Abstract
There has been an increasing body of literature regarding arthroscopic management of femoroacetabular impingement (FAI). Refinement of arthroscopic techniques has allowed for more complete management of FAI, and meta-analysis and systematic reviews have shown comparable outcomes to surgical hip dislocation with appropriate indications. There are still, however, pathomorphologies that are not accessible or much more challenging to address arthroscopically, and open corrective procedures should be considered in these situations. Extra-articular FAI is receiving increased attention and can be secondary to anterior inferior iliac spine/subspine impingement, trochanteric-pelvic impingement, and ischio-femoral impingement. Femoral and acetabular version and their impact on hip stability as well as the concept of impingement induced instability are being increasingly recognized. Acetabular labral and capsular management and repair techniques have also received increased attention. Finally, 3-dimensional imaging and dynamic software analysis are beginning to emerge as potential tools to better evaluate hip pathomorphology.
Keywords: Arthroscopy, Hip arthroscopy, Femoroacetabular impingement, FAI, Labral repair, Hip impingement, Extra-articular hip impingement
Introduction
Femoroacetabular impingement (FAI) is an increasingly recognized hip disorder that is classically described as either Cam-type (femoral sided) or Pincer-type (acetabular sided) FAI [1–3]. FAI has also been implicated as a causative factor for the development of hip arthritis [3]. Arthroscopic FAI correction has had an increasing role for the management of FAI, and indications regarding arthroscopic vs open surgical approaches continue to evolve. More recent studies have significantly improved our overall understanding of FAI. New concepts or refinement of previously described concepts such as extra-articular impingement, role of acetabular and femoral version, impingement induced instability, capsular management techniques, and the role for capsular and labral repair/preservation have been reported. The current paper will review the literature regarding FAI over the last year and attempt to summarize important concepts and data regarding FAI and in particular with respect to arthroscopic FAI correction.
Arthroscopic indications and outcomes
The indications for arthroscopic management of intra-articular FAI continue to evolve. It is critical to recognize those areas accessible to arthroscopic treatment and those that require open surgical procedures to address. There is also a steep learning curve and more challenging cases that can be predictably managed by experienced hip arthroscopists might be better addressed with open approaches for surgeons earlier in their experience.
The acetabulum
The antero-superior acetabular rim and labrum can be predictably managed with an arthroscopic approach. The posterior and postero-inferior acetabular rim is more challenging to access for rim resection and labral repair, requires greater degrees of traction in some cases, and with experience can be managed arthroscopically. Therefore, cases of global acetabular over-coverage can be treated arthroscopically with experience. Protrusio acetabula, however, should be approached with caution arthroscopically, as this can present with a large lunate fossa and relatively deficient articular cartilage that might be better treated with a corrective pelvic osteotomy [4]. In addition, protrusio can be associated with proximal femoral deformities such as coxa vara that cannot be addressed arthroscopically. Although milder degrees of acetabular retroversion can be treated with rim resection, more severe degrees of acetabular retroversion with significant posterior wall deficiency might be best treated with anteversion periacetabular osteotomy (PAO). It is critical to evaluate for acetabular dysplasia, and it is not uncommon to have both impingement and dysplastic features concurrently. Patients with a predominance of instability findings on clinical examination and imaging studies that reveal more than just borderline dysplastic features might be best treated with corrective pelvic osteotomies.
The femur
The anterior femoral head-neck junction, which is best visualized on lateral radiographs, is predictably accessed arthroscopically. One recent study evaluated cam decompression performed arthroscopically compared with surgical hip dislocation and found improved correction with experience without significant differences for correction between the surgical approaches [5]. Medial and lateral cam deformities, which are visualized on AP radiographs, are much more challenging to access arthroscopically (Fig. 1). Although postero-superior (lateral) and postero-inferior (medial) deformities can be reached with experience, a prior study reported that the AP correction was more predictably managed with surgical hip dislocation [6]. Symptomatic posterior femoral head-neck deformities, best visualized on lateral radiographs, cannot be predictably accessed arthroscopically. These posterior femoral head-neck deformities should be managed with SHD when symptomatic. It is also critical to evaluate femoral neck shaft angle, neck length, femoral version, and trochanteric offset issues when contemplating the most appropriate surgical approaches. Coxa vara, coxa breva, femoral retroversion, and greater trochanteric overgrowth/prominence all increase the degree of cam/proximal femoral-type FAI.
Fig. 1.
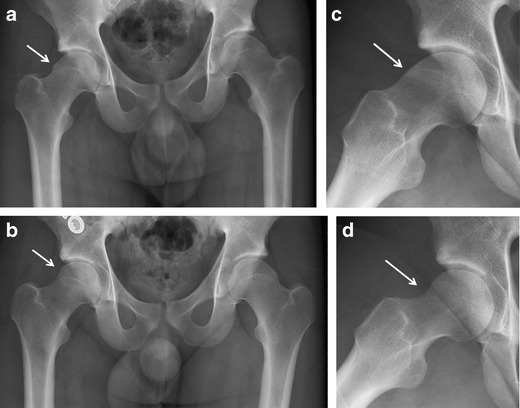
a, Preoperative AP radiograph for a 22 year old collegiate hockey player with right hip pain reveals a cam deformity that extends lateral/postero-superior. b, Postoperative AP radiograph demonstrates adequate correction of this more challenging Cam deformity location with an arthroscopic approach. c, Preoperative lateral radiograph reveals a typical anterior cam deformity, and a postoperative lateral radiograph (d) demonstrates correction of the cam deformity arthroscopically
Systematic reviews have been performed looking at the efficacy of both open and arthroscopic FAI corrective procedures [7–11]. In 1 study, the evidence supporting arthroscopic treatment of FAI was fair [7]. Other studies looking at combined open and arthroscopic approaches found that the majority of patients improved regardless of the surgical approach, with pain relief in 68 %-96 % of patients, and no significant differences for eventual outcomes based on the surgical approach [8–10]. Based on the limited information with regards to specific diagnosis for the studies reviewed, it is difficult to state whether the patients undergoing arthroscopic and open surgical procedures were comparable with respect to pathomorphologies. Currently at institutions that perform both open and arthroscopic FAI corrective procedures, the majority of patients undergoing open corrective procedures for FAI have larger, more complex deformities. Moving forward, it will likely be difficult to directly compare SHD with arthroscopic FAI correction as the patient populations may be quite different. In the end, SHD and hip arthroscopy should be considered approaches rather than procedures for managing various patterns of FAI, and indications for the various approaches should be based on the pathomechanics at work and surgeon experience.
Extra-articular FAI
Although intra-articular FAI has been well described, it is clear that there are cases of FAI that result from extra-articular impingement between the proximal femur and pelvis. The sites of extra-articular impingement described include AIIS/subspine impingement, trochanteric-pelvic impingement, and ischio-femoral impingement. AIIS or subspine impingement has received increased attention recently [12•, 13, 14]. A distally or anteriorly prominent AIIS can be the result of a prior AIIS apophyseal avulsion, prior rectus femoris avulsion with subsequent ossification of the origin, as a result of overcorrection after periacetabular osteotomy, or seen in the setting of acetabular retroversion [14]. These patient’s typically present with straight hip flexion limitations and pain and lack of relief of their flexion based pain with intra-articular anesthetic injection [14]. The first report of arthroscopic subspine decompression reported on 3 representative cases with a mean 18-point improvement for modified HHS at 1 year follow-up [14]. A subsequent case series reported on 10 patients that underwent an arthroscopic subspine decompression for prior avulsion injury [12•]. At a mean 14.7 month follow-up the modified HHS improved a mean 34 points and hip flexion range of motion improved a mean 18 degrees [12•]. Using 3-dimensional (3D) CT and dynamic software analysis, Hetsroni et al. classified AIIS morphology as type 1 (distal AIIS ends proximal to the acetabular rim), type 2 (distal AIIS extends to the acetabular rim), and Type 3 (distal AIIS extends beyond the acetabular rim), and noted decreased flexion and internal rotation ROM with increasing subtypes [13]. The AIIS can be predictably decompressed arthroscopically with the extent of decompression based on the preoperative deformity.
The greater trochanter can also impinge against the pelvis and is classically seen in the setting of Legge Calve Perthes disease, with coxa breva, vara, and a prominent greater trochanter [15, 16]. More subtle cases of trochanteric-pelvic impingement are being described and typically present with motion limitations that are greater than expected based on the pathomorphology seen on plain radiographs and lack of relief with intra-articular anesthetic injections. Anterior trochanteric impingement with flexion internal rotation can be seen in the setting of relative femoral retroversion whereas posterior trochanteric impingement with external rotation can be seen in the setting of increased femoral anteversion. A recent study using 3D CT scan motion analysis evaluated 13 hips with valgus hips and increased antetorsion compared with 22 hips with FAI and 27 normal hips [17]. Hips with coxa valga and increased antetorsion had impingement zones that were more frequently posterior and extra-articular and to a lesser extent anterior against the AIIS [17]. Dynamic ultrasound can assist in the diagnosis, and open trochanteric transfer procedures have been recommended for persistent limiting symptoms. Ischiofemoral impingement is a less commonly described source of extra-articular impingement that occurs when the space between the proximal femur/lesser trochanter and ischial tuberosity is narrowed [18, 19]. These patients typically have pain with hip extension and can be developmental or secondary to prior apophyseal or myotendinous injuries at the lesser trochanter or ischial tuberosity. Magnetic resonance imaging reveals edema within the quadratus femoris muscle and relief with ultrasound or CT guided anesthetic injection into the area of impingement can be diagnostic [18]. Treatment of persistent limiting symptoms can be treated with decompression at the level of the ischial tuberosity, lesser trochanteric decompression/excision or transfer of the lesser trochanter. Specific techniques and outcomes after such procedures, however, require further study.
Version
Variations in acetabular and in particular femoral version have been increasingly discussed with respect to the relationship between the acetabulum and femur and their contributions to hip stability and impingement. There appears to be a significant variability for normal version and a recent 3D CT evaluation of 230 normal hips suggested that there may be a normal complementary developmental relationship between the proximal femur and acetabulum [20]. In some patients, for instance, the presence of acetabular retroversion may not be pathologic and in fact be compensated for by increased femoral anteversion/torsion. In fact, in a recent unpublished study looking at more than 400 CT scans in asymptomatic hips, a positive posterior wall sign (30 %) and acetabular retroversion (15 %) were common findings in asymptomatic hips and more common in males indicating that these imaging findings may be normal variants for a number of patients (Larson CM, et al., unpublished data). As noted previously, increased femoral antetorsion predisposed to posterior extra-articular impingement using 3D CT motion analysis software [17]. In addition, a recent study looked at femoral version in a cohort of 67 consecutive arthroscopic psoas tenotomies [21]. This study found poorer outcomes after such releases in patients who had excessive (>25 degrees) femoral anteversion and suggested that the psoas myotendinous complex may play a significant role in dynamic anterior stability in hips with subtle anterior instability secondary to excessive femoral anteversion [21]. The proposed concepts are as follows: excessive acetabular anteversion can result in anterior hip instability and posterior impingement, excessive acetabular retroversion can result in anterior impingement and posterior hip instability, excessive femoral neck anteversion can result in anterior hip instability and posterior impingement, and excessive femoral neck retroversion can result in anterior hip impingement and posterior hip instability. Ultimately the relationship between femoral and acetabular morphologies need to be considered in order to better define the anatomical relationships as potentially pathologic vs compensatory, but clearly further study is required in order to better understand these complex morphologic variations.
Impingement induced instability
The concept of FAI induced instability has been recently described [22–24]. The proposed theory is that anteriorly based FAI and in particular cam deformity can lever against the anterior rim in flexion with resultant posterior subluxation/dislocation. Steppacher et al. compared 53 hips that had a prior history of traumatic posterior hip dislocation with 85 normal hips and found a higher prevalence of cam deformities and acetabular retroversion in the dislocation group [22]. Another recent article looked at a series of 22 athletes with a confirmed diagnosis of posterior hip dislocation with an associated small posterior wall fracture. Sixteen of 18 athletes had significant FAI and in particular a large cam deformity and had sustained a low energy twisting or noncontact injury [24]. One-half of the patients required subsequent arthroscopic hip surgery and 20 of 22 athletes ultimately returned to their sport with a mean 4 years (range, 2–16 years) follow-up [24]. Both of these studies proposed the concept of anterior cam deformity levering on the anterior rim predisposing these patients to posterior instability episodes [22, 24]. Treatment of the cam deformity in these patients, when surgical treatment is indicated, might have the secondary benefit of decreasing the potential for further FAI induced posterior instability.
There are, however, more subtle cases of FAI induced instability typically seen in females, which can be seen with high range of motion activities and in the setting of capsular laxity. Radiographs may be normal or show findings consistent with high range of motion impingement such as distal femoral neck and AIIS sclerotic changes. These patients may participate in activities requiring excessive range of motion such as dance, gymnastics, and yoga. Recent studies have looked at impingement with extreme hip range of motion in ballet dancers [25•, 26]. Two recent studies evaluated impingement tests, hip range of motion, and MRI findings (additional splits position for dancers) in professional female ballet dancers compared with healthy matched females [25•, 26]. No differences between groups for hip range of motion, alpha angles, acetabular and femoral version, and acetabular depth were found between the groups and hips in both groups were noted to be morphologically normal [25•]. Hip MRI’s for dancers in the splits position revealed femoral head subluxations and labral and chondral pathology that was typically postero-superior compared with antero-superior in location for non-dancers [25•]. These studies support the concept of impingement induced instability that can occur in the absence of obvious FAI or potentially in the presence of dysplasia with extreme range of motion activities. Capsular laxity may also play a role with increased translation of the femur in the acetabulum with movements that might allow for greater degrees of subluxation. These can be very challenging patients to treat when conservative measures fail. If dysplasia is the predominate finding, corrective osteotomies should be considered. If high range of motion impingement findings is present, femoral resections further distal on the neck, AIIS decompressions, and capsular repairs/plications in the presence of laxity might be considered as part of the surgical treatment. Outcomes after surgical management are needed in order to better determine the best treatment options in this difficult patient population.
The acetabular labrum
Prior studies have reported that the acetabular labrum functions to provide a seal and decrease contact stresses in the hip joint compared with the hip without a labrum [27]. Two prior studies looking at consecutive groups of labral excision vs debridement after surgical hip dislocation and arthroscopy noted better outcomes scores in the labral preservation group at early follow-up [28, 29]. Larson et al. recently reported an update on the arthroscopic repair vs debridement cohort at a mean 3.5 year follow-up (range 2 to 6 years) [30]. They found that labral preservation (50 hips) continued to have better outcomes (MHHS, SF-12, VAS) compared with focal labral excision (44 hips) with 92 % good to excellent results vs 68 % good to excellent results, respectively [30]. More recently Krych et al. conducted a prospected, randomized study looking at labral repair (18 patients) vs selective labral debridements (18 patients) in females [31]. They noted better outcomes with labral repair for the ADL and Sports subscale of the Hip Outcomes Score at a mean 32 months follow-up [31]. A recent study looked at the sealing function (fluid efflux) of the native labrum, labral tear, labral repair, partially resected labrum, and labral reconstruction in a cadaveric model [32]. This study reported that the native labrum and labral repair provided a better seal (less fluid efflux) than the labral tear, partial resection, and labral resection conditions [32]. The native labrum, however, still provided a better seal than labral repair, and interestingly, labral reconstruction was similar to the labral tear and partial resection conditions with regards to maintaining the labral sealing function [32]. Labral reconstruction can be performed in the labrum deficient state as seen in the setting of global acetabular over-coverage with rim ossification and prior labral resection. There is very limited literature with respect to outcomes after arthroscopic labral reconstruction. One study reported on 47 patients who underwent arthroscopic labral reconstruction with iliotibial band autograft reconstruction with a mean 18 months follow-up [33]. Ten patients were either lost to follow-up or underwent total hip arthroplasty, and the remaining were reported to have a mean 23 point improvement using the modified Harris Hip Score [33]. Based on these recent clinical and cadaveric studies, labral preservation/repair is preferred to labral excision/debridement as part of joint preservation procedures for the majority of cases. Further follow-up and study, however, are required to determine the long term advantages of labral preservation vs excision/debridement and the role for labral reconstructive procedures.
The hip capsule
There has been recent interest in capsular management techniques in order to maximize exposure to deformities and preserve/repair/plicate the capsule in order to preserve soft tissue stability (Fig. 2) [34]. A recent systematic review reported on 47 published articles that met the inclusion criteria and concluded that the capsule was an important hip stabilizer and that surgeons should be competent in repair and plication techniques in certain situations when performing hip arthroscopy [35]. A prior study evaluated 11 patients with clinical and imaging evidence for chronic capsular incompetence [36]. A loss of normal recoil with passive external rotation of the hip and MRI evidence for insertional thinning of the lateral ligament, attenuation of the iliofemoral ligament with hip external rotation, and appearance of laxity of the iliofemoral ligament with maximal external rotation were all felt to be consistent with anterior capsular laxity [36]. Although patients with connective tissue disorders such as Ehlers Danlos may be the most extreme example, there appears to be a subset of patients with activity induced anterior laxity and subtle dysplastic variants/borderline dysplasia for which preservation or even plication of the capsule might be an important factor to consider if arthroscopic management is pursued. In addition, there has been a recent case report of a mildly dysplastic hip that underwent labral repair, partial ligamentum teres debridement, and modest capsulotomy without repair [37]. Despite preservation of the labrum and no rim resection, this patient developed hip subluxation 3 months post-operatively with end stage arthritis at a year. This indicates that preservation of the anterior capsule/iliofemoral ligament might play a critical role in stability for some hips and in particular for those with borderline dysplastic features [37]. There are no published controlled studies to date, however, reporting outcomes and or stability after repaired and unrepaired capsulotomies.
Fig. 2.
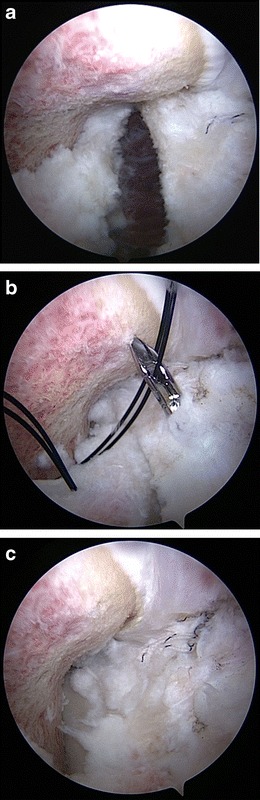
a, Arthroscopic view of the R hip in a female with extreme ROM/capsular laxity induced instability reveals the interportal capsulotomy after labral repair and femoral resection. b, A looped suture is shuttled from the distal to the proximal limb of the capsular incision and retrieved with a penetrating grasper. c, Sutures are then tied in order to close and mildly plicate the capsule
Capsulotomy techniques are also potentially important to maximize exposure and ability to correct impingement deformities during hip arthroscopy [34]. Minimal capsulotomies at the level of the portals, interportal capsulotomies, T capsulotomy, and capsulectomies have been proposed as techniques to improve arthroscopic exposure. In order to address lateral and medial cam deformities beyond the medial and lateral synovial folds, various positions of the hip flexion, extension, internal and external rotation, and occasionally traction can help to reach these difficult regions. Larger interportal (anterior to posterolateral portal) and T cut capsulotomies can significantly improve the ability to access these regions. The current author favors a large interportal capsulotomy followed by capsular repair or plication when indicated. Although a T-cut can also be utilized and provides excellent exposure, it may be best to avoid this additional T-cut in hips with pathomorphology consistent with subtle dysplastic variants. It should also be noted that capsular plication alone should not be considered a treatment option for more significant degrees of dysplasia, which is best addressed with corrective pelvic osteotomies.
3D imaging and dynamic evaluation
Although plain radiographs have been the cornerstone for defining hip pathomorphology, it has become clear that 2-dimensional radiographic indices occasionally lead to errors in diagnosis secondary to improper pelvic alignment, and are not highly reliable between surgeons. As a result, there has been an increased interest in 3D evaluation of the hip. A recent study looked at 100 CT scans in hips with symptomatic cam deformities and compared the maximal alpha angles as determined on plain radiographs, CT scans, and with software CT analysis [38]. The maximal alpha angle was typically located between 12:45 and 1:45 on the clock face, and the study reported that the automated 3D assessment provided the most accurate depiction of the cam deformity [38]. Another study compared the presence of a cross over sign on plain radiographs with 3D CT acetabular version measurements [39]. Seventy-two percent (38 of 53 hips) of plain radiographs had a positive cross over sign but only 50 % of those had acetabular retroversion based on CT measurements. The other 50 % had an anteverted acetabulum by CT scan and a low AIIS was responsible for the appearance of a cross over sign on plain radiographs in each of those cases [39]. Three-dimensional CT scans allow for a predictable correction of pelvic alignment in order to more accurately evaluate acetabular version and femoral head coverage by the acetabular rim. A recent study evaluated the accuracy of standardized AP pelvic radiographs for diagnosing acetabular retroversion (cross over and posterior wall signs) compared with 3D CT version measurements after correction for pelvic tilt [40]. They found a low level of agreement for cross over and posterior wall signs between plain radiographs and CT scans [40]. They further concluded that plain radiographs have limited diagnostic accuracy for evaluating acetabular retroversion secondary to variations in pelvic tilt [40].
In addition, 3D CT range of motion software has begun to emerge in the literature as a useful research tool. One study evaluated CT range of motion analysis in 30 patients undergoing surgical hip dislocation for FAI [41•]. The accuracy of the CT range of motion analysis was compared with the intra-operative findings at the time of surgical hip dislocation and was found to have a high degree of accuracy for defining the areas of impingement [41•]. As previously noted, a prior study used 3D CT software motion analysis to evaluate range of motion with various degrees of AIIS deformity [13]. They reported decreased forward flexion and internal rotation range of motion with greater AIIS deformities using this novel software [13]. Although this dynamic software analysis has been utilized from a research standpoint to date, it may become available for clinical use in the future. This would allow for preoperative dynamic evaluation of the hip and potentially virtual bony resections in order to better define appropriate surgical corrections and identify the most appropriate surgical approaches based on the areas of impingement.
Conclusions
Our understanding of FAI is rapidly advancing. The introduction of new concepts and refinement of traditional concepts are significantly adding to our understanding of hip pathomechanics. These recent studies regarding FAI concepts and surgical outcomes continue to better define the role for arthroscopic management of FAI.
Compliance with Ethics Guidelines
Conflict of Interest
Christopher M. Larson is a consultant for and has stock options in A3 Surgical. He is also a consultant for Smith and Nephew. Rebecca M. Stone declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Lavigne M, Parvizi J, Beck M, et al. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61–66. doi: 10.1097/00003086-200401000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Beck M, Leunig M, Parvizi J, et al. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67–73. doi: 10.1097/00003086-200401000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 4.Ferguson SJ, Liechti EF, Tannast M. Joint degeneration pattern in severe pincer impingement and its implications for surgical therapy. In: 2012 ORS annual meeting program. Rosemont, IL: Orthopaedic Research Society, 2012.
- 5.Büchler L, Neumann M, Schwab JM, et al. Arthroscopic versus open cam resection in the treatment of femoroacetabular impingement. Arthroscopy. 2013;29:653–660. doi: 10.1016/j.arthro.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 6.Bedi A, Zaltz I, De La Torre K, Kelly BT. Radiographic comparison of surgical hip dislocation and hip arthroscopy for treatment of cam deformity in femoroacetabular impingement. Am J Sports Med. 2011;39(Suppl):20S–28S. doi: 10.1177/0363546511412734. [DOI] [PubMed] [Google Scholar]
- 7.Ng VY, Arora N, Best TM, Pan X, Ellis TJ. Efficacy of surgery for femoroacetabular impingement: a systematic review. Am J Sports Med. 2010;38:2337–2345. doi: 10.1177/0363546510365530. [DOI] [PubMed] [Google Scholar]
- 8.Botser IB, Smith TW, Jr, Nasser R, Domb BG. Open surgical dislocation vs arthroscopy for femoroacetabular impingement: a comparison of clinical outcomes. Arthroscopy. 2011;27:270–278. doi: 10.1016/j.arthro.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 9.Clohisy JC, St John LC, Schutz AL. Surgical treatment of femoroacetabular impingement: a systematic review of the literature. Clin Orthop Relat Res. 2010;468:555–564. doi: 10.1007/s11999-009-1138-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matsuda DK, Carlisle JC, Arthurs SC, Wierks CH, Philippon MJ. Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy. 2011;27:252–269. doi: 10.1016/j.arthro.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 11.Bedi A, Chen N, Robertson W, Kelly BT. The management of labral tears and femoroacetabular impingement of the hip in the young, active patient. Arthroscopy. 2008;24:1135–1145. doi: 10.1016/j.arthro.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 12.Hetsroni I, Larson CM, Dela Torre K, et al. Anterior inferior iliac spine deformity as an extra-articular source for hip impingement: a series of 10 patients treated with arthroscopic decompression. Arthroscopy. 2012;28:1644–1653. doi: 10.1016/j.arthro.2012.05.882. [DOI] [PubMed] [Google Scholar]
- 13.Hetsroni I, Poultsides L, Bedi A, Larson CM, Kelly BT. Anterior Inferior Iliac Spine Morphology Correlates With Hip Range of Motion: A Classification System and Dynamic Model. Clin Orthop Relat Res. 2013. doi:10.1007/s11999-013-2847-4. [DOI] [PMC free article] [PubMed]
- 14.Larson CM, Kelly BT, Stone RM. Making a case for anterior inferior iliac spine/subspine hip impingement: three representative case reports and proposed concepts. Arthroscopy. 2011;27:1732–1737. doi: 10.1016/j.arthro.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 15.Macnicol MF, Makris D. Distal transfer of the greater trochanter. J Bone Joint Surg Br. 1991;73:838–841. doi: 10.1302/0301-620X.73B5.1894678. [DOI] [PubMed] [Google Scholar]
- 16.Leunig M, Ganz R. Relative neck lengthening and intracapital osteotomy for severe Perthes and Perthes-like deformities. Bull NYU Hosp Jt Dis. 2011;69(Suppl 1):S62–S67. [PubMed] [Google Scholar]
- 17.Siebenrock KA, Steppacher SD, Haefeli PC, Schwab JM, Tannast M. Valgus Hip With High Antetorsion Causes Pain Through Posterior Extraarticular FAI. Clin Orthop Relat Res. 2013. doi:10.1007/s11999-013-2895-9. [DOI] [PMC free article] [PubMed]
- 18.Taneja AK, Bredella MA, Torriani M. Ischiofemoral impingement. Magn Reson Imaging Clin N Am. 2013;21:65–73. doi: 10.1016/j.mric.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 19.Stafford GH, Villar RN. Ischiofemoral impingement. J Bone Joint Surg Br. 2011;93:1300–1302. doi: 10.1302/0301-620X.93B10.26714. [DOI] [PubMed] [Google Scholar]
- 20.Buller LT, Rosneck J, Monaco FM, et al. Relationship between proximal femoral and acetabular alignment in normal hip joints using 3-dimensional computed tomography. Am J Sports Med. 2012;40:367–375. doi: 10.1177/0363546511424390. [DOI] [PubMed] [Google Scholar]
- 21.Fabricant PD, Bedi A, De La Torre K, Kelly BT. Clinical outcomes after arthroscopic psoas lengthening: the effect of femoral version. Arthroscopy. 2012;28:965–971. doi: 10.1016/j.arthro.2011.11.028. [DOI] [PubMed] [Google Scholar]
- 22.Steppacher SD, Albers CE, Siebenrock KA, Tannast M, Ganz R. Femoroacetabular impingement predisposes to traumatic posterior hip dislocation. Clin Orthop Relat Res. 2013;471(6):1937-43. doi:10.1007/s11999-013-2863-4. [DOI] [PMC free article] [PubMed]
- 23.Manner HM, Mast NH, Ganz R, Leunig M. Potential contribution of femoroacetabular impingement to recurrent traumatic hip dislocation. J Pediatr Orthop B. 2012;21:574–578. doi: 10.1097/BPB.0b013e328357bf04. [DOI] [PubMed] [Google Scholar]
- 24.Krych AJ, Thompson M, Larson CM, Byrd JW, Kelly BT. Is posterior hip instability associated with cam and pincer deformity? Clin Orthop Relat Res. 2012;470:3390–3397. doi: 10.1007/s11999-012-2468-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Duthon VB, Charbonnier C, Kolo FC, et al. Correlation of clinical and magnetic resonance imaging findings in hips of elite female ballet dancers. Arthroscopy. 2013;29:411–419. doi: 10.1016/j.arthro.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 26.Kolo FC, Charbonnier C, Pfirrmann CW, et al. Extreme hip motion in professional ballet dancers: dynamic and morphological evaluation based on magnetic resonance imaging. Skeletal Radiol. 2013;42:689–698. doi: 10.1007/s00256-012-1544-9. [DOI] [PubMed] [Google Scholar]
- 27.Ferguson SJ, Bryant JT, Ganz R, Ito K. The influence of the acetabular labrum on hip joint cartilage consolidation: a poroelastic finite element model. J Biomech. 2000;33:953–960. doi: 10.1016/S0021-9290(00)00042-7. [DOI] [PubMed] [Google Scholar]
- 28.Espinosa N, Rothenfluh DA, Beck M, et al. Treatment of femoroacetabular impingement: preliminary results of labral refixation. J Bone Joint Surg. 2006;88A:925–935. doi: 10.2106/JBJS.E.00290. [DOI] [PubMed] [Google Scholar]
- 29.Larson CM, Giveans MR. Arthroscopic debridement vs refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25:369–376. doi: 10.1016/j.arthro.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 30.Larson CM, Giveans MR, Stone RM. Arthroscopic debridement vs refixation of the acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med. 2012;40:1015–1021. doi: 10.1177/0363546511434578. [DOI] [PubMed] [Google Scholar]
- 31.Krych AJ, Thompson M, Knutson Z, Scoon J, Coleman SH. Arthroscopic labral repair vs selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy. 2013;29:46–53. doi: 10.1016/j.arthro.2012.07.011. [DOI] [PubMed] [Google Scholar]
- 32.Cadet ER, Chan AK, Vorys GC, Gardner T, Yin B. Investigation of the preservation of the fluid seal effect in the repaired, partially resected, and reconstructed acetabular labrum in a cadaveric hip model. Am J Sports Med. 2012;40:2218–2223. doi: 10.1177/0363546512457645. [DOI] [PubMed] [Google Scholar]
- 33.Philippon MJ, Briggs KK, Hay CJ, et al. Arthroscopic labral reconstruction in the hip using iliotibial band autograft: technique and early outcomes. Arthroscopy. 2010;26:750–756. doi: 10.1016/j.arthro.2009.10.016. [DOI] [PubMed] [Google Scholar]
- 34.Bedi A, Galano G, Walsh C, Kelly BT. Capsular management during hip arthroscopy: from femoroacetabular impingement to instability. Arthroscopy. 2011;27:1720–1731. doi: 10.1016/j.arthro.2011.08.288. [DOI] [PubMed] [Google Scholar]
- 35.Domb BG, Philippon MJ, Giordano BD. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: relation to a traumatic instability. Arthroscopy. 2013;29:162–173. doi: 10.1016/j.arthro.2012.04.057. [DOI] [PubMed] [Google Scholar]
- 36.Blakey CM, Field MH, Singh PJ, Tayar R, Field RE. Secondary capsular laxity of the hip. Hip Int. 2010;20:497–504. doi: 10.1177/112070001002000413. [DOI] [PubMed] [Google Scholar]
- 37.Mei-Dan O, McConkey MO, Brick M. Catastrophic failure of hip arthroscopy due to iatrogenic instability: can partial division of the ligamentum teres and iliofemoral ligament cause subluxation? Arthroscopy. 2012;28:440–445. doi: 10.1016/j.arthro.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 38.Milone MT, Bedi A, Poultsides L, et al. Novel CT-based Three-dimensional Software Improves the Characterization of Cam Morphology. Clin Orthop Relat Res. 2013. doi:10.1007/s11999-013-2809-x. [DOI] [PMC free article] [PubMed]
- 39.Zaltz I, Kelly BT, Hetsroni I, Bedi A. The Crossover Sign Overestimates Acetabular Retroversion. Clin Orthop Relat Res. 2012. doi:10.1007/s11999-012-2689-5. [DOI] [PMC free article] [PubMed]
- 40.Wassilew GI, Heller MO, Diederichs G, et al. Standardized AP radiographs do not provide reliable diagnostic measures for the assessment of acetabular retroversion. J Orthop Res. 2012;30:1369–1376. doi: 10.1002/jor.22086. [DOI] [PubMed] [Google Scholar]
- 41.Wassilew GI, Janz V, Heller MO, et al. Real time visualization of femoroacetabular impingement and subluxation using 320-slice computed tomography. J Orthop Res. 2013;31:275–281. doi: 10.1002/jor.22224. [DOI] [PubMed] [Google Scholar]


