Abstract
OBJECTIVE: This was a single-center, prospective, pilot study aiming to evaluate the impact of pharmacist involvement in the admission medication history and reconciliation process and to quantify discrepancies found by pharmacists when compared to information collected by other health care providers at a pediatric institution.
METHODS: A pharmacist completed a thorough medication history and reconciled discrepancies with the medical team. Discrepancies included incorrect medication, dose, route, frequency; omitted information; missing medications; or any other inconsistencies outside of these categories. Information was documented in the electronic medical record via a standardized template, and pertinent discrepancies were communicated with the medical team.
RESULTS: Of the 100 medication histories included in the study, a total of 309 discrepancies were identified and corrected in the electronic medical record. The median length of time it took pharmacists to complete the medication history process was 15 minutes per patient (interquartile range, 10–20 minutes). Thirty discrepancies were determined as pertinent and were reported as intervened on and communicated to the medical team.
CONCLUSION: This study provides evidence that pharmacist-obtained admission medication histories and reconciliation have the potential to prevent potentially significant adverse drug reactions and have a positive impact on patient care.Index terms admission, history, medication, pharmacist, reconciliation
INDEX TERMS: admission, history, medication, pharmacist, reconciliation
INTRODUCTION
Up to one quarter of adverse events in health care are related to medications.1 The Institute of Medicine's report on medical errors generated increased attention to the issue of patient safety in the health care system, reporting that medical errors accounted for 44,000 to 98,000 deaths annually, which exceeds the number of deaths due to motor vehicle accidents, breast cancer, or AIDS. This places medical errors as the eighth leading cause of death in the United States.2 It is estimated that 25% of all medication-related injuries are due to medication errors and are thus considered preventable.3
Up to 60% of patients admitted to the hospital will have 1 or more medication-related discrepancy in their admission medication history (MH).4 An accurate and thorough MH and medication reconciliation (MR) are important for the care of each patient. A thorough MH should consist of a list of the concentration, dose, route, and frequency of all medications the patient is currently taking at home.5 MR is defined as the process of gathering the most accurate list possible of all medications a patient is taking and comparing that list against the ordering provider's admission, transfer, and/or discharge orders. The goal is to provide accurate medications to the patient at all transition points.6 Inaccurate or incomplete MHs and reconciliation may lead to duplication of therapy, unexpected interactions or adverse drug reactions, discontinuation of medications inadvertently, or failure to detect drug-related problems.5
Some barriers to completing an accurate MH include time constraints, language barriers, the severity of the patient's illness, the patient or caregiver's cognitive status, and the patient or caregiver's familiarity with the home medication regimen. It has been postulated that having a formalized process in which the interviewer is familiar with medication names, characteristics, adverse drug reactions, dosage forms, and administration of medications would minimize many of these barriers and improve outcomes.7 Since pharmacists have expertise in understanding medication therapy, this provides an opportunity for pharmacists to have a positive impact in the accuracy and completeness of MHs.
One study that compared physician-obtained MHs to pharmacist-obtained MHs for 55 patients found that pharmacists identified significantly more medications and documented significantly more medication doses and dosage schedules.7 Pharmacists identified 353 discrepancies, including 58 medications not initially identified by physicians (p≤0.001). Another study5 found similar results when MHs taken by emergency department (ED) providers were compared to those taken by clinical pharmacists for 286 patients. The pharmacist-acquired MHs in the ED were more complete than those acquired by other health professionals, specifically identifying more medications, dosing information, allergies, and immunization history.
Fewer data are available in the pediatric population with regard to the benefit of pharmacist-acquired MHs. One study8 used a pharmacy student with pediatric training to obtain an admission MH and perform MR of 272 patients admitted to the general pediatrics team. At least 1 unintentional discrepancy was found for 59 patients (22%), of which 71% were of low clinical importance, 23% were of moderate importance, and 6% had severe potential to cause discomfort or deterioration. Another study9 evaluated pharmacist-obtained hospital admission MR from 5 sources including parent/patient, primary care provider, community-based pharmacy, current admission history, and physical examination note of 23 medically complex children. Thirty-nine errors were identified in 182 admission medications (21%), including 17 omissions that affected 13 patients (57%). Both of these studies demonstrate that admission MH errors are common in pediatric patients. The objective of our study was to implement and evaluate the benefit of pharmacist involvement in admission MH and MR process and to quantify discrepancies found by pharmacists when compared to information collected by other health care providers at a pediatric institution.
METHODS
This was a single-center, prospective, pilot study conducted at a 155-bed pediatric acute care, freestanding, teaching hospital that is part of a larger health care system. The study was approved by the Institutional Review Board at the University of Chicago Medicine. Patients were eligible for inclusion in the study if they were admitted between November 2011 and February 2012 to the general pediatrics service. Patients were excluded if they were being readmitted within 72 hours of discharge, transferred from another inpatient service, or a ward of the state. This pilot was conducted on weekdays during normal business hours, since weekends were operated on a downscaled model.
The general pediatrics service is a multidisciplinary team with its own dedicated clinical pharmacy specialist. Pharmacy residents currently on the general pediatrics rotation are also closely involved in the care of these patients. Although the clinical pharmacist is involved in managing medication therapy for these patients, standard practices at this institution require a physician and nurse who are members of the admitting team caring for the patient to perform and document an admission MH. This is the required admitting procedure for all patients admitted to the hospital. The information obtained during the MH is documented directly into the electronic medical record (EMR) by using Epic v2010 (Epic, Verona, WI) under the prior to admission (PTA) medication tab. Although a patient's medication profile will carry forward from admission to admission, a nurse and physician must document that he or she has obtained and updated the current PTA medication information.
To implement the MH and MR process, the physicians working on the general pediatrics team were notified of the increased involvement of pharmacists in this process. All pharmacists, including clinical specialists as well as residents, caring for patients on this service were given both verbal and written training regarding specific instructions on the methodology of the study in an effort to standardize the process. A uniform MH form was used to document information for each patient.
As part of the study procedures, following completion of an MH by a physician and nurse, a pharmacist completed an MH by speaking with the patient, family, caregiver, and/or pharmacy. The section in the EMR that listed the patients' PTA medications was then updated by the pharmacist to reflect the correct medication regimen. Next, MR was performed by using the information collected and comparing it to the inpatient orders. Any pertinent discrepancies were then communicated verbally with the medical team. These were defined as discrepancies that could potentially cause patient harm if not addressed in a timely fashion. Finally, a note was written in the EMR, summarizing the MH information obtained including any discrepancies identified, medication changes being made, as well as any other pharmacist recommendations.
Information collected included admission date and time, MH date and time, patient's community pharmacy information, allergies, PTA medications as reported in the EMR, pharmacist-obtained PTA medications, number and type of discrepancies identified, number of interventions made to the medical team, a subjective accuracy score, and the time spent completing the process. Discrepancies were categorized as incorrect medication, incorrect dose, incorrect route, incorrect frequency, omitted information, missing medication, or other (consisting of any other inconsistencies outside of these categories). After the pharmacist completed the MH, he or she assigned a subjective accuracy score based on how accurate the information collected seemed, with 1 being the least accurate and 5 being the most accurate.
The primary outcome was the number of discrepancies discovered by pharmacists in admission MH information compared to information collected by other health care providers. Secondary outcomes included time barriers to pharmacist involvement in MHs and the number of interventions made to the medical team by pharmacists. This was a pilot study where descriptive statistics were used to analyze data.
RESULTS
A total of 100 MHs were included in the study. Pharmacists were unable to obtain MH information for many patients. The major reasons for this included patients unfamiliar with their home medication regimen, no family members/caregivers present to provide the medication information, or patients being admitted during the weekend when pharmacists were not available to obtain an MH. Of the 100 MHs included in this pilot, 70 were completed within 24 hours after admission. The primary pharmacy the patient used to fill prescription medications could be obtained for 77 patients. For the 77 patients who had pharmacy information documented, the pharmacist contacted 33 of these pharmacies for additional information. This included clarifying the patient's medication regimen, obtaining information the patient or caregiver did not know, such as a medication name, strength, dose, as well as inquiring about refill history. The mean number of medications documented before pharmacist intervention and after pharmacist intervention was 4.4 ± 3.3 and 4.3 ± 3.9, respectively. The median time it took for a pharmacist to complete the MH process per patient, including documentation in the EMR, was 15 minutes (interquartile range [IQR], 10–20 minutes).
There were a total of 309 discrepancies discovered as seen in the Figure. These included missing medication (n=101, 32.7%), other (n=78, 25.2%), omitted information (n=69, 22.3%), incorrect dose (n=26, 8.4%), incorrect frequency (n=18, 5.8%), incorrect medication (n=9, 2.9%), and incorrect route (n=8, 2.6%). Most discrepancies in the “other” category included medications listed on the patient's PTA medications that he or she was no longer taking.
Figure.
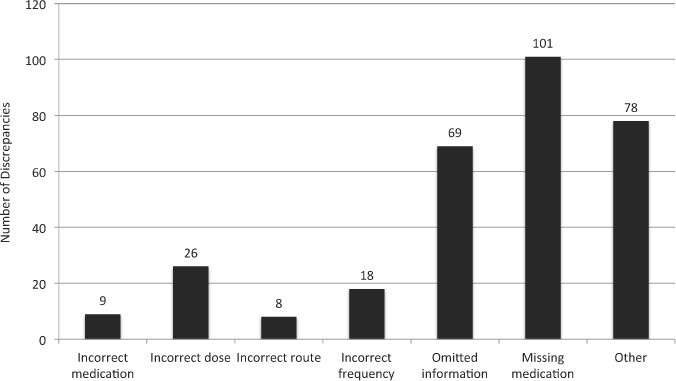
The number of discrepancies identified in each prespecified category.
Of the 87 subjective accuracy scores documented, the mean score was 4.25 ± 1.1, which included a score of 1 (n=5), 2 (n=2), 3 (n=8), 4 (n=22), and 5 (n=50). This indicates overall the pharmacists felt the information obtained was accurate. A total of 30 interventions were made to the medical team; however, only 57 MH forms contained documentation of the number of interventions. Interventions were made for a total of 11 patients with a median of 1 intervention per patient (IQR, 1–5).
DISCUSSION
When comparing pharmacist-obtained MHs with those obtained by physicians and nurses, a total of 309 discrepancies were discovered. There was a median of 2 discrepancies per patient (IQR, 1–4). Most discrepancies were missing medications, which indicated a patient was taking a medication at home that had not been documented in the PTA medication list. Examples of these in this pilot included antiepileptics, insulin, inhaled medications for asthma, and medications to treat gastrointestinal reflux. Pharmacists were able to fill in omitted information 69 times. This included providing the dose, frequency, and/or directions for use.
Thirty interventions were documented as being made to the medical team; however, this was likely underreported. With only 57 of the 100 MH forms indicating this number, it is unknown if any interventions were made for the remaining 43 patients. This is likely related to the location of this data point on the standardized MH form used. However, many clinically significant discrepancies were identified and intervened on by a pharmacist, including correcting the dose of antiepileptic medications, bosentan, sildenafil, and methotrexate; identifying missing medications such as clonazepam and clonidine; and discontinuing medications that had been ordered as inpatient orders and that the patient was no longer taking, such as phenobarbital. These examples serve as supporting evidence that pharmacists had a key role in potentially preventing serious adverse drug reactions from occurring for many of these patients.
The median time of 15 minutes per patient to complete the 5-step process of collecting and documenting the MH and MR was also likely underestimated. The range of time recorded was 5 to 210 minutes; however, it was documented on 18 of the 100 MH forms that the process only took 5 minutes. To complete this process, more than 5 minutes is required.
Several limitations were identified in our study. Incomplete documentation prevented a more thorough evaluation of all aspects of the pharmacist-obtained admission MH and MR process. There was also no objective assessment of the clinical significance of discrepancies identified; however, a subjective accuracy assessment score was implemented to help decipher the reliability of information obtained by pharmacists. In future data collection, we will consider using the National Coordinating Council for Medication Error Reporting and Prevention index for categorizing medication errors to assess the magnitude of discrepancies discovered.10 In this pilot, pharmacist-gathered data were assumed to be the most accurate. Finally, different pharmacists were involved in obtaining MHs and performing MR. Pharmacy residents completed 92 MHs, while a clinical specialist completed 8. Even though universal written and verbal training was provided to all pharmacists involved in this process, differences in technique could have contributed to differences in the amount of medication information collected.
CONCLUSIONS
After evaluating 100 MHs, pharmacists identified and corrected a total of 309 discrepancies when pharmacist-obtained information was compared to physician- and nurse-obtained information. A median of 2 discrepancies per patient was identified by pharmacists in the documented PTA medication information. The most common discrepancy discovered was a missing medication. Examples of discrepancies identified, such as inaccurate antiepileptic regimens, provide evidence that pharmacist involvement in obtaining admission MHs and performing MR has the potential to prevent potentially significant adverse drug reactions and to have a positive impact on patient care. Additionally, this study suggests that pharmacists have the potential to significantly enhance patient care at various transition points as evidenced by the additional information obtained while performing admission MH and MR.
ACKNOWLEDGMENT
The results of this study were presented at the 2012 Residency Project Showcase at the Pediatric Advocacy Group Conference in Houston, Texas.
ABBREVIATIONS
- AIDS
acquired immunodeficiency syndrome
- ED
emergency department
- EMR
electronic medical record
- IQR
interquartile range
- MH
medication history
- MR
medication reconciliation
- PTA
prior to admission
Footnotes
DISCLOSURE The authors declare no conflicts or financial interest in any product or service mentioned in the manuscript, including grants, equipment, medications, employment, gifts, and honoraria.
REFERENCES
- 1.Baker GR, Norton PG, Flintoft V et al. The Canadian adverse events study: the incidence of adverse events among hospital patients in Canada. CMAJ. 2004;170(11):1678–1686. doi: 10.1503/cmaj.1040498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kohn LT, Corrigan JM, Donaldson MS, editors. To Err is Human: Building a Safer Health System. Washington, DC: The National Academies Press; 2000. [PubMed] [Google Scholar]
- 3.Murff HJ, Pepper GA, Kuo GM. Medication errors: incidence and cost. In: Aspden P, Wolcott JA, Bootman JL, editors. Preventing Medication Errors. Washington, DC: The National Academies Press; 2007. pp. 105–141. Pages. [Google Scholar]
- 4.Lau HS, Florax C, Porsius AJ et al. The completeness of medication histories in hospital medical records of patients admitted to general internal medicine wards. Br J Clin Pharmacol. 2000;49(6):597–603. doi: 10.1046/j.1365-2125.2000.00204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carter MK, Allin DM, Scott LA et al. Pharmacist-acquired medication histories in a university hospital emergency department. Am J Health Syst Pharm. 2006;63(24):2500–2503. doi: 10.2146/ajhp060028. [DOI] [PubMed] [Google Scholar]
- 6.Institute for Healthcare Improvement. Getting started kit: prevent adverse drug events. http://www.ihi.org/knowledge/Pages/Tools/MedicationReconciliationReview.aspx. Accessed October 14, 2011.
- 7.Reeder TA, Mutnick A. Pharmacist-versus physician-obtained medication histories. Am J Health Syst Pharm. 2008;65(9):857–860. doi: 10.2146/ajhp070292. [DOI] [PubMed] [Google Scholar]
- 8.Coffey M, Mack L, Streienberger K et al. Prevalence and clinical significance of medication discrepancies at pediatric hospital admission. Acad Pediatr. 2009;9(5):360–365. doi: 10.1016/j.acap.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 9.Stone BL, Boehme S, Mundorff MB et al. Hospital admission medication reconciliation in medically complex children: an observational study. Arch Dis Child. 2010;95(4):250–255. doi: 10.1136/adc.2009.167528. [DOI] [PubMed] [Google Scholar]
- 10.National Coordinating Council for Medication Error Reporting and Prevention. NCC MERP index for categorizing medication errors. http://www.nccmerp.org/pdf/indexColor2001-06-12.pdf. Accessed January 14, 2013.


