Abstract
Adult acquired flatfoot deformity (AAFD), embraces a wide spectrum of deformities. AAFD is a complex pathology consisting both of posterior tibial tendon insufficiency and failure of the capsular and ligamentous structures of the foot. Each patient presents with characteristic deformities across the involved joints, requiring individualized treatment. Early stages may respond well to aggressive conservative management, yet more severe AAFD necessitates prompt surgical therapy to halt the progression of the disease to stages requiring more complex procedures. We present the most current diagnostic and therapeutic approaches to AAFD, based on the most pertinent literature and our own experience and investigations.
Keywords: Flatfoot, AAFD, Adult acquired flatfoot deformity, Adult flatfoot, Posterior tibial tendon insufficiency, Flatfoot staging, Flatfoot treatment
Introduction
Adult acquired flatfoot deformity (AAFD), also known as posterior tibial tendon (PTT) insufficiency, embraces a wide spectrum of deformities [1]. The latter results from the progressive weakening of the PTT, the principal dynamic arch support of the foot. The PTT is affected most often just distal to and at the level of the medial malleolus, commonly evolving from tendinosis to partial and complete tear. However, AAFD results from a combination of PTT insufficiency and failure of both capsular and ligamentous structures of the foot. The spring ligament (ie, calcaneonavicular) is the most frequently affected [2], often leading to a combined plantar sag or forefoot abduction through the talonavicular and subtalar joints. Consequently, a combination of plantar and medial migration of the talar head leads to flattening of the arch as the foot displaces from underneath the talus [3]. The interosseous ligament connecting the calcaneus and talus is also frequently involved, contributing to heel valgus. Dysfunction of the deltoid ligament can lead to medial ankle instability with ankle deformity and foot deformity occurring in the most advanced cases of AAFD. Tightness of the gastrocnemius or Achilles tendon has also been suggested as an aggravating valgus-deforming force [4]. Overall, flatfoot deformity typically consists of a combination of plantar sag, midfoot abduction, and heel valgus.
AAFD has a multifactorial pathology. It affects women more frequently than men, peaking at 55 years of age [3]. A pre-existing flatfoot, which increases stresses on the ligaments that support the arch and the posterior tibial tendon, is present in most patients. Obesity, hypertension, diabetes, and high impact sports have also been identified as risk factors [5]. A tight gastrocnemius muscle or Achilles tendon also contributes to the deformity [4].
The aim of the present paper is to present the most current diagnostic and therapeutic approaches to AAFD, based on the most pertinent literature and our own experience and investigations.
Staging
The clinical manifestation of AAFD is as variegated as its pathophysiology (Table 1). Four stages of the disease have been described [1, 6–8]. Stage I presents without arch collapse, but frequently with a relatively low lying arch that has been present since childhood. Patients may complain of medial ankle pain caused by posterior tibial tenosynovitis and/or tendinosis [6]. Spondyloarthropathy has also been associated with stage I AAFD in a subgroup of patients [1].
Table 1.
Stages of adult acquired flatfoot deformity
| Stage | Description |
|---|---|
| I | No deformity (preexisting relative flatfoot often present) |
| IIa | Moderate flexible deformity (minimal abduction through talonavicular joint, <30 % talonavicular uncoverage) |
| IIb | Severe flexible deformity with either abduction deformity through talonavicular joint (ie, >30 %–40 % talonavicular uncoverage) or subtalar impingement |
| III | Fixed deformity (involving the triple-joint complex) |
| IVa | Hindfoot valgus and flexible ankle valgus without significant ankle arthritis |
| IVb | Hindfoot valgus with rigid ankle valgus or flexible deformity with significant ankle arthritis |
Stage II AAFD manifests with a more significant deformity. The latter is flexible and characteristically correctible through passive inversion at the talonavicular joint and hindfoot. Deland et al. [7] have further subdivided stage II AAFD in stage IIa and stage IIb. Stage IIa is a mild to moderate flexible deformity with minimal abduction through the talonavicular joint as evidenced by less than 30 % talonavicular uncoverage on a standing AP radiograph of the foot (Fig. 1). The interosseous ligament is usually insufficient. Stage IIb presents with a flexible deformity. Commonly, there is more than 30 % talonavicular uncoverage (Fig. 2), determined by a more substantial failure of the spring ligament and secondary restraints of the arch [2]. This results in greater forefoot abduction. The interosseous and superomedial deltoid ligaments are also frequently stretched or torn. Care should be taken to ensure that x-rays are taken with the patient letting their arch collapse so that a true depiction of the deformity is obtained. Also, patients with lateral impingement at the subtalar joint from deformity should be considered stage IIb.
Fig. 1.

This weight-bearing, AP radiograph of the foot demonstrates a patient with flatfoot deformity associated with minimal forefoot abduction as evidenced by less than 30 % talo-navicular uncoverage (arrow)
Fig. 2.

This weight-bearing, AP radiograph of the foot demonstrates a patient with a more severe flatfoot deformity associated with a large amount of forefoot abduction as evidenced by more than 30 % talo-navicular uncoverage (arrow)
Stage III AAFD clinically presents with rigid deformity, which is not passively correctible beyond neutral. The rigidity arises at the triple joint complex (talonavicular, subtalar, and calcaneocuboid joints) leading to fixed hindfoot valgus and abduction through the midfoot [3].
Stage IV AAFD is a foot deformity aggravated by valgus ankle joint deformity (with or without arthritis) [1]. Ankle valgus results from the lateral tilt of the talus as a consequence of the deltoid ligament failure (Fig. 3). Every patient with advanced deformity (stage IIb or above) should have a standing AP ankle x-ray to rule out talar tilt, as heel valgus may be driven by either ankle or hindfoot valgus. Patients with the most severe stage of AAFD should be thoroughly examined - clinically and radiographically - to correctly assess talar tilt, as heel valgus may be driven by either ankle or hindfoot valgus. Stage IV AAFD is further divided into stages IVa and IVb [1]. Stage IVa is characterized by hindfoot valgus with flexible ankle valgus without significant ankle arthritis. Stage IVb refers to hindfoot valgus with rigid ankle valgus or flexible ankle valgus with significant arthritis.
Fig. 3.

A weight-bearing, mortise radiograph of the ankle demonstrates valgus talar tilt and opening at the medial edge of the ankle joint line suggestive of early deltoid ligament insufficiency in the setting of flatfoot deformity
Diagnosis
Clinical
Along with a long history of a low-lying foot arch, female gender, middle age (ie, mid 50’s), and obesity, patients often initially present to the physician with a complaint of “ankle pain”. Medial pain is typically secondary to PTT tendonitis, but can improve and be absent after elongation or complete rupture of the tendon. Therefore, the intensity of the pain is not necessarily associated with the severity of AAFD. As the deformity progresses, patients commonly experience lateral foot pain, arising at the angle of Gissane from talocalcaneal impingement or in more rare cases from fibular abutment against the calcaneus [9•].
Physical examination is paramount to diagnose AAFD. The area posterior to the medial malleolus should be examined for swelling, which has been correlated with tendinitis, tenosynovitis, and tendinosis of the PTT [10•]. As most patients present after the onset of deformity, the foot usually appears flattened and with a significant valgus deformity of the heel. Stage IV AAFD patients will present with ankle valgus as well. The “too many toes” sign (Fig. 4) is also indicative of AAFD, but can occur with other conditions and is therefore not pathognomonic.
Fig. 4.

This clinical photograph demonstrates the finding of the “too many toes sign.” When looking at the heel from the back of the patient, only the fifth toe and part of the fourth toe are seen in a normal foot. In a flatfoot, more toes are seen (arrow). In this case, the patient has bilateral hindfoot valgus and flatfoot. However, the left is more severe
Palpation along the distal portion of the PTT is highly suggestive of PTT degeneration. Eliciting pain at the lateral aspect of the hindfoot is suggestive of lateral impingement. Patients with stages III or IV may also experience pain on palpation of arthritic joints (ie, talonavicular, subtalar, calcaneocuboid, and ankle). The inability to perform a single heel rise is highly suggestive of PTT insufficiency. Ankle range of motion must also be evaluated, as dorsiflexion is often compromised due to gastrocnemius/Achilles tendon tightness [4].
Harris mat score
Coughlin and Kaz [11] reported significant correlations between Harris mat imprint and heel valgus, lateral talometatarsal angle, and first metatarsocuneiform height. Harris mat scores may therefore be useful to quantify the extent of the acquired flatfoot deformity.
Radiographic
Clinical suspicion of AAFD should be confirmed with weight-bearing AP and lateral foot, and AP ankle radiographs. These views will help assess arch collapse (ie, perhaps best assessed by Meary’s or the lateral first tarsometatarsal angle), forefoot abduction (at the talonavicular joint), talar head uncoverage [3, 12], and talar tilt in stage IV AAFD. Talar head uncoverage can be calculated either as a percentage (>30 % or <30 %) or as the lateral talonavicular incongruency angle, which correlates well with the coverage angle and uncoverage percent [12]. On the lateral view of the foot, naviculocuneiform and first tarsometatarsal joint collapse should also be investigated. Hindfoot valgus can be evaluated with either a hindfoot alignment view [13] (Fig. 5) or long axial view [14]. All radiographs should be carefully examined to identify arthritic changes that could substantially affect treatment choice (ie, joint fusion vs soft tissue procedures and osteotomies).
Fig. 5.

A weight-bearing, hindfoot alignment view of both feet demonstrates bilateral hindfoot valgus deformity as evidenced by the lateral and valgus position of the calcaneus with respect to the axis of the tibia. The left (labeled “L”) is much more severe than the right (labeled “R”)
MRI is not crucial to further investigate AAFD, although it helps assess the extent of cartilage, tendon, and ligament involvement. Bone edema on T2-weighted scans may reveal signs of lateral bony impingement, particularly between the talus and calcaneus at the angle of Gissane. Assessment of spring ligament integrity is important for surgical planning and ligament reconstruction for patients with large amounts of deformity.
In recent years, we have utilized weight-bearing, multiplanar axial imaging of the hindfoot [9•, 12] to overcome radiographic limitations related to patient and radiographic beam positioning. We have shown that lateral pain in patients with flatfoot deformity most commonly occurs from the above mentioned impingement at the angle of Gissane, but can be multifactorial as well.
Treatment
Conservative management
All patients affected by any stage of AAFD should undergo non surgical treatment before considering surgery. Nielsen et al. [15] reported on 64 consecutive patients with a diagnosis of PTT tendinosis treated with physical therapy modalities; medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs); oral administration or local infiltration of corticosteroid; and orthotics or bracing such as a foot orthoses, an arch and ankle brace, a low-articulating ankle-foot orthosis (LAFO) or similar AFO, cast-boot (“cam” walker), or shoe modifications. The authors reported an 87 % success rate defined as not requiring further surgical treatment. Similar results have been reported by other authors assessing non-operative management of PTT insufficiency with success rates ranging from 67 %–90 % [16–18]. In particular, Alvarez et al. [18] treated 47 consecutive patients with stage I or II posterior tibial tendon dysfunction. Patients were treated in a short, articulated AFO or foot orthosis, high-repetition exercises, aggressive plantarflexion activities, and an aggressive high-repetition home exercise program that included gastrocsoleus tendon stretching. The strengthening exercises were for the posterior tibial, peroneals, anterior tibial, and gastroc-soleus muscles and included isokinetic exercises, exercise band, heel rises (double and single support), and toe walking. Success was defined as 10 % strength deficit (compared with the uninvolved side), the ability to perform 50 single-support heel rises with minimal or no pain, the ability to ambulate 100 feet on the toes with minimal or no pain, and the ability to tolerate 200 repetitions of the home exercises for each muscle group. With this treatment protocol, 89 % of patients were satisfied.
The effectiveness in improving pain is, however, counterbalanced by the cumbersome nature of the braces and the restriction in motion that they cause [17]. For such reasons, braces are seldom recommended for more than 2 months if they fail to improve symptoms [3]. Obesity has also been suggested as a possible risk factor for failing conservative management [15]. This observation is of particular interest given that AAFD patients are often obese [5]. As yet, no study has shown that braces or orthotics can prevent progression of PTT insufficiency and AAFD.
The authors prefer to immobilize patients in a removable boot (“CAM” type) for 3 to 6 weeks. In cases of mild/moderate deformity and a good response to immobilization, patients are progressed in a comfortable shoe with an orthotic with arch support and a medial heel post to correct hindfoot valgus. More significant deformities may be addressed with a short articulated AFO or an Arizona brace [3]. Physical therapy consisting of Achilles tendon stretching, inversion, and toe flexor strengthening along with proprioception exercises is recommended once the pain has subsided.
Surgical management
Stage I
Surgery is indicated in patients who did not respond to 3 months or more of conservative management, but is rarely needed. The condition of the PTT will dictate the type of procedure to perform (ie, tenosynovectomy, repair, tendon transfer), but in our experience soft tissue surgery alone can be insufficient. In order to protect the PTT from excessive stresses, we often combine PTT surgery in many cases with a medializing calcaneal osteotomy to correct heel valgus even though it is not as severe as in the other stages [3, 19]. Heel valgus determines overload along the medial side of the foot, which could consequently lead to failure of the newly repaired PTT. In our hands the combination of a PTT-related procedures and calcaneal osteotomy provides good long-term relief in symptomatic stage I AAFD patients [3]. Subtalar arthroereisis represents a more recent option to treat flexible AAFD, with or without additional soft tissue procedures. Despite some good results associated with subtalar arthroereisis [20, 21], this procedure has a high incidence of sinus tarsi pain until the screw is removed [21] and is therefore controversial. This will be discussed further with respect to the other stages.
PTT procedures and medializing calcaneal osteotomy require postoperative non–weight bearing in a splint for 2 weeks followed by a removable cast for 4 or more weeks. The patient may then be progressed to full weight bearing over a 4 week period. Range-of-motion exercises are begun at 2 weeks, and progressive strengthening exercises are begun at 12 weeks after surgery.
Stage II
The surgical management of asymptomatic stage II deformity or symptomatic deformity responding to conservative management is controversial [18, 22–24]. Given the substantial limitations associated with arthrodesis of joints involved in AAFD [25, 26•], we believe that patients should be surgically treated before progression to stage III.
Stage IIa
As noted above, stage IIa AAFD presents with a mild to moderate flexible deformity associated with ≤30 % talar head uncoverage. Different operative approaches are available to treat the deformity, including sinus tarsi implants (ie, arthroereisis screws), medial column fusion, calcaneal osteotomies, and tendon transfers.
Subtalar arthroereisis has been increasingly used to treat flatfeet in children [21]. This is achieved by inserting a screw-like device into the sinus tarsi, which restricts hindfoot valgus and vertically orients the calcaneus beneath the ankle joint [21]. Moreover, the talus is dorsiflexed and externally deviated, which helps correct talonavicular subluxation [21]. Sinus tarsi implants are also being used to treat stage IIa AAFD [20, 21, 27] as an alternative to medializing calcaneal osteotomies. Despite lacking prospective randomized controlled trials, the literature reports good mid-term clinical and radiographic results with subtalar arthroereisis [20, 21, 28]. Although the procedure prevents complications such as malunions, non-unions, neurovascular lesions, and prolonged immobilization associated with calcaneal osteotomies, it is not exempt from its own complications, which include persistent pain, implant dislocation, implant fracture, talar cysts or osteonecrosis, and foreign body reaction [27]. The most common complication is sinus tarsi pain, reported in over one third of patients [20, 21, 27, 28]. Although the pain disappears with removal of the implant, persistent pain may be experienced [21, 27] and the procedure is less likely to be successful in more advanced deformities.
Medializing calcaneal osteotomy, flexor digitorum longus (FDL) transfer, and gastrocnemius recession represents our treatment of choice in stage IIa AAFD. A tight gastrocnemius or Achilles tendon, which could be responsible for causing or aggravating heel valgus [4], is addressed with either a gastrocnemius recession or a percutaneous Achilles lengthening, respectively. The Silfverskiold test [29] can be performed intraoperatively and if the equinus improves with knee flexion a gastrocnemius recession is preferred since it is not likely to overlengthen the Achilles, while allowing for a quicker recovery [30]. A medializing calcaneal osteotomy is performed to realign the hindfoot from heel valgus. This offloads the spring ligament and increases the inversion moment arm of the gastrocsoleus complex. The FDL tendon transfer to the navicular compensates for the lost function of the degenerated PTT. Recent evidence suggests that significant clinical and radiographic improvements are achieved and maintained when preoperative lateral talometatarsal and tibiocalcaneal angles were <25° and <15°, respectively [31••]. Finally, an elevated medial column can be lowered to treat forefoot supination or varus persisting after hindfoot realignment (ie, to restore the “foot tripod”). If the first TMT joint is stable (ie, not hypermobile), an opening wedge medial cuneiform osteotomy (ie, Cotton osteotomy) (Fig. 6) can be performed to bring down the first ray with respect to the second metatarsal [32–34]. Conversely, an unstable or arthritic first TMT joint can be addressed with a fusion of the joint in the desired position [34] (Fig. 7a and b). Overall medium and long-term functional results of medializing calcaneal osteotomy, FDL transfer, and gastrocnemius recession are reported to be excellent [19, 31••, 35, 36•, 37•]. However, maximal benefit from the procedure is usually observed after 1 year from surgery [37•].
Fig. 6.

A weight-bearing, lateral radiograph of the foot shows the position of the plate used to fix (large arrow) the osteotomy of the medial cuneiform (ie, “Cotton osteotomy”). The radiograph also demonstrates fixation of a lateral column lengthening (small arrow) and a calcaneal heel slide (asterisk)
Fig. 7.
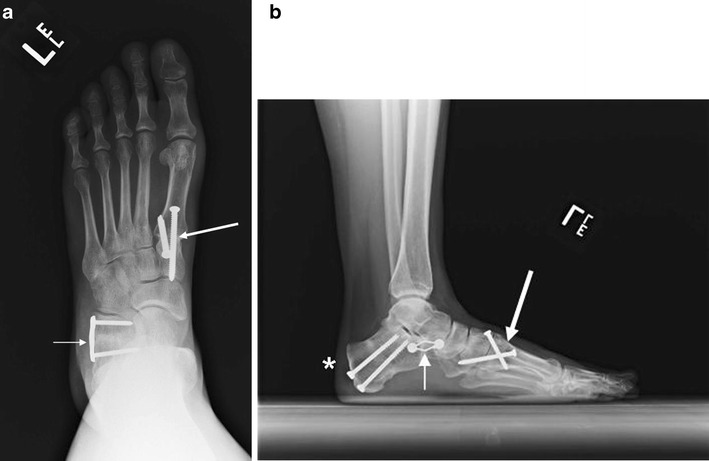
Weight-bearing, AP (a) and lateral (b) radiographs of the foot demonstrate a first tarsometatarsal fusion fixed with 2 cross screws (large arrow) and an Evans lateral column lengthening fixed with a claw plate (small arrow). A medializing calcaneal heel slide was also performed and stabilized with 2 screws (asterisk)
Stage IIb AAFD presents with severe flexible deformity associated with abduction deformity through the talonavicular joint and >30 % talonavicular uncoverage. The treatment for this stage is controversial in terms of adding lateral column lengthening (LCL) to the medializing calcaneal osteotomy, FDL transfer, gastrocnemius recession, and medial column procedures [38, 39]. The purpose of the LCL is to correct talonavicular joint abduction and to increase the foot arch. The lateral column is typically lengthened by means of an Evans-type procedure or calcaneocuboid distraction arthrodesis (Fig. 7a and b). As successful as these procedures have proved to be in terms of foot realignment [40–42], the most frequently observed complication is lateral foot discomfort affecting up to 45 % of patients in 1 study [7]. Pain and discomfort may arise as a consequence of lateral overload in the hindfoot and possibly the forefoot [41, 43••, 44, 45]. At our institution we have found the incidence of lateral overload/pain to decrease significantly (from 15 % to 6 %) with the use of intraoperative metal wedge templates to maintain mean normal eversion of the hindfoot. Such wedges allow the surgeon to intraoperatively assess the correction of abduction through the talonavicular joint and confirm near normal eversion motion [43••]. Other complications resulting from LCL include non-union, fifth metatarsal stress fractures, and stiffness [41, 42, 43••]. Although the ideal amount of LCL is unknown, in our experience the key is to lengthen the lateral column just enough to reasonably reduce talonavicular abduction and heel valgus, Normal eversion motion through the subtalar joint should be maintained. Most importantly, LCL resulting in excessive stiffness on the lateral side must be avoided.
In an attempt to reduce pain following LCL, Griend described a “Z” osteotomy of the anterior calcaneus [46]. At the present time, no medium or long-term clinical studies are available to assess the efficacy of the abovementioned technique, despite its interesting underlying biomechanical principles. The theoretical advantages are that the risk of malunion may be reduced by not needing to use iliac crest graft (whether autograft or allograft), minimizing the risk of elevation of the distal fragment because the osteotomy has a longitudinal arm not dependent upon healing of the bone graft. In addition, lateral foot overload may decrease [47].
Spring ligament repair or reconstruction is also performed at our institution in conjunction with other bony and soft-tissue procedures. While there is no clear clinical data reporting on the precise guidelines for the need for spring ligament reconstruction, spring ligament tear or degeneration has been observed in 70 % of patients with AAFD, commonly in its superomedial portion [48]. The lesion may not necessarily be the cause of AAFD, but it likely participates in the development of the deformity. In our experience, spring ligament reconstruction is indicated in those patients having a LCL, but who are not gaining sufficient correction of forefoot abduction with relatively large grafts [49, 50••]. It is crucial to preserve normal hindfoot eversion motion when doing a LCL as noted above. If the patient has adequate correction and good eversion motion, then the spring ligament is not reconstructed. Conversely, if the correction is inadequate, a spring ligament reconstruction is performed to maintain normal eversion motion by avoiding larger lateral column grafts [49]. In our experience [50••], spring ligament reconstruction using a peroneus longus autograft tendon transfer has yielded very good clinical and radiographic results at a mean of 9 years after surgery. At the present time, we use an allograft Achilles tendon to reconstruct the spring ligament which seems to give good results. However, medium and long-term results are not yet available.
In either stage IIa or stage IIb AAFD reconstruction, postoperative care consists of non–weight bearing in a splint for the first 2 weeks, followed by a cast or removable boot for at least 6 weeks. Range-of-motion exercises are initiated at 2 weeks after surgery. Progression to full weight bearing is allowed between weeks 8 and 10, depending on healing.
Stage III
Stage III AAFD consists of fixed deformity involving the triple-joint complex (ie, subtalar, calcaneocuboid, and talonavicular joints). Correction is achieved by fusing the talonavicular and subtalar joints, where most of the deformity occurs. Whenever possible, we try to spare the calcaneocuboid joint, unless frankly arthritic and symptomatic [51]. Indeed, triple arthrodesis results in notable foot rigidity and difficulty to adapt to uneven ground, while increasing the risk of developing ankle arthritis [25].
Triple arthrodesis is usually performed through 2 incisions. However, Myerson [52] presented a single medial incision technique to access all 3 joints. In their hands, 91 % of the talonavicular joint, 91 % of the subtalar joint, and 90 % of the calcaneocuboid joint could be prepared. A recent case series on 18 feet undergoing double arthrodesis through a single medial incision reported an 11 % non-union rate [53•]. In high risk patients, the lateral incision for arthrodesis eliminates the risk of lateral wound complications.
When correcting the flatfoot deformity, the heel should be fused in ≤5° of valgus with the forefoot in neutral (ie,, no forefoot supination or elevation of the first ray and no forefoot pronation). If heel valgus persists after achieving neutral of the forefoot and triple-joint complex, then a medializing calcaneal osteotomy can be added. It is important to not place the triple joint complex in overcorrection to achieve good alignment of the heel as lateral overload can result from fixed supination deformity. A first TMT procedure (fusion or osteotomy) may be added in patients with an elevated first ray. Besides non-union, stiffness and valgus malalignment are potential complications of triple arthrodesis, which can lead to failure of the deltoid ligament and ankle valgus [54].
Postoperative care consists of non–weight bearing in a cast for 10 to 12 weeks, followed by progressive weight-bearing in a removable boot for 4 weeks.
Stage IV
Stage IV AAFD consists of foot deformity and ankle deformity (lateral talar tilt), which can be either flexible (stage IVa) or fixed (stage IVb). Stage IVa AAFD can be addressed with joint-sparing procedures, while stage IVb is typically treated with foot procedures to correct the flatfoot deformity in conjunction with ankle fusion or replacement. As discussed previously, it is important to note that all patients with advanced deformity (ie,, stage IIb, III, IV) should have standing AP ankle x-rays to make sure ankle deformity is not missed (ie, hindfoot valgus can be caused by either foot deformity, ankle deformity, or both).
Stage IVa deformity is eligible for foot reconstruction without having to fuse or replace the ankle joint. Deltoid ligament reconstruction can be performed with a variety of techniques employing autografts, allografts, or tendon transfers [55, 56•, 57–60]. At our institution deltoid ligament reconstruction has been described using a peroneus longus tendon autograft [55, 56•]. The procedure requires proximal transection of the peroneus longus tendon. The tendon is then passed through a tunnel in the talus and the medial malleolus to replicate the fibers of the deep deltoid. Although now we are using allograft with the same drill holes, the results are not available at this time. Patients need to have cartilage remaining in the lateral ankle and correction of deformity in the foot must be done at the same time so the first ray is stable (ie, not elevated) and that valgus of the heel and ankle are corrected. To date, the technique presented by Deland et al. [55] is the only one with long-term clinical and radiographic results available in the literature [56•]. At almost 9 years follow-up [56•], results in a small cohort of patients were encouraging: the mean valgus talar tilt was 2°, the mean FAOS score was 68, the mean SF-36 score was 76, the mean visual analogue scale was 4, and the mean ankle range of motion was 47°.
Stage IVb AAFD may be addressed in different ways. At our institution patients older than 60 years of age, in good neurovascular and metabolic (ie, no diabetes) conditions, and without severe ankle deformity (≤15° valgus) are eligible for total ankle replacement (TAR). This procedure preserves ankle motion and limits strain across the other joints [61] that are otherwise stressed in the setting of an ankle fusion [62]. The remaining foot deformities can be addressed by means of triple arthrodesis. Moreover, the deltoid ligament complex must be evaluated with distraction from the replacement. Most often, though, enough correction with the implant occurs so that deltoid reconstruction is not necessary. Patients not eligible for TAR are treated with an ankle or pantalar fusion, while the flatfoot can be corrected with either joint-sparing or joint-sacrificing procedures based on their clinical presentation [26•] (Table 2).
Table 2.
Surgical treatment options for stage IV AAFD
| Foot/ankle deformity | Non-arthritic, flexible ankle | Rigid or flexible/arthritic ankle |
|---|---|---|
| Flexible foot | Flatfoot reconstruction with deltoid reconstruction | Flatfoot reconstruction with either ankle fusion or TAR. |
| Rigid foot | Triple arthrodesis with deltoid reconstruction | Triple arthrodesis with TAR or pantalar fusion |
AAFD adult acquired flatfoot deformity, TAR total ankle replacement
Conclusion
The growing complexity of the procedures necessary to address advanced stages of AAFD raises a still unanswered question: how soon should a patient be recommended to undergo surgery? Given the substantial limitations associated with arthrodesis of joints involved in AAFD [25, 26•], we believe that patients should be surgically treated before progression to stage III, or even IIb if possible. Many foot and ankle orthopaedic surgeons approach AAFD in distinct and personalized ways. These differences are especially evident for stages II and IV. Whatever the approach chosen to address the flatfoot deformity, it is paramount to achieve correct alignment of both the foot and ankle and to preserve as much flexibility as possible: the greater the stiffness, the worse the outcome.
Compliance with Ethics Guidelines
Conflict of Interest
Ettore Vulcano declares that he has no conflict of interest. Jonathan T. Deland declares that he has no conflict of interest. Scott J. Ellis declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as:• Of importance •• Of major importance
- 1.Bluman EM, Title CI, Myerson MS. Posterior tibial tendon rupture: a refined classification system. Foot Ankle Clin. 2007;12:233–49. doi: 10.1016/j.fcl.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Deland JT, de Asla RJ, Sung IH, Ernberg LA, Potter HG. Posterior tibial tendon insufficiency: which ligaments are involved? Foot Ankle Int. 2005;26:427–35. [DOI] [PubMed]
- 3.Deland JT. Adult-acquired flatfoot deformity. J Am Acad Orthop Surg. 2008;16:399–406. doi: 10.5435/00124635-200807000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Mann RA. Flatfoot in adults. In: Mann RA, Coughlin MJ, editors. Surgery of the foot and ankle. 7. St. Louis: Mosby; 1999. pp. 733–67. [Google Scholar]
- 5.Adult acquired flatfoot. Available at http://orthoinfo.aaos.org/topic.cfm?topic=a00173. Accessed January 2013.
- 6.Johnson KA, Strom DE. Tibialis posterior tendon dysfunction. Clin Orthop Relat Res. 1989;239:196–206. [PubMed] [Google Scholar]
- 7.Deland JT, Page A, Sung I-H, O'Malley MJ, Inda D, Choung S. Posterior tibial tendon insufficiency results at different stages. HSS J. 2006;2:157–60. [DOI] [PMC free article] [PubMed]
- 8.Vora AM, Tien TR, Parks BG, Schon LC. Correction of moderate and severe acquired flexible flatfoot with medializing calcaneal osteotomy and flexor digitorum longus transfer. J Bone Joint Surg Am. 2006;88:1726–34. [DOI] [PubMed]
- 9.• Ellis SJ, Deyer T, Williams BR, Yu JC, Lehto S, Maderazo A, et al. Assessment of lateral hindfoot pain in acquired flatfoot deformity using weightbearing multiplanar imaging. Foot Ankle Int. 2010;31:361–70. Ten patients with painful flexible flatfoot compared with 10 patients with painless flexible deformity. Multiplanar imaging parameters demonstrated good reliability for many of the standard flatfoot parameters. [DOI] [PubMed]
- 10.• DeOrio JK, Shapiro SA, McNeil RB, Stansel J. Validity of posterior tibial edema sign in posterior tibial tendon dysfunction. Foot Ankle Int. 2011;32:189–92. The authors reviewed medical records of patients with posterior tibial tendon insufficiency that underwent MRI. They found that thorough physical examination may help lower the cost of diagnosis by reducing the need for MRI. [DOI] [PubMed]
- 11.Coughlin MJ, Kaz A. Correlation of Harris Mats, physical exam, pictures, and radiographic measurements in adult flatfoot deformity. Foot Ankle Int. 2009;30:604–11. doi: 10.3113/FAI.2009.0604. [DOI] [PubMed] [Google Scholar]
- 12.Ellis SJ, Yu JC, Williams BR, Lee C, Chiu YL, Deland JT. New radiographic parameters assessing forefoot abduction in the adult acquired flatfoot deformity. Foot Ankle Int. 2009;30:1168–76. [DOI] [PubMed]
- 13.Saltzman CL, El-Khoury GY. The hindfoot alignment view. Foot Ankle Int. 1995;16:572–6. doi: 10.1177/107110079501600911. [DOI] [PubMed] [Google Scholar]
- 14.Buck FM, Hoffmann A, Mamisch-Saupe N, Espinosa N, Resnick D, Hodler J. Hindfoot alignment measurements: rotation-stability of measurement techniques on hindfoot alignment view and long axial radiographs. Am J Roentgenol. 2011;197:578–82. [DOI] [PubMed]
- 15.Nielsen MD, Dodson EE, Shadrick DL, Catanzariti AR, Mendicino RW, Malay DS. Nonoperative care for the treatment of adult-acquired flatfoot deformity. J Foot Ankle Surg. 2011;50:311–4. [DOI] [PubMed]
- 16.Chao W, Wapner KL, Lee TH, Adams J, Hecht PJ. Nonoperative management of posterior tibial tendon dysfunction. Foot Ankle Int. 1996;17:736–41. [DOI] [PubMed]
- 17.Augustin JF, Lin SS, Berberian WS, Johnson JE. Nonoperative treatment of adult acquired flatfoot with the Arizona brace. Foot Ankle Clin. 2003;8:637–45. [DOI] [PubMed]
- 18.Alvarez RG, Marini A, Schmitt C, Saltzman CL. Stage I and II posterior tibial tendon dysfunction treated by structured nonoperative management protocol: an orthosis and exercise program. Foot Ankle Int. 2006;27:2e8. doi: 10.1177/107110070602700102. [DOI] [PubMed] [Google Scholar]
- 19.Myerson MS, Badekas A, Schon LC. Treatment of stage II posterior tibial tendon deficiency with flexor digitorum longus tendon transfer and calcaneal osteotomy. Foot Ankle Int. 2004;25:445–50. doi: 10.1177/107110070402500701. [DOI] [PubMed] [Google Scholar]
- 20.Fernández de Retana P, Alvarez F, Bacca G. Is there a role for subtalar arthroereisis in the management of adult acquired flatfoot? Foot Ankle Clin. 2012;17:271–81. doi: 10.1016/j.fcl.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 21.Needleman RL. A surgical approach for flexible flatfeet in adults including a subtalar arthroereisis with the MBA sinus tarsi implant. Foot Ankle Int. 2006;27:9–18. doi: 10.1177/107110070602700103. [DOI] [PubMed] [Google Scholar]
- 22.Nonoperative treatment of posterior tibial tendonitis. Available at http://www.arizonaafo.com/default/index.cfm/side-bar/clinical-esearch/nonoperative-treatment-of-posterior-tibial-tendonitis. Accessed January 2013.
- 23.O'Connor K, Baumhauer J, Houck JR. Patient factors in the selection of operative vs nonoperative treatment for posterior tibial tendon dysfunction. Foot Ankle Int. 2010;31:197–202. doi: 10.3113/FAI.2010.0197. [DOI] [PubMed] [Google Scholar]
- 24.Durrant B, Chockalingam N, Hashmi F. Posterior tibial tendon dysfunction: a review. J Am Podiatr Med Assoc. 2011;101:176–86. doi: 10.7547/1010176. [DOI] [PubMed] [Google Scholar]
- 25.de Groot IB, Reijman M, Luning HA, Verhaar JA. Long-term results after a triple arthrodesis of the hindfoot: function and satisfaction in 36 patients. Int Orthop. 2008;32:237–41. doi: 10.1007/s00264-006-0295-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Taylor R, Sammarco VJ. Minimizing the role of fusion in the rigid flatfoot. Foot Ankle Clin. 2012;17:337–49. doi: 10.1016/j.fcl.2012.03.010. [DOI] [PubMed] [Google Scholar]
- 27.Needleman RL. Current topic review: subtalar arthroereisis for correction of flexible flatfoot. Foot Ankle Int. 2005;26:336–46. doi: 10.1177/107110070502600411. [DOI] [PubMed] [Google Scholar]
- 28.Zaret DI, Myerson MS. Arthroereisis of the subtalar joint. Foot Ankle Clin. 2003;8:605–17. doi: 10.1016/S1083-7515(03)00041-X. [DOI] [PubMed] [Google Scholar]
- 29.Silfverskiold N. Reduction of the uncrossed two-joints muscles of the leg to one-joint muscles in spastic conditions. Acta Chir Scand. 1924;56:315–28. [Google Scholar]
- 30.Dreher T, Buccoliero T, Wolf SI, Heitzmann D, Gantz S, Braatz F, et al. Long-term results after gastrocnemius-soleus intramuscular aponeurotic recession as a part of multilevel surgery in spastic diplegic cerebral palsy. J Bone Joint Surg Am. 2012;94:627–37. [DOI] [PubMed]
- 31.Niki H, Hirano T, Okada H, Beppu M. Outcome of medial displacement calcaneal osteotomy for correction of adult-acquired flatfoot. Foot Ankle Int. 2012;33:940–6. doi: 10.3113/FAI.2012.0940. [DOI] [PubMed] [Google Scholar]
- 32.Lutz M, Myerson MS. Radiographic analysis of an opening wedge osteotomy of the medial cuneiform. Foot Ankle Int. 2011;32:278–87. doi: 10.3113/FAI.2011.0278. [DOI] [PubMed] [Google Scholar]
- 33.Hirose CB, Johnson JE. Plantarflexion opening wedge medial cuneiform osteotomy for correction of fixed forefoot varus associated with flatfoot deformity. Foot Ankle Int. 2004;25:568–74. doi: 10.1177/107110070402500810. [DOI] [PubMed] [Google Scholar]
- 34.McCormick JJ, Johnson JE. Medial column procedures in the correction of adult acquired flatfoot deformity. Foot Ankle Clin. 2012;17:283–98. doi: 10.1016/j.fcl.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 35.Tellisi N, Lobo M, O'Malley M, Kennedy JG, Elliott AJ, Deland JT. Functional outcome after surgical reconstruction of posterior tibial tendon insufficiency in patients under 50 years. Foot Ankle Int. 2008;29:1179–83. [DOI] [PubMed]
- 36.• Oh I, Williams BR, Ellis SJ, Kwon DJ, Deland JT. Reconstruction of the symptomatic idiopathic flatfoot in adolescents and young adults. Foot Ankle Int. 2011;32:225–32. Reconstruction with combined medializing calcaneal osteotomy and lateral column lengthening in 16 patients achieved a reduction of pain and improved functional outcome including the ability to participate in sporting activities. [DOI] [PubMed]
- 37.Kou JX, Balasubramaniam M, Kippe M, Fortin PT. Functional results of posterior tibial tendon reconstruction, calcaneal osteotomy, and gastrocnemius recession. Foot Ankle Int. 2012;33:602–11. doi: 10.3113/FAI.2012.0602. [DOI] [PubMed] [Google Scholar]
- 38.Hiller L, Pinney SJ. Surgical treatment of acquired adult flatfoot deformity: what is the state of practice among academic foot and ankle surgeons in 2002? Foot Ankle Int. 2003;24:701–5. doi: 10.1177/107110070302400909. [DOI] [PubMed] [Google Scholar]
- 39.Moseir-LaClair S, Pomeroy G, Manoli A., II Intermediate follow-up on the double osteotomy and tendon transfer procedure for stage II posterior tibial tendon insufficiency. Foot Ankle Int. 2001;22:283–91. doi: 10.1177/107110070102200403. [DOI] [PubMed] [Google Scholar]
- 40.Deland JT, Otis JC, Lee KT, Kenneally SM. Lateral column lengthening with calcaneocuboid fusion: range of motion in the triple joint complex. Foot Ankle Int. 1995;16:729–33. doi: 10.1177/107110079501601111. [DOI] [PubMed] [Google Scholar]
- 41.Thomas RL, Wells BC, Garrison RL, Prada SA. Preliminary results comparing 2 methods of lateral column lengthening. Foot Ankle Int. 2001;22:107–19. doi: 10.1177/107110070102200205. [DOI] [PubMed] [Google Scholar]
- 42.Roche AJ, Calder JD. Lateral column lengthening osteotomies. Foot Ankle Clin. 2012;17:259–70. doi: 10.1016/j.fcl.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 43.•• Ellis SJ, Williams BR, Garg R, Campbell G, Pavlov H, Deland JT. Incidence of plantar lateral foot pain before and after the use of trial metal wedges in lateral column lengthening. Foot Ankle Int. 2011;32:665–73. Incidence of planter lateral foot pain after LCL was assessed in 122 patients after flatfoot reconstruction. The use of trial metal wedges, to judge eversion stiffness and position of the foot intraoperatively, reduced the incidence of pain from 14.7% to 6.3%. [DOI] [PubMed]
- 44.Momberger N, Morgan JM, Bachus KN, West JR. Calcaneocuboid joint pressure after lateral column lengthening in a cadaveric planovalgus deformity model. Foot Ankle Int. 2000;21:730–5. doi: 10.1177/107110070002100903. [DOI] [PubMed] [Google Scholar]
- 45.Ellis SJ, Yu JC, Johnson AH, Elliott A, O'Malley M, Deland J. Plantar pressures in patients with and without lateral foot pain after lateral column lengthening. J Bone Joint Surg Am. 2010;92:81–91. [DOI] [PubMed]
- 46.Vander Griend RA. Lateral column lengthening using a “Z” osteotomy of the calcaneus. Tech Foot Ankle Surg. 20087;257–63.
- 47.Vosseller JT, Roberts M, O'Malley MJ, et al. Autograft vs allograft in lateral column lengthening for adult acquired flatfoot deformity. Presented at the AAOS 2011 Annual Meeting San Diego – Foot and Ankle Session, Podium No: 102. February 16, 2011.
- 48.Astion DJ, Deland JT, Otis JC, Kenneally S. Motion of the hindfoot after simulated arthrodesis. J Bone Joint Surg Am. 1997;79:241–6. doi: 10.2106/00004623-199702000-00012. [DOI] [PubMed] [Google Scholar]
- 49.Deland JT. Spring ligament complex and flatfoot deformity: curse or blessing? Foot Ankle Int. 2012;33:239–43. doi: 10.3113/FAI.2012.0239. [DOI] [PubMed] [Google Scholar]
- 50.Williams BR, Ellis SJ, Deyer TW, Pavlov H, Deland JT. Reconstruction of the spring ligament using a peroneus longus autograft tendon transfer. Foot Ankle Int. 2010;31:567–77. doi: 10.3113/FAI.2010.0567. [DOI] [PubMed] [Google Scholar]
- 51.Sammarco VJ, Magur EG, Sammarco GJ, Bagwe MR. Arthrodesis of the subtalar and talonavicular joints for correction of symptomatic hindfoot malalignment. Foot Ankle Int. 2006;27:661–6. doi: 10.1177/107110070602700901. [DOI] [PubMed] [Google Scholar]
- 52.Jeng CL, Tankson CJ, Myerson MS. The single medial approach to triple arthrodesis: a cadaver study. Foot Ankle Int. 2006;27:1122–5. [PubMed] [Google Scholar]
- 53.Anand P, Nunley JA, DeOrio JK. Single-incision medial approach for double arthrodesis of hindfoot in posterior tibialis tendon dysfunction. Foot Ankle Int. 2013;34:338–44. doi: 10.1177/1071100712468564. [DOI] [PubMed] [Google Scholar]
- 54.Funk DA, Cass JR, Johnson KA. Acquired adult flatfoot secondary to posterior tibial-tendon pathology. J Bone Joint Surg Am. 1986;68(1):95–102. [PubMed] [Google Scholar]
- 55.Deland JT, de Asla RJ, Segal A. Reconstruction of the chronically failed deltoid ligament: a new technique. Foot Ankle Int. 2004;25:795–9. doi: 10.1177/107110070402501107. [DOI] [PubMed] [Google Scholar]
- 56.• Ellis SJ, Williams BR, Wagshul AD, Pavlov H, Deland JT. Deltoid ligament reconstruction with peroneus longus autograft in flatfoot deformity. Foot Ankle Int. 2010;31:781–9. Five patients with stage IV flatfoot underwent deltoid ligament reconstruction using a peroneus longus tendon transfer. The technique was useful for reducing tibiotalar tilt. Correction and function were maintained at intermediate-term follow-up. [DOI] [PubMed]
- 57.Boyer MI, Bowen V, Weiler P. Reconstruction of a severe grinding injury to the medial malleolus and the deltoid ligament of the ankle using a free plantaris tendon graft and vascularized gracilis free muscle transfer: a case report. J Trauma. 1994;36:454–7. doi: 10.1097/00005373-199403000-00042. [DOI] [PubMed] [Google Scholar]
- 58.McCormack AP, Ching RP, Sangeorzan BJ. Biomechanics of procedures used in adult flatfoot deformity. Foot Ankle Clin. 2001;6:15–23. doi: 10.1016/S1083-7515(03)00072-X. [DOI] [PubMed] [Google Scholar]
- 59.Haddad SL, Dedhia S, Ren Y, Rotstein J, Zhang LQ. Deltoid ligament reconstruction: a novel technique with biomechanical analysis. Foot Ankle Int. 2010;31:639–51. [DOI] [PubMed]
- 60.Jeng CL, Bluman EM, Myerson MS. Minimally invasive deltoid ligament reconstruction for stage IV flatfoot deformity. Foot Ankle Int. 2011;32:21–30. doi: 10.3113/FAI.2011.0021. [DOI] [PubMed] [Google Scholar]
- 61.Ketz J, Myerson M, Sanders R. The salvage of complex hindfoot problems with use of a custom talar total ankle prosthesis. J Bone Joint Surg Am. 2012;94:1194–2000. doi: 10.2106/JBJS.K.00421. [DOI] [PubMed] [Google Scholar]
- 62.Strasser NL, Turner NS. Functional outcomes after ankle arthrodesis in elderly patients. Foot Ankle Int. 2012;33:699–703. doi: 10.3113/FAI.2012.0699. [DOI] [PubMed] [Google Scholar]


