Abstract
Acromioclavicular (AC) dislocation is a common injury especially among sportsmen. There is still a lack of consensus on whether to conserve or operate type III AC joint dislocations. Even among surgeons inclined to operate AC joint dislocations there is no unanimity on which surgical technique. There are a plethora of choices between mechanical fixation or synthetic materials or biologic anatomic reconstructions. Even among surgeons, there is a choice between open repairs and the latest—arthroscopic reconstructions. This review of AC joint dislocations intends to analyze the available surgical options, a critical analysis of existing literature, actual technique of anatomic repair, and also accompanying complications.
Keywords: AC joint, Acromioclavicular dislocation, Coracoclavicular ligament, Conoid, Trapezoid, AC ligament
Introduction
Acromioclavicular (AC) joint injuries are not uncommon and occur across different age groups. Although a typical athletic injury, AC joint dislocation is often diagnosed after road traffic accidents and fall on the side of the body. As early as 400 BC Hippocrates (460–377 BC), commented that acromioclavicular dislocation often was misdiagnosed as a glenohumeral injury [1]. Galen (129–199 AD) himself suffered an acromioclavicular dislocation and could not tolerate the tight bandaging recommended at the time and, thus, became one of the earliest noncompliant patients [1]. The treatment for AC joint dislocations has not been uniform and the results also vary, based on type of treatment. Strapping is restrictive and often nonproductive and a variety of techniques, from K-wire fixation to synthetic grafts have led to lack of confidence in choosing the correct treatment. AC joint dislocation has an overall incidence of 3 to 4 per 100 000 in the general population, with 25 % to 52 % occurring during sporting activities [2, 3].
Anatomy
The AC joint is a diarthrodial joint formed by the distal clavicle and the medial facet of the acromion. Interposed in the joint is a fibrocartilaginous disk. The acromioclavicular capsule is reinforced by anterior, superior, posterior, and inferior ligaments. The posterior and superior ligaments are the strongest and are invested by the deltotrapezial fascia. Biomechanical studies have shown that the AC ligaments and capsule are important in providing anterior-posterior stability to the AC joint. Coracoclavicular ligaments are the laterally located trapezoid ligament and the more medial conoid ligament. These are thought to be the primary suspensory ligaments of the shoulder. The coracoclavicular (CC) ligaments prevent superior-inferior displacement of the clavicle
Mechanism of injury
The mechanism of injury usually involves a direct blow to the lateral aspect of the shoulder with the arm in an adducted position, leading to downward displacement of the scapula opposed by impaction of the clavicle onto the first rib [3]. The force initially injures the acromioclavicular ligaments. The CC ligament is one of the strongest ligaments in the body. As the force perpetuates, further energy is transmitted to the coracoclavicular ligaments, resulting in greater displacement of the clavicle with reference to the acromion. A major injury will lead to further transmission of force and disruption of the deltoid and trapezius muscles, as the lateral end of clavicle herniates through it [4].
Classification
Tossy et al [5] and Allman [2] initially described the classification of acromioclavicular injuries as types I, II, and III in the 1960s. In 1984, Rockwood modified this classification to include types IV, V, and VI [6]. This classification is shown in Table 1.
Table 1.
Classification of injuries to the acromioclavicular joint [4]
| Injury type | Acromioclavicular ligament | Coracoclavicular ligament | Deltotrapezial fascia | Direction |
|---|---|---|---|---|
| I | Sprain | Intact | Intact | Nondisplaced |
| II | Complete disruption | Sprain | Intact | 25 % Superior |
| III | Complete disruption | Complete disruption | Injury | 25 %–100 % Superior |
| IV | Complete disruption | Complete disruption | Detached | Posterior through the trapezius |
| V | Complete disruption | Complete disruption | Detached | 100 %–300 % Superior |
| VI | Complete disruption | Complete disruption | Detached | Inferior to acromion or coracoid |
Clinical features
Often the deformity is overt and the examiner can observe a prominent AC joint asymmetry in comparison with normal side. Local tenderness and excruciating pain is expected in the acute setting. In a type IV and V dislocation injury, gross deformity and tenting of Trapezius and deltoid is significant along with displacement of skin. In a biclavicular [8, 9] dislocation even the sternoclavicicular joint is dislocated but is a rare occurrence. The ranges are often unaffected, though 20 % of our patients turn up with a stiff shoulder, which is possibly due to collateral injury to rotator cuff or surrounding muscles. The most common complaint in the late setting is a nagging medial scapular pain. The medial scapular pain arises due to disruption of the scapula-thoracic rhythm. Seldom, radiating pain and brachialgia result from the altered scapular biomechanics. Cross adduction tests are positive if there is AC joint synovitis and pain. Piano sign may be elicited with ballottement of the lateral end of clavicle. The O’Brien test may be particularly helpful when attempting to differentiate symptoms of AC joint arthroses from intra-articular lesions, especially with lesions of the superior glenoid labrum. It is vital to evaluate reducibility of the vertical displacement, especially in chronic dislocations. Horizontal displacement can also be measured [10].
It is not uncommon to expect collateral injuries of the Gleno humeral joint. However, it may be difficult to delineate aggravation of old injuries and new injuries. According to S Pauly [11••], they found 7.2 % and 8.8 % acute and intermediate lesions, respectively, among their 125 patients of AC joint dislocation. This makes a good case for at least a diagnostic arthroscopy prior to the AC joint repair/reconstruction procedure.
Radiographic features
Anteroposterior, lateral, and axial views are standard views taken for the shoulder; however, a Zanca view [12] is the most accurate view to look at the AC joint. This view is performed by tilting the X-ray beam 10°–15° toward the cephalic direction. To assess AC joint instability, it is desirable to use a 5 kg weight in each hand and perform bilateral comparative radiographs. Weighted X-rays can help differentiate type I from type II injuries and more importantly type II from occult type III injuries.
The axial view of the shoulder is important in differentiating a type III AC joint injury from a type IV injury. Visualization of the acromion anterior to the clavicle will indicate a type IV lesion. An increase of more than 25 %–50 % distance in CC interval by comparing the unaffected side is suggestive of complete disruption of CC ligament as per [13].
Nonoperative management
Grade I and II dislocations can be treated nonoperatively with an appropriate sling such as a RJ bandage or Kenny Brace. Three to 6 weeks immobilization followed by rehab should restore function between 2–3 months after injury. Some lateral sleeping pain on same side is expected in the early days but full functional restoration is possible. The cosmetic deformity is also not an issue with grade I and II injuries. In our practice we have extended the conservative program even for elderly patients with type III and type IV patients, when cosmetic issues are not of concern and functional restoration is possible due to the lower level of activities required then. On the other hand it is possible that a young patient continues to be symptomatic even after a substantial conservative trial. In such a patient it is important to rule out associated collateral superior labral tear anterior to posterior (SLAP) or rotator cuff injury. The most common cause of discomfort is the scapular dyskinesia, which leads to medial scapular or posterior midthoracic pain or discomfort. A scapular stabilization program beginning with initial taping and/or muscle stimulation. A significant number of patients have been treated conservatively for type III dislocations and hence, the recommendations for treating type III AC joint are controversial. Cosmetic deformity is only one of the aspects of this condition. Not all patients of type III AC joint dislocation suffer disability. There have been athletes from national teams who have happily carried out with their activity. It is, thus, difficult to pinpoint which patient will decompensate his or her shoulder biomechanics.
Operative management
Various surgical procedures have been described, but there is no clear agreement on any one of them. Early fixation techniques described were using K-wires, Steinman pins and cerclage wires. The use of hardware across the AC joint may worsen the intra-articular injury and may hasten the onset of joint arthrosis. Since the CC ligament is ignored, fixation failure is common with K-wire migration, also a possibility. Invariably mere K-wire fixations are likely to fail.
Hook plate
The Hook Plate was originally designed for lateral end clavicle fractures. This application has been extended to AC joint dislocations. It has been associated with numerous complications including Acromial Fractures, plate bending, and AC arthritis as high as 41 %, and a definite second surgery for hardware removal [14]. Hook plate eroding through acromion has been noted as early as 32 days after surgery.
Bosworth screw
Stabilization of AC joint with a screw between clavicle and coracoid. A rigid fixation between Coracoid and clavicle has been an appealing prospect in the form of screw. Due to motion between the coracoid and the clavicle, fatigue of the implant occurs over time. Biomechanical studies in cadaveric models showed that the use of a Coraco-Clavicular screw, reduced joint motion, and significantly increased joint contact pressures, which could have implications for early joint degeneration when this technique is used [15]. Failure could present as Lateral end clavicle osteolysis, hardware failure, or even fracture of coracoid or clavicle [16–19]. There have been reports of high failure of mechanical devices [20].
Weaver-Dunn procedure
This procedure was initially described in 1972, utilized the Coraco-Acromial (CA) ligament to substitute the torn CC ligament; this procedure involved the release of the Coraco-Acromial ligament from the acromion, resection of the distal end of the clavicle, and transfer of the CA ligament to the lateral end of the clavicle, more closely replicating the CC ligaments. There have been several modifications of the Weaver Dunn procedure. Biomechanical studies have shown that this nonanatomic transfer of the CA ligament alone is only 25 % as strong as the native ligaments [21••]. The parent CC ligament is inserted at the very base of the coracoid – whereas the CA ligament is attached much to distally and laterally.
Fixation techniques
Involves the use of various types of materials, for example, heavy suture or surgical tape, allograft, or autograft, which are placed around the base of the coracoid and through the distal end of the clavicle and fixed in place with various fixation means, such as suture anchors, suture buttons, and interference screws. Complications of this technique includes suture cut-out, aseptic foreign-body reaction, and clavicle osteolysis, which can result in failure. The premise of doing fixations in AC joint dislocations is to expect the native CC ligament to heal up once the AC joint is reduced. Thereby these fixation techniques are advocated only for acute Type II AC joint dislocations. The argument appears flawed, as the AC joint dislocates with plastic deformation of the CC ligament followed by eventual rupture. Even if native CC ligament were to heal, it would do so in a lengthened position. A synthetic graft or screw is unlikely to sustain cyclic loading forever.
CC ligament reconstruction
This is described as a ligament reconstruction between the coracoid and the clavicle. This involves anatomic reconstruction of the CC ligament to the base of the coracoid and about 35 mm medial to the AC joint on the clavicle.
The modern approach has been to reconstruct anatomic CC ligament with fixation or a loop at base of coracoid and a biological graft passing through clavicle either through a single drill hole or 2, to mimic the course of the conoid and trapezoid ligament. Farber emphasized the anatomic reconstruction with its benefits [22]. There are several versions of the anatomic approach, varying with biological ligament (Semitendinoses, Gracilis, EHL, and even Palmaris longus), point of fixation (single clavicle hole or 2 holes). Lee et al [23, 24] compared tendon grafts with suture materials and Weaver Dunn grafts in a cadaveric model. They reported that the graft sutured on to itself with supplemental sutures was the most secure method of fixation. Semitendinoses [25, 26••] was considered a superior graft for reconstruction of the CC ligament.
Indications
Cosmetic.
Type III with Medial Scapular Pain, stiffness and difficulty in overhead actions.
Functional in overhead athletes.
Type IV, V, and VI surgery of necessity.
Most common is type III.
Late nonunions of lateral end clavicle fractures (Figs. 1 and 2).
Figure 1.

a, One year 12 months nonunion Kenyan patient, lateral end clavicle fracture with proximal migration.
Figure 2.

Postoperative after CC ligament reconstruction with Semi T graft. No implant. (Same patient as Fig. 1)
Operative technique (ASB Technique)
We are describing here the anatomic technique of reconstructing the CC ligaments with the semitendinoses graft as described by the senior author. Under general anesthesia, with the patient in a beach chair position, the shoulder and arm is draped free. A semitendinoses graft is harvested and prepared by the standard technique. A vertical incision based on AC joint and coracoid is used. Lateral end of the clavicle is excised by about 8 mm from the joint. This is important, to avoid pain from chondrolysis postoperatively. Mazocca and others [7, 27, 28] commented that late AC joint arthritis could occur in as high as 20 % patients. A point about 35 mm medial (Conoid is inserted 45 mm medial and trapezoid 25 mm medial to AC joint) to AC joint is identified and a 4–5 mm drill hole is made depending on the size of the harvested tendon. With the help of an indirect suture shuttle, the graft is passed through the drill hole and kept aside. When the clavicle drill hole is made lateral to the coracoid, the 2 strands of the graft chart a different vector, with each strand charting different course—mimicking the conoid and trapezoid path. By feeling the coracoid through the anterior deltoid, a split in Deltoid is created in line with its fibers to expose the coracoid. The base of the coracoid is skeletonized through a rent in CA ligament and the Pectoralis Minor, without detaching these attachments. The periosteal of the coracoid is abraded with a rasp on both sides to allow the donor graft to integrate with the coracoid. The musculocutaneous nerve lies distally on the medial edge of coracoid and care is taken not to damage it. An indirect suture shuttle (usually Ethilon #1) is passed under the coracoid with the help of a Satinsky forceps from medial to lateral. The 2 ends of the semitendinoses graft are then pulled through, underneath the deltoid. This can be facilitated by the surgeon, using finger dissection, to burrow a tunnel underneath the deltoid flap. During this step the surgeon must ensure not to detach the deltoid from the anterior clavicle. Once the graft is passed around the coracoid one must ensure that the graft is not snagged in any tissue and is rotating smoothly. Bring the 2 ends of the graft anterior to the clavicle. An assistant then reduces the clavicle to its anatomic position with the help of blunt broad periosteum. Once reduced the 2 ends of the graft can be tied over themselves in a firm manner with simple half-hitches. The tied ends of the tendon are reinforced with supplemental Ethibond #2 suture. Simultaneously as the graft is being tightened, firm pressure is maintained on the lateral end of the clavicle, to reduce it into its anatomic location (Fig. 3).
Figure 3.
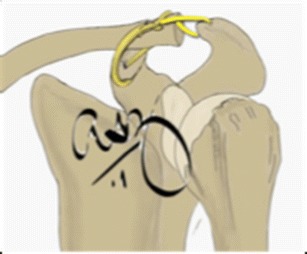
Semitendinoses graft around coracoid through clavicle and extended to Acromion and back.
The excess graft is passed across the AC joint in the anterior acromion and wound back to the lateral end clavicle into a suture anchor in lateral end of clavicle to replace the AC ligament as well. If excess length is available, then one can avoid anchor and tie the 2 ends of the graft near the clavicle and reinforce the same with Ethibond #2. Ensure that the bulk of the knot is either inferior or anterior to clavicle so as not to be prominent subcutaneously (Fig. 4).
Figure 4.
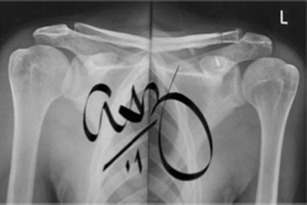
Postoperative left AC joint reconstruction Zenca view. Suture anchor in coracoid.
Postoperative protocol
Patients are discharged on the second postoperative day after a wound dressing. Patients are encouraged to perform pendulum exercises and advised to use the sling only in crowded places. They are restrained from lifting their arm above 90° and lifting heavy objects or driving. At the third week postoperative patients were encouraged to start performing isometric deltoid exercises and active assisted range of movement up to 90° flexion and abduction. After 6 weeks all restrictions are discarded. Most patients do not require a formal rehabilitation program. However, patients with rotator cuff weakness or injuries to the shoulder leading to impingement are sent on a shoulder rehab program for 10 days followed by 4 weeks at home.
Complications
Across the board, each technique has its typical fault lines. However, loss of reduction is not unusual and in one study was as high as over 40 % [29]. The infection rate was also no less and could touch 15 % of the operated cases [30]. The presence of an implant/material in the presence of persistent instability is always a concern for infection, as the implant offers an ideal nidus for infection. K-wire and Steinman pin migrations can create more injury and also embarrassing evidence on postoperative radiographs [31–37]. Failure of surgery or redislocation or implant failure is likely when the implant is not supplemented with a biological graft. Mechanical constructs in isolation can have a rather high failure or breakage rate [38•]. Brachial plexus injury is also possible especially as coracoid is adjacent to the brachial Plexus. Procedures that involve blind drilling of coracoid without dissection may have a high chance of injury to the plexus. Brachial Plexus injury may occur due to the type III AC joint injury itself and associated scapular dyskinesia and strain on the plexus [39]. Complications in our series include 1 of 43 patients with a neuroma due to injury to superficial branch, at the graft donor site. We performed a review of radiological status on an average 5 months after surgery. There was noticeable superior migration of the clavicle in 4 of the 43 patients but none of them were clinically symptomatic.
Recent advances
An arthroscopic CC ligament reconstruction is very much practiced, and there are many techniques of achieving the same. The senior author’s emphasis is on a biologic graft and, hence, our chosen technique is an arthroscopic semitendinoses graft. The technique remains the same, while the challenge is to loop the graft around the coracoid base. We prefer to approach the coracoid extra-articularly from the subacromial space and work in the anterior to coracoid space. The advocates of tight rope work through the gleno humeral joint and resect the rotator interval to approach the coracoid. The future will see more standardized arthroscopic techniques and perhaps we will have clear evidence of which technique works best. An arthroscopic reconstruction could possibly maintain the native superior AC ligaments even after performing a lateral end resection.
It is also important to address the AC ligament. The cosmetic deformity is well taken care of by the CC ligament in the superior-inferior direction. Patient’s pain and discomfort are secondary to the anterior-posterior displacement of the clavicle at the AC joint. This is preventable by adding an AC ligament reconstruction to the surgery. The intact coracoclavicular ligaments cannot compensate for the loss of capsular function during anterior-posterior loading as occurs in type-II acromioclavicular joint injuries [40].
Conclusions
An intact CC ligament after reconstruction with biological graft offers long-term stability. An implant for fixation without addressing the CC ligament is likely to fail. In addition drilling holes or fixation through coracoid can be fraught with complications due to adjacent anatomy of coracoid. Hence, our preference to loop graft around the coracoid, avoiding the risks of coracoid fracture too. The anterior-posterior displacement of AC joint also tends to cause more symptoms, which may be unaddressed, by merely restoring the superior inferior stability with CC ligament reconstruction. So it is advisable to have a biologic graft around the coracoid. The spare graft should be taken through acromion and back to lateral clavicle to reconstruct the AC ligament as well.
Compliance with Ethics Guidelines
Conflict of Interest
Ashish Babhulkar declares that he has no conflict of interest. Aditya Pawaskar declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the authors.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Rockwood CA, Jr, Young DC. Disorders of the acromioclavicular joint. In: Rockwood CA Jr, Matsen FA III, editors. The Shoulder. Philadelphia, PA: WB Saunders; 1990. pp. 413–76. [Google Scholar]
- 2.Allman FL., Jr Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg Am. 1967;49:774–84. [PubMed] [Google Scholar]
- 3.Dias JJ, Gregg PJ. Acromioclavicular joint injuries in sport: recommendations for treatment. Sports Med. 1991;11:125–32. doi: 10.2165/00007256-199111020-00004. [DOI] [PubMed] [Google Scholar]
- 4.Lemos MJ. The evaluation and treatment of the injured acromioclavicular joint in athletes. Am J Sports Med. 1998;1:137–44. doi: 10.1177/03635465980260010801. [DOI] [PubMed] [Google Scholar]
- 5.Tossy JD, Mead NC, Sigmond HM. Acromioclavicular separations: useful and practical classification for treatment. Clin Orthop. 1963;28:111–9. [PubMed] [Google Scholar]
- 6.Rockwood CA., Jr . Injuries to the acromioclavicular joint. In: Rockwood CA Jr, Green DP, editors. Fractures in Adults. Volume 1. 2nd ed. Philadelphia: JB Lippincott; 1984. pp. 860–910. [Google Scholar]
- 7.Mazzocca AD, Arciero RA, Bicos J. Evaluation and treatment of acromioclavicular joint injuries. Am J Sports Med. 2007;35:316–29. doi: 10.1177/0363546506298022. [DOI] [PubMed] [Google Scholar]
- 8.Scapinelli R. Bipolar dislocation of the clavicle: 3D CT imaging and delayed surgical correction of a case. Arch Orthop Trauma Surg. 2004;124:421–4. doi: 10.1007/s00402-004-0669-2. [DOI] [PubMed] [Google Scholar]
- 9.Echo BS, Donati RB, Powell CE. Bipolar clavicular dislocation treated surgically. A case report. J Bone Joint Surg Am. 1988;70:1251–3. [PubMed] [Google Scholar]
- 10.Simovitch R, Sanders B, Ozbaydar M, et al. Acromioclavicular joint injuries: diagnosis and management. J Am Acad Orthop Surg. 2009;17:207–19. doi: 10.5435/00124635-200904000-00002. [DOI] [PubMed] [Google Scholar]
- 11.••.Pauly S, Kraus N, Greiner S, et al. Prevalence and pattern of glenohumeral injuries among acute high-grade acromioclavicular joint instabilities. J Shoulder Elbow Surg. 2013;22:760–6. doi: 10.1016/j.jse.2012.08.016. [DOI] [PubMed] [Google Scholar]
- 12.Matani RJ, Hanlon JJ, Cady GW. Acute, complete acromioclavicular separation. J Bone Joint Surg Am. 1975;57:328–32. [PubMed] [Google Scholar]
- 13.Bearden JM, Hughston JC, Whatley GS. Acromioclavicular dislocation: method of treatment. Am J Sports Med. 1973;1:5–17. doi: 10.1177/036354657300100401. [DOI] [PubMed] [Google Scholar]
- 14.Sim E, Schwarz N, Hocker K, et al. Repair of complete acromioclavicular separations using the acromioclavicular-hook plate. Clin Orthop Relat Res. 1995;314:134–42. [PubMed] [Google Scholar]
- 15.Jari R, Costic RS, Rodosky MW, et al. Biomechanical function of surgical procedures for acromioclavicular joint dislocations. Arthroscopy. 2004;20:237–45. doi: 10.1016/j.arthro.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 16.Baker JE, Nicandri GT, Young DC, et al. A cadaveric study examining acromioclavicular joint congruity after different methods of coracoclavicular loop repair. J Shoulder Elbow Surg. 2003;12:595–8. doi: 10.1016/S1058-2746(03)00050-8. [DOI] [PubMed] [Google Scholar]
- 17.Breslow MJ, Jazrawi LM, Bernstein AD, et al. Treatment of acromioclavicular joint separation: suture or suture anchors? J Shoulder Elbow Surg. 2002. [DOI] [PubMed]
- 18.Calvo E, Lopez-Franco M, Arribas IM. Clinical and radiologic outcomes of surgical and conservative treatment of type III acromioclavicular joint injury. J Shoulder Elbow Surg. 2006. [DOI] [PubMed]
- 19.Wellmann M, Zantop T, Petersen W. Minimally invasive coracoclavicular ligament augmentation with a flip button/polydioxanone repair for treatment of total acromioclavicular joint dislocation. Arthroscopy. 2007;23. [DOI] [PubMed]
- 20.Thiel E, Mutnal A, Gilot GJ. Surgical outcome following arthroscopic fixation of acromioclavicular joint disruption with the tightrope device. Orthopedics. 2011;34. [DOI] [PubMed]
- 21.••.Mazzocca AD, Santangelo SA, Johnson ST, et al. A biomechanical evaluation of an anatomical coracoclavicular ligament reconstruction. Am J Sports Med. 2006;34:236–46. doi: 10.1177/0363546505281795. [DOI] [PubMed] [Google Scholar]
- 22.Farber AJ, Cascio BM, Wilckens JH. Type III acromioclavicular separation: rationale for anatomical reconstruction. Am J Orthop. 2008;37:349–55. [PubMed] [Google Scholar]
- 23.Lee SJ, Nicholas SJ, Akizuki KH, et al. Reconstruction of the coracoclavicular ligaments with tendon grafts: a comparative biomechanical study. Am J Sports Med. 2003;31:648–54. doi: 10.1177/03635465030310050301. [DOI] [PubMed] [Google Scholar]
- 24.Sani Erak MH, Pelletier MH, Woods KR, et al. Acromioclavicular reconstructions with hamstring tendon grafts: a comparative biomechanical study. J Shoulder Elbow Surg. 2008;17:772–8. doi: 10.1016/j.jse.2008.01.143. [DOI] [PubMed] [Google Scholar]
- 25.Tauber M, Gordon K, Koller H, et al. Semitendinosus tendon graft versus a modified Weaver-Dunn procedure for acromioclavicular joint reconstruction in chronic cases: a prospective comparative study. Am J Sports Med. 2009;37:181–90. doi: 10.1177/0363546508323255. [DOI] [PubMed] [Google Scholar]
- 26.••.Carofino BC, Mazzocca AD. The anatomic coracoclavicular ligament reconstruction: surgical technique and indications. J Shoulder Elbow Surg. 2010;19:37–46. doi: 10.1016/j.jse.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 27.Mazzoca, et al. Injuries to the acromioclavicular joint in children. In: Delee JC, Drez D, et al., editors. Orthopedic Sports Medicine. 2nd ed. Philadelphia: Saunders; 2003. [Google Scholar]
- 28.Smith MJ, Stewart MJ. Acute acromioclavicular separations. Am J Sports Med. 1979;7:62–71. doi: 10.1177/036354657900700113. [DOI] [PubMed] [Google Scholar]
- 29.Stam L, Dawson I. Complete acromioclavicular dislocations. Treatment with Dacron ligament. Injury. 1991;173–6. [DOI] [PubMed]
- 30.Larsen E, Bjerg-Nielson A, Christensen P. Conservative treatment of acromioclavicular dislocation. A prospective controlled randomized study. J Bone Joint Surg. 1986;68A:552–5. [PubMed] [Google Scholar]
- 31.Neault MA, Nuber GW, Marymont JV. Infections after surgical repair of acromioclavicular separations with nonabsorbable tape or suture. J Shoulder Elbow Surg. 1996;5:477–8. doi: 10.1016/S1058-2746(96)80021-8. [DOI] [PubMed] [Google Scholar]
- 32.Mazet RJ. Migration of a Kirschner wire from the shoulder region into the lung: report of 2 cases. J Bone Joint Surg. 1943;25A:477–83. [Google Scholar]
- 33.Norrell H, Lyewellyn RC. Migration of a threaded Steinmann pin from an acromioclavicular joint into the spinal canal: a case report. J Bone Joint Surg. 1965;47:1024–6. [PubMed] [Google Scholar]
- 34.Eaton R, Serletti J. Computerized axial tomography— a method of localizing Steinmann pin migration: a case report. Orthopaedics. 1981;4:1357–60. doi: 10.3928/0147-7447-19811201-05. [DOI] [PubMed] [Google Scholar]
- 35.Kappakas GS, McMaster JH. Repair of acromioclavicular separation using a Dacron prosthesis graft. Clin Orthop. 1978;131:247–51. [PubMed] [Google Scholar]
- 36.Nelson CL. Repair of acromioclavicular separations with knitted Dacron graft. Clin Orthop. 1979;143:289. [Google Scholar]
- 37.Park JP, Arnold JA, Coker TP. Treatment of acromioclavicular separations: a retrospective study. Am J Sports Med. 1980;8:251–6. doi: 10.1177/036354658000800407. [DOI] [PubMed] [Google Scholar]
- 38.•.Bindra J, VanDenBogaerde J, Hunter JC. Coracoid fracture with recurrent AC joint separation after tightrope repair of AC joint dislocation. Radiology Case Reports. 2011;6:624. doi: 10.2484/rcr.v6i4.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Meislin RJ, Zuckerman JD, Nainzadeh N. Type III acromioclavicular joint separation associated with late brachial plexus neuropraxia. J Orth Trauma. 1992;6:370–2. doi: 10.1097/00005131-199209000-00017. [DOI] [PubMed] [Google Scholar]
- 40.Debski E, Parsons IM, Woo SL-Y, et al. Effect of capsular injury on acromioclavicular joint mechanics. J Bone Joint Surg Am. 2001;83:1344–51. doi: 10.2106/00004623-200109000-00009. [DOI] [PubMed] [Google Scholar]


