Abstract
Background and Aims:
This study was undertaken, to assess the clinical parameters in patients of poisonous snakebite, complications which occurred in them, their outcome and to evaluate various clinical predictors of mortality
Materials and Methods:
Four hundred and thirty-two patients of snake bite were admitted, of which 172 did not show any signs of envenomation and excluded. Two hundred and sixty patients had signs of local or systemic envenomation and included. Complete clinical examination, blood counts, kidney function tests, serum electrolytes, coagulation profile was done in all patients. All received tetanus toxoid and anti-snake venom (ASV). Appropriate supportive treatment was given. Clinical and laboratory parameters were compared between patients who were discharged (Group A) and those who expired (Group B). All data analysis was performed by using stata software version 10 [StataCorp LP, Texas, USA] and SPSS version 11 [SPSS Inc, Chicago, USA].
Results:
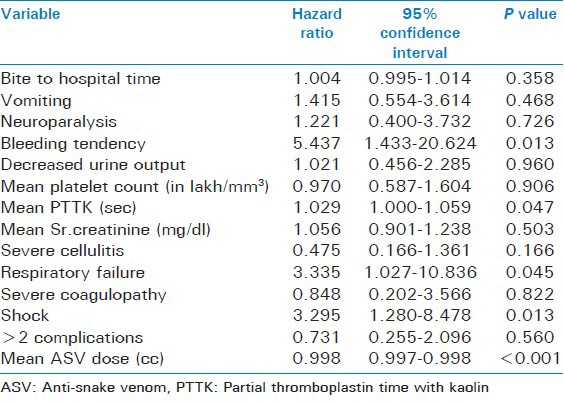
Out of 260 patients, 58 died and 202 survived. Mean age was 34.97 ± 14.07 years. One hundred and eighty-six (71.5%) patients were from rural areas and 74 (28.5%) from urban. 63.4% of bites occurred during rainy season. One hundred and ninety-seven (75.8%) had bite on lower limb and 62 (23.8%) on upper limbs. All 260 patients (100%) had pain at site of bite, local swelling in 252 (96.9%) and blackening of skin, blebs in 18 (6.9%). Seventy-seven (29.6%) had bleeding tendencies. Ptosis was present in all the 65 patients with signs of neuroparalysis. Eighty (30.8%) patients had acute renal failure. The mean duration of stay in survivors was 7.50 + 4.13 days and in non-survivors it was 3.45 + 3.02 days. Out of 58 who died 18 (31%) patients, succumbed within 24 hrs. On multivariate analysis, significant predictors o mortality were bleeding tendency (P = 0.013), mean PTTK (sec) (P = 0.047), respiratory failure (P = 0.045), shock (P = 0.013), mean ASV dose (cc) (P < 0.001).
Conclusions:
Mortality in patients with snake bite can be predicted by simple variables like presence of bleeding tendencies, respiratory failure, and shock. These parameters can help the doctors at peripheral health centers to predict outcome, so that such high risk cases can be referred to higher centers for expertise management without wasting time.
Keywords: Acute renal failure, envenomation, neuroparalysis, snake bite
INTRODUCTION
About 2500 species of snakes exist in the world. India has over 250 species and subspecies, out of which 50 are venomous.[1] Mainly 4 venomous land snakes pose public health problem in India. They are elapidae, including cobra (Naja naja) and krait (Bungarus caeruleus) and viperidae- Russell's viper (Daboia russelii) and saw-scaled viper (Echis carinatus). Worldwide, of the estimated 5 million people bitten by snakes each year, about 125,000 die.[2] More than 200,000 cases of snakebite are reported in India, each year and 35,000-50,000 of them are fatal.[3] However, this hospital based data is likely to underestimate the incidence and mortality of snakebite.[4] Many patients in rural areas also seek traditional treatment and many die at home or during transport to hospital.[5] and valuable period is lost while attending such traditional treatment.
This study was undertaken, to assess the clinical parameters in patients of poisonous snakebite admitted at our institute, complications which occurred in them, their outcome and to evaluate various clinical predictors of mortality.
MATERIALS AND METHODS
Patients
This prospective observational study was conducted from 2006 to 2008, at Department of Medicine in Government Medical College and Hospital, Nagpur, a tertiary care hospital serving population of central India. Four hundred and thirty-two patients of snake bite were admitted, of which 172 did not show any signs of envenomation and were excluded from the study. Two hundred and sixty patients had signs of local or systemic envenomation and were included, after an informed consent for participation in the study. The study was approved by Institutional Ethical Committee of our institute.
Methods
Evidence of bite by a poisonous snake included: (i) fang marks, (ii) swelling, ecchymosis, blister formation and/or bleeding from local site, (iii) disturbances in coagulation mechanism with or without systemic bleeding, and (iv) identification of snake wherever possible. Swelling confined only to the bite site was graded as mild; extension to more than half of the limb as moderate; and extensive swelling with tissue necrosis was graded severe.[6,7] Neurotoxicity was defined as documented ptosis, external ophthalmoplegia, weakness of neck or bulbar muscles, use of neostigmine or ventilatory support (endotracheal intubation, Ambu bag or a mechanical ventilator).[4] Oliguria was defined as 24-hr urine output of <500 ml, and anuria as the complete absence of urine formation (<50 ml).[8] Acute renal failure (ARF) was diagnosed when there was acute rise in serum creatinine to >2.0 mg/dl.[9] Those patients who had platelet count less than 1.5 lakh/mm3 were classified to have thrombocytopenia.[7] Those patients with prolongation of prothrombin time (PT) defined as >1.5 × normal86.[10] and PTTK more than 10 sec above control value were classified as having severe coagulopathy.[11] Shock was defined as presence of mean arterial blood pressure less than 60 mm of Hg in a previously normotensive patient.[12]
Treatment and Follow-up
All patients received tetanus toxoid and anti-snake venom (ASV). The initial dose of ASV given was 50cc in mild local cellulitis, 100cc in moderate to severe envenomation and in those with complications. This dose was repeated as needed as per investigations and clinical improvement. Patients with signs of neuroparalysis were given inj. neostigmine along with atropine as needed. The patients were followed during the hospitalisation and outcome noted as discharged (A) or expired (B).
Statistical analysis
We used t-test for continuous normally distributed variables. For categorical data Chi-square statistics was used and Fischer-exact test was used for small numbers. For variables which were not normally distributed Wilcoxon's Mann-Whitney U-test was used. P value of 0.05 or less was considered statistically significant. Crude hazard ratios were calculated to assess the strength of association between risk factors and outcome i.e. mortality. We used Cox proportional hazard regression model for analysis of multiple predictor variability. All data analysis was performed by using stata software version 10 and SPSS version 11.
RESULTS
Out of 260 patients, 58 patients died and 202 survived. Mortality rate was 22.3%. The mean age of patients was 34.97 ± 14.07 years. The mean age in survivor group (A) was 35.02 + 14.12 years and in non-survivor group (B) 34.81 + 14.00 years. (P = 0.920). Out of the260 paients, 170 were males (65.4%) and 90 (34.6%) were females. The male to female ratio was 1.9:1
186 (71.5%) patients were from rural areas as compared to 74 (28.5%) patients from urban areas. Thus, rural: urban ratio was 2.5:1. Patients coming from rural areas were 142 (70.3%) in group A (i.e. survivors) and 44 (75.9%) in group B (i.e. non-survivors). The number of patients from urban areas were 60 (29.7%) in survivors and 14 (24.1%) in non-survivors. (P = 0.408) Out of 58 patients who died, 44 (75.9%) were from rural areas and 14 (24.1%) were from urban areas.
Maximum no. of patients were admitted during the month of September which was 51 (19.6%). Most of the cases (around 63.4%) of snake bite occurred during the period from June to September i.e. during rainy season. This was followed by winter season (October to January) in which number of patients admitted were 60 (23.1%). The number of patients admitted during summer (March to May) was 27 (10.4%).
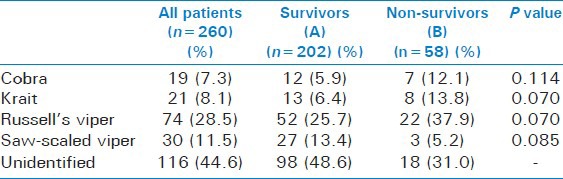
One hundred and ninety-seven (75.8%) patients had bite on lower limb (LL) and 62 (23.8%) had bite on upper limbs (UL). Only one patient had bite on head, face or neck (HFN-ear) and he survived. In survivors (group A), 151 (74.7%) patients had bite on lower limbs and in non-survivors (group B), 46 (79.3%) patients had bite on LL. (P = 0.475) Bites on upper limbs were present in 50 (24.8%) patients in survivor group and 12 (20.7%) patients in non-survivor group. (P = 0.522). Table 1 shows snake identification in the study.
Table 1.
Snake identification
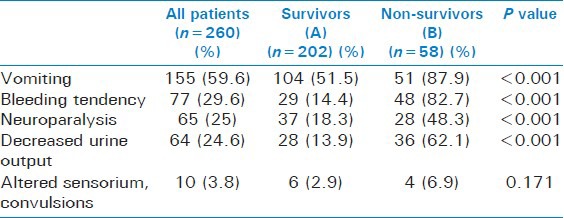
All the 260 patients (100%) had pain at the local site of bite. Local swelling was the second most common complaint present in 252 (96.9%) and blackening of the skin, blebs were present in 18 (6.9%). Local swelling was present in 195 (96.5%) in survivor group and in 57 (98.3%) in non-survivor group. (P = 0.688) Blackening of the skin, blisters and blebs was present in 10 (4.9%) survivors and in 8 (13.8%) non-survivors. This difference was statistically significant. (P = 0.019). The systemic symptoms are shown in Table 2.
Table 2.
Systemic symptoms
Total 77 (29.6%) patients had bleeding tendencies, among which 48 (62.3%) died. Out of them 66 (85.7%) had bleeding from bite site, 42 (54.5%) had hematuria, 49 (63.6%) had malena and 11 (14.3%) had bleeding from other sites like gums, epistaxis, subconjunctival bleed, ecchymotic patches etc., Bleeding from bite site was present in 23 (79.3%) patient in survivor group and in 43 (89.6%) patients in non-survivor group. (P = 0.212) Hematuria was present in 14 (48.3%) patients in survivor group and in 28 (58.3%) patients in non-survivor group. (P = 0.390) Malena was present in 18 (62.1%) patients in survivor group and in 31 (64.6%) patients in non-survivor group. This difference was statistically not significant. (P = 0.824) Bleeding from other sites like gums, etc., was present in 5 (17.2%) patients in survivor group and in 6 (12.5%) patients in non-survivor group (P = 0.565).
Ptosis was present in all the 65 patients who had any of the signs suggestive of neuroparalysis. Similarly, ophthalmoplegia was present in 62 (95.4%) patients and respiratory distress was present in 33 (50.7%) of these patients. Ophthalmoplegia was present in 35 (94.6%) patients in the survivor group and in 27 (96.4%) patients in non-survivor group. (P = 0.727) Respiratory distress was present in 9 (24.3%) patients in survivor group and in 24 (85.7%) patients in non-survivor group. This difference was statistically highly significant (P < 0.001).
Among the 64 patients with acute renal failure, oliguria was present in 46 (71.9%) patients, anuria in 10 (15.6%) patients and oliguria followed by anuria in 8 patients (12.5%). Oliguria was present in 17 (60.7%) patients in survivor group and in 29 (80.6%) patients in non-survivor group. (P = 0.080) Anuria was present in 6 (21.4%) patients of the survivors and 4 (11.1%) patients in non-survivor group. (P = 0.259) Oliguria followed by anuria was present in 5 (17.9%) survivors and in 3 (8.3%) non-survivors. (P = 0.282).
Investigations and mortality
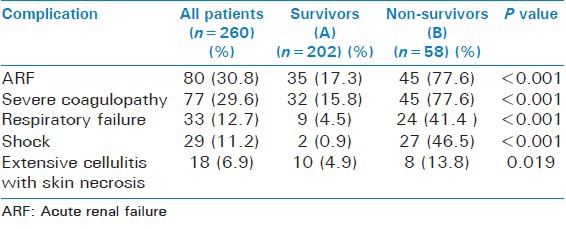
Mean clotting time was 13.76 + 3.21 min. Severe coagulopathy was found to be present in 77 patients as per PT and PTTK. 80 (30.8%) patients had acute renal failure and 77 (29.6%) patients had bleeding tendency. Albuminuria was present in all 80 patients with ARF. Table 3 shows laboratory investigations in patients with acute renal failure and coagulopathy. The complications are depicted in Table 4.
Table 3.
Laboratory investigations in patients with acute renal failure and coagulopathy
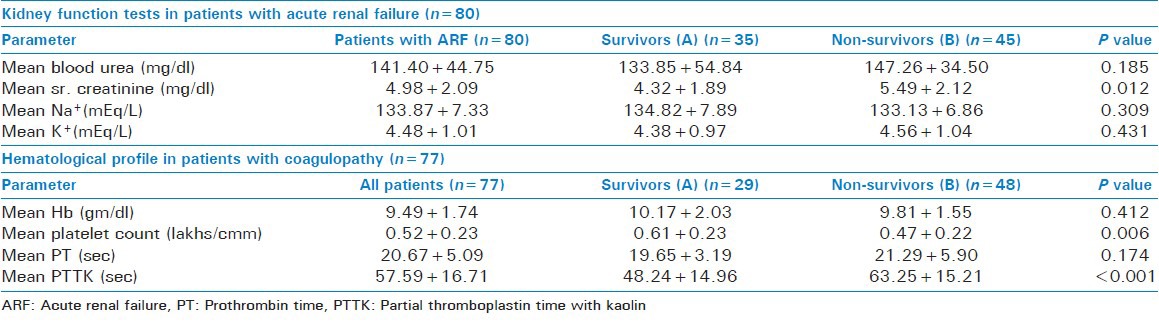
Table 4.
Correlation of complications and mortality
Treatment given to the patients
Six (2.3%) patients required surgical treatment in the form of debridement. Inj. Neostigmine was given to 65 (25%) patients who developed signs of neuroparalysis. Ventilatory support was given to all 33 (12.7%) patients who developed respiratory distress. Renal replacement therapy in the form of either peritoneal dialysis or hemodialysis was given to 33 (12.7%) patients. Various blood components like whole blood, fresh frozen plasma (FFP), platelet transfusion were given to 80 (30.8%) patients. Mean duration of stay for all patients was 6.60 ± 4.25 days. Mean duration of stay in survivors was 7.50 ± 4.13 days and in non-survivors it was 3.45 ± 3.02 days. Out of 58 who died 18 (31%) patients, succumbed within 24 hrs. The multivariate analysis predictors of mortality is shown in Table 5.
Table 5.
Multivariate analysis of various predictors of mortality in snake bite patients
DISCUSSION
In hospital-based studies, mortality rates ranged from 3%[13] to 20%[14,15] Various authors have found important contributors to death in such patients like delay in arrival at hospital (prolonged bite to hospital time),[7,16,17,18] respiratory failure,[4,7,17,19,20,21] ARF,[4,7,9,15,20] presence of severe coagulopathy or DIC[6,7,9,20] shock[15,19,22] etc., However, very few have evaluated the predictors of mortality by doing statistical analysis.[4,5]
The higher incidence in rural areas in this study can be because of large number of people working in fields in rural areas e.g., paddy fields and habit of walking barefoot.[8] Their houses which are built of mud, provide access and shelter to snakes.[2] Sleeping on the floor and outside the house or in farms may also be responsible for increased number of cases in rural areas. However, there was no relation of mortality with patients from any particular area (rural/urban). Kulkarni et al.,(1994)[19] found that 90% were from rural areas. Naik et al.,(1997)[15] reported that 83.6% were from rural areas. Sharma et al.,(2005)[13] found a rural: Urban ratio 4.7:1, which was higher than that in our study group.
Maximum numbers of patients were admitted during rainy season. Probably because of the heavy rains, the holes and burrows are filled up with water and snakes come out of it and number of encounters of men with snakes increase, increasing incidence of snake bites cases. The breeding habits of preys like frogs also follow the monsoon.[23] Naik et al.,(1997)[15] reported that 60.6% cases occurred between June to November. Hansdak et al.,(1998)[24] reported that 51% cases occurred during monsoon (August-October). Steinmann et al.,(2000)[25] found that 64% of the cases occurred in the months of June to September, comparable to our study. Brunda et al.,(2007)[26] also found that rainy season (June-September) accounted for 50% (n = 689) of the snake bite cases reported.
We also found that prolonged bite to hospital time i.e., delayed arrival to hospital was associated with mortality. Most of the studies have observed this correlation between bite to hospital time and complications or mortality.[4,5,7,13,18] This can be explained by the fact that incidence of complications is directly proportional to the duration of venom in the blood prior to its neutralization by ASV due to late arrival of patient at hospital (Narvencar et al.)[18] and as complications occur mortality will increase. This delay can be attributed to lack of awareness of hazards of snake bite, belief in traditional methods of treatment,[23] lack of proper referral systems and transport facilities.[27] Many of the times ASV may not be available at primary health centers (PHCs) and patients may not receive ASV until they reach higher centers. Kulkarni et al.,(1994)[19] found that out of the 633 cases, 42 (6.6%) were admitted within 1 hour of bite and 22% of the patients came to hospital after 24 hours. In a study conducted by Steinmann et al.,(2000)[25] contrary to our study, almost 87% of the patients were brought to the hospital within an hour. Sharma et al.,(2005)[13] found that median bite to hospital time in their study group was 9 hours and delayed arrival was seen in patients presenting with ARF. Kalantri et al.,(2006)[4] studied 277 patients, in whom mean bite to hospital time was 6.5 + 10.3 hrs. In survivors, it was 5.6 + 10.3 hrs and in non-survivors it was 11.4 + 14.5 hrs (P < 0.001).
There was no relation of timing of bite (during day/night) with mortality. More number of bites occurring during daytime can be explained on the basis of increased outdoor activity during daytime which increases possibility of encounter with snakes and hence snake bites. Kulkarni et al.,(1994)[19] reported that 68.2% cases were bitten during day. Sharma et al.,(2005)[13] found that 60.6% bite occurred during night, contrary to our study.
Russell's viper was the most common culprit snake identified. However, identification of any particular type of snake was not related to mortality. Usually after an episode of snake bite, a person is gripped by fear and may not be able to see the snake properly. The snake also doesn’t remain at that site after bite. So it is difficult to identify the type of snake. The snake can be identified correctly only if the culprit snake is brought to the hospital for examination but even examining the snake may be dangerous if it is not confirmed that snake is dead. Therefore WHO has advised the syndromic approach for treatment of snakebite patients.[3] In a study of 633 cases conducted by Kulkarni et al.,(1994)[19] the biting species was identified in only 388 cases (61.2%). The commonest was viper (242 cases-38.2%) followed by cobra (129 cases-20.3%), water snake (10 cases) and krait (7 cases). These findings were somewhat comparable to our study. Punde et al.,(2005)[21] found that out of the 427 patients envenomed by poisonous snakes, 274 (64.2%) were bitten by saw-scaled viper, 71 (16.6%) were bitten by cobra 42 (9.8%) by krait and 40 (9.4%) by Russell's viper.
Tourniquet application was the most commonly used first-aid measure. The use of these various first-aid measures was not related to any particular outcome. According to WHO guidelines, recommended first-aid methods are reassurance, immobilisation of the bitten limb and movement of the patient to a place where they can receive medical care as soon as possible. Pressure immobilisation technique (PIT) which is recommended by WHO[28] was not used in any of our patient.
Vomiting was present in 104 (51.5%) patients in survivor group (A) and in 51 (87.9%) patients in the non-survivor group (B). This difference was statistically highly significant. (P < 0.001) Vomiting, an important feature of severe systemic envenomation, has not received much attention in clinical practice. However, vomiting is not a specific sign of severe envenoming, and may be induced by fear or use of herbal medicines or alcohol after a snake bite, may be a feature of early anaphylactoid reaction to ASV, uraemia or autonomic disturbances. Thus, whether vomiting is a surrogate marker of severity of snake bite requires more research.
Most common feature of neuroparalysis was ptosis. When respiratory failure was present in a patient with snakebite, it was associated with increased mortality. As the severity of neuroparalytic features increase, the symptoms progress to involve respiratory muscles. It is important to distinguish neurotoxic envenoming of krait from cobra: The krait blocks both pre-synaptic and post-synaptic receptors and needs prolonged mechanical ventilation until their receptors are generated (Bawaskar et al.,2002)[29] the cobra blocks post-synaptic receptors (Watt et al.,1986)[30] and needs more antivenom and neostigmine.
Acute renal failure is one the most common complications following snakebite, especially by vipers. Most of the times it co-exists with coagulopathy which adds to the risk of mortality. The signs of uraemia may develop within 3-7 days of the bite.[31] Another important and reliable sign is gross hematuria. If hematuria is persistently found on naked eye examination within the first week of illness, it is likely that the patient would require peritoneal dialysis.[31] This observation was confirmed by Soe et al.,(2005).[32] Many of the studies have found ARF as one the major causes of death in patients of poisonous snakebite.[4,7,13,20,21]
Snake venom contains various procoagulant factors which cause activation of coagulation cascade leading to intravascular coagulation and consumption of various clotting factors and platelets. Thus, thrombocytopenia and hemostatic abnormalities which ultimately result will cause spontaneous bleeding. The presence of spontaneous bleeding is indicative of presence of unneutralized snake venom present in circulation. This is an indication for repeating a dose of ASV in patients.
Disseminated intravascular coagulation (DIC) has been one of the major contributors to death in many studies.[6,7,9,20] Though WHO and Indian National Snakebite Protocols 2007[33] has given recommendation for treatment, in some patients bleeding may continue in spite of giving sufficient doses of ASV. In such cases ASV should be continued until coagulation abnormalities are restored. In our study, in case of neuroparalysis and acute renal failure, we continued ASV until they responded. In a study conducted by Agrawal et al.,(2001).[34] ASV was given to patients with neuroparalysis until recovery of neurological manifestations.
Optimum dose of ASV has been a matter of debate. But, poor outcome is associated with delayed initiation of treatment, associated complications rather than total dose of ASV. Sharma et al., (2005)[13] found that the average dose of antivenom was 51.2 vials (512 cc) for elapid bites and 31 vials (310 cc) for viper bites. Punde et al.,(2005)[21] found that dose of ASV required in treating neurotoxic envenomation was 40-320 ml and for viper bites it was 20-250 ml.
Mean duration of stay for all patients was 6.60 + 4.25 days. Mean duration of stay in survivors was 7.50 + 4.13 days and in non-survivors it was 3.45 + 3.02 days. Omogbai et al.,(2000)[35] studied 433 patients of snake bite with a mean duration of stay in hospital of 5.7 ± 5.1 days. (Range 1-23 days), comparable to our study.
At the end of multivariate analysis bleeding tendency, respiratory failure, shock, PTTK, total ASV dose were independent predictors of mortality.
Though the P value was significant for mean total ASV dose, the hazard ratio and hence the risk ratio was almost equal to 1 (0.998), hence there was no effect of ASV dose on outcome as such. The mean ASV dose was low in non-survivors because they did not receive adequate doses of ASV as they died early. About 18 (31%) patients out of 58 who died, succumbed within 24 hrs This also supports the fact that total ASV dose given to patient cannot be used to predict outcome.
CONCLUSIONS
Thus, we conclude that mortality in patients with snake bite can be predicted by simple variables like presence of bleeding tendencies, respiratory failure, and shock. These prognostic parameters can help the doctors at peripheral health centers to predict outcome, so that such high risk cases can be referred to higher centers for expertise management without wasting time, after giving them necessary initial treatment like initial dose of ASV. For this reason Anti-snake venom (ASV) should be made available at all PHCs (Primary Health Centers). Similarly, the general population should also be educated regarding avoidance of unnecessary procedure like attending the traditional healers and shifting the patient to the hospital as early as possible.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sarangi A, Jena I, Das JP. A Profile of snakebite poisoning with special reference to hematological, renal, neurological, electrocardiographic abnormalities. J Assoc Physicians India. 1977;25:555–60. [PubMed] [Google Scholar]
- 2.Kasturiratne A, Wickremasinghe AR, de Silva N, Gunawardena NK, Pathmeswaran A, Premaratna R, et al. The global burden of snakebite: A literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Med. 2008 Nov 4;5(11):e218. doi: 10.1371/journal.pmed.0050218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Warrell DA. Guidelines for the clinical management of snakebites in the South East Asian regions. Southeast Asian J Trop Med Public Health. 1999;30:1–84. [Google Scholar]
- 4.Kalantri S, Singh A, Joshi R, Malamba S, Ho C, Ezoua J, et al. Clinical predictors of in-hospital mortality in patients with snakebite: A retrospective study from a rural hospital in central India. Trop Med Int Health. 2006;11:22–30. doi: 10.1111/j.1365-3156.2005.01535.x. [DOI] [PubMed] [Google Scholar]
- 5.Sharma SK, Chappuis F, Jha N, Bovier PA, Loutan L, Koirala S. Impact of snake bites and determinants of fatal outcomes in southeastern Nepal. Am J Trop Med Hyg. 2004;71:234–8. [PubMed] [Google Scholar]
- 6.Kularatne SA. Epidemiology and clinical picture of the Russell's viper (Daboia russelii russelii) bite in Anuradhapura, Sri Lanka: A prospective study of 336 patients. Southeast Asian J Trop Med Public Health. 2003;34:855–62. [PubMed] [Google Scholar]
- 7.Suchithra N, Pappachan JM, Sujathan P. Snakebite envenoming in Kerala, South India: Clinical profile and factors involved in adverse outcomes. Emerg Med J. 2008;25:200–4. doi: 10.1136/emj.2007.051136. [DOI] [PubMed] [Google Scholar]
- 8.Denker BM, Brenner BM. Azotemia and urinary abnormality. In: Fauci AS, Kasper DL, Longo DL, Braunwald E, Hauser SL, Jameson JL, Loscalzo J, editors. Harrison's Principles of Internal Medicine. 17th ed. New Delhi: McGraw Hill; 2008. p. 271. [Google Scholar]
- 9.Srimannanarayana J, Dutta TK, Sahai A, Badrinath S. Rational Use of Anti-snake venom (ASV): Trial of various regimens in hemotoxic snake envenomation. J Assoc Physicians India. 2004;52:788–93. [PubMed] [Google Scholar]
- 10.Arruda V, High KA. Coagulation disorders. In: Fauci AS, Kasper DL, Longo DL, Braunwald E, Hauser SL, Jameson JL, Loscalzo J, editors. Harrison's Principles of Internal Medicine. 17th ed. New Delhi: McGraw Hill; 2008. pp. 729–30. [Google Scholar]
- 11.Firkin F, Chesterman C, Penington D, Rush B, editors. de Gruchy's Clinical haematology in Medical Practice. 5th ed. India: Blackwell Science Ltd; 1997. Coagulation Disorders; pp. 406–53. [Google Scholar]
- 12.Maier RV. Approach to the patient with shock. In: Fauci AS, Kasper DL, Longo DL, Braunwald E, Hauser SL, Jameson JL, Loscalzo J, editors. Harrison's Principles of Internal Medicine. 17th ed. New Delhi: McGraw Hill; 2008. pp. 1689–95. [Google Scholar]
- 13.Sharma N, Chauhan S, Faruqi S, Bhat P, Varma S. Snake envenomation in a north Indian hospital. Emerg Med J. 2005;22:118–20. doi: 10.1136/emj.2003.008458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sharma SK, Khanal B, Pokharel P, Khan A, Koirala S. Snakebite-reappraisal of the situation in Eastern Nepal. Toxicon. 2003;41:285–9. doi: 10.1016/s0041-0101(02)00289-1. [DOI] [PubMed] [Google Scholar]
- 15.Naik RS, Tirpude BH, Khajuria BK. Mortality and morbidity pattern in snake bite at MGIMS Sevagram, Wardha: A rural area. Indian Pract. 1997;50:31–5. [Google Scholar]
- 16.Kulartane SA. Common krait (bungarus caeruleus) bite in Anuradhapura, Sri Lanka: A prospective clinical study 1996-98. Postgrad Med J. 2002;78:276–80. doi: 10.1136/pmj.78.919.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Looareesuwan S, Viravan C, Warrell DA. Factors contributing to fatal snake bite in the rural tropics: Analysis of 46 cases in Thailand. Trans R Soc Trop Med Hyg. 1988;82:930–4. doi: 10.1016/0035-9203(88)90046-6. [DOI] [PubMed] [Google Scholar]
- 18.Narvencar K. Correlation between timing of ASV administration and complications in Snake bites. J Assoc Physicians India. 2006;54:717–9. [PubMed] [Google Scholar]
- 19.Kulkarni ML, Anees S. Snake venom poisoning, experience with 633 patients. Indian Paediatr. 1994;31:1239–43. [PubMed] [Google Scholar]
- 20.McGain F, Limbo A, Williams DJ, Didei G, Winkel KD. Snakebite mortality at Port Moresby General Hospital, Papua New Guinea, 1992-2001. Med J Aust. 2004;181:687–91. doi: 10.5694/j.1326-5377.2004.tb06525.x. [DOI] [PubMed] [Google Scholar]
- 21.Punde DP. Management of snake-bite in rural Maharashtra: A 10-year experience. Natl Med J India. 2005;18:71–5. [PubMed] [Google Scholar]
- 22.Paul V, Pratibha S, Prahlad KA, Earali J, Francis S, Lewis F. High- dose anti-snake venom versus low dose anti-snake venom in the treatment of poisonous snake bites: A critical study. J Assoc Physicians India. 2004;52:14–7. [PubMed] [Google Scholar]
- 23.Reddy KS. Essentials of forensic medicine and toxicology. 27th ed. Hyderabad: Laxmi Printers; 2008. Organic irritant poisons; pp. 487–99. [Google Scholar]
- 24.Hansdak SG, Lallar KS, Pokharel P, Shyangwa P, Karki P, Koirala S. A clinico-epidemiological study of snake bite in Nepal. Trop Doct. 1998;28:223–6. doi: 10.1177/004947559802800412. [DOI] [PubMed] [Google Scholar]
- 25.Steinmann L, Devkota UN, Shah LN. Snakebite in Nepal: A study from Siraha District. J Nepal Med Assoc. 2000;39:203–9. [Google Scholar]
- 26.Brunda G, Sashidhar RB. Epidemiological profile of snake-bite cases from Andhra Pradesh using immunoanalytical approach. Indian J Med Res. 2007;125:661–8. [PubMed] [Google Scholar]
- 27.Gaitonde BB, Bhattacharya S. An epidemiological survey of snake-bite cases in India. Snake. 1980;12:129–33. [Google Scholar]
- 28.Warrell DA. Injuries, envenoming, poisoning and allergic reactions caused by animals. In: Warrell DA, Cox TM, Firth JD, editors. Oxford Text Book of Medicine. 4th ed. Oxford: Oxford University Press; 2003. pp. 923–47. [Google Scholar]
- 29.Bawaskar HS, Bawaskar PH. Profile of snakebite envenoming in western Maharashtra, India. Trans R Soc Trop Med Hyg. 2002;96:79–84. doi: 10.1016/s0035-9203(02)90250-6. [DOI] [PubMed] [Google Scholar]
- 30.Watt G, Theakston RD, Hayes CG, Yambao ML, Sangalang R, Ranoa CP, et al. Positive response to endrophonium in patients with neurotoxic envenoming by cobras (Naja naja philippinensis) N Engl J Med. 1986;315:1444–8. doi: 10.1056/NEJM198612043152303. [DOI] [PubMed] [Google Scholar]
- 31.Sharma SK, Koirala S, Dahal G. Krait bite requiring high dose antivenom: A case report. Southeast Asian J Trop Med Public Health. 2002;33:170–1. [PubMed] [Google Scholar]
- 32.Paing SO. Russell's Viper Bite: Correlation of different clinical criteria to peritoneal dialysis and clinical outcome. Regional Health Forum. 2005;9:37–42. [Google Scholar]
- 33.Snakebite First Aid and Treatment Support Concepts, Indian National Snakebite Protocols; 2007. [cited 2013 Sep 26]. Snakebite Prevention; pp. 1–37. Available from: http://www.whoindia.org/LinkFiles/Chemical_Safety_Snakebite_Protocols_2007.pdf . [Google Scholar]
- 34.Agrawal PN, Agrawal AN, Gupta D, Behera D, Prabhakar S, Jindal SK. Management of respiratory failure in severe neuroparalytic snake envenomation. Neurol India. 2001;49:25–8. [PubMed] [Google Scholar]
- 35.Omogbai EK, Zuleikha AM, Imhafidon MA, Ikpeme AA, Ojo D, Nwako CN, et al. Snake bites in Nigeria: A study of the prevalence and treatment in Benin City. Trop J Pharm Res. 2002;1:39–44. [Google Scholar]


