Abstract
Objective
To examine whether trauma and posttraumatic stress disorder (PTSD) are differentially associated with binge and hazardous patterns of drinking among women and men.
Methods
Secondary analysis of the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC); the analytic sample included 31,487 respondents (54.6% female) without past-year alcohol abuse/dependence. Participants’ trauma-exposure/PTSD status was characterized as: no exposure to trauma in lifetime (reference), lifetime trauma exposure, PTSD before past-year, or past-year PTSD. Past-year binge and hazardous drinking were examined with multinomial logistic regression models (past-year abstinence was modeled as the non-event); models included the main effects of trauma-exposure/PTSD status and gender, the trauma-exposure/PTSD status-by-gender interaction, psychiatric comorbidity, and socio-demographic covariates.
Results
The gender-specific effects of trauma, before past-year PTSD, and past-year PTSD were significantly elevated for all drinking behaviors in women (range of odds ratios (ORs)=1.8–4.8), and for some drinking behaviors in men (range of ORs=1.3–2.0), relative to no trauma exposure. Trauma exposure was more strongly associated with high-frequency binge drinking, low-frequency binge drinking, and non-binge drinking among women as compared to men. Past-year PTSD was also more strongly associated with low-frequency binge drinking and non-binge drinking among women compared to men. Findings for hazardous drinking followed a similar pattern, with significant gender-related differences in ORs for hazardous drinking and non-hazardous drinking observed with respect to trauma exposure and past-year PTSD.
Conclusion
Mental health practitioners should be mindful of the extent to which trauma-exposed individuals both with and without PTSD engage in binge and hazardous drinking, given the negative consequences associated with these patterns of drinking.
Keywords: Trauma, PTSD, Binge Drinking, Hazardous Drinking, Gender, Epidemiology
Introduction
Exposure to traumatic life events is common throughout the world with rates ranging from 2–30% (Stein et al., 2010). In the United States, exposure to traumatic life events such as physical and sexual assault, natural disasters, and motor vehicle accidents is also common (see Kessler, 2000). For example, in their community epidemiologic survey, Breslau et al. (1998) found that approximately 90% of respondents indicated that they had experienced at least one traumatic event (as defined by the Diagnostic and Statistical Manual of Mental Disorders; DSM-IV, American Psychiatric Association, 1994) at some point in their life. As a result of trauma, a significant proportion of individuals may go on to develop posttraumatic stress disorder (PTSD), a disorder that is characterized by re-experiencing symptoms related to the trauma (e.g., nightmares, flashbacks), avoidance of trauma-related stimuli, emotional numbing, and increased arousal (e.g., increased anger, hypervigilance).
Trauma exposure and PTSD are associated with high rates of alcohol-use disorders. For example, Kessler et al., 1996 found that that 3.7% and 8.8% of individuals with past-year PTSD met criteria for alcohol abuse and dependence in the past year, respectively, while 6.5% and 28.1% of those with lifetime PTSD met criteria for lifetime alcohol abuse and dependence, respectively. Frequent co-occurrences of trauma, PTSD and problematic alcohol use have been documented not only in community samples, but also in military (McDevitt-Murphy et al., 2010) and treatment-seeking samples (Swett et al., 1991). For example, many individuals seeking treatment for alcohol and other substance-use disorders have histories of trauma exposure (Ouimette et al, 2000; Rice et al., 2001), and as many as 61% of men and 30–59% of women seeking treatment for substance-use disorders meet diagnostic criteria for PTSD (Brady et al., 1994; Dansky et al, 1995; Sharkansky et al., 1999).
Binge and Hazardous Drinking: Associations with Trauma/PTSD
Binge drinking is defined as consuming at least 5 alcoholic beverages (4 for women) on a single occasion (NIAAA, 2004). These amounts when consumed typically bring an individual’s blood alcohol concentration level up to .08 or above. At this level, individuals are more likely to engage in a multiple alcohol-related problematic behaviors, including drunk driving, vandalism, and fights. The amount of alcohol consumed in order to reach this specific level differs for men and women; hence, the different specified amounts. Hazardous drinking is defined consuming as 7 or more drinks per week or more than 3 drinks per occasion for women, 14 or more drinks per week or more than 4 drinks per occasion for men (US Department of Health and Human Services, 2005). Drinking in excess of these daily/weekly amounts is associated with an increased likelihood of being diagnosed with an alcohol-use disorder (Dawson et al., 2005). As with binge drinking, these amounts reflect the amount of alcohol that is associated with significant impairments in cognitive and psychomotor performance.
Features of PTSD and exposure to different traumatic events in the US, both natural and man-made, have been shown to be associated with binge and hazardous drinking. For example, greater exposure to the World-Trade-Center disaster that occurred on September 11, 2001 was associated with greater alcohol consumption, in addition to binge drinking, one-year after the event (Boscarino et al., 2006). Additionally, hurricane-related traumatic events and post-hurricane stressors were associated with more drinking in general and more binge drinking after the Katrina and Rita hurricanes (Cerdá et al., 2011).
Gender-related Differences in Alcohol Use, Trauma and PTSD
Men drink more frequently and more heavily than women (Holmila & Raitasalo, 2005; Wilsnack et al., 2000; Wilsnack & Wilsnack, 1997). Men tend to engage in higher levels of binge and heavy drinking compared to women, and rates of alcohol abuse and dependence are higher among men than among women (Office of Applied Studies, 2006). Although there are several possible reasons for observed gender-related differences in drinking, explanations tend to focus on biological and/or cultural reasons (Wilsnack & Wilsnack, 1997; Wilsnack et al., 2000). For example, women may not need to consume as much alcohol as men to reach peak blood alcohol concentration because women have lower volumes of body water compared to men. In relation to socio-cultural factors, drinking among women may be more socially proscribed, whereas with men, drinking may be more acceptable (Wilsnack et al., 2000). Regardless of the reasons, the observation of these gender-related differences across societies and cultures speaks to the robustness of these findings (although see Keyes et al., 2008 who found that gender-related differences may be narrowing).
Men are exposed to a greater number of traumatic events compared to women (Breslau et al., 1998; Kessler et al., 1995; Stein et al., 1997), although the types of traumatic events tend to differ. Specifically, men are more likely to report being exposed to fire, life-threatening accidents, physical assaults, combat, and threats with a weapon, as well as being held captive, whereas women are more likely to report sexual molestation, sexual assault, and child abuse (Kessler et al., 1995). Although men report more exposure to traumatic events, rates of PTSD are higher among women. Women appear approximately twice as likely as men to develop PTSD, and PTSD tends to be more persistent and chronic in women than in men (Norris et al., 2002). Proposed explanations to account for this gender-related difference include insufficient social support resources among women, increased use of maladaptive coping strategies (including greater use of alcohol to manage trauma-related symptoms) among women, and gender-related differences in acute psychological reactions to trauma (Olf et al., 2007). Although some believe that the increased risk of PTSD among women may relate to their increased likelihood of experiencing rape and sexual assault (as these types of traumas have been considered more devastating compared to other types of trauma; Breslau et al., 1999; Norris, 1992), researchers also have shown that gender-related differences in the rate of PTSD still exist even after controlling for the specific type of threat experienced (see Olf et al., 2007 for a review). Thus, although women may be more likely to experience these types of traumas, this relationship does not seem to account fully for gender-related differences observed in PTSD.
In addition to the observed gender-related differences in alcohol use, trauma exposure, and PTSD, researchers have observed differences between men and women in the co-occurrence of PTSD and alcohol-use disorders. Helzer et al. (1987) found a trend toward higher risk for alcohol-use-disorder/PTSD comorbidity among women relative to men. More specifically, they found that women diagnosed with PTSD were 2.4 times more likely to be diagnosed with alcoholism, whereas men with PTSD were 1.7 times more likely to be diagnosed with alcoholism. Similar findings were reported by Kessler et al. (1997); specifically, they found that the odds of being diagnosed with PTSD in the presence of lifetime alcohol abuse is significantly greater among women than among men. Importantly, women compared to men are more likely to have experienced PTSD prior to developing their alcohol-use disorder (Stewart et al., 2002).
Although researchers have documented gender-related differences in the associations between PTSD and alcohol dependence/abuse, they have not systematically examined whether there are similar differences in the associations between PTSD and binge and hazardous drinking. Examining binge and hazardous drinking is important as both forms of drinking are associated with negative health consequences. For example, binge drinking can result in alcohol poisoning, hypertension, and diabetes-related problems (Naimi et al., 2003) and increase the risk of developing more serious alcohol-related psychiatric disorders (Kuntsche et al., 2004; Standridge et al., 2004). Knowing whether gender-related differences exist in the relationships between PTSD and binge and hazardous drinking has important clinical implications, as it could help inform both prevention and intervention efforts.
In addition, researchers have not consistently examined whether women and men who have been exposed to trauma but not diagnosed with PTSD engage in binge and hazardous drinking. Such research would be important given that researchers have found trauma exposure to be associated with problematic alcohol use even after accounting for symptoms of PTSD (Boscarino et al., 2006) and have observed elevated rates of alcohol use disorders among trauma-exposed individuals both with and without PTSD, compared to those with no trauma histories (Breslau et al., 1997). If trauma-exposed individuals not meeting criteria for PTSD may be at increased risk of engaging in binge and hazardous drinking, increased clinical attention would be warranted to these trauma-exposed individuals. In the current study, we sought to examine the relationships between trauma exposure (without PTSD), PTSD, and binge and hazardous drinking using data from a large national epidemiological study. We hypothesized that trauma exposure and PTSD would be positively associated with binge and hazardous drinking. Given that there is a higher risk for co-occurring alcohol use disorders and PTSD among women compared to men (Helzer et al., 1987), we also hypothesized that there would be stronger associations between trauma exposure/PTSD and binge and hazardous drinking among women compared to men in the current study.
Methods
A detailed description of study methods, including NESARC sample selection procedures, characteristics of the survey instrument, and operationalization of main study variables can be found in Supplemental Materials: Part 1.
Dependent Variables
Past-year binge drinking was categorized by four mutually exclusive levels of response: past-year non-drinking, past-year non-binge drinking, past-year low-frequency binge drinking, and past-year high-frequency binge drinking. Participants who reported consuming less than one alcoholic drink in the past year were characterized as past-year non-drinking. Participants who consumed one or more alcoholic drinks in the past year, but did not engage in any episodes of binge drinking, were characterized as past-year non-binge drinking. Participants who engaged in 1–11 episodes of binge drinking in the past year were characterized as past-year low-frequency binge drinking; participants who engaged in one or more episodes of binge drinking per month were characterized as past-year high-frequency binge drinking.
Past-year hazardous drinking was categorized by three mutually exclusive levels of response: past-year non-drinking, past-year non-hazardous drinking, and past-year hazardous drinking. Past-year non-drinking is characterized as defined above. Participants whose drinking did not exceed either weekly or daily drinking limits in the past year were characterized as past-year non-hazardous drinking; participants whose drinking did exceed either weekly or daily drinking in the past year were characterized as past-year hazardous drinking.
Independent Variables
Trauma-exposure/PTSD status was categorized by four mutually exclusive levels of response: no trauma exposure, trauma exposure without PTSD, PTSD present in the participant’s lifetime but not in the 12 months directly preceding the Wave-2 assessment (before-past-year PTSD), and PTSD present in the 12 months directly preceding the Wave-2 assessment (past-year PTSD).
Covariates
Covariates assessed at Wave 2 included past-year mood disorders (major depression, dysthymia, hypomania, mania), past-year anxiety disorders (panic disorder with or without agoraphobia, agoraphobia, specific phobia, social phobia, generalized anxiety disorder), drug abuse/dependence (sedatives, tranquilizers, opiates [other than heroin or methadone], stimulants, hallucinogens, cannabis, cocaine, inhalants/solvents, heroin, and other drugs), and nicotine dependence. Covariates also included wave-2 socio-demographic variables including age, race, education, marital status, work, and household income.
Data Analytic Strategy
In bivariate analysis, we examined the associations between (1) trauma-exposure/PTSD status and all study covariates (separately for men and women); (2) gender and past-year binge and hazardous drinking; and (3) trauma-exposure/PTSD status and past-year binge and hazardous drinking (separately for men and women). Then, to determine whether trauma-exposure/PTSD status was differentially associated with past-year binge and hazardous drinking among women and men, we constructed multivariate-adjusted multinomial logistic regression models, where trauma-exposure/PTSD was the independent variable and past-year binge drinking and past-year hazardous drinking were the dependent variables. For all multinomial models, past-year non-drinking was modeled as the non-event for the dependent variable (past-year binge drinking and past-year hazardous drinking), and no lifetime trauma exposure served as the reference category for the independent variable (trauma-exposure/PTSD status). Logistic regression models included the main effects of trauma-exposure/PTSD status and gender, in addition to the trauma-exposure/PTSD-status-by-gender interaction. Past-year psychiatric comorbidity and socio-demographic covariates were included in the models as well. Presented are gender-specific odds ratios (ORs) and their associated 95% confidence intervals (95%CIs); the OR quantifies the strength and direction of the association between trauma exposure/PTSD status and the outcomes of interest (past-year binge drinking and past-year hazardous drinking). Furthermore, a 95%CI that does not include the null (1.0) indicates a statistically significant association. Also presented are interaction odds ratios (IORs) and their corresponding 95%CIs. The IOR is the ratio of the gender-specific odds ratios (i.e., OR (women)/OR (men)); in this case, a 95%CI that does not include the null indicates that there is a statistically significant gender-related difference in the association between trauma exposure/PTSD and the outcome of interest. All data were analyzed using the SUDAAN version 10.1 software (Research Triangle Institute).
In exploratory analyses, we repeated these analyses among NESARC participants meeting DSM-IV-TR diagnostic criteria for past-year alcohol abuse/dependence. Please refer to the supplemental section for a description of the sample, methods, and results of these analyses.
Results
Bivariate analysis of study covariates and trauma-exposure/PTSD status, by gender (Table 1)
Table 1.
Bivariate analysis of sample characteristics and trauma-exposure/PTSD status, by gender
| Study covariates | Women | Men | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||||
| No trauma (n=1,783, 9%) | Trauma (n=15,608; 82%) | Before past-year PTSD (n=505; 2%) | Past-year PTSD (n=1,133; 6%) | p | No trauma (n=1,079; 9%) | Trauma (n=10,848; 87%) | Before past-year PTSD (n=173; 1%) | Past-year PTSD (n=358; 3%) | p | |||||||||
|
|
|
|||||||||||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | |||
| Race | <.001 | <.001 | ||||||||||||||||
| White | 720 | 54.6 | 9,035 | 72.2 | 276 | 69.6 | 618 | 68.1 | 481 | 55.7 | 6,692 | 72.0 | 104 | 69.8 | 210 | 73.5 | ||
| Black | 505 | 17.4 | 3,161 | 11.2 | 126 | 14.2 | 255 | 13.4 | 240 | 15.1 | 1,702 | 9.7 | 30 | 11.2 | 75 | 12.7 | ||
| Other | 100 | 9.7 | 675 | 6.4 | 21 | 5.2 | 55 | 6.2 | 304 | 21.1 | 1,950 | 11.7 | 30 | 13.2 | 62 | 10.7 | ||
| Hispanic | 458 | 18.4 | 2,737 | 10.2 | 82 | 11.0 | 205 | 12.3 | 54 | 8.0 | 504 | 6.6 | 9 | 5.9 | 11 | 3.2 | ||
| Marital status | <.001 | <. 001 | ||||||||||||||||
| Married1 | 812 | 57.2 | 8,116 | 62.3 | 230 | 58.0 | 515 | 55.0 | 607 | 63.6 | 6,928 | 71.0 | 98 | 69.3 | 188 | 63.9 | ||
| Formerly married2 | 632 | 27.0 | 4,896 | 23.6 | 213 | 32.7 | 433 | 31.5 | 192 | 12.0 | 1,929 | 12.1 | 37 | 13.9 | 92 | 19.6 | ||
| Never married | 339 | 15.8 | 2,596 | 14.1 | 62 | 9.4 | 185 | 13.5 | 280 | 24.4 | 1,991 | 16.9 | 38 | 16.8 | 78 | 16.5 | ||
| Education | <.001 | <.001 | ||||||||||||||||
| Less than high school | 506 | 25.2 | 2,339 | 13.0 | 82 | 16.8 | 222 | 16.8 | 297 | 23.8 | 1,607 | 13.5 | 25 | 11.3 | 64 | 16.7 | ||
| High school | 574 | 32.4 | 4,313 | 28.0 | 119 | 22.3 | 301 | 26.5 | 308 | 28.8 | 2,833 | 26.5 | 41 | 23.9 | 101 | 30.5 | ||
| More than high school | 703 | 42.3 | 8,956 | 59.1 | 304 | 60.9 | 610 | 56.7 | 474 | 47.4 | 6,408 | 60.0 | 107 | 64.8 | 193 | 52.8 | ||
| Employment | <. 001 | .0012 | ||||||||||||||||
| Full time | 659 | 37.6 | 6,750 | 42.1 | 217 | 40.9 | 442 | 39.0 | 667 | 64.8 | 6,674 | 63.5 | 111 | 64.1 | 169 | 49.1 | ||
| Part time | 194 | 10.3 | 2,071 | 14.5 | 66 | 14.5 | 147 | 14.5 | 93 | 9.2 | 746 | 6.7 | 9 | 6.8 | 23 | 7.7 | ||
| Other | 930 | 52.1 | 6,787 | 43.4 | 222 | 44.6 | 544 | 46.5 | 319 | 26.1 | 3,428 | 29.8 | 53 | 29.1 | 166 | 43.2 | ||
| Income | <.001 | <.001 | ||||||||||||||||
| $0–19,999 | 714 | 33.9 | 4,131 | 21.4 | 156 | 20.0 | 410 | 30.8 | 288 | 22.3 | 1,863 | 14.5 | 29 | 15.7 | 104 | 26.5 | ||
| $20,000–34,999 | 422 | 22.2 | 3,190 | 19.2 | 114 | 20.9 | 275 | 23.6 | 278 | 26.6 | 2,024 | 17.4 | 39 | 19.0 | 90 | 23.1 | ||
| $35,000–69,999 | 423 | 26.9 | 4,711 | 31.8 | 136 | 28.5 | 269 | 26.3 | 307 | 28.5 | 3,618 | 34.1 | 56 | 31.3 | 90 | 28.4 | ||
| ≥ $70,000 | 224 | 17.1 | 3,576 | 27.5 | 99 | 24.6 | 179 | 19.3 | 206 | 22.7 | 3,343 | 34.0 | 49 | 34.0 | 74 | 22.0 | ||
| Any Mood Disorder | <.001 | <.001 | ||||||||||||||||
| Yes | 123 | 6.10 | 1,685 | 10.5 | 116 | 23.4 | 465 | 39.4 | 31 | 2.0 | 635 | 5.8 | 28 | 13.8 | 126 | 35.1 | ||
| No | 1,660 | 93.9 | 13,923 | 89.5 | 289 | 76.6 | 668 | 60.6 | 1,048 | 98.0 | 10,213 | 94.2 | 145 | 86.2 | 232 | 64.9 | ||
| Any Anxiety Disorder | <.001 | <.001 | ||||||||||||||||
| Yes | 111 | 5.7 | 2,236 | 14.1 | 140 | 28.7 | 516 | 43.2 | 36 | 3.4 | 762 | 7.0 | 31 | 14.8 | 129 | 34.8 | ||
| No | 1,672 | 94.3 | 13,372 | 85.9 | 365 | 71.3 | 617 | 56.8 | 1,043 | 96.6 | 10,086 | 93.0 | 142 | 85.2 | 229 | 65.2 | ||
| Nicotine Dependence | <.001 | <.001 | ||||||||||||||||
| Yes | 87 | 5.5 | 1,590 | 10.6 | 89 | 18.9 | 264 | 23.7 | 70 | 6.9 | 1335 | 13.2 | 34 | 23.9 | 97 | 30.0 | ||
| No | 1,696 | 94.5 | 14,018 | 89.4 | 416 | 81.1 | 869 | 76.4 | 1,009 | 93.1 | 9,513 | 86.8 | 139 | 76.2 | 261 | 70.0 | ||
| Drug-use Disorders | <. 001 | .0109 | ||||||||||||||||
| Yes | 7 | 0.32 | 101 | 0.75 | 8 | 1.4 | 37 | 3.1 | 6 | 0.6 | 162 | 1.5 | 6 | 3.9 | 12 | 4.4 | ||
| No | 1,776 | 99.7 | 15,507 | 99.3 | 497 | 98.6 | 1096 | 96.9 | 1,073 | 99.4 | 10,686 | 98.5 | 167 | 96.1 | 346 | 95.6 | ||
| M | SE | M | SE | M | SE | M | SE | M | SE | M | SE | M | SE | M | SE | |||
| Current Age, years | 51.0 | 0.6 | 49.8 | 0.2 | 49.2 | 0.8 | 46.8 | 0.5 | <.001 | 45.6 | 0.7 | 48.9 | 0.2 | 50.2 | 1.4 | 47.8 | 1.0 | <. 001 |
Notes:
Category includes living as married
Category includes separated, widowed, and divorced participants
M, Mean; SE, standard Error
N are unweighted; % are weighted column percentages (columns sum to 100%)
p is for Wald Chi-Square test; bivariate associations between trauma/PTSD status and each covariate are presented, separately by gender.
Trauma-exposure/PTSD status was associated with race, marital status, education, full-time employment, income, and age among both men and women (all p<.01). Trauma-exposure/PTSD status was positively associated with any mood disorder, any anxiety disorder, nicotine dependence, and drug-use disorders among both men and women, with the highest prevalence observed among individuals with past-year PTSD (all p<.05).
Bivariate analysis of gender and binge and hazardous drinking (Table 2)
Table 2.
Bivariate analysis of gender and past-year drinking outcomes
| Binge Drinking | Hazardous Drinking | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||
| Past-year non- drinking |
Past-year non- binge drinking |
Past-year low frequency binge drinking |
Past-year high frequency binge drinking |
Past-year non- drinking |
Past-year non- hazardous drinking |
Past-year hazardous drinking |
||||||||||
|
|
|
|||||||||||||||
| N | % | N | % | N | % | N | % | p | N | % | N | % | N | % | p | |
| Gender | <.001 | <.001 | ||||||||||||||
| Women | 8,307 | 41.3 | 7,829 | 42.4 | 1,793 | 10.2 | 1,092 | 6.1 | 8,307 | 41.3 | 7,001 | 37.8 | 3,714 | 20.8 | ||
| Men | 4,167 | 32.9 | 5,235 | 41.6 | 1,602 | 13.8 | 1,446 | 11.8 | 4,167 | 32.9 | 4,750 | 37.8 | 3,536 | 29.4 | ||
N are unweighted; % are weighted row percentages (rows sum to 100%)
p is for Wald Chi-Square test; bivariate associations between gender and each drinking outcome are presented
Gender differences in past-year binge drinking (p<.001) and hazardous drinking (p<.001) were observed. In general, men demonstrated more severe patterns of drinking as compared to women. For example, relatively more men than women reported engaging in high frequency binge drinking (11.8% vs. 6.1%) and hazardous drinking (29.4% vs. 20.8%).
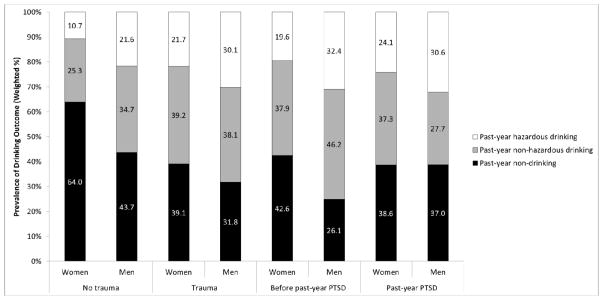
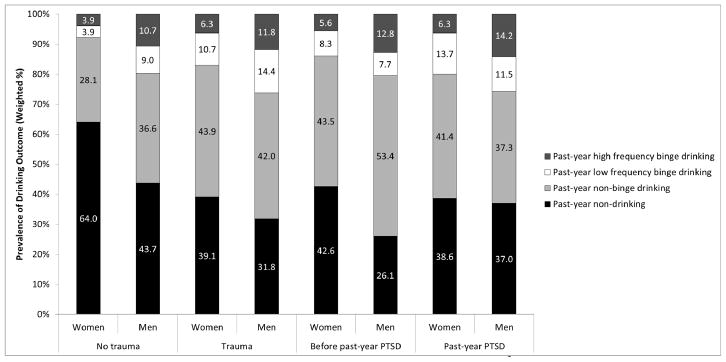
Bivariate analysis of trauma-exposure/PTSD status and binge and hazardous drinking, by gender (Table 3, Figures 1 and 2)
Table 3.
Bivariate analysis of trauma-exposure/PTSD status and past-year drinking outcomes, by gender
| Binge Drinking | Hazardous Drinking | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||
| Past-year non- drinking |
Past-year non- binge drinking |
Past-year low frequency binge drinking |
Past-year high frequency binge drinking |
Past-year non- drinking |
Past-year non- hazardous drinking |
Past-year hazardous drinking |
||||||||||
|
|
|
|||||||||||||||
| N | % | N | % | N | % | N | % | p | N | % | N | % | N | % | p | |
| Women | <.001 | <.001 | ||||||||||||||
| No Trauma | 1,163 | 64.0 | 484 | 28.1 | 65 | 3.9 | 68 | 3.9 | 1,163 | 64.0 | 434 | 25.3 | 183 | 10.7 | ||
| Trauma | 6,461 | 39.1 | 6,671 | 43.9 | 1,548 | 10.7 | 923 | 6.3 | 6,461 | 39.1 | 5,956 | 39.2 | 3,187 | 21.7 | ||
| Before past-year PTSD | 219 | 42.6 | 215 | 43.5 | 44 | 8.3 | 27 | 5.6 | 219 | 42.6 | 192 | 37.9 | 94 | 19.6 | ||
| Past-year PTSD | 464 | 38.6 | 459 | 41.4 | 136 | 13.7 | 74 | 6.3 | 464 | 38.6 | 419 | 37.3 | 250 | 24.1 | ||
| Men | <.001 | <.001 | ||||||||||||||
| No Trauma | 480 | 43.7 | 394 | 36.6 | 91 | 9.0 | 113 | 10.7 | 480 | 43.7 | 367 | 34.7 | 230 | 21.6 | ||
| Trauma | 3,498 | 31.8 | 4,615 | 42.0 | 1,459 | 14.4 | 1,269 | 11.8 | 3,498 | 31.8 | 4,183 | 38.1 | 3,164 | 30.1 | ||
| Before past-year PTSD | 50 | 26.1 | 87 | 53.4 | 15 | 7.7 | 21 | 12.8 | 50 | 26.1 | 76 | 46.2 | 124 | 32.4 | ||
| Past-year PTSD | 139 | 37.0 | 139 | 37.3 | 37 | 11.5 | 43 | 14.2 | 139 | 37.0 | 47 | 27.7 | 95 | 30.6 | ||
Notes:
N are unweighted; % are weighted row percentages (rows sum to 100%)
p is for Wald Chi-Square test; bivariate associations between trauma-exposure/PTSD status and each outcome are presented, separately by gender.
Figure 1.
Prevalence of past-year binge drinking outcomes according to trauma/PTSD status, by gender
Among women, trauma-exposure/PTSD status is significantly associated with Binge Drinking (χ2=9.96, p<.001).
Among men, trauma-exposure/PTSD status is significantly associated with Binge Drinking (χ2=3.77, p<.001).
Gender is significantly associated with Binge Drinking among participants with no trauma exposure (χ2=18.50, p<.001), exposure to trauma (χ2=27.62, p<.001), before past-year PTSD (χ2=4.11, p=.0098), and past-year PTSD (χ2=3.67, p=.0166).
Figure 2.
Prevalence of past-year hazardous drinking outcomes according to trauma exposure/PTSD status, by gender
Among women, trauma exposure/PTSD status is significantly associated with Hazardous Drinking (χ2=13.54, p<.001).
Among men, trauma exposure/PTSD status is significantly associated with Hazardous Drinking (χ2=4.46, p<.001).
Gender is significantly associated with Hazardous Drinking among participants with no trauma exposure (χ2=25.82, p<.001), exposure to trauma (χ2=34.32, p<.001), before past-year PTSD (χ2=5.77, p=.0049); gender was not significantly associated with Hazardous Drinking among participants with past-year PTSD (χ2=1.78, p=.1773).
Among both men and women, trauma-exposure/PTSD status was associated with past-year binge drinking and hazardous drinking (all p<.001). Generally, severe patterns of drinking were most prevalent among men and women with trauma exposure or past-year PTSD.
Multivariate modeling with interaction analyses: Gender-specific effects of trauma-exposure/PTSD status (Table 4)
Table 4.
Multivariate-adjusted multinomial logistic regression modeling of trauma-exposure/PTSD status and past-year drinking outcomes, by gender
| Binge Drinking1 | Hazardous Drinking1 | ||||
|---|---|---|---|---|---|
|
| |||||
| Past-year non-binge drinking | Past-year low frequency binge drinking | Past-year high frequency binge drinking | Past-year non-hazardous drinking | Past-year hazardous drinking | |
|
| |||||
| OR (95 %CI) | OR (95 %CI) | OR (95 %CI) | OR (95 %CI) | OR (95 %CI) | |
| Women | |||||
| No Trauma | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Trauma | 2.03 (1.72–2.40) | 3.66 (2.62–5.12) | 2.42 (1.83–3.22) | 2.03 (1.71–2.41) | 2.75 (2.26–3.35) |
| Before past-year PTSD | 1.89 (1.39–2.57) | 2.56 (1.45–4.52) | 1.98 (1.10–3.57) | 1.85 (1.35–2.54) | 2.24 (1.51–3.32) |
| Past-year PTSD | 2.15 (1.70–2.72) | 4.80 (3.12–7.38) | 2.32 (1.46–3.70) | 2.17 (1.72–2.75) | 3.02 (2.24–4.09) |
| Men | |||||
| No Trauma | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Trauma | 1.30 (1.06–1.60) | 2.02 (1.42–2.85) | 1.61 (1.18–2.19) | 1.26 (1.02–1.55) | 1.80 (1.39–2.32) |
| Before past-year PTSD | 1.98 (1.27–3.11) | 1.36 (0.61–3.06) | 2.11 (0.99–4.49) | 1.85 (1.17–2.94) | 2.02 (1.10–3.72) |
| Past-year PTSD | 1.14 (0.78–1.65) | 1.46 (0.81–2.65) | 1.71 (1.03–2.83) | 1.06 (0.72–1.57) | 1.66 (1.11–2.48) |
| Interaction OR: WomenOR vs. MenOR | IOR (95% CI) | IOR (95% CI) | IOR (95% CI) | IOR (95% CI) | IOR (95% CI) |
| Trauma2 | 1.56 (1.24–1.96) | 1.81 (1.16–2.85) | 1.51 (1.03–2.21) | 1.61 (1.28–2.03) | 1.53 (1.15–2.04) |
| Before past-year PTSD2 | 0.95 (0.57–1.60) | 1.88 (0.70–5.03) | 0.94 (0.37–2.38) | 1.00 (0.59–1.70) | 1.11 (0.55–2.22) |
| Past-year PTSD 2 | 1.89 (1.29–2.77) | 3.28 (1.60–6.71) | 1.36 (0.73–2.52) | 2.04 (1.37–3.03) | 1.82 (1.15–2.88) |
Past-year non-drinking is modeled as the non-event
No trauma exposure is the reference category for the gender-specific odds ratio.
Notes:
OR=Odds ratio; IOR= Interaction Odds Ratio; CI=confidence interval; PTSD=post-traumatic stress disorder
Model covariates include any past-year mood disorder, any past-year anxiety disorder, any past-year drug use disorder, past-year nicotine dependence, age, race, education, marital status, employment status, and household income.
In multinomial logistic regression modeling, trauma-exposure/PTSD status was positively associated with past-year binge drinking and past-year hazardous drinking among women. These associations were found at all levels of the independent variable (reference: no trauma exposure) for all levels of each dependent variable (non-event: past-year non-drinking), after adjustment for all study covariates. Although a similar pattern of positive associations between trauma-exposure/PTSD status and past-year binge drinking and past-year hazardous drinking was observed among men, there were some exceptions. Specifically, before past-year PTSD was not associated with elevated odds for either high-frequency binge drinking or low-frequency binge drinking, and past-year PTSD was not associated with elevated odds for past-year non-binge drinking, past-year low-frequency binge drinking, or past-year non-hazardous drinking.
IORs indicated that the gender-specific associations between trauma exposure and past-year non-binge drinking (IOR=1.56, 95%CI=1.24–1.96), low-frequency binge drinking (IOR=1.81, 95%CI=1.16–2.85), and high-frequency binge drinking (IOR=1.51, 95%CI=1.03–2.21) were stronger for women compared to men. Similarly, the associations between past-year PTSD and non-binge drinking (IOR=1.89, 95%CI=1.29–2.77) and low-frequency binge drinking (IOR=3.28, 95%CI=1.60–6.71) were stronger for women compared to men (see Figure 1). Gender-related differences in the association between before past-year PTSD and binge drinking were not observed.
Gender-related differences were also observed with respect to past-year hazardous drinking. Specifically, both trauma exposure and past-year PTSD were more strongly associated with hazardous drinking (trauma exposure: IOR=1.53, 95%CI=1.15–2.04; past-year PTSD: IOR=1.82, 95%CI=1.15–2.88) and non-hazardous drinking (trauma exposure: IOR=1.61, 95%CI=1.28–2.03; past-year PTSD: IOR=2.04, 95%CI=1.37–3.03) among women as compared to men (Figure 2). Gender-related differences in the association between before past-year PTSD and hazardous drinking were not observed.
Discussion
The findings from the current study are consistent with previous research studies that have documented associations between trauma exposure, PTSD, and problematic alcohol use. These findings also are consistent with research documenting gender-related differences in the associations between PTSD and alcohol-use disorders (Helzer et al., 1987; Kessler et al., 1997; Ouimette et al., 2000), and extend this research to include binge and hazardous drinking. Finally, we provide additional empirical support for the association between trauma exposure without PTSD and binge and hazardous drinking. This relationship was the most consistent finding in the current study-observed across both men and women (although with stronger associations found among women), and across all levels of drinking.
Several possible explanations could account for the elevated odds among trauma-exposed women with and without PTSD of engaging in binge and hazardous drinking. One explanation could be that men and women cope with the experience of traumatic life events differently. Researchers have found that women use less effective strategies to cope with trauma compared to men (Ptacek et al., 1994; Tamres et al., 2002). For example, women have been shown to engage in more emotion- and avoidance-focused coping than men (Matud, 2004; Weidner & Collins, 1993), and these coping styles are associated with problematic alcohol use (Cooper et al., 1998). In addition, if trauma-exposed women experience recent life stressors, it could make effective coping even more difficult and further increase their risk for engaging in problematic drinking. This is consistent with research findings reported by Young-Wolf et al. (2012) who found that recent stressors were associated with problematic drinking among women with childhood maltreatment, but not for men with childhood maltreatment.
Alternatively, compared to men, women who engage in binge and hazardous drinking may be at a greater risk of experiencing certain traumatic events, particularly rape and sexual assault, and in turn developing PTSD. Women who heavily consume alcohol may be more likely to be targeted by perpetrators (Abbey et al., 2004). Moreover, alcohol and other substances may lead to impaired decision making which can increase a woman’s vulnerability of being victimized (Logan et al., 2002). Therefore, although women may be more likely to drink to cope with their traumas and subsequent symptoms of PTSD, their heavy alcohol use may increase their risk of experiencing rape and sexual assault, and subsequently developing PTSD.
Finally, the gender-related differences observed in the association between trauma/PTSD and binge and hazardous drinking could reflect differences between men and women in the biological mechanisms underlying both PTSD and alcohol use (Norman et al., 2012). For example, researchers utilizing the Vietnam Era Twin Study have observed common genetic factors among those with comorbid PTSD and alcohol-use disorders (e.g., Macleod et al., 2001; Xien et al., 2000). More recently, Sartor et al. (2010) found that the genetic factors that contribute to trauma exposure and PTSD account for approximately 30% of the genetic variance in alcohol-use disorders among a sample of female twins. Additional research examining the underlying genetic contributions of these two disorders is needed. Nevertheless, the extent to which there are differences between men and women in the genetic overlap between PTSD and alcohol-use disorders could in part explain results obtained in the current study. Similarly, additional research is needed to examine the extent to which gender-related differences might relate to hormonal factors differing between men and women.
The findings from the current study provide important information about alcohol-related problems associated with trauma exposure and PTSD. Although trauma-exposed individuals with and without PTSD may not necessarily meet diagnostic criteria for an alcohol-use disorder, they may nevertheless be engaging in problematic alcohol use, including binge and hazardous drinking, and this may be particularly so for women. Numerous mental and physical health problems are associated with binge and hazardous drinking (Naimi et al., 2003). Furthermore, binge and hazardous drinking may lead to the subsequent development of alcohol-use disorders (Kuntsche et al., 2004; Standridge et al., 2004). This information can aid in prevention and intervention efforts for individuals who have been exposed to traumatic events who may go on to develop PTSD. Specifically, individuals seeking treatment could be screened early on for current alcohol use, and could be monitored to ensure that any drinking does not become problematic. In addition, trauma-exposed individuals with and without PTSD could be informed about increased risk for binge and hazardous drinking and its adverse effects as part of existing trauma-focused treatment interventions for these individuals.
One of the most consistent findings across gender groups from the current study was among individuals who were exposed to trauma but who did not meet diagnostic criteria for PTSD: for both men and women, trauma exposure (without PTSD) was associated with all levels of binge and hazardous drinking. Furthermore, these associations were stronger among women compared to men. This association could be due to other co-occurring disorders confounding the relationship between trauma exposure and binge/hazardous drinking (Sartor et al., 2010). However, Sartor et al. (2010) observed a significant association between trauma/PTSD and alcohol-use disorders even after controlling for disorders commonly co-morbid with PTSD, including major depressive disorder, conduct disorder, nicotine, and cannabis abuse. Another possibility could be because trauma-exposed individuals, while not exhibiting symptoms of PTSD as a result of trauma exposure, were still experiencing negative affect which may have resulted in an increased risk of engaging in problematic alcohol use. Future research is needed to fully examine the underlying reasons that account for the association between trauma exposure (without PTSD) and problematic alcohol use. Nevertheless, together, these results build upon research that has documented associations between trauma exposure (without PTSD) and alcohol-use disorders (e.g., Breslau et al., 1997; Fetzner et al., 2011; Sartor et al., 2010) to include binge and hazardous drinking, and how there are gender-related differences in these associations. It also underscores the importance of focusing on individuals who have experienced traumatic events but who do not meet diagnostic criteria for PTSD. Despite not meeting criteria, they may engage in problematic alcohol use. Thus, intervention efforts designed to target PTSD should be broadened to include exposure to traumatic events, as trauma-exposed individuals may be at elevated risk for engaging in problematic alcohol use. These individuals could benefit from clinical interventions which emphasize problematic alcohol consumption following trauma exposure.
Several limitations exist. Given the cross-sectional nature of the study, causality cannot be determined. While researchers have discussed how women might develop PTSD prior to their problematic alcohol use (Stewart et al., 2002), we could not examine the temporal ordering of these conditions/behaviors (i.e., [1] how baseline drinking behavior may impact trauma exposure or the development of PTSD over time; and, [2] how baseline trauma/PTSD status may contribute to changes in drinking behavior over time) because trauma and PTSD data were not collected at both Waves 1 and 2 of the NESARC survey.. Additionally, cross-sectional data precludes the calculation of the relative risk, a measure which more accurately reflects the true strength of the association between exposure and disease. Although it is appropriate to calculate the odds ratio for these cross-sectional data, the odds ratio may exaggerate the strength of the exposure-disease association when the outcome is not rare (i.e., greater than 10% prevalence, as in this study). Thus, our results should be interpreted with caution. Given these limitations inherent to cross-sectional designs (temporality issues and the odds ratio vis a vis the relative risk), studies that employ longitudinal designs are imperative in future work. Another limitation is that we could not assess the degree to which subsyndromal (or partial) PTSD among trauma-exposed individuals who did not meet full diagnostic criteria for PTSD contributed to the observed associations between trauma exposure (in the absence of PTSD) and problematic alcohol use. Finally, these results may not generalize to populations that were underrepresented or excluded from the nationally representative sample (e.g. military members and institutionalized persons); work that focuses on these populations specifically is warranted.. In additional to longitudinal designs, future research might explore whether PTSD symptom clusters are differentially associated with binge and hazardous drinking, and if there are gender-related differences in these associations. Such research is important given seemingly inconsistent findings (McFall et al., 1992; Stewart et al., 1999), which could in part reflect the samples studied. Lastly, future research might also examine whether specific events (e.g., childhood trauma versus natural disasters) are more strongly associated with binge and hazardous drinking among men and women with and without PTSD, as past research has documented differences in relation to alcohol abuse and dependence (Fetzner et al., 2011).
In conclusion, our findings add to the existing literature on trauma exposure, PTSD, and alcohol use by focusing on binge and hazardous drinking and gender-related differences in the associations between these two types of drinking and trauma exposure/PTSD. As a result of these research findings, we believe that there should be increased awareness among those in the mental health field and society at large of the possible risks associated with trauma exposure and PTSD. Given that exposure to traumatic events is common in the United States, researchers should continue to extend examinations into this important topic.
Supplementary Material
Acknowledgments
This research was funded in part by a NIAAA grant RL1 AA017539 (MNP), T-32 postdoc fellowship from NIMH (5-T32-MH01423537; CEP) and by the Office of Academic Affiliations, Veterans Affairs Advanced Fellowship Program in Mental Illness Research and Treatment, Department of Veterans Affairs (LKK).
Footnotes
Contributors: Drs. Pilver and Potenza designed the study. Dr. Pilver conducted statistical analyses and contributed to the first draft of the manuscript. Dr. Kachadourian conducted literature research and contributed to the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
Role of Funding Source: The funding agencies did not provide any input as to the content of this manuscript. This manuscript is the product of the authors’ contributions only.
Conflict of Interest: The authors report no conflict of interest with respect to content of the manuscript. Dr. Potenza lists the following disclosures. Dr. Potenza has consulted for Lundbeck and Ironwood pharmaceuticals; received research support from Mohegan Sun Casino, Psyadon pharmaceuticals, the National Center for Responsible Gambling, and the National Institutes of Health (NIH); has participated in surveys, mailings, or telephone consultations related to drug addiction, impulse-control disorders, or other health topics; has consulted for gambling, legal and governmental entities on issues related to addictions or impulse-control disorders; has provided clinical care in the Connecticut Department of Mental Health and Addiction Services Problem Gambling Services Program; has performed grant reviews for the NIH and other agencies; has guest edited journal sections; has given academic lectures in grand rounds, Continuing Medical Education events, and other clinical or scientific venues; and has generated books or book chapters for publishers of mental health texts.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abbey A, Zawacki T, Buck PO, Clinton AM, McAuslan P. Sexual assault and alcohol consumption: what do we know about their relationship and what types of research are still needed? Aggression and Violent Behavior. 2004;9:271–303. doi: 10.1016/S1359-1789(03)00011-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Boscarino JA, Adams RE, Galea S. Alcohol use in New York after the terrorist attacks: A study of the effects of psychological trauma on drinking behavior. Addictive Behaviors. 2006;31:606–621. doi: 10.1016/j.addbeh.2005.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady KT, Killeen T, Saladin M, Dansky BS, Becker S. Comorbid substance abuse and PTSD: Characteristics of women in treatment. American Journal on Addictions. 1994;3:160–164. [Google Scholar]
- Breslau N, Chilcoat HD, Kessler RC, Peterson EL, Lucia VC. Vulnerability to assaultive violence: Further specification of the sex difference in post-traumatic stress disorder. Psychological Medicine. 1999;29:813–821. doi: 10.1017/s0033291799008612. [DOI] [PubMed] [Google Scholar]
- Breslau N, David GC, Andreski P, Peterson EL. Sex differences in posttraumatic stress disorder. Archives of General Psychiatry. 1997;54:1044–1048. doi: 10.1001/archpsyc.1997.01830230082012. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and\posttraumatic stress disorder in the community. Archives of General Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Harvey AG. Gender differences in the relationship between acute stress disorder and posttraumatic stress disorder following motor vehicle accidents. Australian and New Zealand Journal of Psychiatry. 2003;37:226–229. doi: 10.1046/j.1440-1614.2003.01130.x. [DOI] [PubMed] [Google Scholar]
- Carver C, White T. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: the BIS/BAS scales. Journal of Personality and Social Psychology. 1994;67:319–333. [Google Scholar]
- Cerdá M, Tracy M, Galea S. A prospective population based study of changes in alcohol use and binge drinking after a mass traumatic event. Drug and Alcohol Dependence. 2011;115:1–8. doi: 10.1016/j.drugalcdep.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper ML, Russell M, George WH. Coping, expectancies, and alcohol abuse: A test of social learning formulations. Journal of Abnormal Psychology. 1988;97:218–230. doi: 10.1037//0021-843x.97.2.218. [DOI] [PubMed] [Google Scholar]
- Dansky BS, Saladin ME, Brady KT, Kilpatrick DG, Resnick HS. Prevalence of victimization and posttraumatic stress disorder among women with substance use disorders: comparison of telephone and in-person assessment samples. International Journal of the Addictions. 1995;30:1079–1099. doi: 10.3109/10826089509055829. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Li T. Quantifying the risks associated with exceeding recommended drinking limits. Alcoholism: Clinical and Experimental Research. 2005;29:902–908. doi: 10.1097/01.alc.0000164544.45746.a7. [DOI] [PubMed] [Google Scholar]
- Fetzner MG, McMillan KA, Sareen J, Asmundson GJG. What is the association between traumatic life events and alcohol abuse/dependence in people with and withouth PTSD? Findings from a nationally representative sample. Depression and Anxiety. 2011;28:632–638. doi: 10.1002/da.20852. [DOI] [PubMed] [Google Scholar]
- Freedman SA, Gluck N, Tuval-Mashiach R, Brandes D, Peri T, Shalev AY. Gender differences in response to traumatic events: A progressive study. Journal of Traumatic Stress. 2002;15:407–413. doi: 10.1023/A:1020189425935. [DOI] [PubMed] [Google Scholar]
- Fullilove MR, Fullilove RE, III, Smith M, Winkler K, Michael C, Panzer PG, Wallace R. Violence, trauma, and posttraumatic stress disorder among women drug users. Journal of Traumatic Stress. 1993;6:533–543. [Google Scholar]
- Gray JA. A critique of Eysenck’s theory of personality. In: Eysenck HJ, editor. A model for personality. Berlin: Springer-Verlag; 1981. pp. 246–276. [Google Scholar]
- Hamilton KR, Sinha R, Potenza MN. Hazardous drinking and dimensions of impulsivity, behavioral approach, and inhibition in men and women. Alcoholism: Clinical and Experimental Research. 2012;36:958–66. doi: 10.1111/j.1530-0277.2011.01708.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helzer JE, Robins LN, McEvoy L. Post-traumatic stress disorder in the general population: Findings of the Epidemiologic Catchment Area Survey. The New England Journal of Medicine. 1987;317:1630–1634. doi: 10.1056/NEJM198712243172604. [DOI] [PubMed] [Google Scholar]
- Holbrook TL, Hoyt DB. The impact of major trauma: Quality-of-life outcomes are worse in women than in men, independent of mechanism and injury severity. Journal of Trauma. 2004;56:284–290. doi: 10.1097/01.TA.0000109758.75406.F8. [DOI] [PubMed] [Google Scholar]
- Holmila M, Raitasalo K. Gender differences in drinking: why do they still exist? Addiction. 2005;100:1763–1769. doi: 10.1111/j.1360-0443.2005.01249.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC. Posttraumatic stress disorder: The burden to the individual and to society. Journal of Clinical Psychiatry. 2000;61:4–14. [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Archives of General Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank RG, Leaf PJ. The epidemiology of co-occurring addictive and mental disorders: Implications for prevention and service utilization. 1996;66:17–31. doi: 10.1037/h0080151. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the\ National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Keyes K, Grant B, Hasin D. Evidence for a closing gender gap in alcohol use, abuse, and dependence in the United States population. Drug Alcohol Dependence. 2008;93:21–29. doi: 10.1016/j.drugalcdep.2007.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuntsche E, Rehm J, Gmel G. Characteristics of binge drinkers in Europe. Social Science & Medicine. 2004;59:113–127. doi: 10.1016/j.socscimed.2003.10.009. [DOI] [PubMed] [Google Scholar]
- Logan TK, Walker R, Cole J, Leukefeld C. Victimization and substance abuse among women: Contributing factors, interventions, and implications. Review of General Psychology. 2002;6:325–397. [Google Scholar]
- McLeod DS, Koenen KC, Meyer JM, Lyons MJ, Eisen S, True W, et al. Genetic and environmental influences on the relationship among combat exposure, posttraumatic stress disorder symptoms, and alcohol use. Journal of Trauma Stress. 2001;14:259–275. doi: 10.1023/A:1011157800050. [DOI] [PubMed] [Google Scholar]
- Matud MP. Gender differences in stress and coping styles. Personality and Individual Differences. 2004;37:1401–1415. [Google Scholar]
- McFall ME, Mackay PW, Donovan DM. Combat-related posttraumatic stress disorder and severity of substance abuse in Vietnam Veterans. Journal of Studies on Alcohol. 1992;53:357–363. doi: 10.15288/jsa.1992.53.357. [DOI] [PubMed] [Google Scholar]
- McDevitt-Murphy ME, Williams JL, Bracken KL, Fields JA, Monahan CJ, Murphy JG. PTSD symptoms, hazardous drinking, and health functioning among U.S. OEF and OIF veterans presenting to primary care. Journal of Traumatic Stress. 2010;23:108–111. doi: 10.1002/jts.20482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naimi TS, Brewer RD, Mokdad A, Clark D, Serdula MK, Marks JS. Binge drinking among US adults. Journal of the American Medical Association. 2003;289:70–75. doi: 10.1001/jama.289.1.70. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. National Institute of Alcohol Abuse and Alcoholism Council approves definition of binge drinking. NIAAA Newsletter. 2004 Winter;:3. Retrieved October 25, 2007, from http://pubs.niaaa.nih.gov/publications/Newsletter/winter2004/Newsletter_Number3.htm.
- Norris FH. Epidemiology of trauma: Frequency and impact of different potential traumatic events on different demographic groups. Journal of Consulting and Clinical Psychology. 1992;60:409–419. doi: 10.1037//0022-006x.60.3.409. [DOI] [PubMed] [Google Scholar]
- Norris FH, Foster JD, Weisshaar DL. The epidemiology of gender differences in PTSD across developmental, societal, and research contexts. In: Kimerling R, Ouimette P, Wolfe J, editors. Gender and PTSD. New York, NY, US: Guilford Press; 2002. pp. 3–42. [Google Scholar]
- Norman SB, Myers US, Wilkins KC, Goldsmith AA, Hristova V, Huang Z, et al. Review of biological mechanisms and pharmacological treatments of comorbid PTSD and substance use disorder. Neuropharmacology. 2012;62:542–551. doi: 10.1016/j.neuropharm.2011.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Applied Studies. DHHS Publication No. SMA 06-4194, NSDUH Series H-30. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2006. Results from the 2005 National Survey on Drug Use and Health: National findings. 2 Office of Applied Studies. [Google Scholar]
- Olff M, Langeland W, Draijer N, Gersons BPR. Gender Differences in Posttraumatic Stress Disorder. Psychological Bulletin. 2007;133:183–204. doi: 10.1037/0033-2909.133.2.183. [DOI] [PubMed] [Google Scholar]
- Ouimette PC, Kimerling R, Shaw J, Moos RH. Physical and sexual abuse among women and men with substance use disorders. Alcoholism Treatment Quarterly. 2000;18:7–17. [Google Scholar]
- Ptacek JT, Smith RE, Dodge KL. Gender differences in coping with stress: When stressor and appraisals do not differ. Personality and Social Psychology Bulletin. 1994;20:421–430. [Google Scholar]
- Rice C, Mohr CD, Del Boca FK, Mattson ME, Young L, Brady K, Nickless C. Self- reports of physical, sexual, and emotional abuse in an alcoholism treatment sample. Journal of Studies on Alcohol. 2001;62:114–123. doi: 10.15288/jsa.2001.62.114. [DOI] [PubMed] [Google Scholar]
- Sartor CE, McCutcheon VV, Pommer NE, Nelson EC, Duncan AE, Waldron M, Bucholz KK, Madden PAF, Heath AC. Posttraumatic stress disorder and alcohol dependence in young women. Journal of Studies on Alcohol and Drugs. 2010;71:800–818. doi: 10.15288/jsad.2010.71.810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sartor CE, McCutcheon VV, Pommer1 NE, Nelson EC, Grant JD, Duncan AE, et al. Common genetic and environmental contributions to post traumatic stress disorder and alcohol dependence in young women. Psychological Medicine. 2011;41:1497–1505. doi: 10.1017/S0033291710002072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharkansky EJ, Brief DJ, Peirce JM, Meehan JC, Mannix LM. Substance abuse patients with posttraumatic stress disorder (PTSD): Identifying specific triggers of substance use and their associations with PTSD symptoms. Psychology of Addictive Behaviors. 1999;13:89–97. [Google Scholar]
- Seifert SA. Substance use and sexual assault. Substance Use and Misuse. 1999;34:935–945. doi: 10.3109/10826089909037250. [DOI] [PubMed] [Google Scholar]
- Standridge JB, Zylstra RG, Adams SM. Alcohol consumption: An overview of benefits and risks. Southern Medical Journal. 2004;97:664–672. doi: 10.1097/00007611-200407000-00012. [DOI] [PubMed] [Google Scholar]
- Stein DC, Chiu WT, Hwang I, Kessler RC, Sampson N, Alonso J, et al. Cross-National Analysis of the Associations between Traumatic Events and Suicidal Behavior: Findings from the WHO World Mental Health Surveys. PLoS ONE. 2010;5(5):e10574. doi: 10.1371/journal.pone.0010574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MB, Walker JR, Hazen AL, Forde DR. Full and partial posttraumatic stress disorder: Findings from a community survey. The American Journal of Psychiatry. 1997;154:1114–1119. doi: 10.1176/ajp.154.8.1114. [DOI] [PubMed] [Google Scholar]
- Stermac L, Du Mont J, Dunn S. Violence in known assailant sexual assaults. Journal of Interpersonal Violence. 1998;13:398–412. [Google Scholar]
- Stewart SH, Conrod PJ, Pihl RO, Dongier M. Relations between posttraumatic stress symptom dimensions and substance dependence in a community-recruited sample of substance-abusing women. Psychology of Addictive Behaviors. 1999;13:78–88. [Google Scholar]
- Stewart SH, Ouimette P, Brown PJ. Gender and the comorbidity of PTSD with substance use disorders. In: Kimerling R, Ouimette P, Wolfe J, editors. Gender and PTSD. New York, NY, US: Guilford Press; 2002. pp. 232–270. [Google Scholar]
- Swett C, Cohen C, Surrey J, Compaine A, Chavez R. High rates of alcohol use and history of physical and sexual abuse among women outpatients. The American Journal of Drug and Alcohol Abuse. 1991;17:49–60. doi: 10.3109/00952999108992809. [DOI] [PubMed] [Google Scholar]
- Tamres LK, Janicki D, Helgeson VS. Sex differences in coping behavior: A meta-analytic review and an examination of relative coping. Personality and social Psychology Review. 2002;6:2–30. [Google Scholar]
- Weidner G, Collins RL. Gender, coping and health. In: Krohne H, editor. Attention and avoidance: strategies in coping with aversiveness. Seattle, WA: Hogrefe & Huber; 1993. pp. 241–265. [Google Scholar]
- Wilsnack RW, Wilsnack SC. Gender and alcohol: Individual and social perspectives. Piscataway, NJ, US: Rutgers Center of Alcohol Studies; 1997. [Google Scholar]
- Wilsnack R, Vogeltanz N, Wilsnack S, Harris T, Ahlström S, Bondy S. Gender differences in alcohol consumption and adverse drinking consequences: cross-cultural patterns. Addiction. 2000;95:251–265. doi: 10.1046/j.1360-0443.2000.95225112.x. [DOI] [PubMed] [Google Scholar]
- Xian H, Chantarujikapong SI, Scherrer JF, Eisen SA, Lyons MJ, Goldberg J, et al. Genetic and environmental influences on posttraumatic stress disorder, alcohol and drug dependence in twin pairs. Drug Alcohol Depend. 2000;61:95–102. doi: 10.1016/s0376-8716(00)00127-7. [DOI] [PubMed] [Google Scholar]
- Young-Wolff KC, Kendler KS, Prescott CA. Interactive effects of childhood maltreatment and recent stressful life events on alcohol consumption in adulthood. J Stud alcohol Drugs. 2012;73:559–69. doi: 10.15288/jsad.2012.73.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.