Abstract
The purpose of this review is to determine if there is a difference in outcomes after: (1) nonsurgical vs surgical treatment of FAI; (2a) surgical dislocation with greater trochanteric osteotomy, (2b) anterior mini-open, (2c) arthroscopic plus mini-open, and (2d) arthroscopic surgery for FAI; (3) difference in complication and re-operation rates; and (4a) labral refixation and (4b) labral debridement for labral injuries. A systematic review of multiple databases was performed after PROSPERO registration and using PRISMA guidelines. Level I-IV evidence clinical studies with minimum 2-year follow-up were included. Data were compared using 2-sample and 2-proportion Z-test calculators. Study methodological quality was analyzed using Modified Coleman Methodology Score (MCMS). Recommendations were made using SORT (Strength Of Recommendation Taxonomy). Twenty-nine studies were included (2369 subjects; 2507 hips). MCMS was poor. Mean subject age was 34.4+/−8.4 years and mean follow-up was 3.1+/−0.9 years. Statistically significant differences were observed following both nonsurgical and surgical treatment, with greater (P < 0.05) improvements following surgery (SORT B), without consistent significant differences observed between different surgical techniques (SORT C). There was a greater (P < 0.05) reoperation and complication rate following surgical dislocation vs mini-open and arthroscopic techniques (SORT A). Clinical outcomes were significantly better (P < 0.05) following labral refixation vs debridement (SORT B). Outcomes of operative treatment of femoroacetabular impingement are significantly better than nonsurgical management. Surgical treatment significantly improves outcomes, with no consistent significant differences exhibited between open and arthroscopic techniques. Open surgical dislocation has significantly greater reoperation and complication rates vs mini-open and arthroscopic techniques. Outcomes of labral refixation are significantly better than debridement in patients with labral injuries.
Keywords: Hip, Femoroacetabular impingement, Arthroscopy, Surgical dislocation, Labral tear
Introduction
Femoroacetabular impingement (FAI) is a common cause of hip pain that may lead to osteoarthritis [1]. Cam and pincer FAI are 2 distinct anatomic entities that may lead to abnormal articular congruity and subsequent chondrolabral injury [1]. The acetabular labrum is an important structure involved in the normal hip articulation and is commonly injured in FAI [2•]. However, radiographic abnormalities suggestive of FAI have been demonstrated in asymptomatic patients and the natural history of the FAI hip is not completely known [3]. Significant hip-specific [4••], general health-specific [5], and quality-of-life [5] questionnaire improvements have been observed in early- and mid-term follow-up in symptomatic patients undergoing FAI hip preservation surgery. Nonetheless, it is unknown whether FAI and labral surgery has the potential to affect the incidence or progression of osteoarthritis of the hip [6].
Very little literature has been published on the nonoperative treatment of FAI [7]. Further, to date, there have not been any investigations comparing nonoperative and operative treatment. In addition, there is little data in the literature that compares outcomes of the most commonly-utilized surgical techniques in FAI. Management of the acetabular labrum (debride, repair, refixation, reconstruct) is controversial. Therefore, the purpose of this systematic review was to answer the following 4 questions:
Is there a difference in clinical outcomes after (a) nonsurgical and (b) surgical treatment of FAI?
Is there a difference in clinical outcomes after (a) surgical dislocation with greater trochanteric osteotomy; (b) anterior mini-open; (c) arthroscopic plus mini-open; and (d) arthroscopic surgery for FAI?
Is there a difference in complication and re-operation rates after (a) surgical dislocation with greater trochanteric osteotomy; (b) anterior mini-open; (c) arthroscopic plus mini-open; and (d) arthroscopic surgery for FAI?
Is there a difference in clinical outcomes after (a) labral refixation and (b) labral debridement for labral injuries in patients with FAI?
The authors hypothesize that clinical outcomes are significantly better following surgical vs nonsurgical treatment of FAI. The authors hypothesize that there is no significant clinical outcome difference between different surgical techniques for treatment of FAI. The authors hypothesize that the complication and reoperation rate is highest following surgical dislocation and mini-open techniques vs arthroscopy. The authors hypothesize that clinical outcomes are significantly better following labral refixation vs debridement.
Materials and methods
A systematic review was conducted according to PRISMA guidelines (Preferred Reporting Items for Systematic reviews and Meta-Analyses) using a PRISMA checklist [8]. Systematic review registration was performed using the PROSPERO International prospective register of systematic reviews (registration number CRD42013004001) [9]. Two reviewers independently conducted the search on March 1, 2013 using the following databases: Medline, Cochrane Central Register of Controlled Trials, SportDiscus, and CINAHL. The electronic search citation algorithm utilized was: ((((((((((((((labrum [Title/Abstract]) OR labral [Title/Abstract])) OR ((femoroacetabular [Title/Abstract]) AND impingement [Title/Abstract]))) AND hip [Title/Abstract])) NOT shoulder [Title/Abstract]) NOT subacromial [Title/Abstract]) NOT elbow [Title/Abstract]) NOT wrist [Title/Abstract]) NOT hand [Title/Abstract]) NOT knee [Title/Abstract]) NOT ankle [Title/Abstract]) NOT foot [Title/Abstract] AND (English [lang]). English language Level I–IV evidence (2011 update by the Oxford Centre for Evidence-Based Medicine [10]) clinical outcome studies with minimum 2-year follow-up were eligible. Medical conference abstracts were ineligible for inclusion. All references within included studies were cross-referenced for inclusion if missed by the initial search. Duplicate subject publications within separate unique studies were not reported twice. The study with longer duration follow-up, greater number of subjects, or more explicit reporting of rehabilitation was retained for inclusion. Level V evidence reviews, letters to the editor, basic science, biomechanical studies, open hip surgery, imaging, surgical technique, and classification studies were excluded. Inclusive studies necessarily reported post-operative rehabilitation protocols. Qualitative and quantitative reporting of specific rehabilitation parameters was analyzed. Those studies that otherwise would have been eligible for inclusion and analysis (eg, 2 years clinical follow-up after hip arthroscopy) that failed to include any post-operative rehabilitation protocol were excluded.
Participants/subjects/patients of interest in this systematic review were enrolled in a clinical trial with a minimum of 2-years follow-up following nonoperative or operative treatment (intervention) of FAI. Specific surgical techniques of interest were intra-articular procedures including arthroscopic, mini-open, arthroscopic plus mini-open, or open greater trochanteric osteotomy-based surgical dislocation with femoral osteochondroplasty, pincer acetabuloplasty, labral debridement, or refixation/repair, loose body removal, articular cartilage surgery, capsular repair/plication or release, iliopsoas release, and ligamentum teres debridement. Study and subject demographic parameters analyzed included year of publication, years of subject enrollment, presence of study financial conflict of interest, number of subjects and hips, gender, age, body mass index (BMI), diagnoses treated, and surgical procedures performed. Clinical outcome scores sought were the NAHS (nonarthritic hip score), iHOT-12 or 33 (international Hip Outcome Tool - 12 or 33), HOS (Hip Outcome Score - ADL [activities of daily living] and Sports), mHHS (modified Harris Hip Score), HOOS (Hip disability and Osteoarthritis Outcome Score), SF-12 (Short-Form), UCLA activity score, Tegner activity score, and Merle d'Aubigne Postel score. Radiographs and MRI data were extracted when available. Study methodological quality was evaluated using the MCMS (Modified Coleman Methodology Score) [11].
Femoroacetabular cam, pincer, and "mixed" impingement were defined variably across all studies (Table 1), mostly using a combination of radiographic criteria and a coincident physical exam. Radiographic parameters assessed were: alpha angle (via radiograph or MRI), lateral and anterior center edge angle, crossover sign, posterior wall sign, ischial spine sign, and acetabular index. The Tonnis classification (Grade 0 [no signs of osteoarthritis], Grade I [increased sclerosis, slight joint space narrowing, no or slight loss of head sphericity], Grade II [small cysts, moderate joint space narrowing, moderate loss of head sphericity], and Grade III [large cysts, severe joint space narrowing, severe head deformity]) was utilized for classification of degenerative changes of the hip [12].
Table 1.
Heterogeneity in defining cam and pincer femoroacetabular impingement across all studies analyzed. In addition, there was heterogeneity in defining acetabular retroversion, focal anterior acetabular overcoverage, coxa profunda, acetabular protrusio, and loss of sphericity of femoral head. MRI (magnetic resonance imaging)
| Cam | Pincer |
|---|---|
| • Alpha angle on radiographs (or MRI) | • Relative acetabular retroversion |
| ○ Greater than 40° on oblique radiograph | ○ Cross-over sign |
| ○ Greater than 50° on lateral radiograph | ○ Prominent ischial spine sign |
| ○ Greater than 50° on MR arthrogram | ○ Positive posterior wall sign |
| ○ Greater than 55° on oblique radiograph | ○ Lateral center edge angle greater than 25° |
| ○ Greater than 55° on cross-table lateral radiograph | • Focal anterior overcoverage |
| ○ Loss of sphericity of femoral head | ○ Cross-over sign |
| ▪ Extension of lateral epiphysis onto cephalad neck | ○ Negative posterior wall sign |
| ▪ Pistol grip deformity with extension of lateral epiphysis down to base of femoral neck | ○ Lateral center edge angle greater than 25° |
| ○ Reduction in head-neck offset | • Coxa profunda |
| ○ Bump, herniation pit, and abnormal alpha angle | ○ Tear drop (floor of fossa) medial to ilioischial line |
| ○ Lateral center edge angle greater than 35° | |
| • Acetabular protrusio | |
| ○ Medial aspect of femoral head medial to ilioischial line | |
| ○ Lateral center edge angle greater than 40° | |
| • Pincer divot at femoral head-neck junction |
Statistical analysis
Study descriptive statistics were calculated. Continuous variable data were reported as mean ± standard deviation from the mean. Weighted means and standard deviations were calculated for all subject, hip, and surgical parameters. Categorical variable data was reported as frequency with percentages. For all statistical analysis either measured and calculated from study data extraction or directly reported from the individual studies, P < 0.05 was considered statistically significant. Study, subject, and surgical outcomes data were compared using 2-sample and 2-proportion Z-test calculators with alpha 0.05 because of the difference in sample sizes between compared groups.
Results
Twenty-nine studies (Fig. 1), mostly level IV evidence (83 %), were included for analysis in the systematic review [2•, 4••, 5, 7, 13–18, 19•, 20–37] (Table 2). Fifty-nine percent of studies (17 out of 29) denied the presence of any financial conflict of interest, while 14 % (4 studies) failed to report either the presence or absence of a financial conflict. Most studies (72 %) were single-center investigations from the United States of America (52 %), Switzerland (21 %), or the United Kingdom (10 %). Mean MCMS was 37.4 ± 8.2 (poor rating). The 3 highest scoring MCMS items were: (1) length of follow-up, (2) description of treatment, and (3) description of inclusion criteria. The 5 lowest scoring MCMS items were: (1) blinding, (2) randomization, (3) power analysis, (4) clinical effect size measurement, and (5) number needed to treat analysis. There were 2369 subjects analyzed with more males (60 %) than females, mean age 34.4 ± 8.4 years, normal mean BMI (24.5 ± 2.6 kg/m2). Patients were, on average, symptomatic for over 2 years prior to treatment initiation (25.6 ± 15.1 months) with a mean follow-up of 3.09 ± 0.9 years.
Fig. 1.
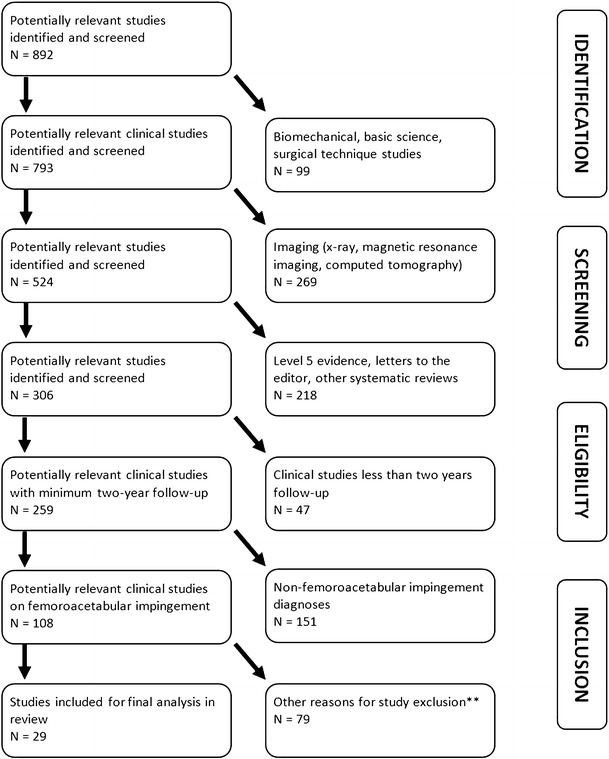
PRISMA flowchart. **Other reasons for study exclusion: duplicate study populations (8), physical exam studies (18), periacetabular osteotomy studies (12), outcome score validation studies (8), surveys (1), revision surgery (9), rehabilitation studies (7), hip trauma (13), and no clinical outcomes reported (1)
Table 2.
Demographic variables of included studies, subjects, and hips
| Parameter | Value (%) |
|---|---|
| Number of studies | 29 |
| Financial conflict of interest | |
| Private present | 8 |
| Public present | 1 a |
| Absent | 17 |
| Not reported | 4 |
| Levels of evidence (number of studies) | 3.76 ± 0.64 |
| I | 1 (3.4%) |
| II | 0 (0%) |
| III | 4 (14%) |
| IV | 24 (83%) |
| Number of centers (number of studies) | |
| Single-center | 21 (72%) |
| Multi-center | 8 (28%) |
| Country of publication (number of studies) | |
| United States of America | 15 |
| Switzerland | 6 |
| United Kingdom | 3 |
| Others | 7 b |
| Mean modified Coleman Methodology Score | 37.4 ± 8.16 |
| Number of subjects | 2369 |
| Males | 1415 (60%) |
| Females | 954 (40%) |
| Mean age | 34.4 ± 8.4 y |
| Mean body mass index | 24.5 ± 2.6 kg/m2 |
| Mean duration of pre-operative symptoms | 25.6 ± 15.1 mo |
| Mean length of follow-up | 3.09 ± 0.88 y |
| Number of studies with independent observer at follow-up | 6 (21%; 497 subjects, 21% of subjects) |
| Number of studies utilizing patient satisfaction questionnaire | 7 (24%) |
| Number of hips | 2507 |
| Right | 362 (58%) |
| Left | 257 (42%) c |
| Surgical treatment | 2470 |
| Nonsurgical treatment | 37 |
a One study reported both a private and public source of financial conflict of interest.
b Australia, New Zealand, South Korea, Mexico, France, Canada, Egypt.
c Right- vs left-sidedness reported in only 619 hips.
Prior to commencing treatment, there was no significant difference (P > 0.05) for comparison of all groups with regard to mean level of evidence, subject age, or mean MCMS (Table 3). However, there were significantly fewer subjects undergoing mini-open (11 % of all hips) and arthroscopy plus mini-open (6.1 %) techniques vs surgical dislocation (24 %) and arthroscopic (59 %) techniques. Further, there were significantly more males in the mini-open group vs arthroscopic (P = 0.008; Z = 2.6) and surgical dislocation groups (P = 0.03; Z = 2.2). In addition, length of clinical follow-up was shorter in the mini-open vs arthroscopic (P = 0.01; Z = 2.5), surgical dislocation (P > 0.001; Z = 3.8), and arthroscopic plus mini-open (P > 0.001; Z = 3.7) groups. Similarly, length of follow-up was shorter in the arthroscopic vs surgical dislocation (p = 0.02; Z = 2.4) and arthroscopic plus mini-open (P = 0.01; Z = 2.5) groups.
Table 3.
Comparison of all groups analyzed in this review
| Arthroscopic | Mini-open | Surgical dislocation | Arthroscopy + mini-open | Nonoperative treatment | |
|---|---|---|---|---|---|
| Number of studies | 12 | 2 | 11 | 3 | 1 |
| Number of patients | 1405 | 255 | 526 | 146 | 37 |
| Number of hips | 1448 b | 274 | 597 | 151 b | 37 |
| Level of evidence | 3.58 ± 0.72 | 3.50 ± 0.70 | 3.91 ± 0.78 | 4 ± 0.80 | 4 |
| Age (y) | 37.2 ± 12.1 | 35.3 ±1.41 | 35.4 ± 5.31 | 35.1 ± 1.93 | 33 ± 5 |
| Length of clinical follow-up (years) | 3.00 ± 0.58 | 2.26 ± 0.07 | 3.54 ± 1.05 | 3.97 ± 1.62 | 2.21 ± 1.5 |
| MCMS | 40.8 ± 9.54 | 35.5 ± 3.54 | 34.5 ± 7.55 | 35.7 ± 4.16 | 39 |
| Diagnosis | |||||
| Isolated cam FAI | 915 | 69 | 200 | 45 | 28 |
| Isolated pincer FAI | 187 | 0 | 56 | 0 | 0 |
| Mixed FAI | 346 | 49 | 341 | 6 | 37 |
| Labral injury | 1388 | nr a | 498 | 139 a | nr |
| Procedures | |||||
| Femoral cam osteochondroplasty | 1335 | 274 | 581 | 51 | n/a |
| Acetabular pincer rim trimming | 536 | nr | 221 | nr | n/a |
| Labral debridement | 1014 | 90 | 236 | 98 | n/a |
| Labral repair / refixation | 309 | 184 | 226 | 40 | n/a |
| Ligamentum teres debridement | 46 | 0 | 0 | 0 | n/a |
| Iliopsoas release | 23 | 0 | 0 | 0 | n/a |
| Microfracture (acetabulum) | 112 | 0 | 67 | 3 | n/a |
MCMS Modified Coleman Methodology Score, n/a not applicable.
a Number of patients/hips with FAI or labral injuries (nr not reported) in both studies.
b 44 % arthroscopies performed in supine position (711 hips), 56 % performed in lateral decubitus position (888 hips).
There was a large number of different clinical outcome tools utilized following treatment: NAHS, HOS (ADL), HOS (Sports), mHHS, VAS, WOMAC overall (and sub-scores pain, stiffness, and function), UCLA activity score, Tegner activity score, SF-12 (PCS and MCS), and Merle d'Aubigne Postel score. No study utilized the HOOS, iHOT-33, or iHOT-12. Various radiographic variables were assessed: Tonnis radiographic arthritis grading, alpha angle, lateral and anterior CEA, crossover sign, posterior wall sign, ischial spine sign, and acetabular index.
Nonoperative vs operative treatment
Pre-treatment, patients undergoing nonoperative treatment had significantly higher NAHS than those undergoing arthroscopy (P > 0.001; Z = 22.3), mini-open (P > 0.001; Z = 19.9), and arthroscopic plus mini-open (P > 0.001; Z = 8.5) (Table 4). At final follow-up, the amount of improvement in NAHS was significantly less in those undergoing nonoperative treatment vs arthroscopy (P > 0.001; Z = 4.6), mini-open (P > 0.001; Z = 16.4), and arthroscopic plus mini-open (P > 0.001; Z = 5.8) (Table 5).
Table 4.
Weighted means at each stage of treatment
| Pre-treatment | 1 y | 2 y | 3 y | 4 y | 5 y | |
|---|---|---|---|---|---|---|
| Arthroscopy | NAHS (346): 56.9 ± 2.7 | NAHS (145): 82.6 ± 3.7 | NAHS (201): 78.2 ± 15.8 | * | ||
| HOS ADL (36): 64.2 ± 5.7 | HOS ADL (36): 86.1 ± 7.3 | |||||
| HOS Sp (148): 52.4 ± 18.8 | HOS Sp (36): 82.5 ± 8.8 | HOS Sp (47): 91.4 ± 14 | HOS Sp (65): 82 | |||
| mHHS (475): 63.4 ± 4.6 | mHHS (381): 87.1 ± 5.7 | mHHS (159): 90.2 ± 0.99 | ||||
| Mini-open | NAHS (118): 58.9 | * | NAHS (118): 91.4 | * | * | * |
| mHHS (274): 60.3 ± 3.3 | mHHS (274): 88.7 ± 5.2 | |||||
| Surgical dislocation | NAHS: n/a | * | mHHS (111): 91.3 ± 1.4 | * | * | * |
| mHHS (111): 68.2 ± 6.4 | ||||||
| Arthroscopy + mini-open | NAHS (135): 60.1 ± 14.4 | * | NAHS (35): 90.9 ± 10.7 | * | * | NAHS (100): 83.9 ± 16 |
| mHHS (51): 63.8 ± 0.0 | mHHS (51): 83.9 ± 8.0 | |||||
| Nonoperative treatment | NAHS (37): 72 ± 4 | NAHS (37): 91 ± 5 | NAHS (37): 91 ± 5 | * | * | * |
| mHHS (37): 72 ± 6 | mHHS (37): 92 ± 4 | mHHS (37): 91 ± 4 |
Table 5.
Weighted means of amount of change from pre-treatment to final follow-up
| Amount of change from pre-treatment to final follow-up | Length of follow-up (y) | |
|---|---|---|
| Arthroscopic | NAHS: 23.1 ± 6.4 | 3.2 |
| HOS ADL: 21.9 ± 6.4 | 2 | |
| HOS Sp: 32.7 ± 16.8 | 2.2 | |
| mHHS: 25.5 ± 5.4 | 2.3 | |
| Mini-open | NAHS: 32.5 | 2.2 |
| mHHS: 28.4 ± 1.8 | 2 | |
| Surgical dislocation | NAHS: n/a | n/a |
| mHHS: 23.1 ± 4.9 | 2 | |
| Arthroscopy + mini-open | NAHS: 25.7 ± 9.4 | 4.2 |
| mHHS: 20.1 ± 8.0 | 2 | |
| Nonoperative treatment | NAHS: 19 ± 4.5 | 2 |
| mHHS: 19 ± 4.5 | 2 |
n/a not applicable
Pre-treatment, patients undergoing nonoperative treatment had significantly higher mHHS than those undergoing arthroscopy (P > 0.001; Z = 8.5), mini-open (P > 0.001; Z = 11.6), surgical dislocation (P = 0.001; Z = 3.3), and arthroscopic plus mini-open (P > 0.001; Z = 8.3) (Table 4). At final follow-up, the amount of improvement in mHHS was significantly less in those undergoing nonoperative treatment vs arthroscopy (P > 0.001; Z = 8.2), mini-open (P > 0.001; Z = 12.6), and surgical dislocation (P < 0.001; Z = 4.7) (Table 5). There was no difference (P = 0.4; Z = 0.8) in mHHS improvement between nonoperative and arthroscopic plus mini-open treatment.
Range-of-motion measurement was performed in 6 studies (1 nonoperative, 5 operative). Following nonoperative treatment, flexion decreased 7° and internal rotation increased 0.6° at 2-years post-treatment. Flexion and internal rotation increased 10.3° and 11.8°, respectively (arthroscopy; 2 studies). Flexion and internal rotation increased 10° and 18.9°, respectively (mini-open; 1 study). Flexion and internal rotation increased 12° and 3°, respectively (surgical dislocation; 1 study). Flexion and internal rotation increased 15.9° and 5.2°, respectively (arthroscopy plus mini-open; 1 study).
Clinical outcomes of surgical treatment
Pre-operatively, patients undergoing arthroscopic plus mini-open surgery had significantly higher NAHS than those undergoing arthroscopy (P = 0.01; Z = 2.6), but not different from those undergoing mini-open (P = 0.3; Z = 0.97) (Table 4). At 2 years following surgery, patients undergoing mini-open and arthroscopic plus mini-open had significantly higher NAHS those undergoing arthroscopy (P < 0.001; Z = 28.6 and P < 0.001; Z = 4.5, respectively). However, there was no significant difference in NAHS at 2 years post-operatively between those undergoing mini-open and arthroscopic plus mini-open (P = 0.78; Z = 0.28). At final follow-up, the amount of improvement in NAHS was significantly greater in those undergoing mini-open treatment vs arthroscopy (p < 0.001; Z = 27.3) and arthroscopic plus mini-open (P < 0.001; Z = 8.4) (Table 5). In addition, the degree of improvement in NAHS was significantly greater in those undergoing arthroscopic plus mini-open vs arthroscopy (P = 0.003; Z = 3.0).
Prior to surgery, patients undergoing surgical dislocation had significantly higher mHHS than those undergoing arthroscopy (P < 0.001; Z = 7.5), mini-open (P < 0.001; Z = 12.4), and arthroscopic plus mini-open (P < 0.001; Z = 7.2) (Table 4). At 2 years following surgery, patients undergoing surgical dislocation had significantly higher mHHS than those undergoing arthroscopy (P < 0.001; Z = 13.1), mini-open (P < 0.001; Z = 7.6), and arthroscopic plus mini-open (P < 0.001; Z = 6.6). Similarly, patients undergoing mini-open had significantly higher mHHS than those undergoing arthroscopy (P < 0.001; Z = 3.7) and arthroscopic plus mini-open (P < 0.001; Z = 4.1). Patients undergoing arthroscopy had significantly greater mHHS than those undergoing arthroscopic plus mini-open (P = 0.006; Z = 2.8). At final follow-up, the amount of improvement in mHHS was significantly greater in those undergoing mini-open treatment vs arthroscopy (P < 0.001; Z = 10.7), surgical dislocation (P < 0.001; Z = 11.1), and arthroscopic plus mini-open (P < 0.001; Z = 7.4) (Table 5). Similarly, the amount of improvement in mHHS was significantly greater in those undergoing arthroscopy vs surgical dislocation (P < 0.001; Z = 4.6) and arthroscopy plus mini-open (P < 0.001; Z = 4.7). Patients undergoing surgical dislocation had significantly greater mHHS improvement than those undergoing arthroscopy plus mini-open (P = 0.01; Z = 2.5).
Labral repair vs labral debridement
Fourteen studies (1847 subjects) performed both labral repair and debridement in the investigation. However, 6 studies failed to compare the 2 groups. Thus, 8 studies (753 subjects) compared these 2 groups (Table 6). Four studies demonstrated significantly (P < 0.05) better clinical outcomes (HOS ADL, HOS Sports, mHHS [2 separate studies], SF-12, VAS pain, patient satisfaction, and Merle d'Aubigne) at 2 to 3.5 years following labral repair vs debridement. However, 4 other studies demonstrated no difference (P > 0.05) in clinical outcomes (mHHS [2 separate studies] and NAHS [2 separate studies]) at 2.2 to 4.9 years following labral repair or debridement.
Table 6.
Comparison of outcomes of labral refixation vs labral debridement
| Study | Participants | Intervention | Follow-up (yrs) | Outcomes |
|---|---|---|---|---|
| Krych, et al. 2013 | Females Pincer or mixed FAI | Arthroscopy | 2.7 | • Significant (P < .05) improvements in both groups (HOS ADL and HOS Sp) |
| • Significantly better (P < .05) HOS ADL, HOS Sp, and satisfaction in repair group | ||||
| Malviya, et al. 2012 | Cam, pincer, mixed FAI | Arthroscopy | 3.2 | • No significant difference in mHHS (translated via Rosser Index Matrix to quality of life score) between labral repair and debridement groups |
| Philippon, et al. 2012 | Cam, pincer, mixed FAI | Arthroscopy | 3 | • Significant (P < .05) improvements in HOS ADL, and mHHS |
| • No difference (P > .05) in mHHS between labral repair and debridement | ||||
| Larson, et al. 2012 | Pincer, mixed FAI | Arthroscopy | 3.5 | • Significant (P < .05) improvements in both groups (mHHS, SF-12, VAS pain) |
| • Significantly (P > .05) better mHHS, SF-12, and VAS in refixation group | ||||
| • 92 % good/excellent results in refixation group; 68 % good/excellent results in debride group | ||||
| Schilders, et al. 2011 | Cam, pincer, mixed FAI | Arthroscopy | 2.4 | • Significant (P < .05) improvements in both groups (mHHS) |
| • Significantly (P < .05) better mHHS in refixation group | ||||
| Chiron, et al. 2012 | Cam, mixed FAI | Mini-open | 2.2 | • Significant (P < .05) improvements in both groups (NAHS) |
| • No difference (P > .05) in NAHS between labral repair and debridement | ||||
| Espinosa, et al. 2006 | Mixed FAI | Surgical dislocation | 2 | • Significant (P < .05) improvements in both groups(Merle d'Aubigne Postel score) |
| • Significantly (P < .05) better improvements in labral repair group at 1 and 2 yrs follow-up | ||||
| • Significantly (P < .05) greater radiographic osteoarthritis (Tonnis system) in debridement group (1 and 2 yrs) | ||||
| Laude, et al. 2009 | FAI | Arthroscopy plus mini-open | 4.9 | • Significant (P < .05) improvements in both groups (NAHS) |
| • No difference (P > .05) in NAHS between labral refixation and debridement |
ADL activities of daily living, FAI femoroacetabular impingement, HOS Hip Outcome Score, mHHS modified Harris Hip Score, NAHS nonarthritic hip score, RCT randomized controlled trial, Sp sports.
Radiographic outcomes
Prior to commencing treatment, there were 1329 hips with a radiographic evaluation for osteoarthritis (Tonnis grade). Eighty-nine percent (1182 hips) were Tonnis grade 0 or 1; 11 % (143 hips) were Tonnis grade 2, and 0.3 % (4 hips) were Tonnis grade 3. Pre-operatively, the proportion of hips with Tonnis grade 0 or 1 was significantly greater in those undergoing arthroscopy plus mini-open vs mini-open (P < 0.001; Z = 4.2) and surgical dislocation (P = 0.006; Z = 2.8). Pre-operatively, the proportion of hips with Tonnis grade 0 or 1 was significantly greater in those undergoing arthroscopy vs mini-open (P < 0.001; Z = 5.1) and surgical dislocation (P = 0.005; Z = 2.8). There was no difference in Tonnis grading between arthroscopic plus mini-open and arthroscopic treatments. There was insufficient post-operative data to determine any change in Tonnis grade following treatment.
Measurement and comparison of pre- and post-operative alpha angles were performed on AP, "oblique", cross-table lateral, false-profile lateral, Dunn lateral, and frog-leg lateral radiographs and also on MRI axial series parallel to femoral neck. Change in alpha angle on AP views was 18.1° and 22.8° on lateral views; and 23.9° on MRI with series parallel to the femoral neck. There was insufficient post-operative data to make valid comparison between different surgical techniques on change in alpha angle using similar imaging techniques.
Re-operations and complications
There were 361 overall re-operations (349 unplanned, 12 planned for removal of hardware) (14.4 % rate of reoperation; 361/2507 hips) (Table 7). One-hundred and ninety hardware removals were performed following surgical dislocation (178 were unplanned and performed for pain; 12 were planned). There were 78 total hip arthroplasty performed (3.1 % rate of conversion to total hip arthroplasty; 78/2507 hips). There were significantly more re-operations following surgical dislocation vs arthroscopy (P < 0.001; Z = 22.6), mini-open (P < 0.001; Z = 9.3), and arthroscopic plus mini-open (P < 0.001; Z = 5.0). There were significantly more re-operations following arthroscopic plus mini-open vs arthroscopy (P < 0.001; Z = 9.1) and mini-open (P = 0.007; Z = 2.7). There were significantly more re-operations following mini-open vs arthroscopy (P < 0.001; Z = 5.3). Other re-operations performed include: repeat arthroscopy for pain/diagnosis with lists of adhesions and debridement (39), repeat femoral osteochondroplasties (15 [11 after open surgical dislocation or mini-open, 4 after arthroscopy]), iliotibial band release (8), hip resurfacing (4), hematoma evacuation (4), incision and drainage for deep infection (2), open capsulectomy (1), suture granuloma excision (1), neuroma excision (1), and 18 reoperations not otherwise specified.
Table 7.
Reoperations and complications following treatment
| Number of re-operations (% of total subjects) | Number of unplanned re-operations (% of total subjects) | Number of total hip arthroplasties (% of total subjects) | Temporary nerve palsy | Infection | Skin damage | Thromboembolic disease | Heterotopic ossification (Brooker grade) | |
|---|---|---|---|---|---|---|---|---|
| Arthroscopic | 43 (3.0 %) | 43 (3.0 %) | 23 (1.6 %) | 10 LFCN | 1 superficial | 1 minor scrotum | 1 SVT | 1: 4 |
| 10 pudendal | 1 minor labia | 2: 0 | ||||||
| 2 partial sciatic | 3: 1 | |||||||
| 2 "foot paresthesias" | ||||||||
| 1 SVT | 1: 67 | |||||||
| Surgical dislocation | 247 (41.4 %) | 235 (39.4 %) | 21 (3.5 %) | 1 partial sciatic | 1 superficial | 0 | 1 DVT | 2: 19 |
| 1 nonfatal PE | 3: 4 | |||||||
| 4: 1 | ||||||||
| Mini-open | 27 (9.9 %) | 27 (9.9 %) | 15 (5.5 %) | 1 LFCN | 0 | 0 | 0 | 1: 24 |
| 2: 8 | ||||||||
| 3: 4 | ||||||||
| Arthroscopic plus mini-open | 29 (19.2 %) | 29 (19.2 %) | 10 (6.6 %) | 6 LFCN | 1 superficial | 0 | 1 DVT | 1: 4 |
| 1 pudendal | 2 deep | 2: 1 | ||||||
| 3: 0 | ||||||||
| Nonoperative | 4 (10.8 %) | 4 (10.8 %) | 0 (0 %) | 0 | 0 | 0 | 0 | 0 |
LFCN Lateral femoral cutaneous nerve.
If exclude removal of hardware from surgical dislocation group (190 cases), the number of unplanned reoperations in that cohort is 57 (9.6 %)
There were significantly more conversions to total hip arthroplasty after surgical dislocation vs arthroscopy (P = 0.007; Z = 2.7). There were significantly more conversions to total hip arthroplasty after arthroscopic plus mini-open vs arthroscopy (P < 0.001; Z = 4.1). There were significantly more conversions to total hip arthroplasty after mini-open vs arthroscopy (P < 0.001; Z = 4.0). All other comparisons within these groups regarding conversion to total hip arthroplasty were not significant (P < 0.05).
Following surgery, complications were infrequent (Table 7). Temporary nerve palsy was most common after arthroscopic plus mini-open (4.6 %), followed by arthroscopy (1.7 %), and surgical dislocation and mini-open (less than 1 % for both). Heterotopic ossification was most common after surgical dislocation (15 %), followed by mini-open (13 %), arthroscopy plus mini-open (3.3 %), and arthroscopy (less than 1 %). Major complications such as femoral neck fracture (1 subtrochanteric fracture after mini-open; 1 neck fracture after arthroscopic plus mini-open), hip dislocation (none), pulmonary embolus (1 after surgical dislocation), intra-abdominal or intra-thoracic fluid extravasation (none), and death (none) were rare.
Discussion
The purposes of this systematic review were to determine and compare outcomes following treatment of femoroacetabular impingement and hip labral tears. The authors hypothesized that surgical treatment was significantly better than nonoperative treatment. This hypothesis was confirmed (SORT Taxonomy grade B) (Table 8). The authors hypothesized that there was no difference in clinical outcomes between different surgical techniques for FAI. This hypothesis was not confirmed (SORT Taxonomy grade C): due to heterogeneity across surgical groups, inconsistent outcome measures, and outcomes were observed. Nonetheless, all surgical treatments resulted in statistically significant and clinically relevant improvements in outcomes. The authors hypothesized that re-operations and complications would be higher following surgical dislocation and mini-open techniques vs arthroscopic techniques. This hypothesis was confirmed (SORT Taxonomy grade A). The authors hypothesized that labral refixation/repair would have significantly better outcomes than labral debridement. This hypothesis was confirmed (SORT Taxonomy grade B).
Table 8.
Strength of recommendation definition: (A) Recommendation based on consistent and good-quality patient-oriented evidence. (B) Recommendation based on inconsistent or limited-quality patient-oriented evidence. (C) Recommendation based on consensus, usual practice, opinion, disease-oriented evidence, or case series for studies of diagnosis, treatment, prevention, or screening
| Question | SORT Grade | Recommendation |
|---|---|---|
| Clinical outcome difference between nonoperative and operative treatment of FAI? | B | • Based on limited quantity, limited quality, consistent evidence, clinical outcomes are better following surgical treatment vs nonoperative treatment |
| Clinical outcome difference between 4 most common surgical techniques used in FAI? | C | • Based on good quantity, limited quality, inconsistent evidence, clinical outcomes demonstrated statistically significant, and clinically relevant improvements with all 4 surgical techniques, with no consistent differences exhibited between groups |
| Difference in reoperations and complications between 4 most common surgical techniques used in FAI? | A | • Based on good quantity, good quality, consistent evidence, reoperation rate, and complication rate was highest following surgical dislocation, and lowest with arthroscopy |
| Clinical outcomes difference after labral refixation vs debridement for patients with labral injuries in FAI? | B | • Based on good quantity, limited quality, inconsistent evidence, clinical outcomes are better following labral refixation vs labral debridement |
Measurement of outcomes of all fields in medicine is in a transition period from "physician/clinician-administered/-based" to "patient-reported/-based". These patient-reported outcomes are becoming integrated into physician and hospital reimbursement and rankings. Thus, evaluations of treatment outcome require meeting patients' expectations. Most frequently, the reason patients choose surgery is for alleviating pain (33 %), followed by fear of getting worse (20 %), improved ADL's (16 %), failed nonoperative treatments (11 %), improved sports (10 %), and others (10 %) [38]. Therefore, given the fact that many asymptomatic patients have abnormal radiographs [3], the clinician must exercise judiciousness in patient selection and "treat the patient, and not the x-ray". Further, over 50 % of patients are often overly optimistic with regard to hip pain, sport, and general physical capacity [38]. In addition, significant improvements in any outcome score ("feeling better") (even if met MCID [minimal clinically important difference]) does not necessarily equate to "feeling good" [39]. Thus, a patient-acceptable symptom state (PASS) may not be met. Nevertheless, the clinician must base his/her assessment of outcome on patient-based outcome tools that have appropriate psychometric properties.
There are over 40 different questionnaires utilized to measure outcomes of hip surgery [40]. For general musculoskeletal complaints of the lower limb, the AAOS Outcomes Questionnaires (American Academy of Orthopedic Surgeons) and MFA (Musculoskeletal Functional Assessment) are both patient-reported measures that evaluate the condition of the hip and/or knee musculoskeletal problems [40]. For hip osteoarthritis, the HOOS (derived from WOMAC [Western Ontario and McMaster Universities]) is a patient-reported measure that was designed to acknowledge and evaluate the higher activity levels of patients with osteoarthritis of the hip [40]. In patients with total hip arthroplasties, the Harris Hip Score is the best tool, although it is clinician-measured and reported [40]. In younger, more active, nonarthritic patients, several tools have been recently developed to improve validity, reliability and responsiveness.
The NAHS is frequently used in the evaluation of younger patients with minimal to no radiographic degenerative changes and a symptomatic hip [41]. Although validated and reliable [41], its development was not ideal, as it arbitrarily chose the number of questions and derived several of them from the WOMAC, which was intended for older, less active patient cohorts. The HOS is, like the NAHS, a patient-reported measure designed to assess outcomes in active patients [42]. However, the HOS has an expanded age range (up to 66 years). It was originally created via evaluation of patients with hip labral tears [42]. It has 2 separate sub-scores: ADL's (activities of daily living) and Sports. It has demonstrated reliability, responsiveness, and construct validity [42–44]. The MCID for the HOS ADL and Sports scores were 9 and 6 points, respectively [43]. More recently, the iHOT (International Hip Outcome Tools) scores (iHOT-33 and iHOT-12) were developed and psychometric properties tested based on meeting of the MAHORN (Multicenter Arthroscopy of the Hip Outcomes Research Network) international group of experts [45•]. The iHOT-33 is a patient-reported health-related quality of life outcome questionnaire with demonstrated reliability, responsiveness, and validity [45•]. The iHOT-33 has an MCID of 6 points [45•]. A shorter version of the iHOT-33 was also recently developed, the iHOT-12, with retention of reliability, responsiveness, and validity [46]. The authors of iHOT scores recommend iHOT-12 for routine clinical practice and iHOT-33 for research. The current systematic review did not identify any study that utilized the iHOT-12 or iHOT-33 and only identified 4 studies (14 %) utilizing HOS, and 7 studies (24 %) utilizing NAHS. Otherwise, all other outcome tools' psychometric properties have not been evaluated in young, active patients with symptomatic FAI.
Limitations
Limitations within a systematic review are related to the studies within which it analyzes. Selection bias was minimized in the review due to the inclusive nature of studies with levels of evidence I-IV. However, minimum 2-year follow-up may miss early differences in outcomes between analyzed groups. Performance bias was also minimal, due to the inclusion of all types of FAI, all patient demographics, all surgical techniques, and all surgical outcome tools. There was wide heterogeneity in patient demographics, surgical procedures, and outcome measures. This increases practical generalizability (increased external validity, with reduced internal validity). The heterogeneity and use of largely nonvalidated outcome measures and lack of inclusion and correlation with imaging findings introduces detection bias. Transfer bias was minimized with length of follow-up. However, given that the intent of hip preservation surgery is to slow or prevent incidence or progression to osteoarthritis, longer follow-up is certainly necessary. Study design bias is present in that over 80 % of the analyzed studies were level IV case series and only 1 analyzed investigation was a randomized controlled trial. This was further supported with the poor MCMS rating. Publication bias is present in that the authors excluded medical conference abstracts, non-English language studies, and nonpublished English language studies. Future research should continue to strive for higher levels of evidence, longer follow-up, and answer important questions. The authors recognize and support (Level V evidence) that the answers to these questions may already be known, however lack literature support at the current time to make this claim: (1) What is the difference in clinical outcomes of surgical treatment for (a) cam; (b) pincer; and (c) mixed FAI; (2) What is the difference in clinical outcomes of patients with FAI undergoing hip preservation surgery with femoral and acetabular osteochondroplasty vs without femoral and/or acetabular osteochondroplasty; (3) What is the difference in clinical outcomes of patients undergoing hip preservation surgery with complete capsular closure vs incomplete or nonclosure of the capsule; and (4) What is the role of surveillance in asymptomatic FAI.
Conclusions
Outcomes of operative treatment of femoroacetabular impingement are significantly better than nonsurgical management. Surgical treatment significantly improves outcomes, with no consistent significant differences exhibited between open and arthroscopic techniques. Open surgical dislocation has significantly greater reoperation and complication rates vs mini-open and arthroscopic techniques. Outcomes of labral refixation are significantly better than debridement in patients with labral injuries.
Compliance with Ethics Guidelines
Conflict of Interest
Shane J. Nho is a paid consultant for Stryker, Pivot, and Ossur.
Joshua D. Harris declares that he has no conflict of interest.
Brandon J. Erickson declares that he has no conflict of interest.
Charles A. Bush-Joseph declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. [DOI] [PubMed]
- 2.Larson CM, Giveans MR, Stone RM. Arthroscopic debridement vs refixation of the acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med. 2012;40:1015–21. doi: 10.1177/0363546511434578. [DOI] [PubMed] [Google Scholar]
- 3.Hack K, Di Primio G, Rakhra K, Beaulé PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92:2436–44. doi: 10.2106/JBJS.J.01280. [DOI] [PubMed] [Google Scholar]
- 4.•• Krych AJ, Thompson M, Knutson Z, Scoon J, Coleman SH. Arthroscopic labral repair vs selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy. 2013;29(1):46–53. Level I evidence randomized controlled trial with 2.6 year follow-up that demonstrated significantly better outcomes in female patients with FAI and labral tears that underwent arthroscopic labral repair vs debridement. [DOI] [PubMed]
- 5.Malviya A, Stafford GH, Villar RN. Impact of arthroscopy of the hip for femoroacetabular impingement on quality of life at a mean follow-up of 3.2 years. J Bone Joint Surg Br. 2012;94:466–70. doi: 10.1302/0301-620X.94B4.28023. [DOI] [PubMed] [Google Scholar]
- 6.Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res. 2004;429:170–7. doi: 10.1097/01.blo.0000150119.49983.ef. [DOI] [PubMed] [Google Scholar]
- 7.Emara K, Samir W, el Motasem H, Ghafar KA. Conservative treatment for mild femoroacetabular impingement. J Orthop Surg (Hong Kong) 2011;19:41–5. doi: 10.1177/230949901101900109. [DOI] [PubMed] [Google Scholar]
- 8.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–34. [DOI] [PubMed]
- 9.The University of York, Centre for Reviews and Dissemination. PROSPERO - International prospective register of systematic reviews. 2013 [cited 2013 March 2, 2013]. Available at: http://www.crd.york.ac.uk/PROSPERO/.
- 10.The University of Oxford, Centre for Evidence Based Medicine. OCEBM 2011 Levels of Evidence System. Oxford Centre for Evidence Based Medicine 2012 [cited 2012 December 20, 2012]. Available at: http://www.cebm.net/index.aspx?o=5653.
- 11.Cowan J, Lozano-Calderon S, Ring D. Quality of prospective controlled randomized trials. Analysis of trials of treatment for lateral epicondylitis as an example. J Bone Joint Surg Am. 2007;89:1693–9. doi: 10.2106/JBJS.F.00858. [DOI] [PubMed] [Google Scholar]
- 12.Tonnis D, Legal H, Graf R, editors. Congenital dysplasia and dislocation of the hip in children and adults. Berlin, Germany: Springer-Verlag; 1987. [Google Scholar]
- 13.Chiron P, Espie A, Reina N, Cavaignac E, Molinier F, Laffosse JM. Surgery for femoroacetabular impingement using a minimally invasive anterolateral approach: analysis of 118 cases at 2.2-year follow-up. Orthop Traumatol Surg Res. 2012;98(1):30–8. [DOI] [PubMed]
- 14.Parvizi J, Huang R, Diaz-Ledezma C, Og B. Mini-open femoroacetabular osteoplasty: how do these patients do? J Arthroplasty. 2012;27(8 Suppl):122–5:e1. doi: 10.1016/j.arth.2012.03.047. [DOI] [PubMed] [Google Scholar]
- 15.Zaltz I, Leunig M. Parafoveal chondral defects associated with femoroacetabular impingement. Clin Orthop Relat Res. 2012;470:3383–9. doi: 10.1007/s11999-012-2453-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walker JA, Pagnotto M, Trousdale RT, Sierra RJ. Preliminary pain and function after labral reconstruction during femoroacetabular impingement surgery. Clin Orthop Relat Res. 2012;470:3414–20. doi: 10.1007/s11999-012-2506-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Philippon MJ, Ejnisman L, Ellis HB, Briggs KK. Outcomes 2 to 5 years following hip arthroscopy for femoroacetabular impingement in the patient aged 11 to 16 years. Arthroscopy. 2012;28:1255–61. doi: 10.1016/j.arthro.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 18.Palmer DH, Ganesh V, Comfort T, Tatman P. Midterm outcomes in patients with cam femoroacetabular impingement treated arthroscopically. Arthroscopy. 2012;28:1671–81. doi: 10.1016/j.arthro.2012.04.154. [DOI] [PubMed] [Google Scholar]
- 19.• Naal FD, Miozzari HH, Schar M, Hesper T, Notzli HP. Midterm results of surgical hip dislocation for the treatment of femoroacetabular impingement. Am J Sports Med. 2012;40(7):1501–10. Level IV evidence case series of 185 patients with 5-year follow-up following surgical dislocation for FAI demonstrating 82% patient satisfaction and overall significantly improved clinical outcomes using WOMAC, HOS, SF-12, and UCLA scores. [DOI] [PubMed]
- 20.Schilders E, Dimitrakopoulou A, Bismil Q, Marchant P, Cooke C. Arthroscopic treatment of labral tears in femoroacetabular impingement: a comparative study of refixation and resection with a minimum two-year follow-up. J Bone Joint Surg Br. 2011;93(8):1027–32. [DOI] [PubMed]
- 21.Javed A, O'Donnell JM. Arthroscopic femoral osteochondroplasty for cam femoroacetabular impingement in patients over 60 years of age. J Bone Joint Surg Br. 2011;93:326–31. doi: 10.1302/0301-620X.93B3.25262. [DOI] [PubMed] [Google Scholar]
- 22.Byrd JW, Jones KS. Arthroscopic management of femoroacetabular impingement: minimum 2-year follow-up. Arthroscopy. 2011;27:1379–88. doi: 10.1016/j.arthro.2011.05.018. [DOI] [PubMed] [Google Scholar]
- 23.Kempthorne JT, Armour PC, Rietveld JA, Hooper GJ. Surgical dislocation of the hip and the management of femoroacetabular impingement: results of the Christchurch experience. ANZ J Surg. 2012;81:446–50. doi: 10.1111/j.1445-2197.2010.05489.x. [DOI] [PubMed] [Google Scholar]
- 24.Nho SJ, Magennis EM, Singh CK, Kelly BT. Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high-level athletes. Am J Sports Med. 2011;39 Suppl:14S–9S. [DOI] [PubMed]
- 25.Clohisy JC, Zebala LP, Nepple JJ, Pashos G. Combined hip arthroscopy and limited open osteochondroplasty for anterior femoroacetabular impingement. J Bone Joint Surg Am. 2010;92:1697–706. doi: 10.2106/JBJS.I.00326. [DOI] [PubMed] [Google Scholar]
- 26.Peters CL, Schabel K, Anderson L, Erickson J. Open treatment of femoroacetabular impingement is associated with clinical improvement and low complication rate at short-term follow-up. Clin Orthop Relat Res. 2010;468:504–10. doi: 10.1007/s11999-009-1152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Horisberger M, Brunner A, Herzog RF. Arthroscopic treatment of femoroacetabular impingement of the hip: a new technique to access the joint. Clin Orthop Relat Res. 2010;468:182–90. doi: 10.1007/s11999-009-1005-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Philippon MJ, Weiss DR, Kuppersmith DA, Briggs KK, Hay CJ. Arthroscopic labral repair and treatment of femoroacetabular impingement in professional hockey players. Am J Sports Med. 2010;38(1):99–104. [DOI] [PubMed]
- 29.Laude F, Sariali E, Nogier A. Femoroacetabular impingement treatment using arthroscopy and anterior approach. Clin Orthop Relat Res. 2009;467:747–52. doi: 10.1007/s11999-008-0656-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Graves ML, Mast JW. Femoroacetabular impingement: do outcomes reliably improve with surgical dislocations? Clin Orthop Relat Res. 2009;467:717–23. doi: 10.1007/s11999-008-0648-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yun HH, Shon WY, Yun JY. Treatment of femoroacetabular impingement with surgical dislocation. Clin Orthop Surg. 2009;1:146–54. doi: 10.4055/cios.2009.1.3.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lincoln M, Johnston K, Muldoon M, Santore R. Combined arthroscopic and modified open approach for cam femoroacetabular impingement: a preliminary experience. Arthroscopy. 2009;25:392–9. doi: 10.1016/j.arthro.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 33.Ilizaliturri VM, Jr, Orozco-Rodriguez L, Acosta-Rodríguez E, Camacho-Galindo J. Arthroscopic treatment of cam-type femoroacetabular impingement: preliminary report at 2 years minimum follow-up. J Arthroplasty. 2008;23:226–34. doi: 10.1016/j.arth.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 34.Beaulé PE, Le Duff MJ, Zaragoza E. Quality of life following femoral head-neck osteochondroplasty for femoroacetabular impingement. J Bone Joint Surg Am. 2007;89:773–9. doi: 10.2106/JBJS.F.00681. [DOI] [PubMed] [Google Scholar]
- 35.Bizzini M, Notzli HP, Maffiuletti NA. Femoroacetabular impingement in professional ice hockey players: a case series of 5 athletes after open surgical decompression of the hip. Am J Sports Med. 2007;35:1955–9. doi: 10.1177/0363546507304141. [DOI] [PubMed] [Google Scholar]
- 36.Espinosa N, Rothenfluh DA, Beck M, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88(5):925–35. [DOI] [PubMed]
- 37.Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67–73. [PubMed]
- 38.Mannion AF, Impellizzeri FM, Naal FD, Leunig M. Fulfilment of patient-rated expectations predicts the outcome of surgery for femoroacetabular impingement. Osteoarthr Cartil. 2013;21:44–50. doi: 10.1016/j.joca.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 39.Impellizzeri FM, Mannion AF, Naal FD, Hersche O, Leunig M. The early outcome of surgical treatment for femoroacetabular impingement: success depends on how you measure it. Osteoarthr Cartil. 2012;20(7):638–45. [DOI] [PubMed]
- 40.Mohtadi N, Pedersen E, Chan D, et al. Assessing outcomes after hip surgery. In: Sekiya J, et al., editors. Techniques in hip arthroscopy and joint preservation surgery. Philadelphia, PA: Elsevier Saunders; 2011. pp. 74–85. [Google Scholar]
- 41.Christensen CP, Althausen PL, Mittleman MA, Lee JA, McCarthy JC. The nonarthritic hip score: reliable and validated. Clin Orthop Relat Res. 2003;406:75–83. [DOI] [PubMed]
- 42.Martin RL, Kelly BT, Philippon MJ. Evidence of validity for the hip outcome score. Arthroscopy. 2006;22:1304–11. doi: 10.1016/j.arthro.2006.07.027. [DOI] [PubMed] [Google Scholar]
- 43.Martin RL, Philippon MJ. Evidence of reliability and responsiveness for the hip outcome score. Arthroscopy. 2008;24:676–82. doi: 10.1016/j.arthro.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 44.Martin RL, Philippon MJ. Evidence of validity for the hip outcome score in hip arthroscopy. Arthroscopy. 2007;23:822–6. doi: 10.1016/j.arthro.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 45.• Mohtadi NG, Griffin DR, Pedersen ME, Chan D, Safran MR, Parsons N, et al. The development and validation of a self-administered quality-of-life outcome measure for young, active patients with symptomatic hip disease: the International Hip Outcome Tool (iHOT-33). Arthroscopy. 2012;28(5):595–605. quiz 606–10 e1. Validation study for the development of a new quality-of-life patient reported outcome measure for young, active patients with hip pathology (iHOT-33). Documented reliability, responsiveness, and face content, and construct validity. [DOI] [PubMed]
- 46.Griffin DR, Parsons N, Mohtadi NG, Safran MR. A short version of the International Hip Outcome Tool (iHOT-12) for use in routine clinical practice. Arthroscopy. 2012;28(5):611–6. quiz 616–8. [DOI] [PubMed]


