Abstract
Central-venous-catheter-related bloodstream infections (CRBSIs) are an important cause of hospital-acquired infection associated with morbidity, mortality, and cost. Consequences depend on associated organisms, underlying pre-morbid conditions, timeliness, and appropriateness of the treatment/interventions received. We have summarized risk factors, pathogenesis, etiology, diagnosis, and management of CRBSI in this review.
Keywords: Antibiotic lock therapy, Candida, catheter related bloodstream infections, Central-venous-catheter, Staphylococcus
INTRODUCTION
Catheter-related bloodstream infection (CRBSI) is defined as the presence of bacteremia originating from an intravenous catheter. It is one of the most frequent, lethal, and costly complications of central venous catheterization and also the most common cause of nosocomial bacteremia. Intravascular catheters are integral to the modern practices and are inserted in critically-ill patients for the administration of fluids, blood products, medication, nutritional solutions, and for hemodynamic monitoring. Central venous catheters (CVCs) pose a greater risk of device-related infections than any other types of medical device and are major causes of morbidity and mortality. They are also the main source of bacteremia and septicemia in hospitalized patients. Majority of CRBSIs are associated with CVCs and in prospective studies, the relative risk for CRBSI is up to 64 times greater with CVCs than with peripheral venous catheters.
Epidemology of catheter related bloodstream infections
Based on the North American data compiled from the National nosocomial infection surveillance system (NNIS) from October 1986 to December 1990, CRBSI incidence was 2.1 per 1000 catheter days for respiratory Intensive Care Units,5.1 for medical-surgical ICUs, 5.8 for trauma ICUs, 30.2 for burn units,[1] More recent data from NNIS from January 1992 through June 2004 showed the median rate of CRBSI in ICUs of all types ranged from 1.8-5.2 per 1000 catheter.[2] According to Leonardo Lorente et al., (2005) incidence of CRBSI was 2.79 infections per 1000 catheter days, among which CVC were responsible for 2.09% of cases.[3] According to S Singh et al., (2010) the overall infection rate for CRBSI was found to be 0.48 per 1000 device days.[4] According to Ramanathan Parameswaran et al., (2011) the incidence of CRBSI was 8.75 per 1,000 catheter days.[5] Incidence of CRBSI reported varies from country to country and even hospital to hospitals. Meta-analytical study done at The Johns Hopkins University showed that bloodstream infections (BSIs) were the third leading cause of hospital-acquired infections. These infections have an attributable mortality rate of 12% to 25%.[6] Individuals counteract 250,000 BSIs each year in the U.S., 60% of CRBSIs were caused by micro-organisms from the patient's skin. CRBSIs often originate in emergency rooms and intensive-care units, where 5.3 bloodstream infections occur per thousand days of central venous catheter insertion.[7] Intravenous catheters were the devices most frequently used for providing fluids directly into the bloodstream. Although the incidence of local or BSIs associated with these devices is usually low, serious infectious complications produce a considerable number of deaths annually because of the frequency with which such catheters are used.
CRBSI accounts for 10% to 20% of hospital-acquired infections in the UK and is associated with both increased ICU stay and mortality. Rates of CRBSI may be modified by clinical care during insertion and utilization of CVCs.[8] As such, the incidence of CRBSI has been proposed as a quality indicator. The incidence of CRBSI varies considerably by type of catheter, frequency of catheter manipulation, and patient-related factors, such as underlying disease and severity of illness. Majority of CRBSIs are associated with CVCs, and in prospective studies, the relative risk for CRBSI is up to 64 times greater with CVCs than with peripheral venous catheters. For short-term CVCs (<10 days),[9] which are most commonly colonized by cutaneous organisms along the external surface of the catheter, the most important preventive systems are those that decrease the extra-luminal contamination. In contrast, with long-term CVCs (>10 days), endo-luminal spread from the hub appears to be the primary mechanism of infection. Technologies that reduce endo-luminal colonization in addition to extra-luminal invasion of the catheter should provide additional protection against CRBSI. The incidence of dialysis-related CRBSI is reported to be 2.5-F5.5 cases per 1,000 catheter days, or 0.9-2.0 episodes per patient-year.[10] The risk of bacteremia is highest in hemodialysis patients using a CVC for vascular access, and increases in a linear fashion with the duration of catheter use.[11] Most nosocomial BSIs among pediatric patients are related to the use of an intravascular device and in critically-ill neonates, the incidence of CRBSI can be as high as 18 cases per 1000 catheter-days[12] [Figure 1].
Figure 1.
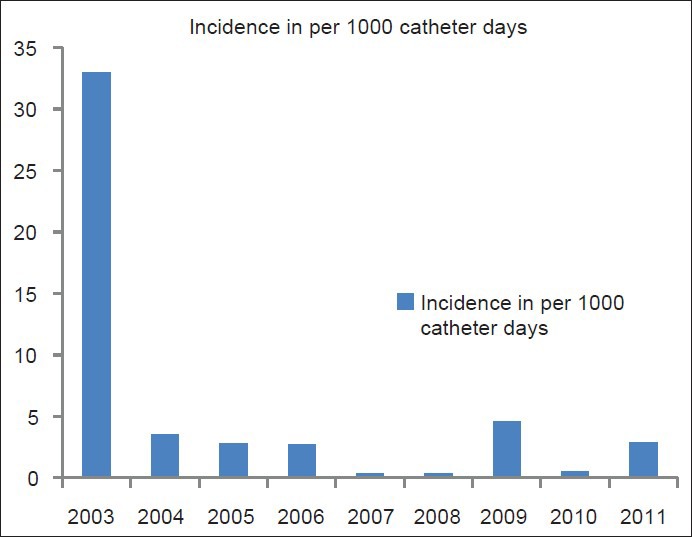
Changing epidemiological trend of CRBSI
Risk factors
Potential risk factors for CRBSI include underlying disease, method of catheter insertion, site of catheter insertion and duration, and purpose of catheterization. The administration of parenteral nutrition through intravascular catheters increases CRBSI risk. Local risk factors, such as poor personal hygiene, occlusive transparent dressing, moisture around the exit site, S. aureus nasal colonization, and contiguous infections support the role of bacterial colonization in the pathogenesis of CRBSI. Other risk factors for dialysis CRBSI include contamination of dialysate or equipment, inadequate water treatment, dialyzer re-use, older age, higher total intravenous iron dose, increased recombinant human erythropoietin dose, lower hemoglobin level, lower serum albumin level, diabetes mellitus, peripheral atherosclerosis, and recent hospitalization or surgery. CRBSI rate varies considerably in different studies.[13]
Pathogenesis of catheter related bloodstream infections
Several interrelated factors have been proposed to participate in the pathogenesis of CRBSI. The catheter itself can be involved in 4 different pathogenic pathways like colonization of the catheter tip and cutaneous tract with skin flora; colonization of the catheter lumen caused by contamination; hematogenous seeding of the catheter from another infected site; and contamination of the lumen of the catheter with infusate [Figure 2]. Resistance to antibiotic therapy due to biofilm formation also has an important role in development of bacteremia. It is important to know that a negative catheter- related sample rules out CRBSI better than a positive sample indicating one. When the blood culture obtained from the catheter is positive, but the percutaneous blood sample is negative, it indicates colonization of the catheter rather than CRBSI. However, if the organism is S. aureus or Candida, or if patient has valvular heart disease or neutropenia, close monitoring is required, which includes evaluation for infective endocarditis and metastatic infection.
Figure 2.
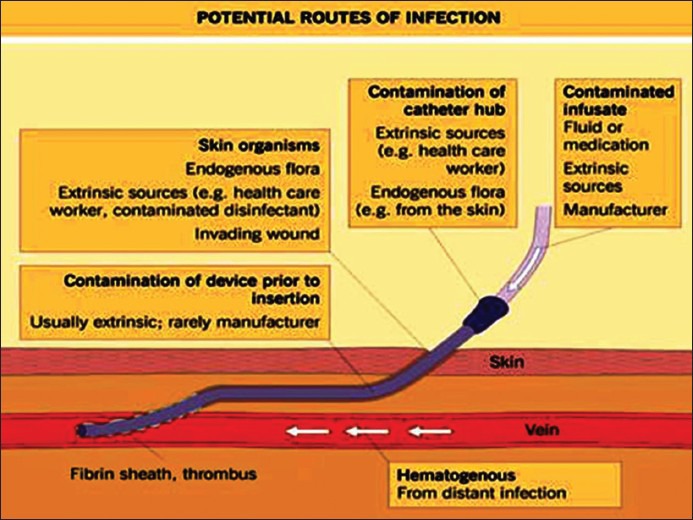
Potential routes of infections causing CRBSI
Catheter related bloodstream infections associated micro-organisms
The organisms associated with CRBSI are usually the normal resident flora of the skin at the insertion site, which may lead to colonization of the catheter inserted. Colonization of the tip of the intravenous catheter is often observed in the ICU practice and can be the source of dangerous bacteremia (CRBSI) and sepsis with multi-organ failure [Figure 3].
Figure 3.
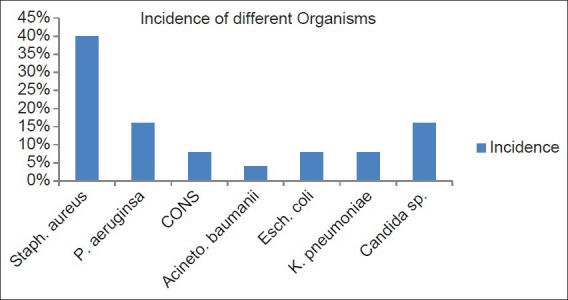
Causative organisms of CRBSI
Bacterial infections
In the study of Ramanathan Parameswaran et al., (2011) 64% of the pathogens causing CRBSI were Gram-positive and 36% were Gram-negative. The commonest pathogen causing CRBSI was S. aureus 40%, Pseudomonas aeruginosa 16%, co-agulase negative staphylococci 8%, E. coli 8%, Klebsiella pneumoniae 8%, and Acinetobacter baumanii 4%.[5] According to Krishnan et al., (2011) Gram-positive cocci constituted 27% of isolates and gram-negative bacilli were 56%. The proportion of Gram-negative CRBSI was much higher than that reported in western hospitals.[14] Seifert et al., (2003) showed coagulase-negative staphylococci were present in 50% cases of CRBSI in their study.[15] In the study of Almuneef et al., (2006) of total 50 CRBSI episodes, 48% were polymicrobial, 32% were due to Gram-negative bacilli, and 10% were due to Gram-positive organisms. The most common organisms isolated were Klebsiella pneumoniae 16%, coagulase-negative staphylococci 14%, and Pseudomonas aeruginosa 11%.[16]
Fungal infection
Various studies have showed different rates of fungal infectious agents responsible for CRBSI, these are mainly yeasts, and no filamentous fungus has been reported. In the study of Ramanathan Parameswaran et al., (2011) 16% of infectious agents were Candida sp.,[5] according to Pawar et al., (2008) fungal pathogen isolated from CVC was Candida 11.7%,[17] and Chopdekar et al. (2011) showed non-albicans Candida spp. in one case.[18]
Viral and Parasitic infections
The CRBSI organisms are usually skin flora, which is mainly bacteria and yeasts, very less is known about normal viral and parasitic skin flora, and no study has shown any viral or parasitic cause of CRBSI.
Catheter related bloodstream infections detection
Detection of CRBSI includes both clinical as well as laboratory examination.
CLINICAL PRESENTATION
The diagnosis of CRBSI is often suspected clinically in a patient using a CVC who presents with fever or chills, unexplained hypotension, and no other localizing sign.[19,20] Mild symptoms include malaise and nausea, and severe symptoms include high fever with rigors, hypotension, vomiting, and changes in mental status in the setting of a normal catheter exit site or tunnel, on physical examination.[21] Exit-site infection is indicated by the presence of erythema, swelling, tenderness, and purulent drainage around the catheter exit and the part of the tunnel external to the cuff. Severe sepsis and metastatic infectious complications, such as infective endocarditis, septic arthritis, osteomyelitis, spinal epidural abscess and septic emboli, can prolong the course of CRBSI[22] and should be considered in patients who do not respond appropriately to treatment. Infective endocarditis should be suspected in those patients with onset of new cardiac murmur, repeatedly positive blood cultures, and other features of the modified Duke criteria. A clinical diagnosis can be made after exclusion of alternative sources of infection.[19]
Laboratory diagnosis of catheter related bloodstream infections
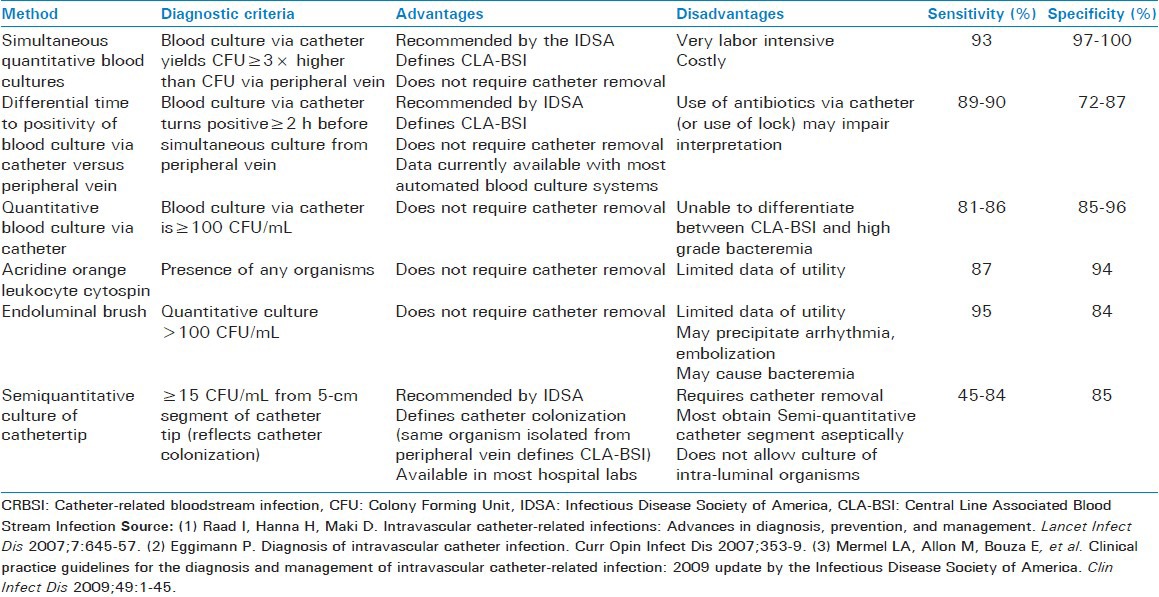
The diagnosis of CRBSI requires a positive culture of blood from a peripheral vein and clear evidence that the catheter is the source. CRBSI means a patient with an intravascular catheter has at least one positive blood culture obtained from a peripheral vein, clinical manifestations of infections (i.e., fever, chills, and/or hypotension), and no apparent source for the BSI, except the catheter. In addition, one of the following is also present: A positive semi-quantitative (>15 CFU/catheter segment)[23] or quantitative (>103 CFU/catheter segment)[24] catheter tip culture also, the same organism (species and anti-biogram) is isolated from the catheter segment and peripheral blood culture. Simultaneous quantitative paired blood cultures with a >5:1 ratio CVC versus peripheral, or differential time to positivity, whereby a non-quantitative blood culture drawn from the CVC that becomes positive at least 2 hr earlier than the peripheral blood culture, is a new method for the diagnosis of CRBSI without removing the catheter[15] [Table 1].
Table 1.
Different microbiological methods to detect CRBSI
Quantitative paired blood culture
CRBSI is defined as a quantitative blood culture ratio of >5:1 (CVC versus peripheral) with proven identity of isolates from positive peripheral and CVC blood cultures confirmed by pulsed-field gel electrophoresis. CRBSI can be diagnosed when colony counts are at least 3-fold higher in cultures of blood obtained via the CVC than in cultures of blood taken from a peripheral vein. The fold difference between the CVC and peripheral blood varies in the literature with suggested cuts offs from 3-fold to 10-fold. To diagnose CRBSI with the CVC in situ, most experts recommend comparative blood cultures obtained via the CVC and a peripheral vein prior to initiating antibiotics. Cultures should be obtained from all lumens of the CVC, it is the most specific method of diagnosing CRBSI. If a blood sample cannot be drawn from a peripheral vein, it is recommended that 2 blood samples should be drawn through different catheter lumens, and the colony count for the blood sample drawn through one lumen is at least 3-fold greater than the colony count for the blood sample obtained from the second lumen should be considered to indicate possible CRBSI.
Differential time to positivity
CRBSI is suggested when blood from the CVC demonstrates microbial growth at least 2 h earlier than growth is detected in blood collected simultaneously from a peripheral vein. Most currently used automated blood culture systems can readily provide this information, and it is likely that this will become a standard diagnostic test.
Short-term catheters, including arterial catheters
For short-term catheter tip cultures, the roll plate technique is recommended for routine clinical microbiological analysis.[25] For suspected pulmonary artery catheter infection, the introducer tip is cultured.[26]
Long-term catheters
Semi-quantitative growth of 15 cfu/catheter segment of the same microbe from both the insertion site culture, and the catheter hub culture strongly suggests that the catheter is the source of a bloodstream infection. A venous access subcutaneous port is removed for suspected CRBSI, and the port is sent to the microbiology laboratory for qualitative culture of the port reservoir contents, in addition to the catheter tip.[27]
Management of catheter related bloodstream infections
Regular ICU rounds by clinical microbiologists and bed-side discussion with intensivists regarding infection management. Prompt communication of urgent microbiology results.
Assessment of infection
This constitutes the central objective of the clinical microbiology round in ICU so that diagnostic, therapeutic, and infection control interventions can be initiated at the earliest. Assessment of infection has to be a broad-based approach relying on an entire gamut of historical, epidemiological, clinical, diagnostic parameters (physical examination, hematological, biochemical, radiological) along with microbiology results.
Infection prevention and control
This consists of microbiology result interpretation and feedback to intensive care unit team regarding anti-microbial resistance, audit and policy implementation, rational utilization of diagnostic, therapeutic and infection prevention/control resources.
General Management
Catheters should be removed from patients with CRBSI associated with any local or systemic inflammation or immunocompromised condition. Antibiotic therapy for catheter-related infection is often initiated empirically. The initial choice of antibiotics will depend on the severity of the patient's clinical disease, the risk factors for infection, and the likely pathogens associated with the specific intravascular device. There are no compelling data to support specific recommendations for the duration of therapy for device-related infection. Vancomycin is recommended for empirical therapy for methicillin-resistant Staphylococcus aureus; for vancomycin minimum inhibitory concentration values >2 μg/mL, alternative agents, such as daptomycin, should be used. Linezolid should not be used for empirical.[28] Empirical coverage for Gram-negative bacilli should be based on local anti-microbial susceptibility data and the severity of disease (e.g., a fourth-generation cephalosporin, carbapenem, or β-lactam/β-lactamase combination, with or without an aminoglycoside). In addition to coverage for Gram-positive pathogens, empirical therapy for suspected CRBSI involving femoral catheters in critically-ill patients should include coverage for Gram-negative bacilli and Candida species.[29] For empirical treatment of suspected catheter-related candidemia, echinocandin is used or, in selected patients, fluconazole.[30] Antibiotic lock therapy should be used for catheter salvage; however, if antibiotic lock therapy cannot be used in this situation, systemic antibiotics should be administered through the colonized catheter.[31]
Antibiotic lock therapy and its use to treat patients with catheter-related infection
Recurrent bacteremia after parenteral therapy is more likely to occur if that therapy is administered through a retained catheter than if the catheter is removed.[32] This likely reflects the inability of most antibiotics to achieve therapeutic concentrations needed to kill microbes growing in a biofilm. Because the majority of infections involving long-term catheters or totally implanted catheters are intra-luminal, eradication of such infections is attempted by filling the catheter lumen with supra-therapeutic concentrations of antibiotics and leaving them indwelling for hours or days, thereby creating an antibiotic lock. Antibiotic lock therapy for CRBSI is used in conjunction with systemic antibiotic therapy and involves installing a high concentration of an antibiotic, to which the causative microbe is susceptible in the catheter lumen. The likelihood of success varies with the site of infection (e.g., tunnel or pocket infection are unresponsive to salvage) and with the microbe causing the infection (e.g., coagulase-negative staphylococci are likely to respond; S. aureus is not).
CONCLUSION
Catheter-related bloodstream infection (CRBSI) is the commonest cause of nosocomial bacteremia. CRBSI is one of the most frequent, lethal, and costly complications of central venous catheterization. CVCs are commonly associated with hospital-acquired bloodstream infections and lead to both increased ICU stay and mortality. Early diagnosis and treatment are vital to reduce the morbidity and mortality involved. National guidelines exist on the prevention of CRBSI, these should be followed, and central venous catheter must be reviewed daily. Different measures have been implemented to reduce the risk for CRBSI, including use of maximal barrier, precautions during catheter insertion, effective cutaneous anti-sepsis, and preventive strategies based on inhibiting micro-organisms originating from the skin or catheter hub from adhering to the catheter. Institution of continuous quality improvement programs, education, and training of health care workers, and adherence to standardized protocols for insertion and maintenance of intravascular catheters significantly reduced the incidence of catheter-related infections and represent the most important preventive measures. New technologies for prevention of infections directed at CVCs, which have been shown to reduce the risk of CRBSI, including catheters and dressings impregnated with antiseptics or antibiotics, new hub models and antibiotic lock solutions, are in use.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.National Nosocomial Infections Surveillance (NNIS) System report, data summary from January 1990-May 1999, issued June 1999. Am J InfectControl. 1999;27:520–32. doi: 10.1016/s0196-6553(99)70031-3. [DOI] [PubMed] [Google Scholar]
- 2.National Nosocomial Infections Surveillance (NNIS) System Report. Am J Infect Control. 2004;32:470–85. doi: 10.1016/S0196655304005425. [DOI] [PubMed] [Google Scholar]
- 3.Lorente L, Henry C, Martin MM, Jimenez A, Mora ML. Central venous catheter-related infection in a prospective and observational study of 2595 catheters. Crit Care. 2005;9(6):R631–5. doi: 10.1186/cc3824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh S, Pandya Y, Patel R, Paliwal M, Wilson A, Trivedi S. Surveillance of device-associated infections at a teaching hospital in rural Gujarat – India. IJMM. 2010;28(4):342–7. doi: 10.4103/0255-0857.71830. [DOI] [PubMed] [Google Scholar]
- 5.Parameswaran R, Sherchan JB, Varma DM, Mukhopadhyay C, Vidyasagar S. Intravascular catheter-related infections in an Indian tertiary care hospital. J Infect Dev Ctries. 2011;5:452–8. doi: 10.3855/jidc.1261. [DOI] [PubMed] [Google Scholar]
- 6.Maki DG, Kluger DM, Crnich CJ. The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc. 2006;81:1159–71. doi: 10.4065/81.9.1159. [DOI] [PubMed] [Google Scholar]
- 7.Soufir L, Timsit JF, Mahe C, Carlet J, Regnier B, Chevret S. Attributable morbidity and mortality of catheter-related septicemia in critically ill patients: a matched, risk-adjusted, cohort study. Infect Control Hosp Epidemiol. 1999;20:396–401. doi: 10.1086/501639. [DOI] [PubMed] [Google Scholar]
- 8.Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, et al. An intervention to decrease catheter-related bloodstream infectionsin the ICU. N Engl J Med. 2006;355:2725–32. doi: 10.1056/NEJMoa061115. [DOI] [PubMed] [Google Scholar]
- 9.Stefania cicaline, Fabrizio palmieri, Nicola petrosillo. Clinical review: New technologies for prevention of intravascular catheter-related infections. Crit care. 2004;8:157–62. doi: 10.1186/cc2380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee H, Manns B, Taub K, Ghali WA, Dean S, Johnson D, et al. Cost analysis of ongoing care of patients with end-stage renal disease: The impact of dialysis modality and dialysis access. Am J Kidney Dis. 2002;40:611–22. doi: 10.1053/ajkd.2002.34924. [DOI] [PubMed] [Google Scholar]
- 11.Powe NR, Jaar B, Furth SL, Hermann J, Briggs W. Septicemia in dialysis patients incidence, risk factors, and prognosis. Kidney Int. 1999;55:1081–90. doi: 10.1046/j.1523-1755.1999.0550031081.x. [DOI] [PubMed] [Google Scholar]
- 12.Garland JS, Buck RK, Maloney P, Durkin DM, Toth-Llyod S, Duffy M, et al. Comparison of 10% povidone-iodine and 0.5% chlorhexidine gluconate for the prevention of peripheral intravenous catheter colonization inneonates: A prospective trial. Pediatr Infect Dis J. 1995;14:510–6. doi: 10.1097/00006454-199506000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Sachdev A, Gupta D, Soni A, Chugh K. Central venous catheter colonization and related bacteremia in pediatric intensive care unit. Indian Pediatr. 2002;39:752–60. [PubMed] [Google Scholar]
- 14.Krishnan R.G, Dorairajan Sureshkumar. Changing Trends in Antimicrobial Susceptibility and Hospital Acquired Infections Over an Year Period in a Tertiary Care Hospital in Relation to Introduction of an Infection Control Programme. JAPI. 2011 [PubMed] [Google Scholar]
- 15.Seifert H, Cornely O, Seggewiss K, Decker M, Stefanik D, Wisplinghoff H. Bloodstream infection in neutropenic cancer patients related to short-termnontunnelled catheters determined by quantitative blood cultures,differential time to positivity, and molecular epidemiological typing with pulsed-field gel electrophoresis. J Clin Microbiol. 2003;41:118–23. doi: 10.1128/JCM.41.1.118-123.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Almuneef MA, Memish ZA, Balkhy HH, Hijazi O, Cunningham G, Francis C. Rate, risk factors and outcomes of catheterrelated bloodstream infection in a paediatric intensive care unit in Saudi Arabia. J Hosp Infect. 2006;62:207–13. doi: 10.1016/j.jhin.2005.06.032. [DOI] [PubMed] [Google Scholar]
- 17.Pawar M, Mehta Y, Kapoor P, Sharma J, Gupta A, Trehan N. Central venous catheter-related blood stream infections:incidence, risk factors, outcome, and associated pathogens. J Cardiothorac Vasc Anesth. 2004;18:304–8. doi: 10.1053/j.jvca.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 18.Chopdekar K, Chande C, Chavan S, Veer P, Wabale V, Vishwakarma K. A JoshiCentral venous catheter-related blood stream infection rate in critical care units in a tertiary care, teaching hospital in Mumbai Central venous catheter-related blood stream infection rate in critical care units in a tertiary care, teaching hospital in Mumbai. IJMM. 2011;29(2):169–71. doi: 10.4103/0255-0857.81796. [DOI] [PubMed] [Google Scholar]
- 19.Allon M. Dialysis catheter-related bacteremia: treatment and prophylaxis. Am J Kidney Dis. 2004;44:779–91. [PubMed] [Google Scholar]
- 20.Nassar GM, Ayus JC. Infectious complications of the hemodialysis access. Kidney Int. 2000;60:1–13. doi: 10.1046/j.1523-1755.2001.00765.x. [DOI] [PubMed] [Google Scholar]
- 21.Beathard GA. Management of bacteremia associated with tunneled-cuffed hemodialysis catheters. J Am Soc Nephrol. 1999;10:1045–9. doi: 10.1681/ASN.V1051045. [DOI] [PubMed] [Google Scholar]
- 22.Kovalik EC, et al. A clustering of epidural abscesses in chronic hemodialysis patients: risks of salvaging access catheters in cases of infection. J Am Soc Nephrol. 1996;7:2264–7. doi: 10.1681/ASN.V7102264. [DOI] [PubMed] [Google Scholar]
- 23.Maki DG, Weise CE, Sarafin HW. A semiquantitative culture method for identifying intravenous-caheter-related infection. N Engl J Med. 1977;296:1305–9. doi: 10.1056/NEJM197706092962301. [DOI] [PubMed] [Google Scholar]
- 24.Brun-Buisson C, Abrouk F, Legrand P, Huet Y, Larabi S, Rapin M. Diagnosis of central venous catheter-related sepsis - critical level of quantitative tip cultures. Arch Intern Med. 1987;147:873–7. [PubMed] [Google Scholar]
- 25.Bouza E, Alvarado N, Alcala L, et al. A prospective, randomized, and comparative study of 3 different methods for the diagnosis of intravascular catheter colonization. Clin Infect Dis. 2005;40:1096–100. doi: 10.1086/428576. [DOI] [PubMed] [Google Scholar]
- 26.Mermel LA, McCormick RD, Springman SR, Maki DG. The pathogenesis and epidemiology of catheter-related infection with pulmonary artery Swan-Ganz catheters: a prospective study utilizing molecular subtyping. Am J Med. 1991;91:197S–205. doi: 10.1016/0002-9343(91)90369-9. [DOI] [PubMed] [Google Scholar]
- 27.Bouza E, Alvarado N, Alcala L, Perez MJ, Rincon C, Munoz P. A randomized and prospective study of 3 procedures for the diagnosis of catheter-related bloodstream infection without catheterwithdrawal. Clin Infect Dis. 2007;44:820–6. doi: 10.1086/511865. [DOI] [PubMed] [Google Scholar]
- 28.Wilcox MH, Tack KJ, Bouza E, et al. Complicated skin and skinstructure infections and catheter-related bloodstream infections: noninferiority of linezolid in a phase 3 study. Clin Infect Dis. 2009;48:203–12. doi: 10.1086/595686. [DOI] [PubMed] [Google Scholar]
- 29.Lorente L, Jiménez A, Santana M, Iribarren JL, Jiménez JJ, Martín MM, et al. Microorganisms responsible for intravascular catheter-related bloodstream infection according to the catheter site. Crit Care Med. 2007;35:2424–7. doi: 10.1097/01.CCM.0000284589.63641.B8. [DOI] [PubMed] [Google Scholar]
- 30.Reboli AC, Rotstein C, Pappas PG, et al. Anidulafungin versus fluconazole for invasive candidiasis. N Engl J Med. 2007;356:2472–82. doi: 10.1056/NEJMoa066906. [DOI] [PubMed] [Google Scholar]
- 31.Fernandez-Hidalgo N, Almirante B, Calleja R, Ruiz I, Planes AM, Rodriguez D, et al. Antibiotic-lock therapy for long-term intravascular catheter-related bacteraemia: Results of an open, non-comparative study. J Antimicrob Chemother. 2006;57:1172–80. doi: 10.1093/jac/dkl103. [DOI] [PubMed] [Google Scholar]
- 32.Raad I, Davis S, Khan A, Tarrand J, Elting L, Bodey GP. Impact of central venous catheter removal on the recurrence of catheter-related coagulase-negative staphylococcal bacteremia. Infect Control Hosp Epidemiol. 1992;13:215–21. doi: 10.1086/646512. [DOI] [PubMed] [Google Scholar]


