Abstract
Invasive ductal carcinoma of the breast with clear cell changes is a very rare pathological entity. There are <150 cases of this breast cancer subtype reported in the literature. Clear cell carcinoma could be easily missed or under-diagnosed in a breast core biopsy specimen due to the fact that this subtype tends to show a papillary pattern with clear cell and pseudo-lactating changes, especially in young female patients. Normal breast tissue may possess clear cells as a consequence of the physiological changes of pregnancy, the clearing of the cytoplasm within myoepithelial cells, or the clearing of the cytoplasm in apocrine metaplasia. Owing to its aggressive clinical course, clear cell carcinoma must be differentiated from other subtypes of breast carcinoma. Special attention given to this rare subtype by pathologists and clinicians could avoid misdiagnosis and delay of treatment.
INTRODUCTION
Breast cancer is the most prevalent cancer worldwide, with an estimated 4.4 million survivors within 5 years of diagnosis [1]. It is the second most common cancer-related cause of death among women, and the second most commonly diagnosed cancer (behind lung cancer) [1]. In the USA, the annual incidence of breast cancer is ∼82.5–99.4/100 000 women [1]. There are ∼180 000 cases diagnosed annually in the USA, with 41 000 deaths annually attributable to breast cancer [2]. Broadly speaking, invasive breast carcinoma may be classified into two groups, ductal and lobular types. There are different subtypes based upon specific morphological and immunohistochemical features. In ∼30–60% of cases, a mixed pattern is present. Clear cell carcinoma of the breast is a very rare neoplasm, with an estimated incidence between 1.4 and 3% of all cases of breast carcinomas [3, 4].
CASE REPORT
In our patient, the breast core biopsy showed multiple tiny foci of papillary proliferation with pseudo-lactational changes. However, the open biopsy showed poorly differentiated invasive ductal carcinoma with clear cell changes (Fig. 1). Ductal carcinoma in situ displays a papillary pattern with focal cystic hypersecretory (pseudo-lactating) features (Fig. 2). Microscopic examination showed that the tumor cells contained abundant fine glycogen granules in their clear cytoplasm, which were stained by a periodic acid-schiff (PAS) stain, but not stained by a diastase-PAS stain. There were features of poorly differentiated carcinoma with a prominent micropapillary growth pattern. Extensive ductal carcinoma in situ with solid, micropapillary, flat and cribriform types with an intermediate-to-high nuclear grade with necrosis was also noted. Invasive and in situ carcinomas both show clear cell and cystic hypersecretory changes. The breast core biopsy specimen showed atypical ductal hyperplasia with clear cell changes.
Figure 1:
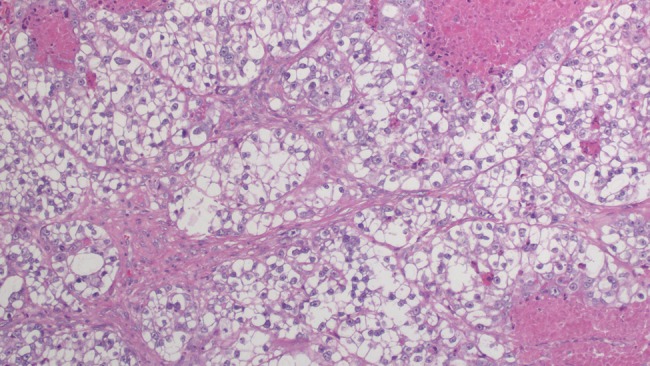
Microscopic examination reveals tumor cells with ample clear cytoplasm, distinct cell borders and pleomorphic nuclear features (×20).
Figure 2:
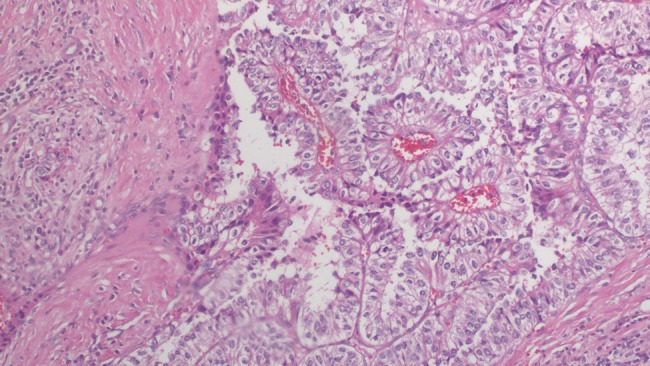
Microscopic examination reveals well-formed angular and papillary epithelial tumor cells with ample clear cytoplasm (×20).
Clear cell carcinoma may be easily missed or under-diagnosed in a breast core biopsy specimen due to the fact that it tends to show a papillary pattern with clear cell and pseudo-lactating changes, especially in young female patients [5]. Normal breast tissue may possess clear cells as a consequence of the physiological changes of pregnancy, clearing of the cytoplasm within myoepithelial cells, or the clearing of the cytoplasm in apocrine metaplasia [5]. Clear cell changes may be found in pre- or post-menopausal women, and may indicate benign changes or carcinoma. In rare cases, clear cell changes and pseudo-lactating changes may both be present in the same breast sample, and may be histologically difficult to distinguish from one another.
Owing to the rarity of the subtype of carcinoma found in our patient, there is a wide discrepancy in the literature with regard to clinical presentation. After a review of case reports in the literature, patients are usually women in their late forties, presenting with a painless mass in their breast. Kuroda et al. report that among 20 cases of glycogen-rich clear cell carcinoma of the breast that they examined, the age at presentation ranged from 33 to 68 years (mean 52 years), size of tumor ranged from 1 to 6.5 cm (mean 2.6 cm) and 7/20 cases (35%) that underwent an axillary lymph node dissection had positive lymph nodes. Fifteen of these cases were followed for 6 years, and 5/15 (33%) died within 5 years of diagnosis [4]. There is no clear consensus regarding prognosis, but it clearly follows an aggressive clinical course with reports of local recurrence, multiple recurrences and distant metastases [3, 4, 6, 7].
DISCUSSION
Breast cancer with glycogen-rich clear cell changes was first described in a 49-year-old woman by Hull et al. in 1981 [4, 6]. Electron microscopy showed neoplastic cells with non-membrane-bound particulate glycogen, which formed many acini. These cells had microvilli apically, and tight junctions as well as desmosomes laterally. Hull et al. [6] concluded that the morphological features were similar to those of fetal breast, as well as to clear cell carcinomas of other organs. It is estimated that the incidence of glycogen-rich clear cell carcinoma of the breast nears 1.4–3% of all breast cancers. The criteria used for the diagnosis of this tumor subtype are that cells consist primarily of cytoplasm that is clear and occasionally granular, with PAS stain positivity and diastase-labile material in at least 90% of the area of the tumor [8].
According to Kim et al., [9] as of 2012, there have been <150 cases of glycogen-rich clear cell carcinoma of the breast reported worldwide. This group advocates for a more organized study of the immunophenotype of glycogen-rich clear cell carcinoma. This group reports three cases, and based upon their findings, they report that the immunophenotype of this rare subtype is not uniform between patients.
Primary clear cell tumors are rare and commonly misdiagnosed. A clear cell pattern occurs in the presence of glycogen, lipid or mucin [10]. The differential diagnoses for breast carcinoma possessing cells with relatively clear cytoplasm are lipid-rich carcinoma, hidradenocarcinoma, histiocytoid lobular carcinoma, apocrine carcinoma, clear cell ‘sugar’ carcinoma, glycogen-rich carcinoma, myoepithelial carcinoma, secretory carcinoma, adenomyoepithelioma, signet ring carcinoma, sebaceous carcinoma and metastatic renal cell carcinoma [3, 7, 10].
Clear cell carcinoma of the breast may be easily missed or misdiagnosed in a breast core biopsy specimen due to the fact that it tends to possess a papillary pattern with clear cell and pseudo-lactating changes, especially in young female patients. Special attention should be given to this specific subtype by pathologists and clinicians in order to potentially avoid misdiagnosis and delay of treatment, since it clearly follows an aggressive clinical course.
REFERENCES
- 1.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 2.American Cancer Society. Breast Cancer Facts and Figures 2007–2008. Atlanta, GA: American Cancer Society Inc.; 2007. [Google Scholar]
- 3.Martín-Martín B, Berná-Serna JD, Sánchez-Henarejos P, López-Poveda MJ, Berná-Mestre JD, Rodríguez-García JR. An unusual case of locally advanced glycogen-rich clear cell carcinoma of the breast. Case Rep Oncol. 2011;4:452–7. doi: 10.1159/000332044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuroda H, Sakamoto G, Ohnisi K, Itoyama S. Clinical and pathological features of glycogen-rich clear cell carcinoma of the breast. Breast Cancer. 2005;12:189–95. doi: 10.2325/jbcs.12.189. [DOI] [PubMed] [Google Scholar]
- 5.Shirley SE, Escoffery CT, Titus IP, Williams EE, West AB. Clear cell carcinoma of the breast with immunohistochemical evidence of divergent differentiation. Ann Diagn Pathol. 2002;6:250–6. doi: 10.1053/adpa.2002.35399. [DOI] [PubMed] [Google Scholar]
- 6.Hull MT, Priest JB, Broadie TA, Ransburg RC, McCarthy LJ. Glycogen-rich clear cell carcinoma of the breast: a light and electron microscopic study. Cancer. 1981;48:2003–9. doi: 10.1002/1097-0142(19811101)48:9<2003::aid-cncr2820480916>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 7.Hayes MM, Seidman JD, Ashton MA. Glycogen-rich clear cell carcinoma of the breast: a clinicopathologic study of 21 cases. Am J Surg Pathol. 1995;19:904–11. doi: 10.1097/00000478-199508000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Gürbüz Y, Ozkara SK. Clear cell carcinoma of the breast with solid papillary pattern: a case report with immunohistochemical profile. J Clin Pathol. 2003;56:552–4. doi: 10.1136/jcp.56.7.552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim SE, Koo JS, Jung WH. Immunophenotypes of glycogen rich clear cell carcinoma. Yonsei Med J. 2012;53:1142–6. doi: 10.3349/ymj.2012.53.6.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Terada T. Clear cell variant of ductal carcinoma in situ of the breast. Breast J. 2012;18:279–80. doi: 10.1111/j.1524-4741.2012.01237.x. [DOI] [PubMed] [Google Scholar]


