Abstract
Hepatic epithelioid hemangioendothelioma (HEH) is a rare neoplasm of vascular origin with variable malignant potential. Because most patients with this condition have multiple bilobar lesions, liver transplantation is the standard treatment, and hepatectomy is much less frequently indicated. We describe a case of a 35-year-old woman with unresectable multiple bilobar HEH successfully treated by combination treatment with hepatectomy and carbon-ion radiotherapy. This case is very meaningful since it demonstrated the effectiveness of carbon-ion radiotherapy for HEH and the possibility of expanding the curative treatment options for multiple bilobar hepatic tumors.
Keywords: Two-stage treatment, Hepatic epithelioid hemangioendothelioma, Hepatectomy, Carbon-ion radiotherapy, Particle radiotherapy, Omental flap spacer
Core tip: Hepatic epithelioid hemangioendothelioma (HEH) is a rare neoplasm with variable malignant potential. Liver transplantation is the most frequently reported treatment because most patients have multifocal bilobar lesions. Here, we describe a case of a 35-year-old woman with unresectable multiple bilobar HEH that was successfully treated by combination treatment of hepatectomy and carbon-ion radiotherapy. This case demonstrated two significant points: the effectiveness of carbon-ion radiotherapy for HEH and the possibility of expanding the curative treatment options for multiple bilobar hepatic tumors.
INTRODUCTION
Hepatic epithelioid hemangioendothelioma (HEH) is a rare vascular tumor characterized by the presence of epithelioid endothelial cells[1,2], which presents varying clinical behaviors reflecting borderline malignancy to aggressive disease. Although several nonsurgical modalities such as chemotherapy, radiotherapy, interferon treatment, antiangiogenic chemotherapy, or transcatheter arterial chemoembolization (TACE) has been explored[3-5], surgical treatments by liver transplantation (LT) or hepatectomy remains the mainstay of treatment for patients with HEH[1]. Here, we report a case of unresectable multiple bilobar HEH that showed complete remission after combination treatment with hepatectomy and carbon-ion radiotherapy. To our knowledge, this is the first case report describing the application of particle radiotherapy in the treatment of this rare hepatic malignant tumor.
CASE REPORT
A 35-year-old female patient was admitted to our department for the surgical treatment of multiple bilobar liver tumors. Four years previously, a routine medical examination had revealed multiple liver tumors, the largest measuring 36 mm in diameter. A histological diagnosis of HEH had been made by fine needle tumor biopsy. Because she had been in the late stage of pregnancy and chest computed tomography (CT) had shown the presence of multiple small nodules in both lungs, the patient was closely followed up by CT every 4 mo. After a normal delivery, both liver and lung tumors did not show any obvious signs of growth until CT showed enlargement of the liver tumor (segment 6) from 36 to 43 mm in diameter. Laboratory data did not indicate any abnormality; the patient was negative for hepatitis B and C virus infection and the serum levels of tumor markers, including α-fetoprotein, prothrombin induced by vitamin K absence or antagonist II, carcinoembryonic antigen, carbohydrate antigen 19-9, and carbohydrate antigen 125, were within normal ranges. The patient had no remarkable medical, surgical, or family history. Abdominal CT showed a total of seven tumors in both lobes, suggestive of an unresectable disease stage (Figure 1). LT was not indicated because of the unavailability of a living donor candidate and a cadaveric donor was unavailable as per the donor organ allocation policy of the Japan Society for Transplantation and organ shortage in Japan. Accordingly, we opted for a treatment strategy that involved right hemihepatectomy and partial resection of the left lateral segment followed by particle radiotherapy to the residual and solitary tumor in segment 4. Furthermore, the residual tumor was predicted to be close to the transection surface to which the colon would adhere and would hamper postoperative radiotherapy. Therefore, we planned to cover the cut surface using an omental flap to ensure spacing between the tumor and bowels.
Figure 1.
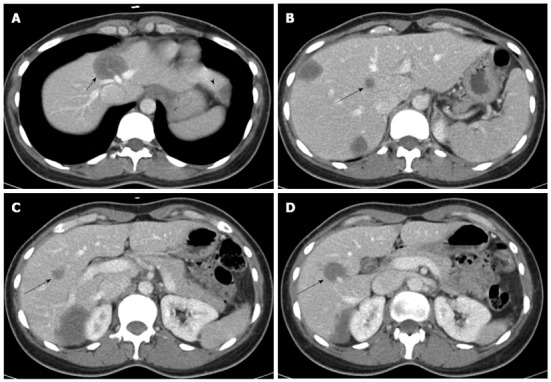
Abdominal computed tomography revealed a total of 7 lesions located in both lobes. A: The tumor of segment 4 (short arrow) hinders the possibility of right hemihepatectomy, because it invades the roots of the middle and left hepatic veins (arrowhead indicates the tumor of segment 3); B-D: The 3 deep-seated tumors in the right lobe (long arrows) hinder the possibility of left hemihepatectomy.
At laparotomy, multiple well-delineated white nodules were seen on the liver surface (Figure 2A). The tumor of segment 6 adhered firmly to Gerota’s fascia (Figure 2B), indicating its invasive nature. We performed right lobectomy with excision of the infiltrated portion of Gerota’s fascia as well as partial hepatectomy of segment 3 (Figure 2C) and then placed the omental flap on the cut surface of the liver (Figure 2D) for spacing. Moreover, to prevent postoperative irradiation to the pericardium, the round ligament was placed below the diaphragm (Figure 2D). Histopathological examination revealed atypical cells containing many vacuolated cells and dendritic cells, and the neoplastic cells were positive for vimentin, factor VIII-related antigen, CD31, and CD34, leading to the establishment of a definite diagnosis of HEH (Figure 3).
Figure 2.
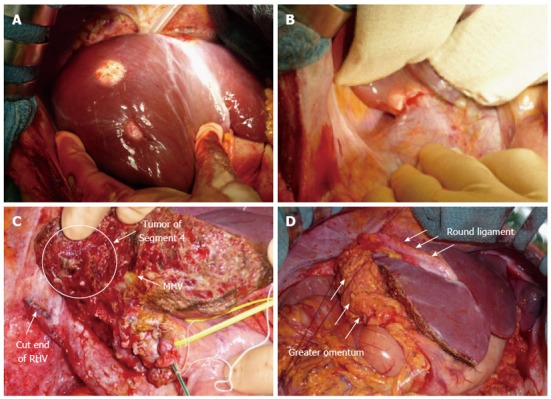
Intraoperative images. A: The tumors were well-circumscribed, whitish, and firm; B: The tumor of segment 6 invaded Gerota’s fascia; C: After right lobectomy, the tumor of segment 4 was very close to the cut surface of the liver; D: A flap of the greater omentum (arrows) was sutured over the cut surface of the liver to cover the tumor of segment 4. MHV: Middle hepatic vein; RHV: Right hepatic vein.
Figure 3.
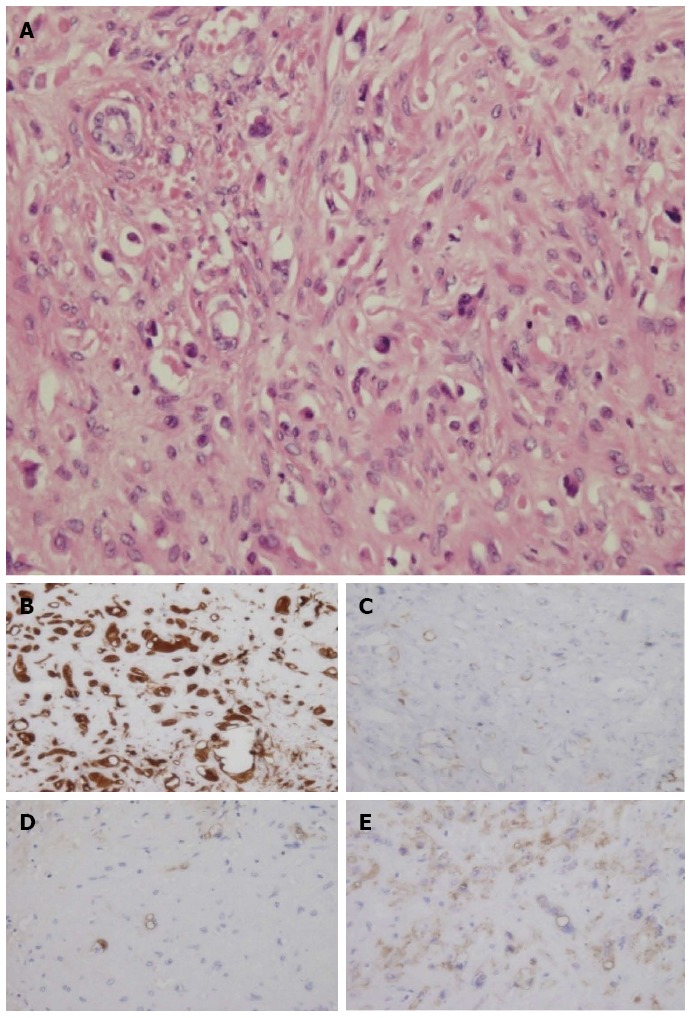
Pathological findings. A: The specimen was composed of many atypical vacuolatd and dendritic cells; B-E: The tumor cells were immunoreactive for vimentin (B), factor VIII-related antigen (C), CD31 (D), and CD34 (E).
Abdominal CT after the operation showed that the omental flap was maintaining sufficient space between the tumor and the gastrointestinal tract (Figure 4A). The postoperative course was uneventful, and the patient was discharged on postoperative day 12. One month after the hepatectomy, carbon-ion radiotherapy of 76 GyE (gray equivalents) was administered in 20 fractions over 30 d (Figure 4B). No acute or late treatment-related toxicities (grade ≥ 2) were observed, and the liver function test results were normal. Follow-up imaging studies showed gradual regression of the tumor until 2 years after irradiation, and no enlargement or vascularity was observed thereafter, indicating complete local control (Figure 4C-E). Chest CT showed no changes in the small lung nodules. The patient remains free of recurrence almost 4 years after combination treatment.
Figure 4.
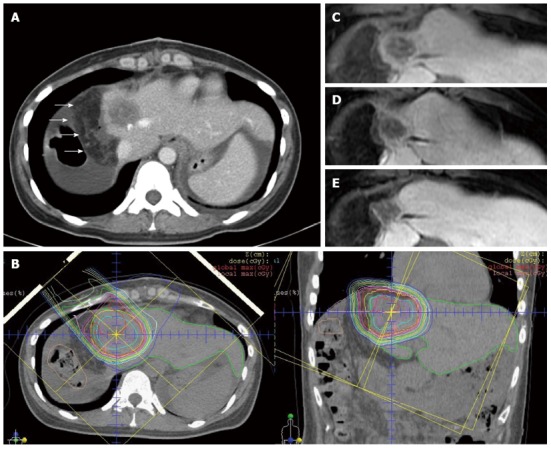
Treatment course. A: Post-operative abdominal computed tomography (CT) showed the greater omental flap (arrows) around the tumor, maintaining a sufficient space between the tumor and the gastrointestinal tract; B: Treatment plan for carbon-ion radiotherapy with a total dose of 76 GyE in 20 fractions. Isodose lines demonstrate 100% of the prescribed dose at the center and decreasing by 10% of the dose from the inside to the outside. Owing to the greater omental flap, the tumor was entirely irradiated with full dose, and the gastrointestinal tract was successfully spared; C: Comparison of abdominal CT and magnetic resonance imaging scans taken over a period of 24 mo after carbon-ion radiotherapy indicated shrinkage of the tumor with decreasing tumor vascularity. The maximum tumor diameter was 35 mm before treatment, and tumor size decreased thereafter to 27 mm after 6 mo; D: Tumor size of 26 mm after 12 mo; E: Tumor size of 24 mm after 24 mo.
DISCUSSION
Surgical intervention has been accepted as first-line treatment, and several studies have suggested that even extrahepatic disease is not a contraindication for surgical treatment[1,6,7]. However, a clear indication for either LT or hepatectomy has yet to be determined. Orthotopic LT has been most frequently indicated in the Western world with good outcomes[8] because > 80% of patients have multiple bilobar lesions at the time of diagnosis[1]. Lerut et al[6] reviewed the cases of 59 patients from the European Transplant Registry and reported 5- and 10- year survival rates of 83% and 72%, respectively, with disease-free survival rates of 82% and 64%, respectively. The United Network for Organ Sharing Registry reported a 5-year survival rate of 64% among 110 patients who underwent LT[9]. In contrast, hepatectomy has been indicated in only a small proportion of patients with limited unilobar disease[1,10]. Mehrabi et al[1] pooled 434 cases from the literature and reported that hepatectomy was performed in only 9.4% (22 patients) of these cases, whereas LT was performed in 45% (110 patients). Nevertheless, it is noteworthy that cases for which hepatectomy was performed with curative intent showed the best 5-year survival rate of 75% compared to 54.5% for cases of LT and 30% for cases of chemotherapy and/or radiation. In this regard, Grotz et al[7] from the Mayo Clinic recently reported comparable results with hepatectomy (11 patients) and LT (11 patients) and suggested that hepatectomy was appropriate for patients with resectable disease, even for those with bilobar lesions by parenchyma-saving resection (partial hepatectomy). They also analyzed the favorable predictive factors such as the largest tumor diameter of ≤ 10 cm and multifocal disease with ≤ 10 nodules. In any case, our patient had unresectable disease because the presence of the tumor in segment 4 and the central location of multiple tumors in the right lobe hindered parenchyma-saving resection and negatively affected the possibility of curative resection by either right or left hemihepatectomy, respectively (Figure 1). Although LT would have been indicated, it is not feasible in Japan unless a living donor is available.
A combination of left hemihepatectomy and radiofrequency ablation was a possible alternative approach but was not suitable in our case. Radiofrequency ablation was relatively contraindicated because of the tumor sizes and the perivascular location, which has been reported to increase the local recurrence rate due to the heat-sink effect[11,12]. Conventional radiotherapy is not usually indicated for multiple lesions because of excessive normal liver tissue toxicities. None of the other nonsurgical therapeutic modalities has been widely accepted since there is little evidence of their efficacy, because of the rarity of this disease. However, TACE was recently recommended by a few researchers. Wang et al[13] reported comparable results with hepatectomy (17 patients) and TACE (12 patients), with 3-year survival rates of 74.1% and 81.6%, respectively. Cardinal et al[5] reported better results with TACE in patients with metastatic diseases than with LT or hepatectomy in a retrospective study including 25 patients, even though the TACE arm included only four patients.
There are even patients in the spontaneous course alive after 5 years without treatment[2,14], indicating the borderline malignant nature of the disease resembling neuroendocrine tumors where patients even with metastases maintains stable disease for years. In fact, our patient has been stable for at least 4 years. However, further investigations are needed to clarify whether such nonsurgical interventions indeed influence the patients’ natural history. Nonetheless, since the biological and clinical behaviors of HEH are varied and unpredictable, no clinical or pathological prognostic factors have yet been identified. Thus, we opted for the more curative treatment option, and consequently chose to administer particle radiotherapy to the single residual lesion in segment 4 following right hemihepatectomy and partial hepatectomy.
Particle radiotherapy using protons or carbon-ions is a new modality that elicits an inherent antitumor effect against various malignant tumors[15]. Owing to the defined range of protons or carbon-ions as exhibited by the Bragg peak, they allow reduction of the irradiated volume and the dose administered to the normal tissues[15,16]. Hepatocellular carcinoma (HCC) is one of the malignancies most suitable for treatment with particle radiotherapy. We recently reported good clinical treatment results with particle radiotherapy for HCC with a local control rate of approximately 90%, indicating that particle radiotherapy may be a useful alternative to conventional local therapies[17,18]. Further, due to our abundant experience with particle radiotherapy for HCC[17], we believe that HEH could be controlled as long as a sufficient dose is administered.
Particle radiotherapy is generally not recommended for tumors that are adjacent to the gastrointestinal tract because the dose tolerated by the intestine is extremely low[19,20]. Unlike conventional photon radiotherapy, a distance of only 5-10 mm between the tumor and the gastrointestinal tract is sufficient for safe and curative irradiation with particle radiotherapy. In our case, we avoided potential bowel adherence to the target lesions using an omental flap as a spacer intraoperatively to facilitate irradiation after hepatectomy. We recently reported the effectiveness of a new two-step treatment with surgical prosthetic spacer placement and subsequent particle radiotherapy for HCC or pelvic malignancies[21,22]. These spacing techniques provide new strategies for radical treatment with radiotherapy.
In summary, this case report described two new important findings: the effectiveness of carbon-ion radiotherapy for HEH and the efficacy and safety of a new strategy for managing multiple bilobar hepatic tumors by combining hepatectomy and particle radiotherapy. These findings provide a new treatment option for HEH and multiple bilobar hepatic tumors.
COMMENTS
Case characteristics
A 35-year-old female patient presented with no sign of subjective symptoms.
Clinical diagnosis
The patient was diagnosed as multiple bilobar hepatic epithelioid hemangioendotheliomas.
Differential diagnosis
Hepatocellular carcinoma, metastatic liver tumor.
Laboratory diagnosis
The patient was negative for hepatitis B and C virus infection and the serum levels of tumor markers, including α-fetoprotein, prothrombin induced by vitamin K absence or antagonist II, carcinoembryonic antigen, carbohydrate antigen 19-9, and carbohydrate antigen 125, were within normal ranges.
Imaging diagnosis
Abdominal CT showed a total of seven liver tumors in both lobes, and the maximal tumor size was 43 mm in diameter.
Pathological diagnosis
Histopathological examination revealed atypical cells containing many vacuolated cells and dendritic cells, and neoplastic cells were positive for vimentin, factor VIII-related antigen, CD31, and CD34, resulting in the definite diagnosis of hepatic epithelioid hemangioendothelioma.
Treatment
The patient was treated with right hemihepatectomy and partial resection of the left lateral segment followed by particle radiotherapy to the residual and solitary tumor in segment 4.
Related reports
Hepatic epithelioid hemangioendothelioma is a rare vascular tumor that occurs exclusively in adults, but there have been few reports describing effective alternative treatment option except for liver transplantation or hepatectomy because of its rarity.
Term explanation
Particle radiotherapy, such as proton or carbon-ions, is a new modality that allows reduction of the irradiated volume and the dose administered to the normal tissues owing to the excellent dose distribution.
Experiences and lessons
This case report provides a new treatment option for hepatic epithelioid hemangioendothelioma and multiple bilobar hepatic tumors.
Peer review
Although this is only a single case report that lack convincing evidence of benefit, our treatment strategy may have a possibility to expand the treatment options for hepatic epithelioid hemangioendothelioma and multiple bilobar hepatic tumors.
Footnotes
P- Reviewers: Akyuz U, Fernandez-Pineda I, Kapischke M S- Editor: Qi Y L- Editor: A E- Editor: Wang CH
References
- 1.Mehrabi A, Kashfi A, Fonouni H, Schemmer P, Schmied BM, Hallscheidt P, Schirmacher P, Weitz J, Friess H, Buchler MW, et al. Primary malignant hepatic epithelioid hemangioendothelioma: a comprehensive review of the literature with emphasis on the surgical therapy. Cancer. 2006;107:2108–2121. doi: 10.1002/cncr.22225. [DOI] [PubMed] [Google Scholar]
- 2.Makhlouf HR, Ishak KG, Goodman ZD. Epithelioid hemangioendothelioma of the liver: a clinicopathologic study of 137 cases. Cancer. 1999;85:562–582. doi: 10.1002/(sici)1097-0142(19990201)85:3<562::aid-cncr7>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 3.Bocci G, Nicolaou KC, Kerbel RS. Protracted low-dose effects on human endothelial cell proliferation and survival in vitro reveal a selective antiangiogenic window for various chemotherapeutic drugs. Cancer Res. 2002;62:6938–6943. [PubMed] [Google Scholar]
- 4.Galvão FH, Bakonyi-Neto A, Machado MA, Farias AQ, Mello ES, Diz ME, Machado MC. Interferon alpha-2B and liver resection to treat multifocal hepatic epithelioid hemangioendothelioma: a relevant approach to avoid liver transplantation. Transplant Proc. 2005;37:4354–4358. doi: 10.1016/j.transproceed.2005.11.022. [DOI] [PubMed] [Google Scholar]
- 5.Cardinal J, de Vera ME, Marsh JW, Steel JL, Geller DA, Fontes P, Nalesnik M, Gamblin TC. Treatment of hepatic epithelioid hemangioendothelioma: a single-institution experience with 25 cases. Arch Surg. 2009;144:1035–1039. doi: 10.1001/archsurg.2009.121. [DOI] [PubMed] [Google Scholar]
- 6.Lerut JP, Orlando G, Adam R, Schiavo M, Klempnauer J, Mirza D, Boleslawski E, Burroughs A, Sellés CF, Jaeck D, et al. The place of liver transplantation in the treatment of hepatic epitheloid hemangioendothelioma: report of the European liver transplant registry. Ann Surg. 2007;246:949–957; discussion 957. doi: 10.1097/SLA.0b013e31815c2a70. [DOI] [PubMed] [Google Scholar]
- 7.Grotz TE, Nagorney D, Donohue J, Que F, Kendrick M, Farnell M, Harmsen S, Mulligan D, Nguyen J, Rosen C, et al. Hepatic epithelioid haemangioendothelioma: is transplantation the only treatment option? HPB (Oxford) 2010;12:546–553. doi: 10.1111/j.1477-2574.2010.00213.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agrawal N, Parajuli S, Zhao P, Satoskar R, Laurin J, Azumi N, Matsumoto C, Shetty K. Liver transplantation in the management of hepatic epithelioid hemangioendothelioma: a single-center experience and review of the literature. Transplant Proc. 2011;43:2647–2650. doi: 10.1016/j.transproceed.2011.06.035. [DOI] [PubMed] [Google Scholar]
- 9.Rodriguez JA, Becker NS, O’Mahony CA, Goss JA, Aloia TA. Long-term outcomes following liver transplantation for hepatic hemangioendothelioma: the UNOS experience from 1987 to 2005. J Gastrointest Surg. 2008;12:110–116. doi: 10.1007/s11605-007-0247-3. [DOI] [PubMed] [Google Scholar]
- 10.Mosoia L, Mabrut JY, Adham M, Boillot O, Ducerf C, Partensky C, Baulieux J. Hepatic epithelioid hemangioendothelioma: long-term results of surgical management. J Surg Oncol. 2008;98:432–437. doi: 10.1002/jso.21132. [DOI] [PubMed] [Google Scholar]
- 11.Mulier S, Ni Y, Jamart J, Ruers T, Marchal G, Michel L. Local recurrence after hepatic radiofrequency coagulation: multivariate meta-analysis and review of contributing factors. Ann Surg. 2005;242:158–171. doi: 10.1097/01.sla.0000171032.99149.fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berber E, Siperstein A. Local recurrence after laparoscopic radiofrequency ablation of liver tumors: an analysis of 1032 tumors. Ann Surg Oncol. 2008;15:2757–2764. doi: 10.1245/s10434-008-0043-7. [DOI] [PubMed] [Google Scholar]
- 13.Wang LR, Zhou JM, Zhao YM, He HW, Chai ZT, Wang M, Ji Y, Chen Y, Liu C, Sun HC, et al. Clinical experience with primary hepatic epithelioid hemangioendothelioma: retrospective study of 33 patients. World J Surg. 2012;36:2677–2683. doi: 10.1007/s00268-012-1714-x. [DOI] [PubMed] [Google Scholar]
- 14.Otrock ZK, Al-Kutoubi A, Kattar MM, Zaatari G, Soweid A. Spontaneous complete regression of hepatic epithelioid haemangioendothelioma. Lancet Oncol. 2006;7:439–441. doi: 10.1016/S1470-2045(06)70697-0. [DOI] [PubMed] [Google Scholar]
- 15.Schulz-Ertner D, Tsujii H. Particle radiation therapy using proton and heavier ion beams. J Clin Oncol. 2007;25:953–964. doi: 10.1200/JCO.2006.09.7816. [DOI] [PubMed] [Google Scholar]
- 16.Brada M, Pijls-Johannesma M, De Ruysscher D. Proton therapy in clinical practice: current clinical evidence. J Clin Oncol. 2007;25:965–970. doi: 10.1200/JCO.2006.10.0131. [DOI] [PubMed] [Google Scholar]
- 17.Komatsu S, Fukumoto T, Demizu Y, Miyawaki D, Terashima K, Sasaki R, Hori Y, Hishikawa Y, Ku Y, Murakami M. Clinical results and risk factors of proton and carbon ion therapy for hepatocellular carcinoma. Cancer. 2011;117:4890–4904. doi: 10.1002/cncr.26134. [DOI] [PubMed] [Google Scholar]
- 18.Komatsu S, Murakami M, Fukumoto T, Hori Y, Hishikawa Y, Ku Y. Risk factors for survival and local recurrence after particle radiotherapy for single small hepatocellular carcinoma. Br J Surg. 2011;98:558–564. doi: 10.1002/bjs.7397. [DOI] [PubMed] [Google Scholar]
- 19.Ishikawa H, Tsuji H, Kamada T, Hirasawa N, Yanagi T, Mizoe JE, Akakura K, Suzuki H, Shimazaki J, Tsujii H. Risk factors of late rectal bleeding after carbon ion therapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2006;66:1084–1091. doi: 10.1016/j.ijrobp.2006.06.056. [DOI] [PubMed] [Google Scholar]
- 20.Kawashima M, Furuse J, Nishio T, Konishi M, Ishii H, Kinoshita T, Nagase M, Nihei K, Ogino T. Phase II study of radiotherapy employing proton beam for hepatocellular carcinoma. J Clin Oncol. 2005;23:1839–1846. doi: 10.1200/JCO.2005.00.620. [DOI] [PubMed] [Google Scholar]
- 21.Fukumoto T, Komatsu S, Hori Y, Murakami M, Hishikawa Y, Ku Y. Particle beam radiotherapy with a surgical spacer placement for advanced abdominal leiomyosarcoma results in a significant clinical benefit. J Surg Oncol. 2010;101:97–99. doi: 10.1002/jso.21417. [DOI] [PubMed] [Google Scholar]
- 22.Komatsu S, Hori Y, Fukumoto T, Murakami M, Hishikawa Y, Ku Y. Surgical spacer placement and proton radiotherapy for unresectable hepatocellular carcinoma. World J Gastroenterol. 2010;16:1800–1803. doi: 10.3748/wjg.v16.i14.1800. [DOI] [PMC free article] [PubMed] [Google Scholar]


