Abstract
When considering the management of shoulder anterior instability with glenoid bone loss ≥25 % of the inferior glenoid diameter (inverted-pear glenoid), the consensus among recent authors is that glenoid bone grafting should be done. Although the engaging Hill-Sachs lesion has been recognized as a risk factor for recurrent anterior instability, there has been no generally accepted methodology for quantifying the Hill-Sachs lesion taking into account the geometric interplay of various sizes and various orientations of bipolar (humeral-sided plus glenoid-sided) bone loss. Keeping the glenoid track concept in mind, if a Hill-Sachs lesion engages the anterior glenoid rim, with or without concomitant anterior glenoid bone loss, it is possible to manage this pathology, reducing the risk of recurrent shoulder instability after surgery. If the Hill-Sachs engages, “Remplissage” or “Latarjet” surgical procedures are indicated depending of glenoid bone loss.
Electronic supplementary material
The online version of this article (doi:10.1007/s12178-013-9194-7) contains supplementary material, which is available to authorized users.
Keywords: Shoulder instability, Humeral bone deficit, Hill-Sachs lesion, Glenoid track, Remplissage procedure
Introduction
It is generally accepted that anteroinferior glenoid bone loss comprising ≥25 % of the inferior glenoid diameter must be addressed by glenoid bone grafting, using a coracoid graft (Latarjet procedure), iliac graft, or allograft. However, there are no clear guidelines as to how to address patients with bipolar lesions who have varying degrees of bone loss of the glenoid as well as the proximal humerus (Hill-Sachs defects). The geometric interplay of these bipolar lesions can be subtle, yet it is critical to understand the pathologic importance of this interplay in developing logical criteria for their surgical treatment.
Biomechanical and anatomical considerations
It is essential to define the role that the anteroinferior labrum and the bone play in distributing forces across the gleno-labral complex during compressive loads, thus guaranteeing an adequate amount of intrinsic stability. It is demonstrated that the progressive labral and bone loss reduced the articular contact area and increased the pressure across the glenohumeral joint under compression loads.
Since progressive bone loss in the anteroinferior quadrant has the effect of causing further increases in mean contact pressure and peak pressure as well as a decrease in contact area, an isolated soft tissue (Bankart) repair without bone graft in a patient with significant glenoid bone loss would have to resist this overload at the bone-soft tissue repair interface. This overload at the repair site would increase the likelihood of failure of the repair. In recent years, efforts have been made to identify the morphology, extent, location, and interaction of the bone losses that, if not restored, may potentially compromise surgical outcome expectations.
Burkhart and De Beer [1••] recognized that one of the risk factors for failure of arthroscopic stabilization was based on the anatomic relationship of the bone loss affecting the humeral head and the glenoid in critical positions. In fact, they introduced the concept of “significant bone loss.”
They defined a significant glenoid bone defect as one in which the arthroscopic appearance of the glenoid when viewed from a superior-to-inferior perspective was an inverted pear. On the humeral side, they defined a significant bone defect to be an engaging Hill-Sachs lesion, oriented in such a way that it engaged the anterior glenoid in a position of athletic function (90° abduction combined with external rotation of approximately 90°). The authors found that the instabilities associated with “engaging type” Hill-Sachs lesions were at high risk for recurrence if treated with the classic arthroscopic capsuloligament repair, confirming that the restoration of the soft tissues alone would not be sufficient to contain the humeral head under stress. The authors emphasized the role of arthroscopy as a dynamic diagnostic tool that was essential in identifying the bone lesions “at risk” so that the surgeon could restore both the anatomy and the biomechanical function of the damaged structures.3 They reported that most arthroscopic repair failures have resulted from traumatic bone defects on either the glenoid or humeral side, and that the underlying cause of failure was not inadequate soft tissue fixation, but rather traumatic bone deficiency. After these considerations, more orthopedic surgeons reconsider the merits of certain more classical surgical techniques [2••].
According to recent papers [2••], we think that there is no simple method available to identify patients who will develop recurrent instability after arthroscopic Bankart procedure and who would be better served by an open operation. In fact, it is important to consider more factors to avoid surgical failure: age of patient at the time of surgery; involvement in competitive or contact sports, or sports involving vigorous overhead activity; shoulder hyperlaxity; and, radiographically identifiable bone defects (a Hill-Sachs lesion on the anteroposterior radiograph of the shoulder in external rotation and/or loss of the sclerotic inferior glenoid border).
Itoi and associates [3••] examined the exact anatomic relationship between the humeral head and theglenoid in various critical positions, when all the anterior soft-tissue structures were preserved. This investigation was a prelude to the critically important concept of the “glenoid track.”
The glenoid track: its relationship to engaging and nonengaging Hill-Sachs lesions
Itoi and associates introduced the concept of the “glenoid track.” Using 3D CT scans, they identified bipolar bone losses that, interacting in different dynamic patterns in abduction and external rotation [3••] 3, may require treatment with bone graft. The authors clarified the contact area of the humeral head and the glenoid from the standpoint of shoulder dislocation. They demonstrated that, as the arm was raised, the glenoid contact area shifted from the inferomedial to the superolateral portion of the posterior articular surface of the humeral head, creating a zone of contact between the glenoid and the humeral head. They defined this contact zone as the glenoid track. An intact glenoid track, without significant bone loss, guarantees bone stability. The distance from the medial margin of the contact area to the medial margin of the rotator cuff attachment onto the humerus was 18.4 ± 2.5 mm or 84 % ± 14 % of the glenoid width with the arm at 60° of abduction to the scapula or 90° of abduction to the trunk [3••]. Omori and colleagues measured the width of the glenoid track in live shoulders [4••]. In this preliminary study using a semi-dynamic method, they reported that the glenoid track width with the arm at 90° of abduction was 85 % ± 12 % of the glenoid width. More recently, they compiled the data of 30 volunteers and concluded that the glenoid track width was 83 % ± 12 % (unpublished data). In this article, we use this most recent value of 83 % obtained in live shoulders. The integrity of the glenoid track and the location of the Hill-Sachs lesion with respect to the medial margin of the glenoid track become essential in identifying those bipolar bone lesions at risk where standard stabilization procedures such as Bankart repair are being considered. We believe that the definition of engaging vs non-engaging Hill-Sachs lesions, although still very important in distinguishing significant loss, is in need of clarification in terms of how these lesions relate to the glenoid track.
Burkhart and DeBeer’s concept of engaging vs non-engaging is completely consistent with Yamamoto and Itoi’s concept of the glenoid track. They are complementary concepts in that they both evaluate the interaction of bipolar bone loss during dynamic shoulder function. The presence of an engaging Hill-Sachs lesion can be detected at arthroscopy with the arm in abduction-external rotation, while the glenoid track can be evaluated by either arthroscopy or CT scan. Itoi and Boileau [5, 6] have stated that all bipolar bone lesions are engaging, due to the fact that engagement was required for formation of the Hill-Sachs lesion. In fact, if the exact mechanism and the same traumatic energy of the initial injury were to be reproduced, all bipolar lesions would engage. This concept was reinforced by Kurokawa et al. [7•], who recommended that the glenoid track rather than dynamic intraoperative assessment be used to assess engaging Hill-Sachs lesions. Dynamic intraoperative assessment is almost always performed before repairing the Bankart lesion.
However, this diagnostic technique could potentially cause an over-diagnosis of engaging Hill-Sachs lesions, since ligament insufficiency might permit the humeral head to excessively translate anteriorly, thus facilitating engagement of the humeral defect with the glenoid rim.
Kurokawa et al. [7•] defined the “true engaging Hill-Sachs lesion” as either one that engages after Bankart repair or one that extends over the glenoid track. Based on the latter definition, they reported that in their series of 100 shoulders with recurrent anterior dislocation, 94 shoulders had a Hill-Sachs lesion, and 7 of them (7 %) were defined as having “a true engaging Hill-Sachs lesion.” On the other hand, Parke [8] reported the prevalence of engaging Hill-Sachs lesions using the former definition. They arthroscopically looked for engagement after Bankart repair in 983 shoulders and found that 70 shoulders (7.1 %) showed engagement. It should be emphasized that the prevalence of a true engaging Hill-Sachs lesion using dynamic arthroscopic assessment after Bankart repair is the same as the one assessed with use of the glenoid track concept. It is noteworthy that the prevalence of true engaging Hill-Sachs lesion (7 %) is not as common as previously reported when using only dynamic arthroscopic assessment before Bankart repair (34 %–46 %) [9–11].
Bipolar bone loss: the non-engaging Hill-Sachs lesion vs the engaging Hill-Sachs lesion
Having confirmed the importance of adequate bone as an element of stability, its interpretation and evaluation become essential. As mentioned previously, the dynamic interaction of bipolar bone loss assessed at arthroscopy, before Bankart repair, risks reproducing a situation that is only partially reliable because it does not correspond to the anatomic and biomechanical context of a shoulder with an intact capsuloligamentous complex. On the other hand, evaluating the engagement arthroscopically after completion of an arthroscopic Bankart repair, albeit more correct from the anatomo-functional standpoint, can put the repair at risk by overstressing the newly repaired capsulolabral complex in abduction and external rotation, thus, compromising the repair itself. In essence, these arthroscopic techniques provide qualitative information about Hill-Sachs engagement. However, we now believe that engagement must be quantified in order to be rigorously demonstrated.
It is precisely on this point that Itoi [2••] emphasized quantification of bipolar bone damage. The diagnostic arthroscopic evaluation that is done prior to Bankart repair to evaluate engaging vs nonengaging Hill-Sachs lesions should thus be reconsidered toward a new concept which comprises an evaluation of the glenoid track, including the influence of associated glenoid bone loss, and the role of the location of the Hill-Sachs lesion with respect to the glenoid track itself.
The width of the glenoid track decreases if there is a glenoid bone defect. In order to calculate the width of the glenoid track in a patient with glenoid bone loss, the width of the defect should be subtracted from 83 % of the glenoid width, which is the width of the glenoid track when there is not a glenoid defect. In this way, the bone defects of the glenoid and humeral head can be assessed with regard to each other. If the medial margin of a Hill-Sachs lesion is within the glenoid track, there is bone support adjacent to the Hill-Sachs, and the Hill-Sachs lesion is “nonengaging” (Fig. 1a); if the medial margin of the Hill-Sachs lesion is more medial than the glenoid track there is no bone support, and the Hill-Sachs lesion is “engaging” (Fig. 1b).
Fig. 1.
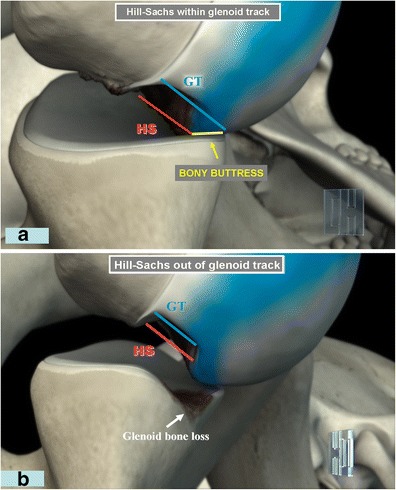
a, Glenohumeral joint in abduction and external rotation. If the Hill-Sachs lesion is within the medial margin of the glenoid track there is still glenoid track support for bone stability (non-engaging Hill-Sachs lesion).This implies that intrinsic stability can be shared between Bankart repair and bone support. b, Glenohumeral joint in abduction and external rotation in shoulder with a glenoid bone loss and a Hill-Sachs lesion (bipolar bone loss). The Hill-Sachs lesion extends medial to the medial margin of the glenoid track, with loss of bone support at the anterior glenoid rim (engaging Hill-Sachs lesion). (GT glenoid track, HS Hill-Sachs)
How to assess engaging or nonengaging Hill-Sachs lesion by means of CT scan: our method
As previously mentioned, the location of the medial margin of the glenoid track is equivalent to 84 % of the glenoid width in cadaveric shoulders [13], and 83 % in live shoulders (unpublished data).
Using this 83 % value as the mean glenoid track width, we will demonstrate how to assess a Hill-Sachs lesion to be engaging or non-engaging. First, we visualize the glenoid and the humeral head using 3D-CT. When we order a unilateral shoulder scanning, a patient is placed in the CT gantry and both shoulders are always placed in the scanning field. With a single scan, the data of both shoulders are recorded regardless of our order of single shoulder scanning. Thus, we can utilize the data of both shoulders whenever we order a single shoulder CT scan. First, we create an en face view of the glenoid. There are various methods to assess the size of the glenoid bony defect: defect length, width-to-length [12], width-to-length ratio [13, 14], glenoid index = defect width/circle diameter [13–15], Pico method = defect area/circle area [16, 17]. We prefer to use the contralateral shoulder as a reference because the difference between the right and left is extremely small. We can reliably use the controlateral glenoid as a reference. We measure the greatest horizontal distance of the glenoid (width) on both shoulders. Using the intact glenoid width as a reference, we calculate the defect size “d” as
 |
Next, using the posterior view of the humeral head, we identify the medial margin of the footprint of the rotator cuff and the Hill-Sachs lesion. Then, we set a line located at a distance equivalent to 83 % of the glenoid width from the medial margin of the rotator cuff footprint.
If there is no bony defect of the glenoid, this line represents the medial margin of the glenoid track (line “G”). If there is a bony defect of the glenoid (d), we subtract the distance “d” from the 83 % line to obtain the medial margin of the true glenoid track. If the Hill-Sachs lesion is located within the glenoid track, we call it a “non-engaging” Hill-Sachs lesion.
If it extends more medially over the medial margin of the glenoid track, we call it an “engaging” Hill-Sachs lesion. It is important to note that there is typically an intact bone bridge between the rotator cuff attachments and the medial margin of the Hill-Sachs lesion. This bone bridge (BB) width plus the width of the Hill-Sachs lesion equals what we call the Hill-Sachs Interval (HSI), whose medial margin is the critical point in determining if a Hill-Sachs lesion is non-engaging or engaging.
The next step: a new paradigm for addressing bone loss in instability
We believe that anterior instability patients with glenoid bone loss ≥ 25 % of the inferior glenoid diameter, regardless of the size of the Hill-Sachs defect, must be treated with a bone graft to the glenoid. The bone graft will widen the glenoid track to such an extent that in virtually all cases, the Hill-Sachs lesion cannot go off the glenoid track. If, after grafting the glenoid, the Hill-Sachs still goes out of glenoid track when the arm is brought into abduction and external rotation, the surgeon would need to consider either concomitant bone-grafting of the Hill-Sachs defect or “remplissage” of the Hill-Sachs. However, this is hardly ever necessary. We prefer to address significant bipolar bone loss with a Latarjet procedure, in which the coracoid bone graft provides additional stability from the sling effect of the conjoined tendon. With this combination of glenoid track enlargement plus the sling effect, the Latarjet procedure is able to effectively address even large degrees of bipolar bone loss without having to resort to additional humeral-sided procedures (humeral bone graft or remplissage).
In cases with glenoid bone loss <25 % of the inferior glenoid diameter, the Hill-Sachs lesion is usually small or nonexistent. In such cases, an arthroscopic Bankart repair should be done.
However, one may see a large Hill-Sachs lesion in association with a glenoid that has little or no bone loss. In such a case, we recommend that the surgeon obtain a preoperative 3D CT scan to measure the width of the Hill-Sachs Interval (HSI = Hill-Sachs lesion plus bone bridge). If the HSI width is >83 % of the inferior glenoid diameter, we recommend that arthroscopic remplissage be added to the arthroscopic Bankart repair. With the “remplissage” procedure it is possible to fill the humeral bone defect with infraspinatus tendon, arthroscopically. Obviously, the surgeon must consider sports-specific and activity-specific demands in each individual patient. More authors reported significant reduction of range of motion of the shoulder after Hill-Sachs “replissage” in vitro and in vivo assessment [18•, 19••]. Elkinson [18•] reported a significant reduction of ROM in specimens shoulders with 30 % Hill-Sachs lesion consider adduction (14,5° ± 11,3°) and abduction (6,2° ± 9,3°) position. Boileau [19••] reported a deficit in external rotation of 8° ± 7° with the arm at the side of the trunk and 9° ± 7° with arm in abduction after arthroscopic Bankart repair combined with Hill-Sachs “remplissage” in 47 patients. For this reason, in an overhead athlete one may wish to avoid remplissage because of the loss of motion that accompanies this procedure, particularly with the arm in abduction and external rotation. Conversely, in certain high-risk collision athletes the surgeon might choose to do a Latarjet procedure, even with lesser degrees of bone loss, in order to reduce the chance of recurrent instability. It should be noted that MRI measurement techniques are in development and should soon obviate the need for CT scan, thereby eliminating the concerns about excessive radiation to the patient.
Conclusions
Based on the foregoing discussion, we prefer to categorize all of our anterior instability patients, regardless of the degree of bipolar bone loss, into one of 4 categories (Table 1).
= glenoid defect < 25 % plus non-engaging Hill-Sachs;
= glenoid defect < 25 % plus engaging Hill-Sachs;
= glenoid defect ≥ 25 % plus non-engaging Hill-Sachs;
= glenoid defect ≥ 25 % plus engaging Hill-Sachs.
Table 1.
Anterior instability categories
| Group | Glenoid Defect | Hill-Sachs |
|---|---|---|
| 1 | < 25 % | non-engaging |
| 2 | < 25 % | engaging |
| 3 | ≥ 25 % | non-engaging |
| 4 | ≥ 25 % | engaging |
Using these categories, our recommended surgical treatment paradigm is as follows (Table 2).
: Arthroscopic Bankart repair;
: Arthroscopic Bankart repair plus remplissage;
: Latarjet
: Latarjet plus humeral-sided procedure (humeral bone graft or remplissage) if Hill- Sachs is engageable by surgeon on the OR table after Latarjet; if the Hill-Sachs is not engageable by the surgeon after the Latarjet, do Latarjet only.
Table 2.
ᅟ
| Group | Treatment |
|---|---|
| 1 | Arthroscopic Bankart repair |
| 2 | Arthroscopic Bankart repair plus remplissage |
| 3 | Latarjet |
| 4 | Latarjet ± humeral-sided procedure (humeral bone graft or remplissage), depending upon engagement of H-S after Latarjet |
We believe that conversion of an engaging Hill-Sachs lesion to a non-engaging Hill-Sachs lesion is essential in stabilizing the shoulder with anterior instability. Our paradigm consistently achieves that goal.
Electronic supplementary material
When the arm is raised, the glenoid contact area shifts from the inferomedial to the superolateral portion of the posterior articular surface of the humeral head, creating a zone of contact between the glenoid and the humeral head, called “glenoid track”. When the glenoid bone-loss is on the humeral glenoid track, the Hill-Sachs lesion engages the anterior glenoid rim, causing anterior shoulder dislocation. (MOV 4185 kb)
Acknowledgments
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Giovanni Di Giacomo declares that he has no conflict of interest. Andrea De Vita declares that she has no conflict of interest. Alberto Costantini declares that he has no conflict of interest. Nicola de Gasperis declares that she has no conflict of interest. Paolo Scarso declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the authors.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.••.Burkhart S, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted–pear glenoid and the humeral engaging Hill-Sachs Lesion. Arthroscopy. 2000;16:677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 2.••.Itoi E, Yamamoto N, Kurokawa D, Sano H. Bone loss in anterior instability. Curr Rev Musculoskelet Med. 2013. Clear paper about bone loss problems in shoulder instability [DOI] [PMC free article] [PubMed]
- 3.••.Yamamoto N, Itoi E, Abe H, Minagawa H, Seki N, Shimada Y, Okada K. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elbow Surg. 2007;649–56. It is the first paper to clarify the possibility of evaluating engaging and non-engaging Hill-Sachs lesion [DOI] [PubMed]
- 4.••.Omori Y, Yamamoto N, Koishi H Tanaka M, Futai K, Goto A, et al. Measurement of the glenoid track in vivo, investigated by the three-dimensional motion analysis using open MRI. Read at the 57th Annual Meeting, ORS, Long Beach, 2011; Transactions of ORS. 2011;Poster No. 502. Interesting for in vivo measurement of glenoid track.
- 5.Jon J, Warner P, Gerber C, Itoi E, Lafosse L. Shoulder instability: an international perspective on treatment. Moderator: AAOS. 2013; ICL 107.
- 6.Provencher MT, Abrams JS, Boileau P, Richard K, Ryu N, Tokish JM. Challenging problems in shoulder instability: how to get it right the first time and what to do if you don’t. Moderator: AAOS. 2013; ICL 282.
- 7.•.Kurokawa D, Yamamoto N, Nagamoto H, Omori Y, Tanaka M, Sano H, et al. The prevalence of a large Hill-Sachs lesion that needs to be treated. J Shoulder Elbow Surg. 2013 (in press). Clarifies the concept of Hill-Sachs evaluation for correct treatment [DOI] [PubMed]
- 8.Parke, et al. Read at the 39th Annual Meeting of Japan Shoulder Society, Tokyo, 2012.
- 9.Cho SH, Cho NS, Rhee YG. Preoperative analysis of the Hill-Sachs lesion in anterior shoulder instability: how to predict engagement of the lesion. Am J Sports Med. 2011;39:2389–2395. doi: 10.1177/0363546511398644. [DOI] [PubMed] [Google Scholar]
- 10.Haviv B, Mayo L, Biggs D. Outcomes of arthroscopic "remplissage": capsulotenodesis of the engaging large Hill-Sachs lesion. J Orthop Surg Res. 2011;6:29. doi: 10.1186/1749-799X-6-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhu YM, Lu Y, Zhang J, Shen JW, Jiang CY. Arthroscopic Bankart repair combined with remplissage technique for the treatment of anterior shoulder instability with engaging Hill-Sachs lesion: a report of 49 cases with a minimum 2-year follow-up. Am J Sports Med. 2011;39:1640–1647. doi: 10.1177/0363546511400018. [DOI] [PubMed] [Google Scholar]
- 12.Gerber C, Nyffeler RW. Classification of glenohumeral joint instability. Clin Orthop Relat Res. 2002;400:65–76. doi: 10.1097/00003086-200207000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Itoi E, Lee SB, Berglund LJ, Berge LL, An KN. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am. 2000;82:35–46. doi: 10.2106/00004623-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Griffith JF, Antonio GE, Tong CWC, Ming CK. Anterior shoulder dislocation: quantification of glenoid bone loss with CT. Am J Roentgenol. 2003;180:1423–1430. doi: 10.2214/ajr.180.5.1801423. [DOI] [PubMed] [Google Scholar]
- 15.Chuang TY, Adams CR, Burkhart SS. Use of preoperative three dimensional computed tomography to quantify glenoid bone loss in shoulder instability. Arthroscopy. 2008;24:376–382. doi: 10.1016/j.arthro.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 16.Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am. 2003;85-A:878–884. doi: 10.2106/00004623-200305000-00016. [DOI] [PubMed] [Google Scholar]
- 17.Baudi P, Righi P, Bolognesi D, et al. How to identify and calculate glenoid bone deficit. Chir Organi Mov. 2005;90:145–152. [PubMed] [Google Scholar]
- 18.•.Elkinson I, Giles JW, Faber KJ, Boons HW, et al. The effect of the remplissage procedure on shoulder stability and range of motion. J Bone Joint Surg Am. 2012;94:1003–1012. doi: 10.2106/JBJS.J.01956. [DOI] [PubMed] [Google Scholar]
- 19.••.Boileau P, O’Shea K, Vargas P, Pinedo M, Old J, Zumstein M. Anatomical and functional results after arthroscopic Hill-Sachs remplissage. J Bone Joint Surg Am. 2012;94:618–626. doi: 10.2106/JBJS.K.00101. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
When the arm is raised, the glenoid contact area shifts from the inferomedial to the superolateral portion of the posterior articular surface of the humeral head, creating a zone of contact between the glenoid and the humeral head, called “glenoid track”. When the glenoid bone-loss is on the humeral glenoid track, the Hill-Sachs lesion engages the anterior glenoid rim, causing anterior shoulder dislocation. (MOV 4185 kb)


