Abstract
Dislocation remains one of the most common complications after total hip arthroplasty, regardless of the surgical approach. While multiple reasons as laxity, implant position, improper implant choice, and impingement etc. might be leading factors for dislocation, an exact identification of the exact reason is of major importance, to plan for a proper surgical or nonsurgical correction. This article describes in detail the definition, etiology, reduction, and possible treatment options for dislocation after primary and revision total hip arthroplasty that are currently used at the Endo Klinik in Hamburg. It furthermore includes a distinct overview of possible surgical treatment options, based on the main pathology leading to dislocation.
Keywords: Dislocation, Surgical approach, Head size, Closed reduction, Open reduction
Introduction
Dislocation after total hip arthroplasty (THA) is the most common early complication following primary implantation [1]. For example, the Swedish Hip Arthroplasty Register has tracked the number of dislocations until the year 2000, which has clearly shown that dislocation, in both cemented and uncemented THA, is considered to be the number 1 short-term complication requiring a reoperation within the first 2 years [2].
The incidence of dislocation after primary THA is reported from 0.2%–1.7%; the Swedish nation-wide mean rate is reported to be 0.6% [2, 3•]. At THA revision, the reported revision rate because of dislocation can be 10-fold higher [4, 5].
The posterior approach seems to be at higher risk for dislocation and possible early reoperation, despite all of its advantages [6].
Definition
The articulation of the prosthetic head and the acetabular liner allow for a range of motion nearly close to that of the physiologic values of the intact anatomic hip. Dislocation occurs if the head moves out of the acetabular component for any reason. In 75% of the cases, the prosthetic head dislocates posteriorly.
Typical clinical signs of dislocation include leg shortening with either external or internal rotation, in combination with a pathologic and painful telescoping of the limb. Often, the patients report a sudden onset of pain with a kind of snapping feeling, followed by being unable to walk or load the affected leg. Conventional radiographs or physical examination under fluoroscopy is usually needed for an accurate documentation after dislocation.
Localization of dislocation
Posterior dislocation occurs in flexion-adduction and internal rotation of the hip. The anterior aspect of the implant neck impinges with the anterior acetabular rim, and the head dislocates from the socket. After a posterior approach, the capsule and the short external rotators are weakened or damaged, facilitating a posterior dislocation [7]. Theoretically, the leg is internally rotated and shortened because of the entrapment of the head behind the acetabulum, being unable to rotate externally. This is usually associated with a relevant shortening and external rotation of the limb.
Anterior dislocation occurs if the hip is extended, adducted, and externally rotated. Soft tissue impingement or osteophytes at the posterior aspect of the joint along with absence or weakening of the anterior capsule may lead to anterior dislocation, which is more frequently associated with any anterior approach to the hip joint.
Etiology
Laxity of the hip joint for any reason is the most obvious factor leading to a dislocation. Shortening of the original neck length by improper choice of the head-neck length ratio is one of the reasons, but this technical error occurs quite infrequently [8]. Post-traumatic hips are more likely to dislocate even after proper implantation [6]. In revision cases, it is more common that soft tissue tension gradually decreases within the first weeks after operation even after proper restoration of the center of rotation [3•]. Intraoperative assessment of the tension by telescoping of the femoral stem is a common method; however, the influence of anesthetic relaxation of the patient makes this somewhat unreliable.
The most common mechanism of dislocation is impingement. Osteophytes on both the acetabular or femoral side, capsular tissue, or scar tissue can cause a dislocation displacing the head to posterior or anterior. The femur becomes proximalized by the force of the abductors and adductors. This might also be called positional dislocation because the patient moves the leg into an insecure position, outside of the safe range for a total hip replacement, especially during the first month after implantation.
Technical errors such as malpositioning of the components are noted to be a common cause of dislocation [1, 5, 9–11]. High inclination of the acetabular component (acetabular abduction angle) of more than 60° can reduce superior coverage of the prosthetic head, whereas inclination below 30° can lead to lateral impingement in abduction and flexion. A retroverted or neutral cup does not provide stability when the patient is sitting or flexing the hip predisposing to posterior dislocation. Increased anteversion of the socket makes it possible to impinge at the posterior margin resulting in anterior dislocation. The effect of orientation of the acetabular component in correlation with dislocation is discussed in recent papers [1, 12]. The version of the femoral component (antetorsion) is also an important factor for proper hip stability. Over-antetorsion can lead to posterior impingement and anterior instability, and retrotorsion can lead to anterior impingement and posterior instability.
Neuromuscular disorders with pathologically increased muscle tension such as Parkinson’s disease, cerebral palsy, and epilepsy represent a higher risk for dislocation after THA [3•, 13]. Surgeons must be mindful of these disorders when considering patients for hip replacement and may consequently consider the use of a constrained coupling mechanism or a dual mobility design of socket. Another reason for dislocation can be any traumatic displacement [3•] of the hip with or without associated fracture. Excessive alcohol consumption or extreme obesity may facilitate this condition.
In developmental dysplasia of the hip (DDH), the anatomy and biomechanics of the hip are different from the normal hip. Shortening of the iliopsoas tendon, weakness of the gluteus medius muscle, and the anatomical position of the greater trochanter are factors that may cause dislocation even after proper positioning of the implants.
In a recent study, Hailer et al. stated that after analyzing more than 70,000 hip implantations in Norway, patients with femoral neck fracture or osteonecrosis of the femoral head are at a higher risk of dislocation [3•]. Use of the minimally invasive and posterior approaches also increases this risk.
In revision surgery, there are multiple factors influencing the stability of the hip. Scar tissue formation, weakness of the gluteal muscles including palsy of the gluteus medius, the need for resection of the proximal femur, or bone defect of the greater trochanter are conditions to deal with, representing a surgical challenge in order to avoid postoperative dislocation. Use of larger head diameters (36 or 40 mm) is suggested to lower the risk [6, 9, 14, 15].
Position of the implants
The ‘safe zone’ of the acetabular component was described by Lewinnek with 40° of inclination and 15° of anteversion ±10°. It has been shown that values outside this range have a higher risk for implant dislocation to occur [16].
Increased cup inclination, leads to a more “open” socket position, thus the cranial buttress for the femoral head might be less sufficient—less offset stability is given and the femoral head is more likely to lever the liner to superior. The maximum safe inclination is dependent on the cup design, but more than 60° has been shown to be related to increased dislocation rates. Intraoperative anatomical landmarks, that might be used are the anterior inferior iliac spine and the incisura of acetabulum, an imaginary line between these 2 structures has an angle of 40°–45° to the horizontal axis, if anatomy is normal [1, 12].
Anteversion follows the natural position of the acetabulum, represented by the transverse acetabular ligament [17]. Less anteversion means less stability when the patient is sitting and adducting the leg while internally rotating; this occurs quite often in daily life. When a posterior approach is used, meticulous attention is required to achieve correct anteversion in order to avoid posterior dislocation. Similarly, using an anterior approach, extensive anteversion should be avoided to reduce the risk of anterior dislocation [1].
The antetorsion of the stem has to follow the natural rotation of the proximal femur of approximately 15° ± 5° to the transepicondylar axis of the knee. The proper alignment of the stem is often not a surgical challenge, therefore, relatively rarely seen as a mayor reason of dislocation.
The most important aspect is the ‘combined anteversion’ of the implants. In THA combined anteversion (ie, the sum of cup anteversion and stem antetorsion) are used as parameters to assess the appropriateness of overall prosthetic alignment [5, 10, 11, 18]. Intraoperatively, an “equator test” can be performed as suggested by Ranawat and the phenomenon is observed when the leg is in neutral position (the hip is fully extended) and 45° internally rotated: if the head is observed to be coplanar with the socket then the combined anteversion is 45° [8].
Widmer has defined a ‘mathematic’ recommendation for positioning of the components [18]; the articulating hemispheric surface of the acetabular cup should be oriented between 40°–45° of radiographic inclination, between 20°–28° of anteversion (AV), and should be combined with stem antetorsion so that the sum of cup anteversion plus 0.7 times the stem antetorsion (AT) equals 37° [AV + 0.7AT = 37°].
Head diameter
Smaller head diameters (22–28 mm) tend to have optimal wear characteristics but are more likely to dislocate [2]. Head sizes above 28 mm are considered to be safer because of a favorable head-neck ratio and a larger “jump distance.” At primary THA, larger head diameters (28–32 mm) are widely used. In acetabular cup sizes beyond 56 mm, head diameter of 36 mm is recommended by some authors [14]. In revision cases, head diameters of 36–40 mm may be used to reduce the risk of dislocation [15]. Larger head sizes are associated with a lower dislocation risk, however, the potential for greater polyethylene wear secondary to the increased sliding distance must be considered [19•].
Dislocation treatment
Closed reduction
Dislocation of THA is a painful condition; patients are usually unable to walk. Closed reduction is carried out as soon as possible after diagnosis to avoid neurologic injury [20]. Optimally, general anesthesia and fluoroscopy are required, and commonly, 2 surgeons are required to safely perform the reduction maneuver [21]. Before the procedure, the mechanism and reason for dislocation should be analyzed. The various methods of closed reduction are described below [22–25].
Anterior dislocation
To reduce an anterior dislocation the pelvis is stabilized by 2 hands of 1 surgeon on the fluoroscopy table or bed, while the second surgeon pulls the dislocated leg along the longitudinal axis and rotates internally. The prosthetic head than returns into the acetabular liner.
Posterior dislocation
To reduce a posterior dislocation the pelvis is similarly stabilized by 2 hands, the surgeon holds the adducted and internally rotated thigh and the hip is flexed above 90°. Then the surgeon brings the femoral head near the posteroinferior rim of the acetabulum while traction is maintained, and the prosthetic head is levered into the liner by abduction, external rotation, and extension of hip (Bigelow’s maneuver [24]). A snap is normally felt by the person stabilizing the pelvis.
Another technique for reducing a posterior dislocation is described in the Rochester Method [24] or Tulsa Technique [26]. The patient is placed supine with the uninjured hip and knee flexed. One of the surgeon’s hands is placed underneath the injured knee and over top of the uninjured knee; this knee acts as a pivot point for the surgeon’s hand. The patient’s injured hip and knee are flexed, the other hand of the surgeon grabs the ankle of the injured side and applies gradually traction, and at the same time, the ankle can be used to rotate the hip.
Open reduction
If closed reduction fails or re-dislocation occurs within several days after the reduction, open reduction is to be considered [27]. Before surgery, all possible reason(s) for the dislocation should be identified and the proper treatment option should be chosen. If dislocation with massive hematoma formation and/or palsy of the femoral or sciatic nerve occurs, open reduction is mandatory within several hours. At open surgery, the fluid or hematoma is removed to decrease the joint tension. The membrane in and around the joint is debrided to encourage the soft tissues to form a new pseudocapsule which provides more stability. A posterior soft tissue repair is considered and carried out if possible to prevent the joint from re-dislocating. Possible surgical treatment options are listed in Figs. 1 and 2, Table I.
Fig. 1.
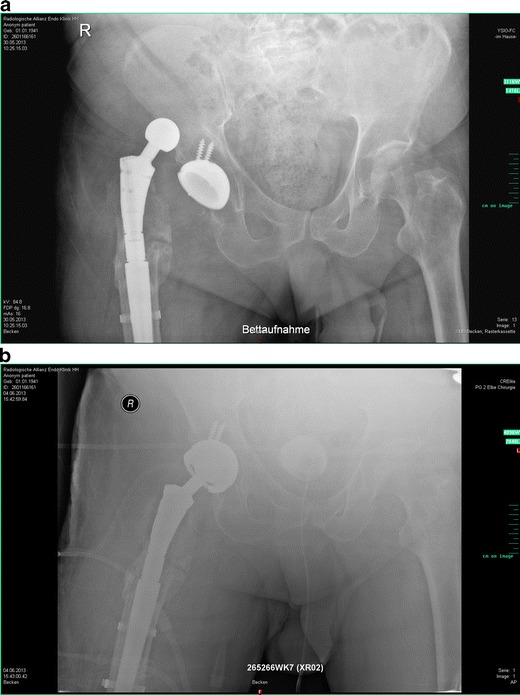
A + B. Patient with massive osteolysis of the right proximal femur with modular THA (A). Due to recurrent dislocation constrained acetabular liner was inserted to achieve stability (B).
Fig. 2.
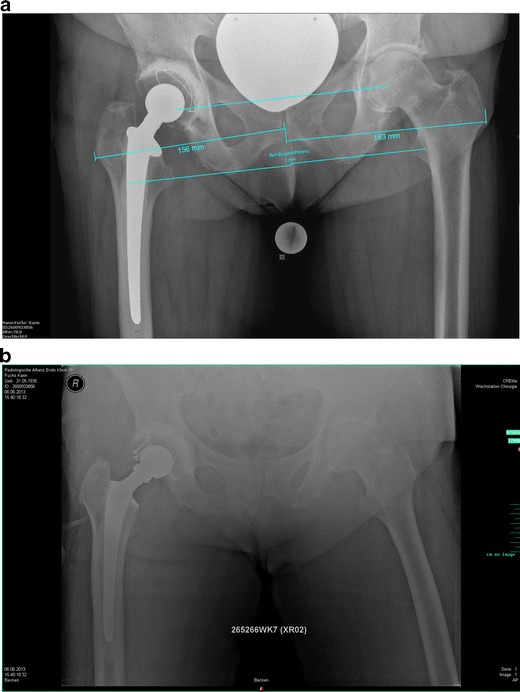
A+ B. Patient with recurrent dislocation: measurements (A) reveal a decreased offset right (156 mm) vs left (163 mm) site. The inclination of the cup was 53°, within the safe zone. At open reduction (B) a retainment ring and an offset head were implanted for correction.
Table I.
Possible surgical treatment options at dislocation of THA
| Reason for Dislocation | Treatment option |
|---|---|
| Shortening, laxity | Head exchange (consider offset head) |
| Anteversion low | Dorsal retainment ring |
| Cup inclination high | Cranial retainment ring or cup exchange |
| Cup in retroversion | Cup exchange |
| Anterior impingement | Remove osteophytes and scar tissue, longer head |
| Anteversion high | Cup exchange or offset head |
| Cup horizontal, impingement in flexion | Cup exchange |
| Multidirectional instability | Bipolar hypermobility cup or constrained cup with head exchange |
| Deficient abductors | Constrained cup or bipolar hypermobility cup |
Prevention of dislocation
The best option to ‘treat’ THA dislocation is to prevent the occurrence in the first instance [7]. Using a posterior approach, the general repair of the posterior structures capsule and external rotators (piriformis tendon) with nonabsorbable sutures is a valuable option but not always possible to carry out. At final reduction, with the trial heads one should perform the dislocation tests, the equator test, and check for telescoping of the components. Appropriate head size and length are to be chosen. In case of instability, a retainment ring can provide more stability and can be a good option. In addition, most implant companies now offer lipped (ie, dorsal rim) poly-liner options. At preoperative planning, the center of rotation should be determined and during the surgery restored to fulfill the biomechanical environment of the hip. After implantation of THA in early postoperative period, abduction cushions may be used to prevent the patient from adducting the operated leg.
In case of revisions with loss of the greater trochanter or insufficient gluteus medius, or after resection of the proximal femur (eg, in septic surgery) a dual mobility cup [28] or a constrained cup [6] should be considered. The dual mobility cup consists of a metal shell that encloses a movable polyethylene liner. The femoral head (diameter 22 or 28 mm) is encased by the hemispheric liner so that it also allows rotation of the femoral head within the polyethylene sphere. The polyethylene casing can articulate partly against the metal casing and partly against the femoral head fixed on the stem. The concept differentiates from the constrained liner used for uncemented cups. In this implant, the insert is rigidly fixed to the metal shell while the liner in the dual mobility cup can also articulate with the metal shell. From a biomechanical perspective, a dual mobility system should have advantages compared with a constrained liner because extreme movements are not translated to a shear force at the cup-bone interface [6, 28].
Patient education
Before primary THA, patients should be educated as to what range of motion is to be expected after the implantation and what movements and actions are to be avoided to prevent dislocation, especially in the early postoperative phase. Adduction and internal rotation after posterior approach is avoided for at least 3 months. After anterior approach adduction, external rotation and hyperextension are avoided for 6–12 weeks. In both cases, patient should refrain from deep sitting with the hips flexed above 90°.
Post-dislocation treatment
After closed reduction, 24 hours of rest is recommended, followed by gradual mobilization under the supervision of a physiotherapist. Normally, full weight bearing can be allowed, unless the soft tissues are painful. Crutches are normally required. In recurrent cases or in non-compliant patients, a brace can be applied with restriction of the range of motion of the injured hip. Adduction, flexion over 90°, and rotation of the hip is limited by the brace for 6 weeks. Then, gradually increase each motion modality, but adduction and internal rotation should be avoided for 3 months. After this period of time, strengthening of the pelvicrural muscles, especially the gluteal muscles, can be emphasized. Home trainer and swimming are advantageous for muscle training, of course under the guidance of a trained physiotherapist.
Conclusions
Dislocation remains a mayor complication after THA. While multiple reasons may be contributing factors leading to dislocation, a precise identification of the exact reason is of major importance, to plan for a proper surgical or non-surgical correction. Based on the identified pathology, in most cases a closed reduction can be performed. Operative revision scenarios are based most often on the achieved implant orientation or soft tissue laxity after primary implantation.
Acknowledgments
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Akos Zahar declares that he has no conflict of interest. Amit Rastogi declares that he has no conflict of interest. Daniel Kendoff declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stöckl B. Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Joint Surg Br. 2005;87:762–9. doi: 10.1302/0301-620X.87B6.14745. [DOI] [PubMed] [Google Scholar]
- 2.Swedish Hip Arthroplasty Register, Annual Report 2011, http://www.shpr.se.
- 3.Hailer NP, Weiss RJ, Stark A, Kärrholm J. The risk of revision due to dislocation after total hip arthroplasty depends on surgical approach, femoral head size, sex, and primary diagnosis. An analysis of 78,098 operations in the Swedish Hip Arthroplasty Register. Acta Orthop. 2012;83:442–8. doi: 10.3109/17453674.2012.733919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Devane PA, Wraighte PJ, Ong DC, Horne JG. Do joint registries report true rates of hip dislocation? Clin Orthop Relat Res. 2012;470:3003–6. doi: 10.1007/s11999-012-2323-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moskal JT, Capps SG. Acetabular component positioning in total hip arthroplasty: an evidence-based analysis. J Arthroplasty. 2011;26:1432–7. doi: 10.1016/j.arth.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 6.Sikes CV, Lai LP, Schreiber M, Mont MA, Jinnah RH, Seyler TM. Instability after total hip arthroplasty: treatment with large femoral heads vs constrained liners. J Arthroplasty. 2008;23(7 Suppl):59–63. doi: 10.1016/j.arth.2008.06.032. [DOI] [PubMed] [Google Scholar]
- 7.Patel PD, Potts A, Froimson MI. The dislocating hip arthroplasty: prevention and treatment. J Arthroplasty. 2007;22(4 Suppl 1):86–90. doi: 10.1016/j.arth.2006.12.111. [DOI] [PubMed] [Google Scholar]
- 8.Ranawat CS, Rao RR, Rodriguez JA, Bhende HS. Correction of limb-length inequality during total hip arthroplasty. J Arthroplasty. 2001;16:715–20. doi: 10.1054/arth.2001.24442. [DOI] [PubMed] [Google Scholar]
- 9.Amstutz HC, Le Duff MJ, Beaule PE. Prevention and treatment of dislocation after total hip replacement using large diameter balls. Clin Orthop Relat Res. 2004;108. [DOI] [PubMed]
- 10.Amuwa C, Dorr LD. The combined anteversion technique for acetabular component anteversion. J Arthroplasty. 2008;23:1068. doi: 10.1016/j.arth.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 11.Fukunishi S, Fukui T, Nishio S, Fujihara Y, Okahisa S, Yoshiya S. Combined anteversion of the total hip arthroplasty implanted with image-free cup navigation and without stem navigation. Orthop Rev. 2012;4:e33. doi: 10.4081/or.2012.e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meftah M, Yadav A, Wong AC, Ranawat AS, Ranawat CS. A novel method for accurate and reproducible functional cup positioning in total hip arthroplasty. J Arthroplasty. 2013;28:1200–5. doi: 10.1016/j.arth.2012.09.018. [DOI] [PubMed] [Google Scholar]
- 13.Queally JM, Abdulkarim A, Mulhall KJ. Total hip replacement in patients with neurological conditions. J Bone Joint Surg Br. 2009;91:1267–73. doi: 10.1302/0301-620X.91B10.22934. [DOI] [PubMed] [Google Scholar]
- 14.Peters CL, McPherson E, Jackson JD, et al. Reduction in early dislocation rate with large-diameter femoral heads in primary total hip arthroplasty. J Arthroplasty. 2007;22(6 Suppl 2):140. doi: 10.1016/j.arth.2007.04.019. [DOI] [PubMed] [Google Scholar]
- 15.Rodriguez JA, Rathod PA. Large diameter heads: is bigger always better? J Bone Joint Surg Br. 2012;94(11 Suppl A):52–4. doi: 10.1302/0301-620X.94B11.30508. [DOI] [PubMed] [Google Scholar]
- 16.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–20. [PubMed] [Google Scholar]
- 17.Archbold HAP, Mockford B, Molloy D, et al. The transverse acetabular ligament, an aid to acetabular component placement during total hip arthroplasty. J Bone Joint Surg Br. 2006;88:883. doi: 10.1302/0301-620X.88B7.17577. [DOI] [PubMed] [Google Scholar]
- 18.Widmer KH, Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22:815–21. doi: 10.1016/j.orthres.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 19.Garbuz DS, Masri BA, Duncan CP, Greidanus NV, Bohm ER, Petrak MJ, et al. The Frank Stinchfield Award: dislocation in revision THA: do large heads (36 and 40 mm) result in reduced dislocation rates in a randomized clinical trial? Clin Orthop Relat Res. 2012;470:351–6. doi: 10.1007/s11999-011-2146-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gaines RJ, Hardenbrook M. Closed reduction of a dislocated total hip arthroplasty with a constrained acetabular component. Am J Orthop. 2009;38:523–5. [PubMed] [Google Scholar]
- 21.Schafer SJ, Anglen JO. The East Baltimore Lift: a simple and effective method for reduction of posterior hip dislocations. J Orthop Trauma. 1999;13:56–7. doi: 10.1097/00005131-199901000-00013. [DOI] [PubMed] [Google Scholar]
- 22.Amstutz HC, Kody MH. Dislocation and subluxation. In Amstutz HC, editor. Hip arthroplasty. Churchill Livingstone, New York; 1991.
- 23.DeLee JC. Fracture and dislocation of the hip. In Rockwood CA, Green DP, Bucholz RW, editors. Fractures in adults. 3rd edition. JB Lippincott, Philadelphia; 1991.
- 24.Wheeless CR. Dislocations and fracture dislocations of the hip. In: Wheeless’ Textbook of Orthopaedics (on line), www.wheelessonline.com.
- 25.Skoff HD. Posterior hip dislocation, a new technique for reduction. Orthop Rev. 1986;15:405–9. [PubMed] [Google Scholar]
- 26.Vosburgh CL, Vosburgh JB. Closed reduction for total hip arthroplasty dislocation. The Tulsa Technique. J Arthroplasty. 1995;10:693–4. doi: 10.1016/S0883-5403(05)80218-9. [DOI] [PubMed] [Google Scholar]
- 27.Bourne RB, Mehin R. The dislocating hip: what to do, what to do. J Arthroplasty. 2004;19(4 Suppl 1):111–4. doi: 10.1016/j.arth.2004.02.016. [DOI] [PubMed] [Google Scholar]
- 28.Grazioli A, Ek ET, Rüdiger HA. Biomechanical concept and clinical outcome of dual mobility cups. Int Orthop. 2012;36:2411–8. doi: 10.1007/s00264-012-1678-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


