Abstract
Poisoning is a significant public health threat as the second leading cause of injury-related death in the US. Disagreements on cause of death determination may have widespread implications across several realms of public health including policy and prevention efforts, interpretation of the poisoning literature, epidemiologic data analysis, medical-legal case outcomes, and individualized autopsy interpretation. We aimed to test agreement between the cause of death determined by the medical examiner (ME) and a medical toxicologist (MT) adjudication panel (MTAP) in cases of poisoning. This retrospective 7-year study evaluated all deaths attributed to poisoning in one large urban catchment area. Cross-matched data were obtained from Department of Vital Statistics and the Poison Control Center (PCC). Out of >380,000 deaths in the catchment area over the study period, there were 7050 poisonings in the Vital Statistics database and 414 deaths reported to PCC. Cross-matching yielded 321 cases for analysis. The ME and MTAP concurred on cause of death in 66%, which was only fair agreement (κ 0.25, CI 0.14–0.38). Factors associated with the likelihood of agreement were peri-mortem fire exposures, prehospital cardiac arrest, and timing of drug toxicity (chronic versus acute). In conclusion, agreement for poisoning cause of death between specialties was much lower than expected. We recommend an improved formal process of information sharing and consultation between specialties to assure that all existing information is analyzed thoroughly to enhance cause of death certainty.
Keywords: Poisoning, Medical examiner, Toxicology, Cause of death
1. Introduction
Poisoning, typically defined as injury from exposure to drugs, chemical, or toxins, remains a significant and growing public health threat. Based on recent data from the Centers for Disease Control and Prevention, poisoning has moved into second place for leading causes of injury-related death in the United States, only ranking behind motor vehicle collisions [1]. According to the American Heart Association, poisoning is the leading cause of cardiac arrest in victims under age 45 [2]. Poisoning affects a wide variety of races, ethnicities, ages, and social strata [3]. The World Health Organization placed poisoning amongst the top 15 causes of death for persons ages 5–44 years old and estimated that 99% of poisoning fatalities worldwide occur in developing countries [4]. In 2007, there were over 2.4 million suspected poisonings referred to Poison Control Centers (PCC) in the United States, of whom 1597 (0.1%) died and 1239 (78%) were determined to be poison related fatalities by a panel of medical toxicologists [5]. Despite mandatory reporting of poisoning under the Health Code and State Public Health Law in the catchment area of study (Health Code Sections 11.03 and 11.04, 10 RR Section 2.10 and Public Health Law Section 2130), data collected likely significantly underestimate the actual incidence of poisoning due to the passive nature of the PCC reporting system [6].
Epidemiologic studies customarily reflect reliance upon the official medical examiner (ME) assessment of poisoning related fatality (PRF) as gold standard [7]. However, a critical role of the clinical responsibilities of the medical toxicologist (MT) is to reduce PRF on a case-by-case basis, which typically occurs either through consultation using a medical toxicology service or in collaboration with a PCC. Indeed, clinical management of poisoned patients as well as clinical studies or case series of poisoning management may represent the assessment of the MT alone [5,8]. It is unclear whether the assessment of causality in PRF would be similar if made by an MT or an ME. Disagreement on cause of death determination may have widespread implications across several realms of public health including policy and prevention efforts, interpretation of the poisoning literature, epidemiologic data analysis, medical-legal case outcomes, and individualized autopsy interpretation.
The goal of this study was to compare the assessments of PRF in cases that were independently evaluated by both an ME and an MT in an urban setting with a relatively high rate of death due to poisoning. The specific aim was to test agreement between the cause of death determined by the ME and an MT adjudication panel (MTAP) in cases of PRF. We hypothesized that there would be excellent agreement between the two evaluations.
2. Materials and methods
2.1. Study design, setting
This was a retrospective study involving data collected from a 7-year period (2000–06). All human deaths from a single large metropolitan city that were attributed to poisoning were analyzed regardless of age using cross-matched databases from two sources covering the same catchment area: the Department of Vital Statistics and the regional Poison Control Center (PCC). The number of deaths per year in the catchment area was >55,000. The referral volume for the PCC is approximately 75,000 cases annually.
2.2. Case selection
Deaths from all causes were eligible for inclusion from both databases. An encrypted aggregate database comprising all ME cases with death from poisoning as the final cause of death, was provided to the study investigators by the Department of Vital Statistics. Data from the Department of Vital Statistics was determined by final causes of death from ME-determined ICD-10 codes, and were obtained with IRB approval (protocol #06-069). No coroners were involved in cause of death determination. PCC electronic medical records were provided for all reported deaths with suspicion of poisoning over the same time period, again with IRB approval. A cross-matched database was then created by the Department of Vital Statistics using de-identified case data that included ME case number (if available), date of death, age, and gender. As a data quality control measure, only exact case matches (i.e., exact age, exact date of death) were included in the final database for analysis.
2.3. Data collected
Cases that were successfully cross-matched underwent data-extraction from the PCC electronic medical record by analysis of free-text medical data entry by one trained reviewer. Extracted data included demographics (age, gender), co-morbidities (coronary disease, congestive heart failure, diabetes, hypertension, chronic obstructive pulmonary disease), peri-mortem circumstances (burns, trauma), drug exposures by class (i.e., sympathomimetics, opioids, caustics, etc.), timing of exposure (acute versus chronic toxicity, prehospital arrest) and clinical data (suicidal intent, antidote administration).
2.4. Definitions and adjudication
The study outcome of interest was PRF, defined in two ways: PRF according to the ME and according to the MT. PRF according to the ME was defined by the ICD-10 code listed as the primary cause of death based on standard reporting from the Department of Vital Statistics; if the ICD-10 code was directly related to poisoning (see Table 1), then the death was identified as PRF according to the ME.
Table 1.
Medical examiner ICD-10 Codes included as cause of death due to PRF.
| F10–F19: mental and behavioral disorders due to psychoactive substance use |
| T36–T50: poisoning by drugs, medicaments, and biological substances |
| T51–T65: toxic effects of substances chiefly non-medicinal as to source |
| X40–X49: accidental poisoning by and exposure to noxious substances |
| X60–X69: intentional self-poisoning |
| X85–X90: homicidal poisoning |
| Y10–Y19: poisoning by undetermined intent |
ICD, international classification of diseases; PRF, poison related fatality.
MT adjudication panel (MTAP): PRF according to the MT was defined by independent formal adjudication by three MTs with a range of clinical experience (3–25 years practicing clinical toxicology, all board certified by either the American Board of Emergency Medicine or the American Board of Osteopathic Emergency Medicine). MTAP determined PRF based on review of the PCC record. The PCC record has detailed clinical information for medical decision-making and typically includes ME pathology results if available, but does not include the underlying cause of death determination coded in the Vital Statistics database. All members of the MTAP were blinded to the underlying cause of death determination coded in the Vital Statistics database. After review of the PCC record, each MT was asked to determine the relationship between poisoning and the cause of death according to one of the following five categories: (a) probable/definite, (b) possible, (c) unclear, (d) improbable, or (e) definitely unrelated. For each case, these five determinations were then dichotomized into PRF (a or b) versus non-PRF (c, d, or e). Dichotomized data from two adjudicators was initially used to decide if the death was poison related. Disagreements were settled by adjudication from a 3rd senior MT.
2.5. Data analysis
Descriptive statistics for demographics of fatalities were calculated using percentages and means (± standard deviation). Agreement was assessed using κ statistics with 95% confidence intervals (CI). We calculated odds ratios (OR) with 95% CI, using the estimated standard error method. Significant trends in factor analysis were defined as p < 0.10. In the analysis of drug exposure class, the Bonferroni correction was used to adjust for multiple comparisons (total of 31 drug classes). Computer calculations were performed using SPSS version 17 software (SPSS Inc., Chicago, IL).
3. Results
3.1. Poisoning related fatalities
Out of >350,000 deaths that occurred in the catchment area during the study period, there were 7050 poisoning fatalities (73% male, mean age 43.6) in the Vital Statistics database and 414 fatalities (79% male, mean age 45.3) in the PCC database. The vast majority (99.3%) of poisoning deaths in the Vital Statistics database were cases referred to the ME. Of 414 PCC-reported fatalities, only 375 had sufficient data to allow matching of records between the Vital Statistics database. Matches were obtained in 321 cases, of which 256 had ME cause of death interpretations (i.e., 65 PCC cases resulting in fatality were not accepted for evaluation by the ME) and were thus analyzed for agreement. Selection of cases and matching for analysis of PRF agreement are outlined in Fig. 1.
Fig.1.
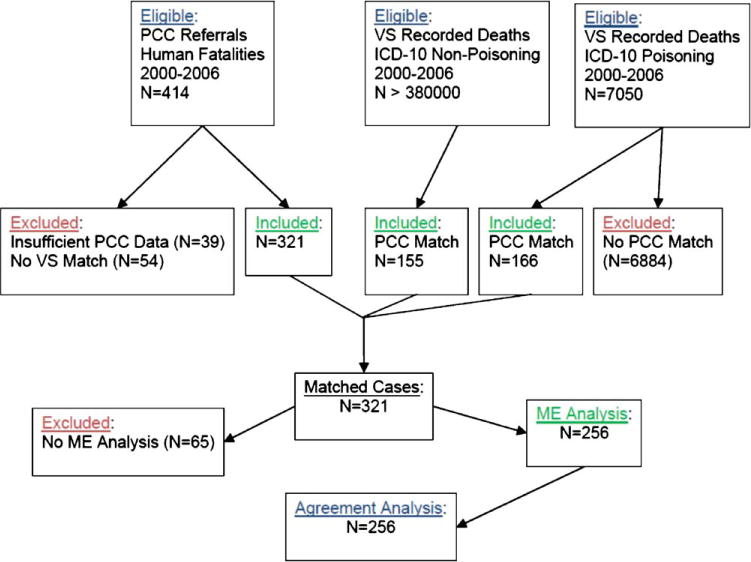
Case selection and matching process. Matching cases between databases from the PCC and the Department of VS is depicted here. Matched cases had entriesin both the PCC and VS databases as well as ME analysis. ICD, international classification of diseases; ME, medical examiner; N, number; PCC, poison control center; VS, vital statistics.
3.2. Agreement
Out of 256 matched cases, the ME and the MTAP agreed on 168 cases (66%). Agreement on poisoning as cause of death occurred in 120 cases (47%), non-poisoning as cause of death in 48 cases (19%) and disagreement occurred in 88 cases (34%). The κ agreement coefficient (range 0–1.0, higher number indicating better agreement) between the ME and the MTAP was 0.25 (95% CI 0.14–0.38), whereas inter-MT agreement occurred in 70–89% of cases (κ range 0.53–0.80, CI 0.45–0.89). Agreement between each of the three MTs and the ME occurred in 64%, 65%, and 67% of cases (p value not significant). Agreement data is outlined in Table 2.
Table 2.
Poison related fatality agreement in 256 database matches that included analysis by the medical examiner.
| PRF according to MTAP | PRF according to MEa
|
|
|---|---|---|
| Yes | No | |
| Yes | 120 (47%) | 42 (16%) |
| No | 46 (18%) | 48 (19%) |
PRF, poison related fatality; ME, medical examiner; MTAP, medical toxicology adjudication panel.
See Table 1 for definition according to ICD-10 codes.
3.3. Factors associated with cause of death interpretation
Factors associated with cause of death interpretation (i.e., agreement versus disagreement) were analyzed according to demographics, peri-mortem circumstances, drug exposures, timing of drug toxicity, and clinical events. Circumstances involving fires had 4-fold increased odds of disagreement (OR 4.0, p = 0.04) between the ME and the MTAP, while prehospital cardiac arrest was associated with 45% lower odds of disagreement (OR 0.55, p = 0.037). A full summary of the factor analysis based on ME/MTAP cause of death determination is itemized in Table 3. Based on univariate analysis, factors with impact (at least a trend toward significance) on cause of death interpretation are summarized in Table 4.
Table 3.
Factor analysis based on ME/MTAP agreement versus disagreement for cause of death.
| Factors | Total | Agreed | Disagreed | p value* |
|---|---|---|---|---|
|
| ||||
| Number or mean (% or SD) | ||||
| Demographics | ||||
| Mean age | 41.4 (17.2) | 40.1 (17.5) | 43.7 (16.3) | 0.12 |
| Male sex | 156 (60) | 106 (63) | 50 (57) | 0.33 |
| Co-morbidities | ||||
| CHF | 2 (1) | 1 (0.6) | 1 (1) | 1.0 |
| COPD | 4 (2) | 2 (1) | 2 (2) | 0.6 |
| Coronary disease | 7 (3) | 5 (3) | 2 (2) | 1.0 |
| Diabetes mellitus | 7 (3) | 4 (2) | 3 (3) | 0.7 |
| Hypertension | 17 (7) | 13 (8) | 4 (5) | 0.43 |
| Exposures | ||||
| Anticonvulsants | 22 (9) | 11 (7) | 11 (13) | 0.10a |
| APAP | 53 (21) | 39 (23) | 14 (16) | 0.17 |
| Caustics | 9 (4) | 9 (5) | 0 (0) | 0.03a |
| Opioids | 76 (29) | 53 (32) | 23 (26) | 0.37 |
| Sympathomimetics | 45 (17) | 26 (15) | 19 (22) | 0.22 |
| Circumstances | ||||
| Fires | 9 (4) | 3 (2) | 6 (7) | 0.04 |
| Trauma | 15 (6) | 10 (6) | 5 (6) | 1.0 |
| Timing | ||||
| Chronic toxicity | 32 (13) | 17 (10) | 15 (17) | 0.10 |
| Prehospital cardiac arrest | 92 (36) | 68 (40) | 24 (27) | 0.037 |
| Clinical data | ||||
| Antidote administration | 112 (45) | 77 (46) | 35 (40) | 0.35 |
| Suicidal Intent | 110 (44) | 70 (42) | 40 (47) | 0.51 |
| Total | 256 (100) | 168 (100) | 88 (100) | – |
CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; ME, medical examiner; MTAP, medical toxicology adjudication panel; PRF, poison related fatality; SD, standard deviation.
No trend or significance after Bonferroni correction.
p values based on χ2 (or Fisher’s exact test when appropriate) and independent samples t-test for categorical and continuous variables, respectively. Significant p values listed in bold.
Table 4.
Factors with impact* on cause of death interpretation between ME and MTAP.
| Factors | OR (95% CI)a |
|---|---|
| Agreement | |
| Prehospital cardiac arrest | 0.55 (0.3–0.97) |
| Disagreement | |
| Fires | 4.0 (1.01–16.5) |
| Chronic toxicity | 1.9 (0.9–3.9) |
CI, confidence intervals; ME, medical examiner; MTAP, medical toxicology adjudication panel; OR, odds ratio.
Odds for disagreement between ME and MTAP; thus factors with OR>1.0 are associated with disagreement whereas factors with OR<1.0 are associated with agreement.
Impact defined as at least a trend (p < 0.10) toward significance on univariate analysis from Table 3.
3.4. Case examples
The following three case examples demonstrate disagreements between the ME and MTAP with regards to cause of death. The following cases (all data from the PCC medical record) were chosen for description in order to elucidate the difficulties in the individual interpretation of suspected PRF. Two cases have been chosen where the ME ruled against PRF (Cases 1and 3), and one has been chosen in which MTAP adjudicated against PRF (Case 2).
3.5. Case 1
A 44 year-old woman with a history of chronic low back pain, type II diabetes mellitus, hypertension, and depression who had been taking large doses of acetaminophen (2.6 g every 4 h) for several weeks. She presented to the emergency department with upper gastrointestinal bleeding and hypotension. Initial laboratory values were significant for AST 11,272 (U/L), ALT 4529 (U/L), INR 4.2, creatinine 2.6 (mg/dL), total bilirubin 3.1 (mg/dL), arterial pH 7.38, lactate 6.6 mmol/L, and hematocrit 32%. Serum toxicology screens revealed acetaminophen concentration of 71 mcg/mL and salicylate of 11 mg/dL. Her clinical course was significant for a hematocrit drop 3 h later down to 20% and emergent upper endoscopy. In addition, she was treated with three doses of oral N-acetylcysteine, intravenous fluids, anti-emetics, activated charcoal and fresh frozen plasma. Despite treatment, the patient expired within hours after presentation. Autopsy revealed hepatic necrosis and confirmed upper gastrointestinal hemorrhage. ME cause of death was listed as “Y34: Unspecified event, undetermined intent,” while the MTAP panel unanimously adjudicated in favor of PRF.
3.6. Case 2
A 52 year-old man with a history of diabetes mellitus, chronic foot ulcerations, hypertension, arthritis, liver cirrhosis and access to chronic medications including acetaminophen/hydrocodone, temazepam, indomethacin, and tramadol, was found unresponsive in the evening by family after having 2 days of diarrhea. Emergency Medical Services found him lying in his bathtub with his head above water level, at which time they administered intravenous dextrose, naloxone, and thiamine without any response. He arrived in the emergency department 40 min after being found, at which time the cardiac monitor revealed atrial fibrillation, and vital signs revealed: hypotension (80/40 mmHg); tachycardia (120/min); agonal respirations (requiring bag-valve-mask ventilation); and hypothermia (temperature rectally 88.6 degrees Fahrenheit). Toxicology analysis included ethanol concentration of 8 mg/dL (one-tenth the legal intoxication level); negative serum screens for acetaminophen, and aspirin; and positive urine screens for opioids and benzodiazepines. Other laboratories were significant for hyperammonemia (131 mcg/dL), hyponatremia (128 mmol/L), acidosis (pH 6.8), leukocytosis with bandemia (white blood count 40 cells × 109/L with 42% neutrophils and 39% bands), and negative cardiac troponin. Chest radiograph and head computed tomography were normal.
His initial hospital course included endotracheal intubation, Foley catheter placement, nasogastric tube placement with activated charcoal administration, warming blankets, intravenous fluid resuscitation, and broad-pectrum antibiotics. In the Intensive Care Unit, he had anuria, and persistent shock requiring vasopressors. Less than 24 h after hospital arrival he suffered a cardiac arrest and was unable to be resuscitated. After pathology, the ME cause of death was listed as “Accidental poisoning by and exposure to alcohol,” while the MTAP adjudicated unanimously against PRF.
3.7. Case 3
34 year-old woman with a history of HIV disease presented to the emergency department with coma and suspected acute drug abuse. Emergency Medical Services administered intravenous naloxone, dextrose, and thiamine without response. Emergency Department vital signs were significant for respiratory failure (apnea), tachycardia (160 beats/min), and hyperthermia (rectal temperature 106 °F). Urine toxicology was positive for cocaine metabolite. Additional laboratory evaluation revealed leukocytosis, coagulopathy, and renal insufficiency. The initial hospital course included endotracheal intubation and vasopressor support for shock. After weeks in the Intensive Care Unit, despite receiving aggressive supportive care including empiric antibiotics, she developed disseminated intravascular coagulation, multisystem organ failure, and expired. Based on the above information the MTAP adjudicated in favor of PRF. However, after autopsy evaluation revealed evidence of bacterial meningitis, the medical examiner cause of death was listed as “G009: bacterial meningitis, unspecified.”
4. Discussion
Our data has identified disagreement between the ME and MT about cause of death in poisoning. We found that agreement between ME and MTAP was only fair (κ 0.26), whereas inter-MT agreement was moderate to substantial (κ range 0.53–0.80). Furthermore, we have identified factors associated with likelihood of agreement, including peri-mortem situations (fires, prehospital cardiac arrest) and timing of drug toxicity (chronic versus acute). Additionally, this data demonstrate that the vast majority of poisoning deaths in the Vital Statistics database are referrals to the ME (99.3% referred) and are not reported to the PCC (97.7% not reported).
Our results have identified three key factors that may confound determination of PRF between specialties. Peri-mortem fire exposures increased disagreement in cause of death determination (p = 0.04), which may be explained by the fact that there are many potentially life-threatening sequelae of fire exposures (i.e., smoke inhalation, carbon monoxide poisoning, cyanide poisoning, as well as morbidity caused by the burn itself), thus ascribing cause of death due to poisoning (instead of the burn injury, for example) in such cases becomes difficult. In addition, our data demonstrate that presence of chronic toxicity (i.e., not an acute exposure) demonstrated a trend (p < 0.10) towards enhanced disagreement, which may have multiple explanations such as any of the following: chronic drug toxicity typically can occur at lower serum concentrations than acute drug toxicity; chronic drug toxicity typically is a subtle clinical diagnosis; and chronic presentations are probably less likely to be recognized by clinicians without specialized training (in toxicology, for example). Conversely, we found that presence of prehospital cardiac arrest enhanced agreement between specialties (p = 0.04), which may echo a shared sentiment across specialties that PRF is more likely to occur in the prehospital setting.
Several complex variables may confound the interpretation of cause of death due to poisoning. For example, post-mortem toxicology testing typically assesses the presence and concentration of a drug or toxin after death. This information is used to understand the likely pharmacologic effects at the time of death. Several variables such as post-mortem redistribution or metabolism [9], cell lysis [10], the particular fluid sample collected [11], may cause changes in drug concentrations during the interval between the time of death and subsequent autopsy. Forensic toxicologists and forensic pathologists may interpret post-mortem drug concentrations in order to decide whether these drugs were incidental or contributory to the cause of death. The disagreements found between the various specialists in the present study may be explained in several ways, including interpretation in the line of daily work (ME) as opposed to a study protocol (MTAP), differential weighting of clinical data over forensic data, incomplete data availability for interpretation (e.g., Case 3), systematic bias existing in the interpretation of forensic toxicology data analyzed (e.g., pre-mortem versus post-mortem), and differences in the training background influencing the medical interpretation (i.e., clinical versus forensic).
One potential criticism of decisions based on autopsy and forensics may be that the interpreter “overcalls” PRF. For example, if pathology is normal and there is a modest but elevated postmortem concentration of methadone in the blood, one may be tempted to determine that methadone was the cause of death in the absence of other clear causes. However, our agreement data (see Table 2) show that disagreements occurred in almost identical proportions for “ME yes/MT no” (46 subjects, 18% of database matches) versus “MT yes/ME no” (42 subjects, 16% of database matches). In fact, there were relatively equal numbers of cases on each side of disagreement. This seems to refute the existence of one-sided “overcalling” by either specialty, and suggests that random differences more appropriately explain the equal dispersion of disagreement. Alternatively, other factors (e.g., clinical data, post-mortem interpretation, training background, experience) create disagreement error in both directions.
Our data demonstrate that only 2.4% of deaths coded by the Department of Vital Statistics with ICD-10 codes related to poisoning were found in the PCC database (166 out of 7050), suggesting substantial underreporting of poisoning deaths to the PCC. Previously, Linakis and Frederick [12] conducted a 4-year study comparing deaths from poisoning reported to the Rhode Island Medical Examiner with those reported to the area poison center. Not surprisingly, the medical examiner reported many more deaths: 369 compared to 45 reported by the poison center. Although the majority of these cases not reported to the poison center were victims who died at home, were pronounced dead on arrival to the hospital, or those in whom poisoning was not suspected until the post-mortem analysis, 79 patients who were never reported to the PCC were actually admitted to the hospital. In 10 of these cases, the authors suggested that a toxicology consultation might have altered the outcome.
Legal jurisdiction of death investigation in the United States is the responsibility of either coroners or the ME, depending on the state and/or county. The medical-legal autopsy is usually performed by a forensic pathologist, who establishes the cause of death. Cause of death is the physiologic agent or event necessary for death to occur and is represented by one or several unique ICD-10 code identifiers. The ME must make the best determination of the cause of death based on the available evidence, which typically includes access to the medical record, information from police such as photographs of a crime scene if available, forensic pathology data, and the autopsy report. Determination of cause of death may also have important legal consequences such as law enforcement investigation, life insurance payment, double-indemnity insurance clauses, religious burials, and liability suits in workplace disasters. Our data suggest that this determination may depend on the training background of the medical expert called upon to interpret cause of death.
The inter-MT interpreter reliability on the MTAP panel demonstrated moderate to substantial agreement (κ range 0.53–0.80). This variable inter-observer agreement amongst panel members may reflect the differential weighting of data (e.g., clinical versus forensic), systematic bias, clinical experience, or other factors. Despite this, we feel the utilization of formal adjudication to define PRF was appropriate for this study. Furthermore, the present study is not able to determine which interpretation, MT versus ME, was “more correct” or which best approximates “truth.” The sub-excellent agreement amongst MTs suggests the need for formal definitions in place to identify PRF in order to standardize this process for use in future study.
Our analysis has highlighted the complexity behind classifying cause of death due to poisoning and the important implications for public health policy and prevention efforts. Based on this data, we feel inclined to offer several recommendations moving forward. We recommend the establishment of formal definitions to identify PRF in order to standardize interpretation of cause of death. Additionally, enhanced communication between specialties of forensic pathology, law, and medical toxicology should be encouraged. These efforts may take the form of case conferences, enhanced exchange of ideas, adjudication and panel discussions, or improved formal guidelines on classification of cause of death.
4.1. Limitations
Some limitations to this dataset must be considered when interpreting our results. Differences in the definition of PRF between the ME and MTAP may have exacerbated disagreement. For this reason, enhanced communication between specialties of forensic pathology and medical toxicology should be encouraged. Additionally, underreporting to the PCC may have introduced a reporting bias due to the actual reporting process, which is voluntary, passive, and provided over the phone [6]. However, we feel that this limitation would have only biased toward the null as the most severe cases are likely reported to PCC and reviewed by the ME. In addition, omission of relevant ICD-10 codes may have excluded some cases from Vital Statistics available for the cross-matched database. However this was unlikely to factor into the actual interpretation and thus the agreement between the MTAP and the ME. An argument can be made that the MTAP members should have more diverse backgrounds; however the fact that all three members were board certified in one specialty (although notably from different training backgrounds) was intentional in order to compare the cause of death interpretation between medical toxicologists and the medical examiner. Other limitations to the interpretation of our results include possible incomplete data in the electronic PCC database, and complex decision-making that may not always be representable by one ICD-10 code.
5. Conclusions
In summary, in this large retrospective study, agreement for poisoning cause of death between specialties was much lower than expected, and there was no significant evidence of “overcalling” by one specialty. Factors associated with the highest likelihood of disagreement were peri-mortem fire exposures and chronic drug toxicity. Implications regarding the future of public health policy, poisoning prevention efforts, interpretation of poisoning literature, medical-legal disputes, and individualized autopsy results deserve further study. We recommend an improved formal process of information sharing and consultation between specialties to assure that all existing information is analyzed thoroughly to enhance cause of death certainty.
Acknowledgments
We would like to thank the New York Department of Vital Statistics for the preparation of the aggregate matching database used in the study.
Funding
This work was supported in part by the Speaker’s Fund for Biomedical Research: Towards the Science of Patient Care, awarded by the City of New York. The funding source had no role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Abbreviations
- PRF
poisoning related fatality
- PCC
poison control center
- MT
medical toxicologist
- ME
medical examiner
- MTAP
medical toxicologist adjudication panel
References
- 1.Centers for Disease Control and Prevention, Web-based Injury Statistics Query and Reporting System (WISQARS) [Online] National Center for Injury Prevention and Control, Centers for Disease Control and Prevention (producer); Available at: www.cdc.gov/ncipc/wisqars, 2003 (accessed 29.06.09) [Google Scholar]
- 2.American Heart Association Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, part 10.2: toxicology in emergency cardiovascular care. Circulation. 2005;112(Suppl. I):IV-126–IV-132. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services (USDHHS), Substance Abuse and Mental Health Services Administration, Office of Applied Studies, Drug Abuse Warning Network. The DAWN Report – trends in drug-related emergency department visits, 1994–2002 at a glance. Available at: dawninfo.samhsa.gov/old_-dawn/pubs_94_02/shortreports/files/DAWN_EDvisits_glance.pdf, 2003 (accessed 29.06.09)
- 4.Peden M, McGee K, Krug E, editors. Injury: A Leading Cause of the Global Burden of Disease. World Health Organization; Geneva: 2002. [Google Scholar]
- 5.Bronstein AC, Spyker DA, Cantilena LR, Jr, et al. 2007 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 25th Annual Report. Clin Toxicol (Phila) 2008;46:927–1057. doi: 10.1080/15563650802559632. [DOI] [PubMed] [Google Scholar]
- 6.Blanc PD, Kearney TE, Olson KR. Underreporting of fatal cases to a regional poison control center. West J Med. 1995;162:505–509. [PMC free article] [PubMed] [Google Scholar]
- 7.Vlahov D, Wang C, Ompad D, et al. Collaborative Injection Drug User Study: mortality risk among recent-onset injection drug users in five U.S. cities. Subst Use Misuse. 2008;43:413–428. doi: 10.1080/10826080701203013. [DOI] [PubMed] [Google Scholar]
- 8.Stolbach AI, Hoffman RS, Nelson LS. Mechanical ventilation was associated with acidemia in a case series of salicylate-poisoned patients. Acad Emerg Med. 2008;15:866–869. doi: 10.1111/j.1553-2712.2008.00205.x. [DOI] [PubMed] [Google Scholar]
- 9.Giaginis C, Tsantili-Kakoulidou A, Theocharis S. Quantitative structure-activity relationship (QSAR) methodology in forensic toxicology: modeling postmortem redistribution of structurally diverse drugs using multivariate statistics. Forensic Sci Int. 2009 doi: 10.1016/j.forsciint.2009.05.003. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 10.Oehmichen M, Hennig R, Meissner C. Near-drowning and clinical laboratory changes. Leg Med (Tokyo) 2008;10:1–5. doi: 10.1016/j.legalmed.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 11.Boonyoung S, Narongchai P, Junkuy A. The relationship of alcohol concentration in epidural or acute sub-dural hematoma compared with vitreous humor and femoral blood. J Med Assoc Thai. 2008;91:754–758. [PubMed] [Google Scholar]
- 12.Linakis LG, Frederick KA. Poisoning deaths not reported to the regional poison control center. Ann Emerg Med. 221993:1822–1828. doi: 10.1016/s0196-0644(05)80408-1. [DOI] [PubMed] [Google Scholar]


