Abstract
The history and physical examination of the hip is the key component for evaluation of patients presenting with hip pain. As our understanding of the anatomy and biomechanics of the normal hip vs the pathologic hip advances, the physical examination progresses as well. As with the shoulder and knee examinations, there are critical steps that form the basis of the examination of the hip joint. This hip examination contains 21 steps, which compares well with the shoulder 20 step exam and the knee 33 step exam. Consideration should be given for the hip as comprised of 4 layers: the osseous, capsulolabral, musculotendinous, and neurovascular. The hip represents the link between the upper body and lower body, therefore the fifth layer, the kinematic chain, plays an essential role in treatment recommendations. A clinical evaluation of the hip that incorporates this multifactor thought process will lead to an accurate diagnosis in a timely manner. This paper is a description of the 21 core examinations of a standardized clinical evaluation of the hip.
Keywords: History, Symptoms, Layers, Hip physical exam, Hip clinical examination
Introduction
The history of the patient is first obtained prior to the physical examination of the hip. A complete history should consider all hip layers, including the kinematic chain. Key aspects for the consideration of treatment include patient age, the date of onset, presence or absence of trauma, and mechanisms of injury [1]. Date of onset, or duration of symptoms, can help determine treatment efficacy [2]. Absence of trauma may suggest degenerative disease or a predisposition to injury, whereas a history of trauma may indicate a treatable problem [3]. Pain characteristics along with the presence or absence of popping will aid in the determination of intra-articular vs extra-articular causes. It is also necessary to identify related symptoms of the spine, abdomen, and lower extremity, primarily referred knee pain. A history of night pain, sit pain, weakness, numbness, or paraesthesia in the lower extremity may suggest neural compression, which may occur in the lumbar spine or within the subgluteal space [4•].
In addition, the following items must documented: previous consultations; surgical interventions; past injuries; childhood or adolescent hip disease; ipsilateral knee disease; history of inflammatory arthritis; and risk factors for osteonecrosis. Factors related to the patient’s social history that can affect the blood supply to the femoral head are reviewed and family medical history is also taken into account. Clearly define any treatments to date and obtain a detailed account of current functional limitations. A history of sports and recreational activities can help determine the type of injury and also guide the treatment, considering the patient’s goals and expectations.
Quantification of hip pain, function, and severity of symptoms can be obtained by 1 or more questionnaires. The modified Harris Hip Score [5] (HHS) is the most documented and standardized functional score to date, which is a quantitative score based on pain and function. Other hip scores have been used for more specific patient populations such as; Merle d’Aubigné [6] (MDA), the Non-Arthritic Hip Score [7] (NAHS), Musculoskeletal Function Assessment [8] (MFA), Short Form 36 [9] (SF-36), and the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) [10]. The MAHORN (Multicenter Arthroscopy of the Hip Outcomes Research Network) Group has validated the International Hip Outcome Tool (iHOT-33) [11]. Developed through an international multicenter study, the iHOT-33 is a self-administered questionnaire with a target population of active adult patients with hip pathology. While the iHOT-33 was developed for research purposes, a short form (iHOT-12) [12] was also described for use in routine clinical practice. The use of a verbal analog score is also useful for the quantification of pain at rest and pain with activities.
Patient goals and realistic expectations of treatment are discussed. Patients may differ from surgeons regarding the issues they feel are important when considering treatment outcomes [13]. Communication and understanding are important for obtaining an accurate history. Presented in Table 1 are the key items for the history evaluation.
Table 1.
Key points of patient history
| Age | AVN |
| Date of onset | Previous evaluations |
| Trauma | Social history |
| Popping/locking | Family history |
| Treatment to date | Quality of life/function (HHS/IHOT) |
| Limitations | Pain (at rest/activity) |
| Associated complaints | Sport/activity |
| Goals in treatment |
The physical examination of the hip
The 21 step physical examination of the hip (Table 2) is a comprehensive assessment of 4 distinct layers: osteochondral; capsulolabral; musculotendinous; and neurovascular. A consistent hip examination is performed quickly and efficiently to find the comorbidities that coexist with complex hip pathology by assessing the hip, back, abdominal, neurovascular, and neurologic systems. Loose-fitting clothing about the waist is helpful for exposure and patient comfort. Documentation of the exam by an assistant on a standardized written form aids in accuracy and thoroughness. The use of a common language and specific technique for each examination test will eliminate multi-clinical discrepancy and improve reliability. The MAHORN (multicenter arthroscopy of the hip outcomes research network) Group outlined the common tests that form the basis of a multilayered hip evaluation [14•].
Table 2.
Twenty-one step physical examination of the hip
| Standing | 1. Gait | Pelvic tilt/rotation, stride length, stance phase, FPA |
| 2. Single Leg Stance Phase Test | Neural loop/abductor strength | |
| 3. Inspection | Leg lengths, forward bend/spine, body habitus, global laxity | |
| Seated | 4. Neurovascular/Reflex | Skin, lymphedema, sensory, DTR |
| 5. ROM | Internal and external rotation | |
| Supine | 6. Palpation | Abdomen, adductor tubercle |
| 7. ROM | Abduction, Adduction, flexion | |
| 8. Hip Flexor Contracture Test | Psoas/Hip flexor contracture | |
| 9. DIRI | FAI | |
| 10. DEXRIT | FAI, anterior inferior instability, apprehension | |
| 11. FADDIR | FAI | |
| 12. FABER | Hip vs. SI | |
| 13. Dial Test | Laxity/instability | |
| Lateral | 14. Palpation | GT facets and bursae, glutei origin/insertion |
| 15. Strength | Abduction, gluteus medius, gluteus maximus | |
| 16. Passive Adduction Tests | Tensor fascia lata, gluteus medius, gluteus maximus | |
| 17. Lateral Rim Impingement Test | FAI, laxity, apprehension | |
| 18. Posterior Rim Impingement Test | FAI, apprehension, contre-coup | |
| 19. Apprehension Test | Laxity, contre-coup | |
| Prone | 20. Rectus Femoris Contracture Test | Rectus femoris contracture |
| 21. Femoral Version Test | Femoral anteversion |
Standardization enhances the physical examination reliability [15] and the most efficient order of examination begins with standing tests followed by seated, supine, lateral tests, and ending with prone tests [16].
Standing examination
A general location of pain is noted by the patient pointing with 1 finger will usually help direct the examination. The groin region may be indicative of an intra-articular problem. Lateral-based pain may be associated with intra- or extra-articular aspects. A characteristic sign of patients with intra-articular hip pain is the “C Sign” [17]. The patient will hold his or her hand in the shape of a C and place it above the greater trochanter, with the thumb positioned posterior to the trochanter and fingers extending into the groin. Posterior-superior pain requires the differentiation of hip and back pain. Bilateral shoulder and iliac crest heights in the standing position are compared to evaluate leg length discrepancies (Fig. 1a and b). Incremental heel lifts placed under the short side foot will help with orthotic considerations. Trunk bending (side-to-side and forward) is performed to evaluate the lumbar spine and to differentiate structural from nonstructural scoliosis (Fig. 1c and d). General body habitus and joint laxity are easily assessed in the standing examination (Fig. 1e).
Fig. 1.
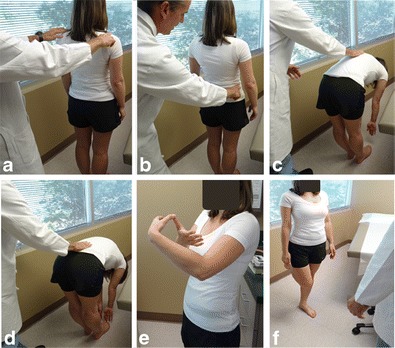
Standing evaluation. a and b Shoulder and iliac crest heights are examined with the patient with dynamic loading of the hip joint in the standing position. c As the patient bends forward at the trunk, spinal alignment is palpated. d The degree of trunk flexion is noted in full flexion. e Laxity of the thumb. f Recurvatum of the elbow. g The single leg stance phase test is performed bilaterally and observed from behind and in front of the patient. The patient flexes the hip and knee at 45° and hold this position for 6 seconds
Gait abnormalities often help detect hip pathology and the kinematic chain. The patient is taken to an area large enough to observe a full gait of 6 to 8 stride lengths. The key elements of gait evaluation include foot progression angle, pelvic rotation, stance phase, and stride length. The following abnormal gait patterns can be associated with hip pathologies: winking gait with excessive pelvic rotation in the axial plane; abductor deficient gait (Trendelenburg gait or abductor lurch); antalgic gait with a shortened stance phase on the painful side; and short leg gait with dropping of the shoulder in the direction of the short leg.
The single-leg stance phase test (Trendelenburg test) is performed during the standing evaluation of the hip. The single-leg stance phase test is performed bilaterally, with the non-affected leg examined first, to establish a baseline (Fig. 1f). A positive is noted if the pelvis drops toward the non-bearing side or shift of more than 2 cm toward the bearing (affected) side, which may indicate that the abductor musculature is weak or the neural loop of proprioception is disrupted on the bearing side. Trunk inclination for the bearing (affected) side is also noted in a positive single leg stance test. This assessment is performed in a dynamic fashion by some examiners.
Seated examination
The seated hip examination consists of a thorough vascular, lymphatic, and neurologic examination, which are performed even in apparently healthy individuals. Vascular and lymphatic assessment includes the posterior tibial pulse, any swelling of the extremity, and inspection of the skin. The neurologic evaluation includes sensibility, motor function, and deep tendon reflexes (Patellar and Achilles). The presence of radicular neurologic symptoms is detected by the straight leg raise test, performed by passively extending the knee into full extension.
The seated position provides a reproducible platform for the assessment of hip internal and external rotation (Fig. 2a and b). The ischium is square to the table at 90° of hip flexion. Values of hip rotation measured in different positions (seated, prone, supine) can be compared for an assessment of ligamentous vs osseous abnormality. Passive internal and external rotation is performed until a gentle endpoint is obtained and compared bilaterally. Proper hip function requires sufficient internal rotation and there should be at least 10° of internal rotation at the midstance phase of normal gait [18], but less than 20° is abnormal. Excessive femoral anteversion may be indicated by increased internal rotation combined with a decreased external rotation.
Fig. 2.

Seated external a and internal b rotation range of motion. Passive internal and external rotation testing are compared from side to side. In the seated position, the ischium is square to the table, thus providing sufficient stability at 90° of hip flexion. The seated position offers the most reproducible platform for the accurate rotational measurement
Supine examination
The supine examination begins with the inspection of leg length discrepancy. Tenderness with palpation is documented for the abdomen, pubic symphysis, and adductor tubercle. Differentiation of isolated adductor tendinitis and sports hernia may be made by a resisted sit-up torso flexion.
Hip ranges of motion are recorded for passive abduction, adduction, and flexion. Bring both of the patient’s legs into flexion (knees to chest, Fig. 3a) and note the pelvic position because the hip may stop early in flexion resulting in pelvic rotation to achieve end range of motion. With both legs in flexion, the pelvis is in a zero set-point (eliminating lumbar lordosis) important for the Hip Flexion Contracture Test (Thomas test). The patient holds 1 knee to their chest and passively moves the contralateral leg into extension (Fig. 3b). Inability for the back of the thigh to reach the table indicates the presence of contracture and patients with hyperlaxity or lumbar spine hyperlordosis can result in a false-negative. In patients with hyperlaxity or connective tissue disorders, the zero set point can be established with an abdominal contraction. The dial test is an assessment of capsular laxity. It includes passive internal rotation of the leg, followed by releasing the leg and allowing it to external rotate. External rotation of more than 45°, relative to vertical, is a positive test [19].
Fig. 3.

Supine examination starting position, hip flexion contracture test and FABER test a Starting position. Zero set point of the pelvis is achieved by having the patient hold the contralateral leg in full flexion, thus establishing neutral pelvic inclination. b Hip flexion contracture test. With the patient holding the contralateral leg in full flexion (zero set point for the lumbar spine), the examined hip is passively extended toward the (lack of terminal hip extension) this demonstrates a hip flexion contracture. c Flexion, abduction, external rotation test (FABER). The examiner brings the leg into 90° of flexion and externally rotates and abducts it so that the ipsilateral ankle rests distal to the knee of the contralateral leg
Hip joint vs sacroiliac joint pain is detected by the flexion, abduction, external rotation test (FABER), historically known as the Patrick test (Fig. 3c). The leg is placed in Fig. 4 position with the knee in flexion and hip in flexion, abduction, and externally rotation so that the ankle rests on the contralateral thigh. Ipsilateral or contra-lateral sacroiliac discomfort may be felt. Re-creation of hip pain can be associated with posterior femoroacetabular impingement, ligamentous injury, or trochanteric pathologies.
Fig. 4.
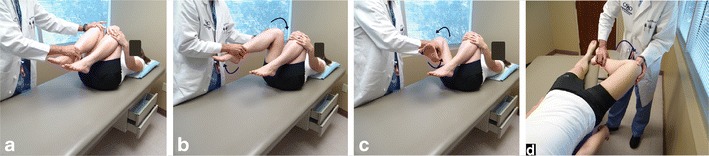
Femoroacetabular congruence tests in the supine position. a Patient is in the supine position and instructed to hold the nonaffected leg in flexion beyond 90°, thus establishing a zero pelvic set point and eliminating lumbar lordosis b DIRI: the examined hip is brought into 90° flexion or beyond and is passively taken through a wide arc of adduction and internal rotation. c DEXRIT: the hip is then brought into 90° flexion or beyond and dynamically taken through a wide arc of abduction and external rotation d Posterior rim impingement test. The patient rests at the edge of the examining table, with affected leg hanging freely at the hip while holding the contralateral leg in full flexion. The examined leg is then brought into full hip extension, abducted and externally rotated
Several tests exist for the assessment of femoroacetabular congruence, instability, or intra-articular pathology. Ganz originally described the flexion, adduction, and internal rotation test [20], and McCarthy later described the dynamic assessment of the femoroacetabular congruence and relationship to the labrum [21].
The dynamic internal rotatory impingement (DIRI) test is the assessment of anterior femoroacetabular congruence (DIRI). The zero set-point of the pelvis must be obtained by the patient holding the contralateral leg in flexion. The hip is dynamically taken in a wide arc from abduction/external rotation to flexion, adduction, and internal rotation (Fig. 4a and b). Re-creation of the complaint pain is a positive result. Note the degree of flexion that causes impingement, which helps determine the degree, type, and location of anterior impingement. The Scour test is performed in the same manner as DIRI, while applying pressure at the knee to increase pressure on the hip joint.
The dynamic external rotatory impingement test (DEXRIT) includes a wide arc movement of passive abduction and external rotation. The patient holds the contralateral leg in flexion to establish the zero set point of the pelvis. The is dynamically taken from 90° flexion or beyond through an arc of abduction and external rotation to extension (Fig. 4c). The DEXRIT is an assessment of supero-lateral and posterior femoroacetabular impingement. Patients with antero-inferior hip instability, antero-inferior acetabular hypoplasia, torn teres ligament, and capsular laxity may also exhibit a positive DEXRIT. A positive result is noted with re-creation of pain or feeling of instability. Both the DEXRIT and DIRI can be performed intraoperatively for direct visualization of femoroacetabular congruence.
The posterior rim impingement test is performed to assess the congruence between the posterior wall and femoral neck (Fig. 4d). The patient is positioned at the edge or end of the examination table so that the leg can hang freely to full extension. The patient established the pelvic zero set-point with both legs held in flexion. The examined leg is allowed to reach full extension off the table, and then taken into abduction and external rotation. Recreation of the symptoms is a positive test and can also present as an apprehension sign in cases of anterior instability.
Lateral examination
Palpation in the lateral position includes suprasacroiliac area, sacroiliac (SI) joint, gluteus maximus origin, piriformis muscle, and sciatic nerve. The facets of the greater trochanter (anterior, lateral, supero-posterior and posterior) are palpated. The insertion of the gluteus minimus located at the anterior facet, the gluteus medius at the supero-posterior and lateral facets, and the trochanteric bursa at the posterior facet.
Strength is assessed with any type of lateral-based hip complaint. The tests are performed in lateral decubitus with the patient actively abducting the hip against resistance. The gluteus medius strength test is performed with the knee in flexion to release the gluteus maximus contribution for the iliotibial band. The overall abductor strength is evaluated with the knee in extension and the gluteus maximus is tested asking the patient to abduct and extend the hip.
A set of passive adduction tests (similar to Ober’s test) is performed with the leg in 3 positions - extension (tensor fascia lata contracture test) (Fig. 5a), neutral (gluteus medius contracture test) (Fig. 5b), and flexion (gluteus maximus contracture test) (Fig. 5c).
Fig. 5.

Passive adduction tests a The tensor fascia lata contracture test: With the knee in extension, the examiner passively brings the hip into extension then adduction. b Gluteus medius contracture test is performed with knee flexion, thus excluding the gluteus maximus contribution for the iliotibial band. The examiner passively adducts the hip toward the examination table. c The gluteus maximus contracture test is performed with the ipsilateral shoulder rotated toward the examination table. With the examined leg held in knee extension, the examiner passively brings the hip into flexion then adduction
The lateral decubitus is also utilized for femoroacetabular congruence evaluation. The passive flexion adduction internal rotation (FADDIR) test is performed in a dynamic manner (Fig. 6a) Any reproduction of the patient’s complaint and the degree of femoroacetabular impingement are noted. FADDIR is traditionally performed as part of the supine assessment.
Fig. 6.

Femoroacetabular congruence tests in the lateral position. a Flexion, adduction, internal rotation (FADDIR). In the lateral position, the examiner dynamically brings the examined hip into flexion, adduction and internal rotation, while monitoring the superior aspect of the hip. b Lateral rim impingement test. The examiner cradles the patient’s lower leg with one arm and monitors the hip joint with the opposing hand. The affected hip is passively brought through a wide arc from flexion to extension in continuous abduction while externally rotating the hip. c Apprehension test. The examiner brings the hip from flexion to extension in external rotation and abduction. With the opposite hand, the examiner forces forward the proximal femur to provoke anterior inferior subluxation of the femoral head
The lateral rim impingement test is performed with the hip passively abducted and externally rotated (Fig. 6b). Reproduction of the patient’s pain is scored positive and can be caused by anterior instability or posterior impingement. If the feeling of guarding or anterior pain is present, the test is positive for instability. An apprehension test with a provocative maneuver is also executed in the lateral position (Fig. 6c), including a forward force to test antero-inferior instability [22]. Beyond the capsular and teres ligament, this test is also useful to detect acetabular antero-inferior hypoplasia.
Prone examination
In the prone position is also performed the rectus contracture test (also known as Ely test) (Fig. 7b). Passively bring the lower leg into flexion noting the end range of motion. The femoral anteversion test, traditionally known as Craig’s test, will give the examiner an idea of femoral anteversion and retroversion (Fig. 7a). Palpate the greater trochanter and internally/externally rotate the hip until the greater trochanter is in the most lateral position. Note the angle of the lower leg compared with vertical. Normally, femoral anteversion is between 10° and 20°.
Fig. 7.
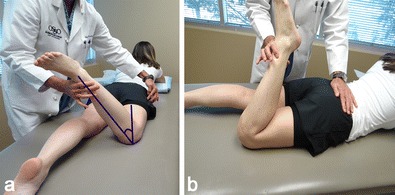
Femoral anteversion and rectus contracture tests. a Femoral anteversion test. The knee is flexed to 90° and the examiner manually rotates the leg while palpating the greater trochanter. The examiner positions the greater trochanter so that it protrudes most laterally, noting the angle between the axis of the tibia and an imaginary vertical line. b Rectus contracture test. The lower extremity is flexed toward the gluteus maximus. Any raise of the pelvis or restriction of knee flexion motion is indicative of rectus femoris contracture
Specific tests
Complex coexisting conditions may present, such as snapping hip, extra-articular peritrochanteric pain, and extra-articular posterior pain, which will require further examination. In these cases, specific tests have been described for the differential diagnosis [3, 21, 23, 24, 25•, 26]. The clinical exams described in this paper form the basis of a thorough physical examination that will guide the examiner toward the incorporation of specific tests when necessary.
Conclusion
As our understanding of anatomy and biomechanics evolve, the structured 21-step physical examination of the hip allows for a 4 layer assessment in the patients who present with hip pain [27•].
Compliance with Ethics Guidelines
Conflict of Interest
Hal D. Martin declares that he has no conflict of interest.
Ian J. Palmer declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Scopp JM, Moorman CT., III The assessment of athletic hip injury. Clin Sports Med. 2001;20:647–59. doi: 10.1016/S0278-5919(05)70277-5. [DOI] [PubMed] [Google Scholar]
- 2.Aprato A, Jayasekera N, Villar R. Timing in hip arthroscopy: does surgical timing change clinical results? Int Orthop. 2012;36:2231–4. doi: 10.1007/s00264-012-1655-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Domb BG, Brooks AG, Byrd JW. Clinical examination of the hip joint in athletes. J Sport Rehabil. 2009;18:3–23. doi: 10.1123/jsr.18.1.3. [DOI] [PubMed] [Google Scholar]
- 4.Martin HD, Shears SA, Johnson JC, et al. The endoscopic treatment of sciatic nerve entrapment/deep gluteal syndrome. Arthroscopy. 2011;27:172–81. doi: 10.1016/j.arthro.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 5.Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16:578–87. doi: 10.1053/jars.2000.7683. [DOI] [PubMed] [Google Scholar]
- 6.D'Aubigne RM, Postel M. Function al results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–75. [PubMed] [Google Scholar]
- 7.Christensen CP, Althausen PL, Mittleman MA, et al. The nonarthritic hip score: reliable and validated. Clin Orthop Relat Res. 2003;406:75–83. doi: 10.1097/00003086-200301000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Martin DP, Engelberg R, Agel J, Swiontkowski MF. Comparison of the musculoskeletal function assessment questionnaire with the short form-36, the western Ontario and McMaster universities osteoarthritis index, and the sickness impact profile health-status measures. J Bone Joint Surg Am. 1997;79:1323–35. doi: 10.2106/00004623-199709000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–40. [PubMed] [Google Scholar]
- 11.Mohtadi NG, Griffin DR, Pedersen ME, et al. The development and validation of a self-administered quality-of-life outcome measure for young, active patients with symptomatic hip disease: the International Hip Outcome Tool (iHOT-33) Arthroscopy. 2012;28:595–605. doi: 10.1016/j.arthro.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 12.Griffin DR, Parsons N, Mohtadi NG, Safran MR. A short version of the International Hip Outcome Tool (iHOT-12) for use in routine clinical practice. Arthroscopy. 2012;28:611–6. doi: 10.1016/j.arthro.2012.02.027. [DOI] [PubMed] [Google Scholar]
- 13.Martin RL, Mohtadi NG, Safran MR, et al. Differences in physician and patient ratings of items used to assess hip disorders. Am J Sports Med. 2009;37:1508–12. doi: 10.1177/0363546509333851. [DOI] [PubMed] [Google Scholar]
- 14.Martin HD, Kelly BT, Leunig M, et al. The pattern and technique in the clinical evaluation of the adult hip: the common physical examination tests of hip specialists. Arthroscopy. 2010;26:161–72. doi: 10.1016/j.arthro.2009.07.015. [DOI] [PubMed] [Google Scholar]
- 15.Cibere J, Thorne A, Bellamy N, et al. Reliability of the hip examination in osteoarthritis: effect of standardization. Arthritis Rheum. 2008;59:373–81. doi: 10.1002/art.23310. [DOI] [PubMed] [Google Scholar]
- 16.Martin HD. Clinical examination of the hip. Oper Tech Orthop. 2005;15:177–81. doi: 10.1053/j.oto.2005.07.008. [DOI] [Google Scholar]
- 17.Byrd JW. In: Operative hip arthroscopy. New York, NY: Springer, 2005:78–83.
- 18.Perry J. Gait analysis normal and pathological function. Thorofare, NJ: SLACK Inc.; 1992. [Google Scholar]
- 19.Philippon M, Zehms C, Briggs K, et al. Hip instability in the athlete. Oper Tech Sport Med. 2007;15:189–94. doi: 10.1053/j.otsm.2007.10.004. [DOI] [Google Scholar]
- 20.Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–20. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 21.McCarthy JC, Busconi BD, Owens BD. Assessment of the painful hip. In: McCarthy JC, editor. Early hip disorders. New York, NY: Springer; 2003. pp. 3–6. [Google Scholar]
- 22.Martin RL, Palmer I, Martin HD. Ligamentum teres: a functional description and potential clinical relevance. Knee Surg Sports Traumatol Arthrosc. 2012;20:1209–14. doi: 10.1007/s00167-011-1663-1. [DOI] [PubMed] [Google Scholar]
- 23.Byrd JWT. Physical examination. In: Byrd JWT, editor. Operative hip arthroscopy. 2. New York: Springer; 2005. pp. 36–50. [Google Scholar]
- 24.Martin HD, Shears SA, Palmer IJ. Evaluation of the hip. Sports Med Arthrosc. 2010;18:63–75. doi: 10.1097/JSA.0b013e3181dc578a. [DOI] [PubMed] [Google Scholar]
- 25.Plante M, Wallace R, Busconi BD. Clinical diagnosis of hip pain. Clin Sports Med. 2011;30:225–38. doi: 10.1016/j.csm.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 26.Reider B, Martel J. Pelvis, hip and thigh. In: Reider B, Martel J, editors. The orthopedic physical examination. Philadelphia: WB Saunders; 1999. pp. 159–99. [Google Scholar]
- 27.Draovitch P, Edelstein J, Kelly BT. The layer concept: utilization in determining the pain generators, pathology and how structure determines treatment. Curr Rev Musculoskelet Med. 2012;5:1–8. doi: 10.1007/s12178-011-9105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


