ABSTRACT
Background and objectives: Fluoride is being used for the prevention of dental caries since a long time. Incorporation of fluoride in pit and fissure sealants has been found to reduce initiation and progression of pit and fissure caries. Authors conducted this study to evaluate and compare the effect of fluoride releasing pit and fissure sealants on the inhibition of demineralization of adjacent enamel and to reduce wall lesion frequency.
Materials and methods: A total of 60 caries-free human third molars were randomly assigned into three groups receiving conventional resin sealant without fluoride (Group A), fluoride releasing resin sealant (Group B), glass ionomer pit and fissure sealant (Group C). Fissure cavities of 5 × 2 × 1.5 mm were prepared on buccal surfaces of teeth using fissurotomy bur and sealants were applied onto the cavities.
The teeth were then thermocycled and exposed to acidified gelatin gel for 6 weeks to induce caries like lesions. A 150 μ m section was taken from each tooth and observed under polarized light microscope to measure the depth of advancing front of outer enamel lesion. The outer lesion depths of all three groups were compared.
Results: Enamel demineralization was least in glass ionomer pit and fissure sealant while the demineralization exhibited by nonfluoridated resin and fluoridated resin were comparable. Wall lesion frequency was found to be 0% in all groups.
Conclusion and interpretation: The glass ionomer pit and fissure sealant exhibited highest anticariogenic efficacy and hence can be advocated as a means of preventing dental caries.
How to cite this article: Prabhakar AR, Dahake PT, Raju OS, Basappa N. Fluoride: Is It Worth to be added in Pit and Fissure Sealants?. Int J Clin Pediatr Dent 2012;5(1):1-5.
Keywords: Dental caries, Pit and fissure sealants, Fluorides
INTRODUCTION
Dental caries is the most prevalent chronic disease affecting the human race.1 Dental caries remains the singlemost common disease of childhood, occurring five to eight times more commonly than asthma, which is the second most common disease of childhood.2
Occlusal surface represents 12.5% of total surface of permanent dentition but accounts for more than 50% of caries in school children. Occlusal pits and fissures are the areas of caries initiation. Attempts are being made since a long time to prevent initiation and progression of pit and fissure caries by various means.3 Introduction of Bis-GMA has revolutionized the pit and fissure sealant treatment. Since then, many advancements have been made to improve their adhesive and mechanical properties. Pit and fissure sealants are an economical and adequate means for prevention of dental caries on occlusal surface of molars and premolars and to maintain dental health. Various other materials like flowable composites, glass ionomer cements, resin-modified glass ionomer cements, compomers and different types of bonding agents have also been used nowadays as pit and fissure sealants.
The topical and systemic fluorides are effective in reducing the smooth surface caries but are ineffective in preventing pits and fissures caries.4 Incorporation of fluorides in pit and fissure sealants has been found to play a promising role in the reduction of pit and fissure caries, thereby reducing overall caries incidence. Different types of fluoride releasing pit and fissure sealants can be used to protect smooth surfaces, hypoplastic enamel and areas around orthodontic brackets. Considering these advantages, use of sealants is advocated in various public health prevention measures and has to be proved successful.5
Hence, the present study was conducted to evaluate and compare the potential of fluoride releasing pit and fissure sealants on the inhibition of demineralization of adjacent enamel and to reduce wall lesion frequency.
MATERIALS AND METHODS
A total of 60 third molars extracted for therapeutic purpose were included in the study. All the teeth were evaluated under a stereomicroscope (Leica Wild M3Z, Germany) to ensure the absence of white spot lesions or caries, developmental defects, microfractures and discoloration.6All the samples were stored in 0.01% thymol solution7 to achieve disinfection and prevent dehydration. Fluoride-free prophylaxis8 was done and teeth were stored in double deionized distilled water at room temperature until further use.
The samples were divided into three groups—A, B and C, each containing 20 teeth. On the middle third of buccal surface of each of the third molar tooth, fissure cavity9 was prepared using Fissurotomy bur (SS White Burs, Lakewood, NJ) and a high speed handpiece (NSK, PANA AIR) of size 5 × 2 × 1.5 mm without bevel or feather edge preparation. The dimensions of the cavity were measured with a William’s periodontal probe (Hu-Friedy PQW6, USA) to ensure uniformity of the enamel window in all the samples. All the three groups were color coded for identification as per shown in Table 1 and filled with pit and fissure sealants according to manufacturers’ instructions.
Table 1: Color coding of groups along with pit and fissure sealants
| Sr. no. | Group | Color coding | Pit and fissure sealant | ||||
| 1. | Group A | Red | Nonfluoridated resin sealant (Helioseal® pit and fissure sealant) | ||||
| 2. | Group B | Green | Fluoride-releasing resin sealant (Guardian Seal™ pit and fissure sealant) | ||||
| 3. | Group C | Pink | Glass ionomer pit and fissure sealant (GC Fuji VII™ GI pit and fissure sealant) |
Application of Sealants to the Cavities
Group A (Nonfluoridated pit and fissure sealant; Helioseal® pit and fissure sealant): The cavity in each sample was acid etched10 with 37% phosphoric acid gel for 30 seconds,11 rinsed with double deionized distilled water for 10 seconds and dried with oil-free compressed air for 10 seconds. The material was then placed in the cavity of each tooth with the manufacturer’s direct delivery system up to cavosurface margin and light cured for 40 seconds with light curing unit (Bee Cool, Plus Top light – LED light curing unit, Taiwan).
Group B (Fluoride-releasing pit and fissure sealant, Guardian Seal™ pit and fissure sealant): The same procedure as described for group A was followed with respect to the samples belonging to group B.
Group C (Glass ionomer pit and fissure sealant, GC Fuji VII™ GI pit and fissure sealant): The cavity of each sample was cleaned for 15 seconds with cavity conditioner,12 rinsed with double deionized distilled water for 10 seconds and dried with oil-free compressed air for 10 seconds. The powder and liquid were mixed according to manufacturer’s instructions and placed into cavities. Excess material was removed with plastic instrument and light cured for 40 seconds (Bee Cool, Plus Top light – LED light curing unit, Taiwan). All the surfaces of molars were coated with acid resistant varnish leaving 1 mm rim of exposed sound enamel surrounding the sealant-filled cavities and subjected to thermocycling13 in artificial saliva.14
Samples were suspended in acidified gelatin gel15 for 6 weeks at 37°C to induce artificial caries like lesion on exposed enamel rim. The acidified gelatin gel was changed at weekly interval, as pH of solution gets altered with time. Each tooth was then cleaned thoroughly with double de- ionized distilled water.
Longitudinal tooth section of 150 μ m thickness was obtained by cutting through the enamel window of tooth using a Silverstone-Taylor hard tissue microtome (Leica SP 1600, Leica Microsystems, Nussloch, Germany). The section was mounted on glass slide and evaluated under polarized light microscope (Leica, Leica Microsystems, Nussloch, Germany).16
Quantification of the Lesions using Leica QWin Software
Each section was examined under polarized light microscope and photomicrograph of each section was taken. The mean lesion depths of caries like lesions were determined in a blinded fashion by projecting the photomicrographs onto a computer interfaced digitized tablet and measuring 10 points along the advancing front lesions. Using the same protocol, the presence or absence of wall lesions was determined for each specimen. The advancing front along the body of the outer surface lesion was measured, with the first measurement located 100 micrometers from the cavity preparation (Fig. 1).
Fig. 1.
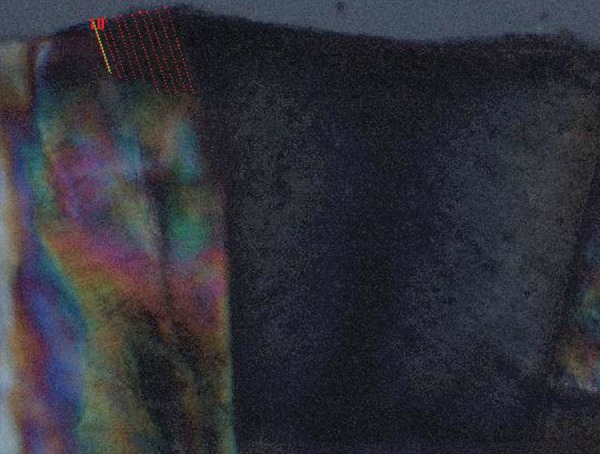
Photomicrograph showing measurement of advancing front of caries like lesions at 10 points
For statistical analysis, one-way ANOVA was used for multiple group comparisons followed by post hoc Tukey’s test for groupwise comparison (A vs B, A vs C, B vs C). The results were expressed as mean ± SD, coefficient of variation and range values.
RESULTS
Table 2 and Figure 2 show the mean depths of the outer lesions from the three treatment groups. The mean depth of outer lesions was compared using ANOVA and post-hoc Tukey’s test for groupwise comparison (significance level of p < 0.05).
Table 2: Descriptive statistics showing the intergroup comparison of the significance p-values of difference in demineralization among three experimental groups
| Groups |
Demineralization
Mean ± SD |
Difference between groups | Significance | |||||||
| Groups compared | Mean difference | p-value* | ||||||||
| Group A | 214.44 ± 97.44 | A-B | 8.29 | 0.93 NS | p > 0.05 | |||||
| Group B | 222.73 ± 80.66 | A-C | 58.45 | 0.049 S | p < 0.05 | |||||
| Group C | 155.99 ± 37.87 | B-C | 66.74 | 0.021 S | p < 0.05 | |||||
ANOVA F = 4.51; p < 0.05; S: Significant; p > 0.05; NS: Not significant; *: Post-hoc Tukey’s test; SD: Standard deviation
Fig. 2.
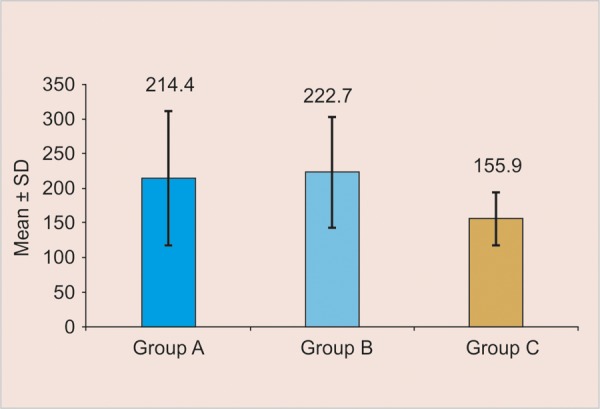
Mean demineralization values of groups A, B and C
The mean outer lesion depth was the least for group C (glass ionomer pit and fissure sealant) at 73%. The difference in outer lesion depth of group C with that of the remaining groups was found to be significant. As shown in Table 3, the outer lesions adjacent to cavities filled with the conventional nonfluoride-containing sealant had a reduction of 3% in depth when compared with those filled with fluoride-releasing sealant. The outer lesions adjacent to the cavities filled with glass ionomer sealant had a reduction of 27% in depth when compared with the conventional nonfluoride-containing sealant. The glass ionomer sealant group also had a 30% reduction in outer lesion depth when compared with the fluoride-releasing sealant group. The percentage of reduction was calculated by dividing the mean lesion depth for the treatment group by the mean lesion depth for the control group and multiplying the result by 100%.
Table 3: Effect of fluoride release from sealant material on enamel demineralization and wall lesion frequency
| Sealant | Mean outer lesion depth (micrometers) | Wall lesion frequency | Reduction in outer lesion depth | |||
| Group A (nonfluoridated pit and fissure sealant) | 214.44 ± 97.44 | 0% | 3% when compared with fluoride-releasing sealant | |||
| Group B (fluoridated pit and fissure sealant) | 222.73 ± 80.66 | 0% | ||||
| Group C (glass ionomer pit and fissure sealant) | 155.99 ± 37.87 | 0% | 27% when compared with conventional nonfluoride-containing seal style="border-bottom:solid 1px #000000;"ant 30% when compared with the fluoride- releasing sealant group |
DISCUSSION
Pits and fissures are more vulnerable to caries initiation due to variation in shapes, tortuousness with invaginations or irregularities and narrowness (~ 0.1 mm wide). As a result these are ideal sites for the retention of bacteria and food remnants, rendering mechanical means of debridement inaccessible as toothbrush bristle (0.2 mm) is too large to penetrate most of the fissures.4
Attempts were made to prevent pit and fissure caries by various means like prophylactic odontotomy, enameloplasty, use of topical and systemic fluorides and various adhesive materials like cements and resins.4 Use of pit and fissure sealants was thus conceptualized to prevent initiation of caries in fissures which is conservative modality of caries prevention.17 The cariostatic properties of sealants are attributed to the physical obstruction of the pits and fissures preventing colonization of new bacteria and penetration of fermentable carbohydrates, so that remaining bacteria cannot produce acid in cariogenic concentration.18 The role of fluoride released from dental materials in the prevention of caries19 has been evidenced from in vitro and in vivo studies, supporting the contention that frequent supply of F– at low concentration decrease the enamel demineralization and accelerates the remineralization process.20
Although other agents, such as fluoridated varnishes, dentifrices, mouth rinses and gels can reduce the prevalence of caries, the fluoride released from dental materials also plays a promising role in caries prevention.21,22 The ability of a dental material to act as a fluoride reservoir is a distinct advantage in caries resistance, both at the enamel restorative interface and adjacent to the outer enamel surface near the fluoride-releasing dental material.23,24 Glass ionomer cement (GIC) is shown to release fluoride slowly over a period of time25 into the surrounding enamel yielding cariostatic effects.26 Chemical bonding of GIC to enamel and dentin without etching is the additional advantage, making it much easier to handle.12 Because of its well-known cariostatic effect, attempts were made consistently for more than 25 years to add fluoride in resin sealants27 and efforts to combine the two continue today.28
In the present study, glass ionomer pit and fissure sealant has shown highest inhibition of demineralization of adjacent enamel. The difference in inhibition of demineralization between glass ionomer pit and fissure sealant and fluoridated and nonfluoridated resin sealant was statistically significant. The result is attributed to F– released from glass ionomer cement by means of three discrete mechanisms: Surface wash off, diffusion through pores and cracks and bulk diffusion.29 Similar findings were confirmed by some in vitro and in vivo studies showing a sustained fluoride release from GIC to the surrounding dental structures30 and tooth microenvironment.31 Study evaluating GIC as pit and fissure sealants clinically has proved to reduce caries susceptibility.32
There was no significant inhibition of demineralization seen between fluoridated as well as nonfluoridated resin sealants thus, confirming previous results.30,33
The above findings could be explained by the differences in the composition between ionomeric and resinous materials, resulting in subsequent differences in fluoride releasing profiles.33 Diffusion of water into the material is necessary for the formation of hydrogen ions that attack the fluoride-containing glass particles, releasing fluoride. That is why ionomeric materials are more permeable to water, enhancing fluoride diffusion and release.34 On the other hand, the matrix of resinous sealants is much less hydrophilic, making fluoride release more difficult.35
No wall lesions were found in any of the specimens in this study. Absence of wall lesions may be justified due to reduction of microleakage along the tooth-sealant material interface due to acid etching or conditioning of enamel. Micropores and microprojections are created on enamel surface causing penetration and polymerization of sealants in these areas, forming a mechanical bond with the tooth. Optimal bonding of resin sealants to enamel depends on proper and adequate conditioning of enamel.36 The result obtained in this study can be confirmed by other studies showing that the sealants exhibited small or no dye microleakage at the interface between sealant and dental enamel.37
Depending on the environment, all pit and fissure sealants may act differently due to other variables like preparation of fissures, enamel etching and conditioning, application of bonding agents and contamination of prepared surfaces of fissures. Appropriate method of application of sealants is also a determining factor to reduce the microleakage thus, reducing wall lesion, which may further lead to formation of secondary caries.
CONCLUSION
The inhibition of demineralization in enamel adjacent to glass ionomer pit and fissure sealants was the highest followed by fluoridated and nonfluoridated resin sealants.
The inhibition of demineralization in enamel adjacent to fluoridated and nonfluoridated resin sealants was comparable.
No wall lesions were found in any of the specimens in all of the pit and fissure sealants.
Footnotes
Source of support: Nil
Conflict of interest: None declared
Contributor Information
AR Prabhakar, Professor and Head, Department of Pedodontics and Preventive Dentistry, Bapuji Dental College and Hospital, Davangere-577004 Karnataka, India, e-mail: attiguppeprabhakar@gmail.com.
Prasanna T Dahake, Postgraduate Student, Department of Pedodontics and Preventive Dentistry, Bapuji Dental College and Hospital, Davangere, Karnataka India.
OS Raju, Professor, Department of Pedodontics and Preventive Dentistry, Bapuji Dental College and Hospital, Davangere, Karnataka, India.
N Basappa, Professor, Department of Pedodontics and Preventive Dentistry, Bapuji Dental College and Hospital, Davangere, Karnataka, India.
REFERENCES
- 1. Newbrun E. History and early theories of the etiology of caries. In: Newbrun E (Ed). Cardiology. (3rd ed) Chicago: Quintessence; 1989. pp. 13–28 p. [Google Scholar]
- 2. Mc-Donald RE, Avery DR, Stookey GK. Dental caries in the child and adolescent. In: McDonald RE, Avery DR, Dean JA editors. Dentistry for the child and adolescent. (8th ed) New Delhi: Elsevier; 2005. pp. 203–235 p. [Google Scholar]
- 3. Hicks J, Flaitz CM. Pit and fissure sealants and conservative adhesive restorations: Scientific and clinical rationale. In: Pinkham JR, Casamassimo PS, McTigue Fields, Jr, HW, Nowak AJ editors. Pediatric Dentistry Infancy through Adolescence. (4th ed) New Delhi: Saunders An Imprint of Elsevier; 2005. pp. 520–576 p. [Google Scholar]
- 4. Nikiforuk G. Occlusal sealants. In: Nikiforuk G (Ed). Understanding dental caries, etiology and mechanisms, basic and clinical aspects. Vol. 2. New York: Karger; 1985. pp. 145–173. [Google Scholar]
- 5. Salar DV, Garcia-Godoy F, Flaitz CM, Hicks MJ. Potential inhibition of demineralization in vitro by fluoride releasing sealants. J Am Dent Assoc. 2007;138(4):502–506. doi: 10.14219/jada.archive.2007.0203. [DOI] [PubMed] [Google Scholar]
- 6. Ellwood RP, O’Mullane D. The association between developmental enamel defects and caries in populations with and without fluoride in their drinking water. J Public Health Dent. 1996;56(2):76–80. doi: 10.1111/j.1752-7325.1996.tb02400.x. [DOI] [PubMed] [Google Scholar]
- 7. Moura JS, Rodrigues LKA, Del Bel Cury AA, Lima EMCX, Garcia RMCR. Influence of storage solution on enamel demineralization submitted to pH cycling. J Appl Oral Sci. 2004;12(3):205–208. doi: 10.1590/s1678-77572004000300008. [DOI] [PubMed] [Google Scholar]
- 8. Ansari G, Oloomi K, Eslami B. Microleakage assessment of pit and fissure sealant with and without the use of pumice prophylaxis. Int J Pediatr Dent. 2004;14(4):272–278. doi: 10.1111/j.1365-263X.2004.00565.x. [DOI] [PubMed] [Google Scholar]
- 9. Garcia-Godoy F, de Araujo FB. Enhancement of fissure sealant penetration and adaptation: The enameloplasty technique. . J Clin Pediatr Dent. 1994;19(1):13–18. [PubMed] [Google Scholar]
- 10. Salama FS, Al-Hammad NS. Marginal seal and compomer materials with and without enameloplasty. Int J Pediatr Dent. 2002;12(1):39–46. [PubMed] [Google Scholar]
- 11. Buonocore MG. A Simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. J Dent Res. 1955;34(6):849–853. doi: 10.1177/00220345550340060801. [DOI] [PubMed] [Google Scholar]
- 12. Aboush YE, Jenkins CBG. An evaluation of the bonding of glass ionomer restoratives to dentin and enamel. Br Dent J. 1986;161(5):179–184. doi: 10.1038/sj.bdj.4805923. [DOI] [PubMed] [Google Scholar]
- 13. Smith LA, O’brain JA, Retief DH, Marchman JL. Microleakage of two dentinal bonding restorative systems. J Dent Res. 1988;67:309. [Google Scholar]
- 14.el Mallakh BF, Sarkar NK. Fluoride release from glass ionomer cements in deionized water and artificial saliva. Dent Mater. 1990;6(2):118–122. doi: 10.1016/s0109-5641(05)80041-7. [DOI] [PubMed] [Google Scholar]
- 15. Kidd E. The early carious lesion in enamel. In: Murray JJ (Ed). The prevention of dental diseases. Oxford, England: University Press; 1983. pp. 192–217. [Google Scholar]
- 16. Arends J, ten Bosch JJ. Demineralization and remineralization evaluation technique. J Dent Res. 1992;71:924–928. doi: 10.1177/002203459207100S27. [DOI] [PubMed] [Google Scholar]
- 17. Gordon PH, Nunn JH. Fissure sealants. In: Murray JJ (Ed). The prevention of oral disease. (3rd ed) New York: Oxford University Press; 1996. pp. 78–94 p. [Google Scholar]
- 18. Sanders BJ, Feigal RJ, Avery DR. Pit and fissure sealants and preventive resin restorations. In: Mc-Donald RE, Avery DR, Dean JA (Ed). Dentistry for the child and adolescent. (8th ed) New Delhi: Elsevier; 2005. p. 355. [Google Scholar]
- 19. Jensen ME, Wefel JS, Triolo PT, Hammesfahr PD. Effects of a fluoride-releasing sealant on artificial enamel caries. Am J Dent. 1990;3(2):75–78. [PubMed] [Google Scholar]
- 20. Page DJ. A study of the effect of fluoride delivered from solution and dentifrices on enamel demineralization. Caries Res. 1991;25(4):251–255. doi: 10.1159/000261372. [DOI] [PubMed] [Google Scholar]
- 21. Cain K, Hicks J, English J, Flaitz C, Powers JM, Rives T. In vitro enamel caries formation and orthodontic bonding agents. Am J Dent. 2006;19(3):187–192. [PubMed] [Google Scholar]
- 22. Bynum AM, Donly KJ. Enamel de/remineralization on teeth adjacent to fluoride releasing materials without fluoride dentifrice exposure. ASDC J Dent Child. 1999;66(2):89–92. [PubMed] [Google Scholar]
- 23. Francci C, Deaton TC, Arnold RR, Swift EJ Jr, Perdigao J, Bawden JW. Fluoride release from restorative materials and its effects on dentin demineralization. J Dent Res. 1999;78(10):1647–1654. doi: 10.1177/00220345990780101001. [DOI] [PubMed] [Google Scholar]
- 24. Donly KJ. Enamel and dentin demineralization inhibition of fluoride- releasing materials. Am J Dent. 1994;7(5):275–278. [PubMed] [Google Scholar]
- 25. Swartz ML, Philips RW, Clark HE. Long-term fluoride release from glass ionomer cements. J Dent Res. 1984;63(2):158–160. doi: 10.1177/00220345840630021301. [DOI] [PubMed] [Google Scholar]
- 26. Garcia-Godoy F. Preventive glass ionomer restorations. Am J Dent. 1988;1(3):97–99. [PubMed] [Google Scholar]
- 27. Lee H, Ocumpaugh DE, Swartz ML. Sealing of developmental pits and fissures: II. Fluoride release from flexible fissure sealants. J Dent Res. 1972;51(1):183–190. doi: 10.1177/00220345720510011401. [DOI] [PubMed] [Google Scholar]
- 28. Rock WP, Foulkes EE, Perry H, Smith AJ. A comparative study of fluoride releasing composite resin and glass ionomer materials used as fissure sealants. J Dent. 1996;24(4):275–280. doi: 10.1016/0300-5712(95)00061-5. [DOI] [PubMed] [Google Scholar]
- 29. Kuhn AT, Wilson AD. The diffusion mechanism of silicate and glass ionomer dental cements. Biomaterials. 1985;6(6):378–382. doi: 10.1016/0142-9612(85)90096-1. [DOI] [PubMed] [Google Scholar]
- 30. Wessenberg G, Hals E. The in vitro effect of glass ionomer cement on dentin and enamel walls. J Oral Rehabil. 1980;7(1):35–42. doi: 10.1111/j.1365-2842.1980.tb01461.x. [DOI] [PubMed] [Google Scholar]
- 31. Hatibovic-Kofman S, Koch G, Ekstrand J. Glass ionomer materials as rechargeable fluoride release system. Int J Paediatr Dent. 1997;7(2):65–73. doi: 10.1111/j.1365-263x.1997.tb00281.x. [DOI] [PubMed] [Google Scholar]
- 32. Arrow P, Riordan PJ. Retention and caries preventive effects of a GIC and a resin-based fissure sealant. Community Dent Oral Epidemiol. 1995;23(5):282–285. doi: 10.1111/j.1600-0528.1995.tb00249.x. [DOI] [PubMed] [Google Scholar]
- 33. Glasspoole EA, Erickson RL, Davidson CL. Demineralization of enamel in relation to the fluoride release of materials. Am J Dent. 2001;14(1):8–12. [PubMed] [Google Scholar]
- 34. Asmussen E, Peutzfeldt A. Long-term fluoride release from glass ionomer cement, a compomer, and from experimental resin composites. Acta Odontol Scand. 2002;60(2):93–97. doi: 10.1080/000163502753509482. [DOI] [PubMed] [Google Scholar]
- 35. Preston AJ, Agalamanyi EA, Higham SM, Mair LH. The recharge of esthetic dental restorative materials with fluoride in vitro - two years’ results. Dent Mater. 2003;19(1):32–37. doi: 10.1016/s0109-5641(02)00011-8. [DOI] [PubMed] [Google Scholar]
- 36. Roydhouse RH. Prevention of occlusal fissure caries by use of a sealant: A pilot study. ASDC J Dent Child. 1968;35(3):253–262. [PubMed] [Google Scholar]
- 37. Hatibovivic-Kofman S, Wrigth GZ, Braverman I. Microleakage of sealants after conventional, bur, and air-abrasion preparation of pits and fissures. Pediatr Dent. 1998;20(3):173–176. [PubMed] [Google Scholar]


