracture 17.
Virtually all published clinical studies on bicondylar plateau fractures report the outcome of a single surgical technique. In our study, there was no significant difference in anatomical outcome, the presence of osteoarthritis and the need of TKR for bicondylar tibial plateau fracture patients in cases of internal versus external fixation. The main drawback of the present study is the non-randomised design, and the relatively small number of cases. The authors acknowledge that a longer follow-up period would be preferred to further detect the development of osteoarthritis and the need for TKR. A prospective study of a modern fine-wire external fixator and a minimally invasive plating system would be a useful addition to the literature.
Conclusion
Based on our findings, either internal or external fixation can be chosen for treatment of these injuries with the expectation of reasonable results, as there was no significant difference in the treatment outcome between bicondylar tibial plateau fractures treated with either method. The mean Rasmussen score, rate of clinical complications, incidence of osteoarthritis and need for subsequent TKR surgery was similar in both groups.
References
- 1.Mueller KL, Karunakar MA, Frankenburg EP, Scott DS. Bicondylar tibial plateau fractures: a biomechanical study. Clin Orthop & Rel Res. 2003;412:189–195. doi: 10.1097/01.blo.0000071754.41516.e9. [DOI] [PubMed] [Google Scholar]
- 2.Covall DJ, Fowble CD, Foster TE, Whitelaw GP. Bicondylar tibial plateau fractures: principles of treatment. Contemporary Orthopaedics. 1994;28:115–122. [PubMed] [Google Scholar]
- 3.Ali AM, Burton M, Hashmi M, Saleh M. Treatment of displaced bicondylar tibial plateau fractures (OTA-41C2 & 3) in patients older than 60 years of age. J Orthop Trauma. 2003;17:346–352. doi: 10.1097/00005131-200305000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Dirschl DR, Dahners LE. Current treatment of tibial plateau fractures. Journal of the Southern Orthopaedic Association. 1997;6:54–61. [PubMed] [Google Scholar]
- 5.Egol KA, Su E, Tejwani NC, Sims SH, Kummer FJ, Koval KJ. Treatment of complex tibial plateau fractures using the less invasive stabilization system plate: clinical experience and a laboratory comparison with double plating. Journal of Trauma- Injury Infection & Critical Care. 2004;57:340–346. doi: 10.1097/01.ta.0000112326.09272.13. [DOI] [PubMed] [Google Scholar]
- 6.Müller ME, Nazarian S, Koch P, Schatzker J. Tibia/fibula. The comprehensive classification of fractures of long bones. Berlin: Springer-Verlag; 1990. pp. 148–191. [Google Scholar]
- 7.Rasmussen PS. Impairment of knee joint stability as an indication for surgical treatment. J Bone Joint Surg [Am.] 1973;55:1331–1350. [PubMed] [Google Scholar]
- 8.Katsenis D, Vasilis A, Panayiotis M, Minos T, Lambiris E. Minimal internal fixation augmented by small wire transfixion frames for high-energy tibial plateau fractures. J Orthop Trauma. 2005;19:241–248. doi: 10.1097/01.bot.0000155309.27757.4c. [DOI] [PubMed] [Google Scholar]
- 9.Young MJ, Barrack RL. Complications of internal fixation of tibial plateau fractures. Orthop Rev. 1994;23:149–154. [PubMed] [Google Scholar]
- 10.Mallik AR, Covall DJ, Whitelaw GP. Internal versus external fixation of bicondylar tibial plateau fractures. Orthop Rev. 1992;21:1433–1436. [PubMed] [Google Scholar]
- 11.Ali AM, Yang L, Hashmi M, Saleh M. Bicondylar tibial plateau fractures managed with the Sheffield Hybrid Fixator.Biomechanical study and operative technique. Injury. 2001;32:86–91. doi: 10.1016/s0020-1383(01)00165-6. [DOI] [PubMed] [Google Scholar]
- 12.Farrar M, Yang L, Saleh M. The Sheffield hybrid fixators – a clinical and biomechanical review. Injury. 2001;32:8–13. doi: 10.1016/s0020-1383(01)00166-8. [DOI] [PubMed] [Google Scholar]
- 13.Horwitz DS, Bachus KN, Craig MA, Peters CL. A biomechanical analysis of internal fixation of complex tibial plateau fractures. J Orthop Trauma. 1999;13:545–549. doi: 10.1097/00005131-199911000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Cole PA, Zlowodzki M, Kregor PJ. Less Invasive Stabilization System (LISS) for fractures of the proximal tibia: indications,surgical technique and preliminary results of the UMC Clinical Trial. Injury. 2003;34:16–29. doi: 10.1016/s0020-1383(03)00254-7. [DOI] [PubMed] [Google Scholar]
- 15.Gosling T, Schandelmaier P, Marti A, Hufner T, Partenheimer A, Krettek C. Less invasive stabilization of complex tibial plateau fractures: a biomechanical evaluation of a unilateral locked screw plate and double plating. J Orthop Trauma. 2004;18:546–551. doi: 10.1097/00005131-200409000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Barei DP, Nork SE, Mills WJ, Henley MB, Benirschke. -. Complications associated with internal fixation of high-energy bicondylar tibial plateau fractures utilizing a two-incision technique. J Orthop Trauma. 2004;18:649–657. doi: 10.1097/00005131-200411000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Carlson DA. Posterior bicondylar tibial plateau fractures. J Orthop Trauma. 2005;19:73–78. doi: 10.1097/00005131-200502000-00001. [DOI] [PubMed] [Google Scholar]


