Abstract
Background:
The risks of repeat concussions and returning to play (RTP) prior to the resolution of concussive symptoms are medically established. However, RTP guidelines for high school sports are varied and often notably absent. The island of Guam, a US territory, has a robust athletics program but lacks structure to reduce concussions or establish RTP protocols. Consequently, there is an opportunity to limit the incidence of “second-hit syndrome” and other harmful effects through education and testing.
Methods:
We evaluated the feasibility of Sideline Concussion Testing SCT) as a novel feature of Guam high school athletics. Thirteen high school football players were observed over three consecutive football games. They were first given a questionnaire about concussion history, symptoms, medical evaluation, and RTP. Researchers used the King–Devick Test, a SCT tool, and baseline scores were recorded. If players were then observed to have significant head trauma or to show concussive symptoms, they were sidelined and tested.
Results:
Five of 13 students had a previous concussion and limited awareness of RTP guidelines. Of those five, four received no medical consultation or stand down period before RTP. There was also a lack of understanding of what constitutes a concussion; five out of eight individuals who denied previous concussion confirmed having bell ringers, seeing stars, and other classic concussive symptoms. Over the course of the study the SCT identified three concussions, with significant deviations from baseline time on a test that measured visual and speech disturbances.
Conclusions:
The feasibility of SCT use in Guam high school football was established and our pilot study identified areas for improvement. Established definitions of concussion and RTP guidelines were lacking. Therefore, an opportunity exists through public health efforts that involve the entire community to increase concussion awareness and reduce injuries in high school sports on Guam.
Keywords: Adolescent, athletics, concussion, football, Guam, head injury, public health
INTRODUCTION
Despite the numerous benefits of athletics for children and adolescents, the unique risks of concussion on the developing brain are a genuine health concern that is driving change in high school sports.[1,5,15,18] At the forefront are contact sports, and most medical and sports societies now offer definitions of concussive events and guidelines for return to play (RTP).[10,13,20] The risks of repeated concussions and the dangers of RTP prior to complete resolution of the concussive symptoms are firmly established, and ongoing research continues to add new information to formal guidelines in the future.[10,11,20] However, the success of implementing these guidelines throughout high school sports programs has been mixed. Cultural, economic, and regional variables have all been proposed as causes.[4,16]
The unincorporated US territory of Guam is located in the Pacific Ocean, 6000 miles west of the continental United States. The Micronesian island has a population of approximately 170,000 people comprised mostly of the indigenous Chamorro population, as well as other Pacific Islanders and Asians.[3,9,17] There are six public high schools in Guam for adolescents aged 14-18 years, and enrollment is compulsory until they complete grade 12. As Guam's adolescent population grows,[2,17] so does their participation in interscholastic sports, but at present, the schools in Guam have no formal guidelines to reduce concussion, or to delay RTP after a concussion has occurred. Given this lack, and the recent advancements in concussion research, Guam may benefit from increasing high school awareness of concussions, and a more formalized program to reduce them, in order to limit the potential long-term deleterious effects of concussions on Guam's youth.
During the 2013-2014 high school football season, we evaluated the feasibility of performing Sideline Concussion Testing (SCT) at high school games. We first established preseason baseline testing with the King-Devick Test (KDT), a rapid concussion assessment tool that evaluates deficiencies in visual tracking and saccadic eye movement (shown to be one indicator of mild traumatic brain injury [TBI]). Using this test and our baselines, we then examined the effectiveness of sideline testing for identifying concussions on the field, and evaluated the feasibility of implementing standardized SCT. Although the school administration and coaching staff strongly supported the project, there were several players and their parents who chose not to participate for various reasons. We found that SCT testing was feasible, and during the process we identified several areas for improvement in education and the process of implementing SCT and RTP.
MATERIALS AND METHODS
Participants
The target group of the study included 13 high school football players from the same team, whose median age was 16.5 (±2) years, and who were observed over a period of three consecutive football games. Prior to any research, approvals were obtained from the school administration and coaching staff and all subjects were required to obtain informed consent form their parents (Supplemental Material 1) before participating in the research study.
Concussion definition
Despite recent increased awareness of head injury and its harmful effects, there remains a wide spectrum of understanding of the term “concussion” and the diagnosis, recovery, and underlying brain pathology that is associated with it.[16,20] For this study, concussion is defined as a traumatically induced, temporary disturbance of brain function, which is a subset of mild TBI that generally falls on the milder end of the brain injury spectrum, and is a complex pathophysiological process.
Previous history questionnaire
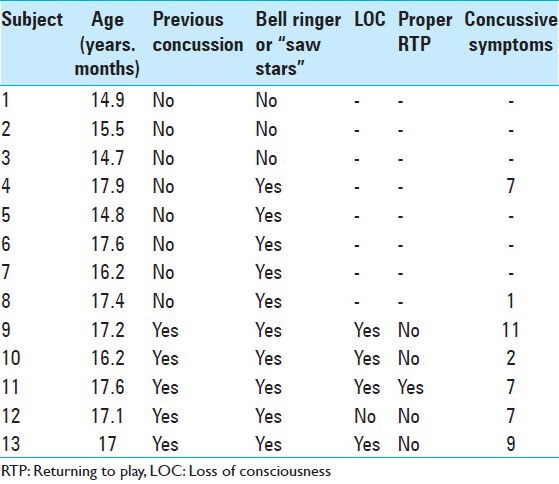
The initial step in the study was for the high school athletes to complete a past-history questionnaire (Supplemental Material 2) about any prior concussions, injuries, and their health in general [Table 1]. The questionnaires specifically asked about previous concussions received, loss of consciousness, other symptoms, medical clearance to return to play, and other RTP procedures.
Table 1.
Past-history questionnaire data
Baseline testing
Prior to playing, participants were tested using the King–Devick sideline concussion-screening test to establish baselines. The KDT is a physical and objective method of evaluating the visual tracking and saccadic eye movements of a subject while they perform a timed rapid number naming test.[6,7,8] The participant is given a series of three test cards and must read aloud a sequence of single digit numbers from top to bottom, and left to right as quickly as possible without making any errors. The test administrator follows along and records any errors, and also times the test if they are using the physical placard version. The total time taken to complete the three test cards is recorded as the summary score for the entire test.
Match and postmatch testing
After baseline values were determined, the participants were observed over a series of three football games. Over the course of a game, if a player was seen to get “dinged”, receive a direct blow to the head, or rise slowly or unsteadily following a collision, they were removed from the game and given the SCT. At the conclusion of the match, all players were tested in order to pick up any potentially unrecognized concussive events. If a player failed the SCT, they were not returned to play and were advised to consult a medical professional before returning to the field again.
RESULTS
Population analyzed
Out of 43 football athletes from one Guam high school who were asked to participate in the study, 13 agreed. The players were all male and their median age was 16.5 (±2) years old. A large proportion of players who did not participate said they were reluctant to be involved in the study because it might be used later by the coaching staff to prevent them from playing, or would be kept as records and used by the administration to prevent them playing other sports. Others said their parents refused to sign the informed consent form because they did not want their children involved in a concussion study, or they were concerned that records of concussive events could be used against their children during college recruiting or by the school administration. The researchers felt that a general lack of understanding about the project and the purpose of the concussion study might have contributed to their reluctance to participate. However, as the study progressed and several players were tested, researchers observed increasing tolerance for the test administrators at the football games as both players and parents saw the potential value in concussion testing and RTP procedures.
Past-history questionnaire
The past-history questionnaire was given to all participants, prior to baseline testing, to evaluate their general knowledge about concussion and establish prior concussive history [Table 1]. Out of the 13 participants, 5 answered “yes” when asked if they had a previous concussion due to sport, with each reporting an average of 7.2 postconcussive symptoms. One of the most informative results of the questionnaire was the lack of adolescent awareness and their knowledge of what constituted a concussion. Five out of eight participants who answered “no” to having had a previous concussion answered “yes” to having incidents in sport that were described as “bell ringers,” “seeing stars,” or feeling dizzy when getting up after a blow to the head. In addition, two of these individuals also described having symptoms that are associated with concussion and TBI.
The questionnaire also revealed there was a lack of established or uniform RTP guidelines following a concussive event. In fact four out of five individuals with previous concussions due to sport answered “no” to consulting a medical professional that would have required a period of contact sport cessation of contact before returning to the field.
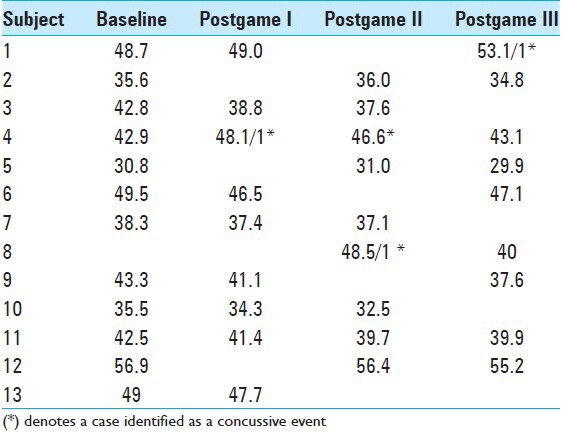
Sct baseline readings and postinjury data
The KDT was selected as the leading SCT tool[6,7,8] due to its ease of administration and the short time required by individuals to take the test, compared with other leading sideline diagnostic tools. Over the course of the games observed, we witnessed three concussions, and the players involved were removed from play and given the SCT [Table 2]. All three players showed several symptoms of concussion, made errors in the SCT, and took a significantly longer overall time (+5–8 s) to complete the test. For one player, Subject 8, there was no baseline available. However, testing of this individual 1-week after the concussion showed a significant improvement of 8.5 s without errors. Subject 4, who was identified as concussed Postgame I, also showed marked improvement back to baseline over the course of 2 weeks. All players who were diagnosed as concussed due to the SCT consulted medical professionals before RTP.
Table 2.
Baseline and post-game times (seconds) followed by errors if they occurred
DISCUSSION
The need for reducing concussions in sports is now widely accepted. Although international sports societies have attempted to provide consensus statements for concussions, implementing concussion management and prevention programs in high schools remains highly variable.[8,14,20] Given the long-term neurological consequences resulting from head injuries to the developing adolescent brain, managing and preventing concussion is a major public health concern. The US island territory of Guam was chosen to assess the feasibility of using SCT at high school football games. Based on the changing population dynamics of Guam, the percentage of people that reside in more urban areas is increasing.[2,17] Furthermore, the fraction of the population at high school age is also predicted to increase, as is the expected number of adolescents that enroll in contact sports. Guam presents a unique opportunity to determine if SCT can impact the health of children by allowing them to benefit from athletics, but in an environment that limits the harmful effects of concussions and the severe neurological disability associated with “second hit syndrome.” This syndrome is unique to children but can be prevented by using SCT and following strict RTP guidelines.[5,18,19]
To evaluate the feasibility of SCT in the high school interscholastic football program on Guam, several steps were taken prior to beginning of play. Areas for concern or improvement were identified by meeting with coaches and evaluating student questionnaires about concussion history. We found that despite genuine concern for player safety, there was no consensus or straightforward concept of what constituted a concussion; coaches and parents were unclear of what exactly amounts to significant head injury. The students shared this lack of clarity, some of whom reported “never having had a concussion”, but also recalled symptoms that would qualify them as being concussed. Overall, the status of high school football on Guam is similar to that of the USA several years prior to 2007, when the National Football League (NFL) established guidelines to detect concussions and began campaigning for player safety education.[19] Implementing similar island-wide education and awareness of concussion, combined with more stringent SCT and RTP guidelines, is feasible, and should be considered for the Guam high school football program.
We used the KD sideline-testing tool as our SCT because it had certain logistical advantages and data indicating its efficacy.[6,7,8,12,14] The value of the KD test is in its brevity (2-3 min) and ease of administration. In addition, postinjury recommendations are specific for each player, with respect to their established baseline, which means the test is more IQ-independent and can be performed by most athletes. Furthermore, the test administrator needs no formal or extensive training to use the iPad application or to administer the physical test, which increases the value of KD. It is an SCT that can be administered by coaches, athletic trainers, or parents depending on the resources available to the team.
However, based on our experience the test did have some limitations. Despite the relative ease of the test, the overall times for all tests improved with increased familiarity, suggesting the number of tests used to determine the baseline may need to be increased. In addition, the participant does have the ability to manipulate the baseline time by intentionally performing the test more slowly. Increasing the number of tests to determine the baseline could improve the personalization and test accuracy. Another hurdle with the testing SCT feasibility was missing information. If the test is not made mandatory then some players may not have any baseline information in the event of a concussive episode along with some players who try to avoid test administrators if they feel they may have been injured but do not want to sit out.
The SCT also requires the user to read a series of numbers aloud as quickly as possible without errors, which can be a challenge on the sideline of an ongoing game. We strongly recommend the player be removed from the immediate sideline, so the test can be administered in a location with fewer distractions and limit false positive test results. Finally, it has been widely accepted that neurocognitive testing both preseason and postinjury is the most accepted tool in identifying concussions,[13,14,19] and can address areas that the SCT alone cannot. Therefore, we also strongly recommend that any implementation of SCT should be paired with efforts to perform more in-depth neurocognitive testing of players prior to the beginning season and postinjury for a more nuanced diagnosis to guide RTP decisions.
As discussed earlier, the data revealed a general lack of understanding about what constitutes a concussion, together with the potential to underreport concussive symptoms. The term “concussion” remains nebulous to players, coaches, and parents; although they consider loss of consciousness unequivocally as a concussion, to many of them it is unclear that double vision, new onset headache, slurred speech, or unstable gait are concussive symptoms that should be an immediate trigger for removing the athlete from play. The players themselves stated they wished to compete and were reluctant to be removed from play because they were participating in an optional SCT study. Some players who were receptive to participation had parents who expressed concerns about the data being used to create a “concussion history” that could potentially be used in the future against their children, by the school administration, or during collegiate recruitment. A mandatory SCT program required by Guam schools would remove these obstacles. Furthermore, uniformly applying SCT and RTP guidelines to all students would give coaches objective guidelines for removing an athlete from play based on safety concerns, irrespective of any opposition by the player or parent.
International sports societies are continually promoting and improving concussion awareness and management guidelines. The additive value of neurocognitive testing and increased awareness in order to make better informed RTP decisions in the best interest of the players cannot be understated. This synergistic combination can help prevent the bulk of the more severe multiple concussion issues such as second hit syndrome. These recommendations, however, are not always well established or effective in certain heterogeneous geopolitical areas and they are in need of this type of direction to limit brain injuries in sport. In Guam there is robust agreement to improve youth player safety, but no entity championing the effort. Based on our feasibility assessment and new research showing that concussions occur at higher rates in high school athletes than professional athletes,[1,18,19] we believe Guam represents an ideal location for the public education of concussion awareness and the introduction of SCT. Parents, players, and school administrations could then collaborate to improve the safety and long-term health of local children and adolescents who play contact sports.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2014/5/1/91/134364
Contributor Information
Matthew Duenas, Email: mduenas@coh.org.
Greg Whyte, Email: gregwhyte27@yahoo.co.uk.
Rahul Jandial, Email: rjandial@coh.org.
REFERENCES
- 1.Bailes JE, Petraglia AL, Omalu BI, Nauman E, Talavage T. Role of subconcussion in repetitive mild traumatic brain injury. J Neurosurg. 2013;119:1235–45. doi: 10.3171/2013.7.JNS121822. [DOI] [PubMed] [Google Scholar]
- 2.2008 Guam Statistical Yearbook. Territory of Guam: Bureau of Statistics and Plans; 2009. Bureau of Statistics and plans, Office of Governor Felix P. Camacho. [Google Scholar]
- 3.The World Factbook. Australia-Oceania: Guam Web site; [Last accessed on 2013 Jun 01]. Central Intelligence Agency. Available from: https://www.cia.gov/library/publications/the-world-factbook/geos/gq.html . [Google Scholar]
- 4.Chrisman SP, Quitiquit C, Rivara FP. Qualitative study of barriers to concussive symptom reporting in high school athletics. J Adolesc Health. 2013;52:330–5.e3. doi: 10.1016/j.jadohealth.2012.10.271. [DOI] [PubMed] [Google Scholar]
- 5.Davis GA, Purcell LK. The evaluation and management of acute concussion differs in young children. Br J Sports Med. 2014;48:98–101. doi: 10.1136/bjsports-2012-092132. [DOI] [PubMed] [Google Scholar]
- 6.Duenas MJ, Hsu SN, Jandial R. Visual screening test for rapid sideline determination of concussive and sub-concussive events. Neurosurgery. 2013;73:N17–8. doi: 10.1227/01.neu.0000435117.18521.01. [DOI] [PubMed] [Google Scholar]
- 7.Galetta KM, Barrett J, Allen M, Madda F, Delicata D, Tennant AT, et al. The King-Devick test as a determinant of head trauma and concussion in boxers and MMA fighters. Neurology. 2011;76:1456–62. doi: 10.1212/WNL.0b013e31821184c9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Galetta KM, Brandes LE, Maki K, Dziemianowicz MS, Laudano E, Allen M, et al. The King-Devick test and sports-related concussion: Study of a rapid visual screening tool in a collegiate cohort. J Neurol Sci. 2011;309:34–9. doi: 10.1016/j.jns.2011.07.039. [DOI] [PubMed] [Google Scholar]
- 9.Government of Guam. [Last accessed on 2013 Jun 02]. Available from: http://www.guam.gov .
- 10.Harmon KG, Drezner JA, Gammons M, Guskiewicz KM, Halstead M, Herring SA, et al. American Medical Society for Sports Medicine position statement: Concussion in sport. Br J Sports Med. 2013;47:15–26. doi: 10.1136/bjsports-2012-091941. [DOI] [PubMed] [Google Scholar]
- 11.Jandial R, Duenas MJ, Chen MY. Neuroanatomy changes with repetitive mild head injury in athletes. Neurosurgery. 2013;72:N20. doi: 10.1227/01.neu.0000430739.63491.ba. [DOI] [PubMed] [Google Scholar]
- 12.Heitger MH, Jones RD, Macleod AD, Snell DL, Frampton CM, Anderson TJ. Impaired eye movements in post-concussion syndrome indicate suboptimal brain function beyond the influence of depression, malingering or intellectual ability. Brain. 2009;132:2850–70. doi: 10.1093/brain/awp181. [DOI] [PubMed] [Google Scholar]
- 13.McCrory P, Meeuwisse WH, Aubry M, Cantu RC, Dvořák J, Echemendia RJ, et al. Consensus statement on concussion in sport: The 4th International Conference on Concussion in Sport, Zurich, November 2012. J Athl Train. 2013;48:554–75. doi: 10.4085/1062-6050-48.4.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murphy A, Kaufman MS, Molton I, Coppel DB, Benson J, Herring SA. Concussion evaluation methods among Washington State high school football coaches and athletic trainers. PM R. 2012;4:419–26. doi: 10.1016/j.pmrj.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 15.Putukian M, Raftery M, Guskiewicz K, Herring S, Aubry M, Cantu RC, et al. Onfield assessment of concussion in the adult athlete. Br J Sports Med. 2013;47:285–8. doi: 10.1136/bjsports-2013-092158. [DOI] [PubMed] [Google Scholar]
- 16.Tsushima WT, Shirakawa N, Geling O. Neurocognitive functioning and symptom reporting of high school athletes following a single concussion. Appl Neuropsychol Child. 2013;2:13–6. doi: 10.1080/09084282.2011.643967. [DOI] [PubMed] [Google Scholar]
- 17.U.S. Census Bureau. International Program, International Database Web site. [Last accessed on 2013 June]. Available from: http://www.census.gov/population/international/data/idb/informationGateway.php .
- 18.Urban JE, Davenport EM, Golman AJ, Maldjian JA, Whitlow CT, Powers AK, et al. Head impact exposure in youth football: High school ages 14 to 18 years and cumulative impact analysis. Ann Biomed Eng. 2013;41:2474–87. doi: 10.1007/s10439-013-0861-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.USA: National Academies Press; 2013. US Institute of Medicine. Sports-Related Concussions in Youth: Improving the Science, Changing the Culture. [PubMed] [Google Scholar]
- 20.West TA, Marion DW. Current recommendations for the diagnosis and treatment of concussion in sport: A comparison of three new guidelines. J Neurotrauma. 2014;31:159–68. doi: 10.1089/neu.2013.3031. [DOI] [PMC free article] [PubMed] [Google Scholar]


