Abstract
Recent national surveys suggest that child obesity in the United States may have reached a plateau, but corresponding trends in energy intake have not been examined in depth. This article evaluates medium-term trends in children’s reported energy intake by using 4 waves of national dietary surveillance from 2003–2004 to 2009–2010. The analysis uses up to 2 24-h dietary recalls, incorporating methods that address challenges in estimating usual intake, accounting for intraindividual variance and covariates such as the presence of atypical consumption days. Quantile regression was used to assess disparities in intake among sociodemographic subgroups at extremes of the distribution as well as at the median, and the potential influence of misreporting was evaluated. Results indicated that after an initial decline in intakes across all age groups through 2007–2008, there were significant increases of ∼90 kcal/d at the median among adolescents in 2009–2010, whereas intakes in younger children remained steady. Among adolescent boys, the recent increase was larger at the 90th percentile than at the median. Intake trends did not vary by race/ethnic group, among whom intakes were similar at the upper end of the distribution. Misreporting did not influence trends over time, but intakes were lower in younger children and higher in older children after excluding misreporters. Overall, findings suggest that declines in children’s energy intake from 2003–2004 through 2007–2008 were consistent with the obesity plateau observed in most age and gender subgroups through 2009–2010. However, there is evidence of increased intakes among adolescents in 2009–2010, which may threaten the earlier abatement in overweight in this older age group.
Introduction
Energy intakes are thought to be a major driver of the obesity epidemic (1, 2). Several studies indicate that the dramatic increase in U.S. child obesity that occurred over the past few decades was followed by a plateau in 2009–2010 (3–8). However, researchers have yet to examine to what extent this shift is reflected by concomitant changes in energy intake. The role of energy intake trends in population changes in obesity is a subject of debate, given a number of factors. First, numerous studies exploring longer-term dietary trends corresponding to the timing of the increase in obesity reported substantial, albeit unexpected, declines in energy intake in both children and adults (9–12). It is uncertain to what extent this apparent inconsistency may be due in part to factors such as long-term changes in reporting biases or intake assessment methods, which may be less problematic in studies focused on medium-term dietary shifts. Concerns have also been expressed about the ability to estimate usual intakes from a limited number of dietary recalls, as well as the potential impact of reporting biases on the validity of these trends (13, 14). Moreover, although analyses of trends generally focus on changes in the mean, shifts at extremes of the distribution may be more relevant for changes in weight status.
This study examines patterns of change in child energy intake in detail, with the aim of gaining insights on the extent to which trends in intake correspond to shifts in obesity. Rather than long-term trends, this study examines changes in energy intake among U.S. children and adolescents by using data from nationally representative cross-sectional surveys conducted between 2003–2004 and 2009–2010, coinciding with the timing of recently reported shifts in child obesity trends (3, 8). Unlike studies focused on long-term trends that pool multiple waves of data, each 2-y survey cycle is analyzed separately to capture shorter-term fluctuations that may contribute to the shifts observed in patterns of obesity. To provide the most valid assessment of intake trends, methods to address a number of other potential limitations were incorporated.
Previous literature on dietary trends using these surveillance data generally focused on changes in mean intake estimates based on a single dietary recall (9, 10, 15). However, because weight status is affected by habitual intake, this analysis incorporates methods to better estimate usual intake from 2 recalls, by accounting for intraindividual variability and covariates that influence reporting (16, 17). Rather than mean intake, this article uses quantile regression to examine shifts in the upper, median, and lower ends of the distribution and provides greater insights on where the most notable changes are occurring. Long-term increases in child overweight and obesity have disproportionately affected minority and lower socioeconomic status subpopulations, which recent declines do not appear to have redressed (3, 18, 19). It was therefore considered important to explore evidence of inequalities in the magnitude of changes in intake across the caloric distribution by using quantile regression models to test for age, race/ethnic group, gender, and socioeconomic status disparities in patterns of change. Finally, to address concerns that changes over time in misreporting of energy intake may be influential (13), the impact of under- and over-reporting on energy intake trends was assessed.
Participants and Methods
Dietary data on participants aged 2–18 y from 4 cycles (2003–2004, 2005–2006, 2007–2008, and 2009–2010) of What We Eat in America, the dietary component of the NHANES, were used. These multistage, stratified probability samples of the U.S. population all used the same USDA food composition data to estimate energy intake (20–29). Two nonconsecutive days of intake data were obtained from 24-h dietary recall interviews administered by using the USDA’s Automated Multiple-Pass Method (30). The first recall was collected by trained interviewers in the mobile examination center, and the second recall was collected on most participants 3–10 d later by telephone. Dietary interviews were self-completed by adolescents aged 12–18 y, whereas children aged 6–11 y were assisted by an adult, and interviews were completed by proxy for children ages 2–5 y.
Participants were excluded from analyses if parental education was missing (n = 477) and if the indicators of whether reported energy intake were atypical were missing (n = 32), 0 kcal (n = 5), or >4 SDs beyond individual estimated energy requirements (n = 136) and thus physiologically implausible estimates of habitual intake. Estimated energy requirement was calculated according to equations provided by the Institute of Medicine’s Dietary Reference Intakes (2005) (31), with SD values calculated to identify implausible dietary reports by using the formula provided by Huang et al. (32). Accelerometry data were available only for NHANES 2003–2006 (33), and self-report data have been shown to substantially overestimate activity levels (34, 35). Therefore, to account for the contribution of physical activity to the estimates of energy needs used to identify implausible intake reports, SD bounds were estimated on the basis of sedentary physical activity levels (PALs)10 to identify under-reporters and very active PALs to identify over-reporters. Supplementary sensitivity analyses excluding children whose energy intakes did not fall within the 1.5-SD bounds of estimated requirements used less conservative assumptions, applying a low-active PAL for the lower bound and an active PAL for the upper bound; results did not change meaningfully from the main findings presented (data not shown). The final sample included 12,909 children over all 4 survey cycles, with a total of 24,159 dietary recalls (88% of the sample had 2 recalls). The sociodemographic distribution of the sample is shown in detail in Supplemental Table 1.
The National Cancer Institute (NCI) method was used to estimate the distribution (means and percentiles) of usual energy intake in children by using multiple 24-h recalls (16, 17). This method allows 1) estimating the within- and between-person variance components and correcting for the high intraindividual variation intrinsic to 24-h recalls and 2) adjusting for important covariates, which helps improve the estimates by explaining the variability (e.g., intake differences due to recall sequence, or weekend consumption). Specifically, a 1-part nonlinear mixed model for repeated 24-h recalls was fit by using the NCI MIXTRAN macro (17, 36), applying Box-Cox transformations and adjusting by NHANES survey cycle, age group, gender, race/ethnicity, parental education, weekend (including Friday), season (November–April or May–October), self-report intake amount (more, same, or less than usual), and recall sequence. Regression coefficients from this model are provided in Supplemental Table 2. The distribution of usual intake was then estimated empirically with the NCI DISTRIB macro (16, 17, 36), which performs Monte Carlo simulation by using estimated parameters from the model fit in the NCI MIXTRAN macro. The usual energy intake distribution is estimated for the first recall adjusted for the second recall and for usual self-report amount (as opposed to less or more). The simulated population has the same covariate pattern as NHANES for gender, race/ethnicity, and education. Finally, the distribution of usual energy intake for each survey cycle was standardized to the NHANES 2003–2004 age distribution. Because NHANES uses a complex, multistage probability design, variance estimation was carried out via the Balanced Repeated Replication technique and a Fay coefficient of 0.3 (37).
One limitation of the NCI method is that the effect from covariates on usual intake is constant on the transformed scale for all percentiles, because the model specification is for the mean. In contrast, quantile regression (38, 39) estimates regression coefficients in all parts of the distribution of a response variable and hence allows the estimation of different effects at different percentiles of the distribution. To apply quantile regression to assess changes in intake at specific percentiles, we first predicted usual energy intake for each individual with the NCI INDIVINT macro (16, 17, 36, 40) by using previously estimated parameters. Note that even for individuals with only one 24-h recall, a predicted usual intake enhanced with the information from all other individuals is obtained, which therefore is not based solely on the single day that happens to be observed. Quantile regression was then used to test the significance of differences in changes in intake associated with age, gender, parental education, and race/ethnicity at the 10th, 50th, and 90th percentiles of predicted usual energy intake with the use of an α level of 0.05 to define significance. Specifically, interactions between survey cycle and each covariate were included, and global tests for each interaction performed. Models were reduced when global tests were not significant at a 0.05 α level. Race/ethnic group analyses focused on Mexican Americans, non-Hispanic blacks, and non-Hispanic whites (NHWs) because other groups were small and heterogeneous. Last, predicted margins from the quantile regression were obtained to illustrate the size of the effects; predicted estimates are shown for the 10th, 50th (median), and 90th percentiles. Analyses accounted for the complex survey design and sampling weights (dietary recall weights for day 1) by using SAS version 9.3 software (SAS Institute) and the qreg2 command in STATA version 13.0 (StataCorp) to perform quantile regression with robust and clustered SEs.
Results
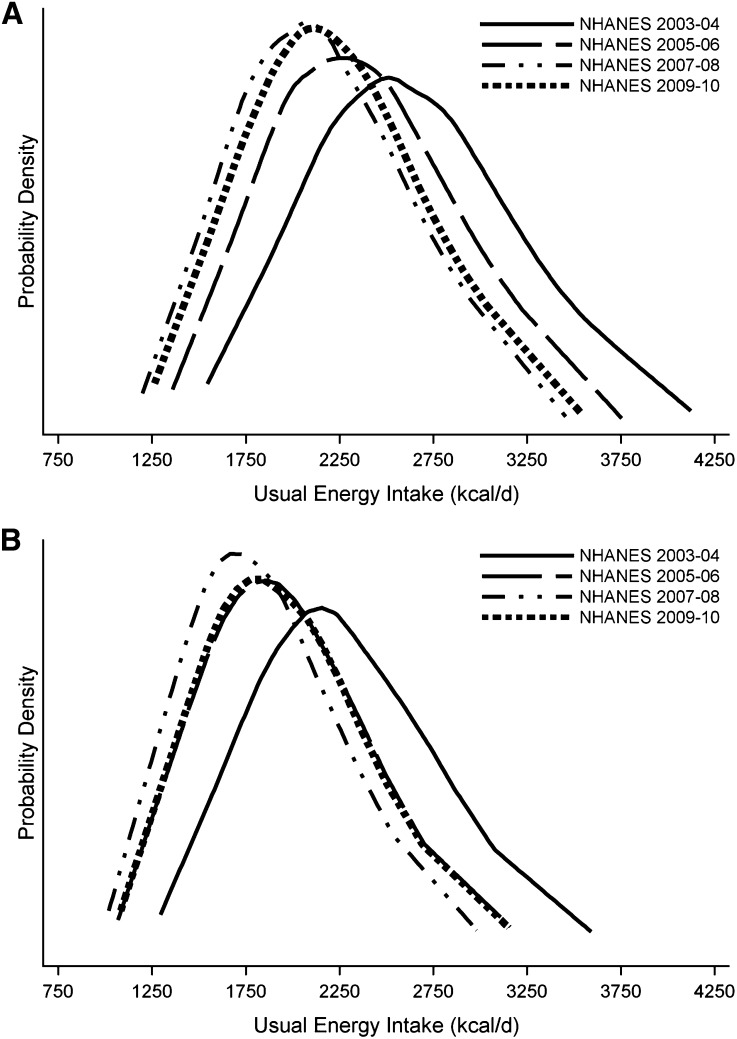
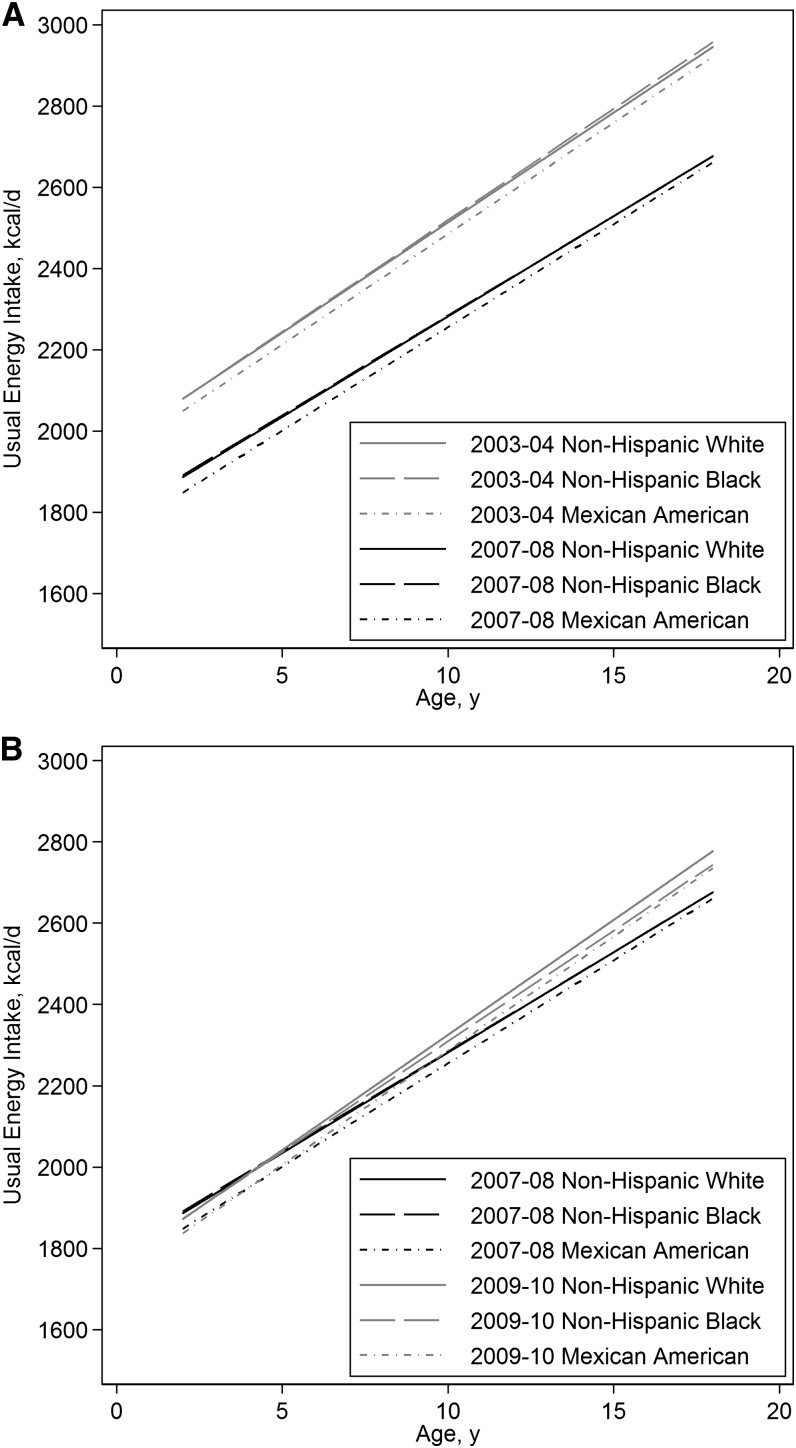
As shown in Figure 1 for adolescents, usual energy intakes estimated by using the NCI method declined from 2003–2004 to 2007–2008, with a downward shift in the entire distribution. Similar declines were observed for younger age groups (Supplemental Figs. 1 and 2). Figure 1 also shows that in 2009–2010, there was a substantial upward shift in the intake distribution among adolescents, with smaller changes among younger children (Supplement Figs. 1 and 2). Among adolescent boys, this shift led to intakes exceeding those in 2007–2008. In adolescent girls, there was a larger rightward shift in the intake distribution, which returned to 2005–2006 levels. As shown by using intakes at the 90th percentile, this pattern was similar across all race/ethnic groups (Fig. 2). There was a substantial reduction at the 90th percentile in intakes across all ages between 2003–2004 and 2007–2008 (Fig. 2A), followed by an increase in 2009–2010 among older children (Fig. 2B).
FIGURE 1.
Estimated distributions of usual total energy intake among U.S. adolescents (aged 12–18 y) by NHANES survey (2003–2004 to 2009–2010) for boys (A) and girls (B) based on the National Cancer Institute method, described in detail in the Methods section (36).
FIGURE 2.
Estimated usual energy intakes at the 90th percentile by age group and race/ethnicity on the basis of quantile regression results shown in Table 1: NHANES 2003–2004 vs. 2007–2008 (A) and NHANES 2007–2008 vs. 2009–2010 (B). P < 0.05 for differences in intakes at the 90th percentile in 2003–2004 vs. 2007–2008 at all ages. P < 0.05 for differences in intakes at the 90th percentile for the 12–18-y age group only. P > 0.10 for all differences among race/ethnic groups.
Quantile regression was used to test whether these shifts in intakes over time were significant, and whether they differed across population subgroups (coefficients shown in Supplemental Table 3). Predicted usual intakes (Table 1) from final models showed that overall, compared with the 2003–2004 survey, there was a large and significant reduction in intake at each percentile examined in 2007–2008. However, although reported intakes remained significantly lower than in 2003–2004, there were significant increases in intakes for 2009–2010 compared with 2007–2008 among older children (P = 0.01 for age group by year interactions, P = 0.07 for main effect). After declines between 2003–2004 and 2007–2008 of 159–240 kcal/d at the median, intakes in 2009–2010 among male and female adolescents increased by 72 and 100 kcal/d, 59 and 97 kcal/d, and 92 and 83 kcal/d at the 10th, 50th, and 90th percentiles, respectively. Similarly, among younger children, the substantial declines in reported intake observed across earlier survey cycles halted in 2009–2010, although the subsequent increase in intake was more modest than that observed in older children.
TABLE 1.
Usual energy intakes at the 10th, 50th, and 90th percentiles among U.S. children and adolescents: NHANES 2003–2004 to 2009–20101
| 10th Percentile |
50th Percentile (median) |
90th Percentile |
|||||||
| 2003–2004 | 2007–2008 | 2009–2010 | 2003–2004 | 2007–2008 | 2009–2010 | 2003–2004 | 2007–2008 | 2009–2010 | |
| kcal/d | kcal/d | kcal/d | |||||||
| Age group | |||||||||
| 2–5 y | |||||||||
| Boys | 1481 ± 20 | 1373 ± 15 | 1360 ± 12 | 1863 ± 14 | 1654 ± 10 | 1643 ± 13 | 2235 ± 21 | 1967 ± 24 | 1990 ± 17 |
| Girls | 1251 ± 17 | 1120 ± 14 | 1134 ± 16 | 1533 ± 16 | 1375 ± 9 | 1401 ± 11 | 1811 ± 16 | 1671 ± 18 | 1686 ± 16 |
| 6–11 y | |||||||||
| Boys | 1796 ± 22 | 1657 ± 23 | 1655 ± 21 | 2241 ± 13 | 2008 ± 12 | 2011 ± 12 | 2720 ± 27 | 2429 ± 22 | 2422 ± 26 |
| Girls | 1566 ± 21 | 1404 ± 21 | 1429 ± 19 | 1911 ± 13 | 1729 ± 14 | 1769 ± 13 | 2297 ± 27 | 2133 ± 23 | 2118 ± 17 |
| 12–18 y | |||||||||
| Boys | 1815 ± 27 | 1631 ± 24 | 1704 ± 23 | 2357 ± 16 | 2117 ± 22 | 2177 ± 19 | 2995 ± 15 | 2655 ± 17 | 2747 ± 26 |
| Girls | 1585 ± 19 | 1378 ± 21 | 1478 ± 20 | 2027 ± 13 | 1838 ± 16 | 1935 ± 16 | 2571 ± 20 | 2360 ± 24 | 2443 ± 29 |
| Race/ethnicity | |||||||||
| Non-Hispanic white | 1658 ± 17 | 1527 ± 16 | 1542 ± 17 | 2054 ± 14 | 1895 ± 10 | 1922 ± 12 | 2481 ± 16 | 2340 ± 18 | 2355 ± 18 |
| Non-Hispanic black | 1590 ± 16 | 1458 ± 15 | 1473 ± 19 | 2007 ± 16 | 1848 ± 12 | 1875 ± 12 | 2473 ± 19 | 2332 ± 22 | 2347 ± 20 |
| Mexican American | 1598 ± 19 | 1467 ± 18 | 1482 ± 18 | 2007 ± 14 | 1848 ± 12 | 1875 ± 13 | 2444 ± 17 | 2304 ± 18 | 2318 ± 17 |
| Other Hispanic | 1600 ± 26 | 1468 ± 25 | 1483 ± 22 | 2027 ± 17 | 1869 ± 15 | 1895 ± 14 | 2464 ± 21 | 2324 ± 24 | 2339 ± 20 |
| Other/mixed race | 1608 ± 26 | 1477 ± 28 | 1491 ± 29 | 1999 ± 22 | 1841 ± 18 | 1867 ± 18 | 2441 ± 28 | 2300 ± 25 | 2315 ± 21 |
Values are predicted estimates ± SEs of usual energy intake at each percentile from quantile regression models shown in detail in Supplemental Table 3.
There were no significant changes over this time period in the magnitude of energy intake disparities among vulnerable subgroups (P > 0.10 for all subgroup by survey cycle interaction terms). Moreover, coefficients from quantile regression models (Supplemental Table 3) showed that in contrast to the large and significant deficits in intake reported among non-Hispanic blacks and Mexican Americans compared with NHWs at lower percentiles, intake disparities at the 90th percentile (more relevant for obesity risk) were small and in some cases nonsignificant. Similarly, the absence of interactions indicated that parental education did not predict differences in how children’s energy intakes changed over this time frame. Moreover, unlike race/ethnicity, parental educational level was not strongly associated with disparities in children’s energy intake during this period. Associations between intake and parental education were significant only at the 10th percentile: at this percentile, intakes among children whose parents had less than a high school education were 39 kcal/d less than in those who were more educated.
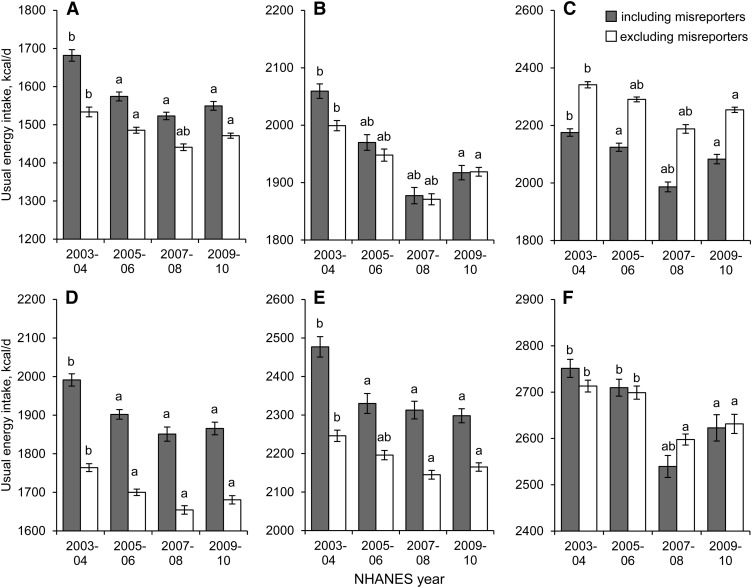
Figure 3 highlights the large decline in intakes across all age groups from 2003–2004 to 2007–2008 and the subsequent increase among adolescents in 2009–2010, additionally showing that these trends were unchanged after excluding energy intake misreporters. Excluding misreporters tended to decrease energy intakes at the median among children ages 2–5 and 6–11 y in whom over-reporting was highly prevalent but to increase the median intake among adolescents due to the higher prevalence of under-reporting at older ages.
FIGURE 3.
Adjusted predictions (with SEs) of usual energy intakes with and without misreporters from NHANES 2003–2004 to 2009–2010 at the 50th percentile for ages 2–5 y (A), 6–11 y (B), and 12–18 y (C) and at the 90th percentile for ages 2–5 y (D), 6–11 y (E), and 12–18 y (F). Misreporters were defined on the basis of a disparity in reported energy intake vs. estimated energy requirements exceeding ±1.5 SDs, where estimated energy requirement was estimated for each participant on the basis of doubly labeled water predictions and SDs were estimated on the basis of CVs in daily energy intake, predicted energy requirements, and measured energy expenditure as prescribed by Huang et al. (32). Results were consistent whether or not misreporters were included in the analysis. aDifferent from 2003–2004, P < 0.05; bdifferent from 2009–2010, P < 0.05.
Discussion
By using nationally representative data and methods to improve the estimation of usual intake, we found that a decline in reported energy intakes between 2003–2004 and 2007–2008 was not maintained in 2009–2010. An estimated initial decline of 159–240 kcal/d at the median was observed across all age groups. However, there was a subsequent significant increase in 2009–2010 observed among adolescents aged 12–18 y (median increases of 59 and 97 kcal/d in boys and girls, respectively), whereas intakes in younger children appeared to reach a plateau (changes of −11 to 40 kcal/d). Although intakes leveled off in younger children, the recent upturn in estimated usual intakes among adolescents may pose a threat to abatement of obesity in this age group. Indeed, consistent with our findings, in contrast to the plateaus and declines in obesity observed in younger children, the most recent analyses of NHANES data showed small increases in obesity among adolescents (3, 41). Importantly, to address concerns that a substantial proportion of reported energy intake data lacks validity as estimates of usual consumption (13), trends and age group disparities were re-examined after excluding participants likely to have misreported their usual intake; no meaningful differences were found.
The magnitude of the recent increase in median energy intake among adolescents is cause for concern, because the estimated average energy deficit needed to prevent further weight increases for children is 41 kcal/d (67 kcal/d in adolescents) (42, 43). The average energy deficit to reach the Healthy People 2010 goal (5% prevalence of obesity) by 2020 is estimated to be even larger, 120 kcal/d (177 kcal/d in adolescents). However, more so than changes at the mean or median, shifts at the upper end of the energy intake distribution are of particular concern given the persistently high levels of child obesity in the United States (3). With the skewed distributions commonly observed for dietary intake variables, focusing only on the mean may provide an incomplete picture of patterns of change. Among adolescent boys, the estimated upturn in intakes in 2009–2010 was larger at the 90th percentile than at the median (92 vs. 59 kcal/d).
As observed previously for long-term trends in reported intakes (10), race/ethnic group differences remained constant over this period. However, in contrast to large deficits in intake relative to NHWs at the 10th and 50th percentiles, the race/ethnic disparity in energy intake at the 90th percentile was either nonsignificant or relatively small in magnitude. Sustained, comparably high intakes across ethnic groups at this upper end of the distribution are consistent with the persistent disproportionate burden of overweight among minorities (3).
This study used several strategies in an effort to address concerns about the utility of a limited number of self-reported 24-h recalls to evaluate trends in energy intake. Rather than a single day of energy intake as in most previous studies that used NHANES data (15), this analysis estimated usual intakes using up to 2 d of recalls, accounting for intraindividual variation and incorporating covariates that predict under- and overestimation of habitual intake (16, 17). Other studies with multiple recalls (44) found that incorporating a second day and accounting for covariates such as weekend days can substantially improve estimation of usual energy intake. The NCI method used to estimate usual energy intake was shown to provide reliable estimates of the intake distribution (16). Our extension to apply quantile regressions enabled us to assess the significance of trends in intake at extremes of the distribution, as well as the significance of differences associated with factors such as age and race/ethnicity.
As in adults, studies that used doubly labeled water indicate that energy intakes in children may be substantially under- or over-reported (32, 45, 46). Another recent study identified substantial energy intake misreporting in NHANES adults (14). In that study, under-reporting estimates may have been elevated by applying basal metabolic rate equations that perform poorly in populations with high rates of obesity (46, 47). Importantly, our analysis, which estimated misreporting on the basis of doubly labeled water equations (32, 46), suggests that misreporting in children did not influence trends in intake. Neither analysis took into account weight loss from dieting, which may increase estimates of under-reporting that assume weight stability (48). Although both children (49) and adults (50) in NHANES reported such diets, the proportion of children who successfully achieve meaningful weight loss is uncertain, and, in contrast to adults, it was not possible to take this issue into account. The focus on recent intake trends in this article also reduced the likelihood of bias related to methodologic changes.
Although misreporting did not influence trends over time, it did modify estimates of intake, which were lower in younger children and higher in older children when misreporters were excluded. These changes reflect the higher proportion of over-reporting at younger ages (45). Under- and over-reporting prevalence estimates were 4% and 14% among children 2–5 y, 5% and 5% among children 6–11 y, and 13% and 2% among children 12–18 y in 2003–2004. In 2009–2010, the corresponding prevalence rates were 6% and 10% among children 2–5 y, 6% and 2% among children 6–11 y, and 14% and 1% among children 12–18 y. These estimates suggest that the prevalence of misreporting among children did not appreciably increase during this short time span. Under-reporting estimates were comparable to those derived on the basis of doubly labeled water (51, 52). Nonetheless, despite efforts to maximize the validity of the data used, it is not possible to ascertain to what extent error or bias in reported intakes may have influenced the trends observed (13).
Another limitation of this analysis is uncertainty with regard to the extent to which recent increases in energy intake among adolescents may be attributable to increases in physical activity. Although accelerometry data for part of this period suggest small increases in active time among younger children, there was no evidence of such increases among adolescents (53). It is unclear whether small increases in adolescent self-reports of active time on the basis of crude measures such as days per week being active reflect meaningful changes, and whether any increases in active time may have been offset by simultaneous increases in video game and computer use (54). Moreover, current knowledge is limited on the extent to which physical activity promotes higher energy intake, and whether it may do so more than sedentary activities such as television watching (55–57).
In summary, this study, which used nationally representative dietary data and accounted for variability in usual intake and misreporting, found evidence that short-term declines in the distribution of U.S. children’s energy intakes between 2003–2004 and 2007–2008 may have halted in 2009–2010 among younger children, with increases in intake among older children. Despite the limitation of relying on self-reported data, intake trends are consistent with temporal patterns in child obesity. This recent shift in energy intake trends, if real, may pose a threat to the positive changes in child overweight achieved just before this period.
Supplementary Material
Acknowledgments
The authors thank Frances L. Dancy for administrative assistance and Tom Swasey for graphics support. B.M.P. conceived of the project; D.R.M. implemented analyses with oversight from D.S.-A. and substantial input from M.A.M. and M.M.S.; and M.A.M. took the lead on interpretation of results and writing, with substantial input from D.S.-A., B.M.P., and M.M.S. All authors contributed to the design of the overall research plan. All authors read and approved the final manuscript.
Footnotes
Abbreviations used: NCI, National Cancer Institute; NHW, non-Hispanic white; PAL, physical activity level.
References
- 1.Swinburn B, Sacks G, Ravussin E. Increased food energy supply is more than sufficient to explain the US epidemic of obesity. Am J Clin Nutr 2009;90:1453–6. [DOI] [PubMed] [Google Scholar]
- 2.Swinburn BA, Sacks G, Lo SK, Westerterp KR, Rush EC, Rosenbaum M, Luke A, Schoeller DA, DeLany JP, Ravussin E. Estimating the changes in energy flux that characterize the rise in obesity prevalence. Am J Clin Nutr 2009;89:1723–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 2012;307:483–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA 2010;303:242–9. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Vital signs: obesity among low-income, preschool-aged children—United States, 2008–2011. MMWR Morb Mortal Wkly Rep 2013;62:629–34. [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Obesity prevalence among low-income, preschool-aged children—United States, 1998–2008. MMWR Morb Mortal Wkly Rep 2009;58:769–73. [PubMed] [Google Scholar]
- 7.Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, Harris WA, Lowry R, McManus T, Lim C, et al. Youth risk behavior surveillance—United States, 2007. MMWR Surveill Summ 2008;57:1–131. [PubMed] [Google Scholar]
- 8.Pan L, Blanck HM, Sherry B, Dalenius K, Grummer-Strawn LM. Trends in the prevalence of extreme obesity among us preschool-aged children living in low-income families, 1998–2010. JAMA 2012;308:2563–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ford ES, Dietz WH. Trends in energy intake among adults in the United States: findings from NHANES. Am J Clin Nutr 2013;97:848–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kant AK, Graubard BI. 20-Year trends in dietary and meal behaviors were similar in U.S. children and adolescents of different race/ethnicity. J Nutr 2011;141:1880–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Troiano RP, Briefel RR, Carroll MD, Bialostosky K. Energy and fat intakes of children and adolescents in the united states: data from the national health and nutrition examination surveys. Am J Clin Nutr 2000;72:1343S–53S. [DOI] [PubMed] [Google Scholar]
- 12.Kant AK, Graubard BI. Family income and education were related with 30-year time trends in dietary and meal behaviors of American children and adolescents. J Nutr 2013;143:690–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schoeller DA, Thomas D, Archer E, Heymsfield SB, Blair SN, Goran MI, Hill JO, Atkinson RL, Corkey BE, Dhurandar V, et al. Self-report–based estimates of energy intake offer an inadequate basis for scientific conclusions. Am J Clin Nutr 2013;97:1413–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Archer E, Hand GA, Blair SN. Validity of U.S. nutritional surveillance: National Health and Nutrition Examination Survey caloric energy intake data, 1971–2010. PLoS ONE 2013;8:e76632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ervin RB, Ogden CL. Trends in intake of energy and macronutrients in children and adolescents from 1999–2000 through 2009–2010. NCHS data brief, no. 113. Hyattsville (MD): National Center for Health Statistics; 2013. [PubMed] [Google Scholar]
- 16.Tooze JA, Kipnis V, Buckman DW, Carroll RJ, Freedman LS, Guenther PM, Krebs-Smith SM, Subar AF, Dodd KW. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: the NCI method. Stat Med 2010;29:2857–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tooze JA, Midthune D, Dodd KW, Freedman LS, Krebs-Smith SM, Subar AF, Guenther PM, Carroll RJ, Kipnis V. A new statistical method for estimating the usual intake of episodically consumed foods with application to their distribution. J Am Diet Assoc 2006;106:1575–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Madsen KA, Weedn AE, Crawford PB. Disparities in peaks, plateaus, and declines in prevalence of high BMI among adolescents. Pediatrics 2010;126(3):434–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang Y. Disparities in pediatric obesity in the United States. Adv Nutr 2011;2:23–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Health and Nutrition Examination Survey data. Hyattsville (MD): National Center for Health Statistics; CDC; U.S. Department of Health and Human Services; 2003–2004 [cited 2012 Oct 17]. Available from: http://www.cdc.gov/nchs/nhanes/about_nhanes.htm.
- 21.National Health and Nutrition Examination Survey data. Hyattsville (MD): National Center for Health Statistics; CDC; U.S. Department of Health and Human Services; 2007–2008 [cited 2012 Oct 17]. Available from: http://wwwn.cdc.gov/nchs/nhanes/search/nhanes07_08.aspx.
- 22. National Health and Nutrition Examination Survey data. Hyattsville (MD): National Center for Health Statistics; CDC; U.S. Department of Health and Human Services; 2005–2006 [cited 2012 Oct 17]. Available from: http://wwwn.cdc.gov/nchs/nhanes/search/nhanes05_06.aspx.
- 23.Bodner J, Perloff B. Databases for analyzing dietary data—the latest word from What We Eat in America. J Food Compos Anal 2003;16:347–58. [Google Scholar]
- 24.USDA. Food and Nutrient Database for Dietary Studies, 2.0. Beltsville (MD): USDA, Agricultural Research Service, Food Survey Research Group; 2006.
- 25.USDA. Food and Nutrient Database for Dietary Studies, 4.1. Beltsville (MD): USDA, Agricultural Research Service, Food Survey Research Group; 2010.
- 26.USDA. Food and Nutrient Database for Dietary Studies, 3.0. Beltsville (MD): USDA, Agricultural Research Service, Food Survey Research Group; 2008.
- 27.National Health and Nutrition Examination Survey data. Hyattsville (MD): National Center for Health Statistics; CDC; U.S. Department of Health and Human Services; 2009–2010.
- 28.Slining MM, Ng SW, Popkin BM. Food companies’ calorie-reduction pledges to improve U.S. diet. Am J Prev Med 2013;44:174–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Slining MM, Popkin B. Trends in intakes and sources of solid fats and added sugars among U.S. children and adolescents: 1994–2010. Pediatr Obes 2013;8:307–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moshfegh AJ, Rhodes DG, Baer DJ, Murayi T, Clemens JC, Rumpler WV, Paul DR, Sebastian RS, Kuczynski KJ, Staples RC, et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr 2008;88:324–32. [DOI] [PubMed] [Google Scholar]
- 31.Institute of Medicine. Dietary Reference Intakes for energy, carbohydrates, fiber, fat, protein and amino acids (macronutrients). Washington: National Academies Press; 2005. [Google Scholar]
- 32.Huang TTK, Roberts SB, Howarth NC, McCrory MA. Effect of screening out implausible energy intake reports on relationships between diet and BMI. Obes Res 2005;13:1205–17. [DOI] [PubMed] [Google Scholar]
- 33.Tudor-Locke C, Troiano RP. A catalog of rules, variables, and definitions applied to accelerometer data in the National Health and Nutrition Examination Survey. Prev Chronic Dis 2012;9:E113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.LeBlanc AG, Janssen I. Difference between self-reported and accelerometer measured moderate-to-vigorous physical activity in youth. Pediatr Exerc Sci 2010;22:523–34. [DOI] [PubMed] [Google Scholar]
- 35.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc 2008;40:181–8. [DOI] [PubMed] [Google Scholar]
- 36.Parsons RMS, Buckman DW, Tooze JA, Dodd KW. User's guide for analysis of usual intakes. National Cancer Institute; 2009 [cited 2012 Oct 17]. Available from: http://appliedresearch.cancer.gov/diet/usualintakes/Users_Guide_Mixtran_Distrib_Indivint_1.1.pdf.
- 37.Korn EL, Graubard BI. Analysis of health surveys. Hoboken (NJ): John Wiley and Sons; 1999. [Google Scholar]
- 38.Cade BS, Noon BR. A gentle introduction to quantile regression for ecologists. Front Ecol Environ 2003;1:412–20. [Google Scholar]
- 39.Koenker R, Bassett G. Regression quantiles. Econometrica 1978;46:33–50. [Google Scholar]
- 40.Kipnis V, Midthune D, Buckman DW, Dodd KW, Guenther PM, Krebs-Smith SM, Subar AF, Tooze JA, Carroll RJ, Freedman LS. Modeling data with excess zeros and measurement error: application to evaluating relationships between episodically consumed foods and health outcomes. Biometrics 2009;65:1003–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang YC, Gortmaker SL, Sobol AM, Kuntz KM. Estimating the energy gap among US children: a counterfactual approach. Pediatrics 2006;118:e1721–e33. [DOI] [PubMed] [Google Scholar]
- 43.Wang YC, Orleans CT, Gortmaker SL. Reaching the Healthy People goals for reducing childhood obesity: closing the energy gap. Am J Prev Med 2012;42:437–44. [DOI] [PubMed] [Google Scholar]
- 44.Ma Y, Olendzki BC, Pagoto SL, Hurley TG, Magner RP, Ockene IS, Schneider KL, Merriam PA, Hébert JR. Number of 24-hour diet recalls needed to estimate energy intake. Ann Epidemiol 2009;19:553–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Burrows TL, Martin RJ, Collins CE. A systematic review of the validity of dietary assessment methods in children when compared with the method of doubly labeled water. J Am Diet Assoc 2010;110:1501–10. [DOI] [PubMed] [Google Scholar]
- 46.Mendez MA, Popkin B, Buckland G, Schroder H, Amiano P, Barricarte A, Huerta J-M, Quirós J, Sánchez M-L, González C. Alternative methods of accounting for under- and overreporting in associations between dietary intakes and body mass index. Am J Epidemiol 2011;173:448–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Frankenfield DC. Bias and accuracy of resting metabolic rate equations in non-obese and obese adults. Clin Nutr 2013;32(6):976–82. [DOI] [PubMed] [Google Scholar]
- 48.Rennie KL, Coward A, Jebb SA. Estimating under-reporting of energy intake in dietary surveys using an individualised method. Br J Nutr 2007;97:1169–76. [DOI] [PubMed] [Google Scholar]
- 49.Chung AE, Perrin EM, Skinner AC. Accuracy of child and adolescent weight perceptions and their relationships to dieting and exercise behaviors: a NHANES study. Acad Pediatr 2013;13:371–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nicklas JM, Huskey KW, Davis RB, Wee CC. Successful weight loss among obese U.S. adults. Am J Prev Med 2012;42:481–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fisher JO, Johnson RK, Lindquist C, Birch LL, Goran MI. Influence of body composition on the accuracy of reported energy intake in children. Obes Res 2000;8:597–603. [DOI] [PubMed] [Google Scholar]
- 52.Subar AF, Kipnis V, Troiano RP, Midthune D, Schoeller DA, Bingham S, Sharbaugh CO, Trabulsi J, Runswick S, Sunshine J, et al. Using intake biomarkers to evaluate the extent of dietary misreporting in a large sample of adults: the OPEN study. Am J Epidemiol 2003;158:1–13. [DOI] [PubMed] [Google Scholar]
- 53.Gortmaker SL, Lee R, Cradock AL, Sobol AM, Duncan DT, Wang YC. Disparities in youth physical activity in the United States: 2003–2006. Med Sci Sports Exerc 2012;44:888–93. [DOI] [PubMed] [Google Scholar]
- 54.Iannotti RJ, Wang J. Trends in physical activity, sedentary behavior, diet, and BMI among US adolescents, 2001–2009. Pediatrics 2013;132:606–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thivel D, Aucouturier J, Doucet E, Saunders TJ, Chaput JP. Daily energy balance in children and adolescents. Does energy expenditure predict subsequent energy intake? Appetite 2013;60:58–64. [DOI] [PubMed] [Google Scholar]
- 56.Donnelly JE, Herrmann SD, Lambourne K, Szabo AN, Honas JJ, Washburn RA. Does increased exercise or physical activity alter ad-libitum daily energy intake or macronutrient composition in healthy adults? A systematic review. PLoS ONE 2014;9:e83498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chaput JP, Klingenberg L, Astrup A, Sjodin AM. Modern sedentary activities promote overconsumption of food in our current obesogenic environment. Obesity Rev 2011;12:e12–20. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.