Abstract
Purpose
To determine if oral fluoroquinolone exposure is associated with an increased hazard for having a retinal tear or detachment.
Methods
A retrospective cohort study was performed using individuals who met inclusion criteria from The Health Improvement Network (THIN) database. Cohorts were created for individuals who had a prescription written for either an oral fluoroquinolone or an oral β-lactam antibiotic (comparison group). Subjects were excluded if they had a previous diagnosis of a retinal tear or detachment (hereafter retinal break, or RB) or a procedure code to treat an RB, were in the practice for less than 365 days, had a previous prescription for either antibiotic within 365 days of the index date, or had intraocular surgery or a diagnosis of endophthalmitis within 90 days prior to the antibiotic prescription. Covariates of interest were age, gender, diabetes and year of index. The primary outcome measure of interest was the hazard ratio of undergoing a procedure to treat a RB within 7, 30, 90 or 365 days after exposure to an oral fluoroquinolone prescription versus an oral β-lactam prescription.
Results
After exclusions, 6,604,423 prescriptions (290,393 fluoroquinolone; 6,314,030 β-lactam) from 3,413,498 patients (247,073 fluoroquinolone; 3,303,641 β-lactam) and, 2,685 RB procedures were eligible for analysis (661 retinal tears, 2,024 retinal detachments). For fluoroquinolones, zero, one, five, and 23 retinal breaks occurred at the 7-, 30-, 90-, and 365-day time points, respectively. For β-lactam prescriptions, 7, 28, 87, 373 retinal breaks occurred at the 7-, 30-, 90-, and 365-day time points, respectively. Due to zero events occurring in the fluoroquinolone cohort during the 7-day observation period an unadjusted or an adjusted hazard ratio (and subsequent p-value or confidence intervals) were unable to be calculated. Univariate and multivariate analysis demonstrated that fluoroquinolones were not significantly associated with RB in the 30-, 90- or 365-day observation periods (30-day HR=0.78, p=0.80, 95% CI: 0 .11, 5.71; 90-day HR=1.25, p=0.63, 95% CI: 0.51, 3.08; 365-day HR= 1.35, p=0.16, 95% CI: 0.89 2.06).
Conclusions
Our results do not support an association between oral fluoroquinolone use and subsequent procedures to treat a retinal break.
Keywords: fluoroquinolones, retinal detachment, retinal tear, retinal break, cohort, Cox regression
Introduction
Fluoroquinolones (FQ) are a staple in the armamentarium of antibiotic therapies for infectious disease and annually one of the most commonly prescribed antibiotics.1 While efficacious and generally well tolerated, they are not without adverse effects. Because of their widespread use, the discovery of new adverse effects typically is met with great interest, as was certainly the case when a potentially landmark study done by Etminan and colleagues found an association between retinal detachments (RD) and fluoroquinolone use.2 Since its publication in mid-2012, two other recent reports have demonstrated conflicting results with one corroborating the findings of Etminan and another refuting.3,4 Due to the widespread use of fluoroquinolones and the severity of vision loss possible from retinal detachments, this issue has been of great concern and interest leading to numerous editorial comments regarding the implications for patient care.5-13 These concerning findings are particularly important in ophthalmology, where surgical patients—who are already at higher risk of retinal detachment— are frequently given topical fluoroquinolones post-operatively as prophylaxis against endophthalmitis due to their excellent ocular penetration.14
With regards to eye disease, previous case reports have linked fluoroquinolone use with conditions ranging from corneal perforations to optic nerve disease.15-17 The mechanism by which oral fluoroquinolone use would increase the risk of retinal detachment is unknown. Etminan et al. suggest that the known effect of fluoroquinolone on collagen dissolution, which is the proposed mechanism for increased risk of Achilles tendon rupture, could lead to early liquefaction of the vitreous gel, premature posterior vitreous detachment and subsequently increase the rate of RDs.2
Along this proposed pathogenic pathway, a necessary intermediate step preceding the rhegmatogenous retinal detachment is a retinal tear. When viewed this way, a retinal detachment is simply a progression of disease that if diagnosed acutely enough, would be found as a retinal tear. Acute, symptomatic tears are typically treated in the office and, similar to retinal detachments, have their own unique diagnosis and reparative procedure codes that are identifiable in medical administrative databases. Our study aims to examine the relationship between oral fluoroquinolone use and treatments for retinal breaks—defined as either a retinal tear or detachment—in a population-based medical database from the United Kingdom (UK).
Methods
Dataset
This is a retrospective cohort study using The Health Improvement Network (THIN) database which contains the de-identified electronic medical records of 11.1 million patients (3.7 million active) which currently collects from 562 general medical practices in the UK, covering 6.2% of the UK population. All patients who are registered with one of the 562 practices are included within THIN. The earliest THIN data starts in June 1994, and for this study is inclusive for data through January 2012. The database contains medical diagnoses, procedures, and laboratory and all outpatient pharmaceutical data. The population within THIN has been found to have good generalizability to the UK population as a whole with similar demographics, systemic disease rates and death rates.18 Because general practitioners (GP) in the UK coordinate their patients’ care, all medical services delivered by a specialist such as an ophthalmologist generates a notification to the GP specifying the diagnosis for which the patient was seen and any procedures performed at that visit. The GP then inputs the data into the patient's electronic medical record utilizing the Vision software system, which is retrieved by THIN. The National Health Service in the UK also requires that all outpatient prescriptions be administered by the GP, including those requested by specialists. This study was approved by the Scientific Review Committee for the THIN database and was deemed exempt from review by The University of Pennsylvania Institutional Review Board due to the de-identified nature of the data.
Cohorts
Cohorts for this study were defined by having a prescription written for fluoroquinolones (FQ) or β-lactam (BL) antibiotics between June 1994 and January 2012. Similar to the previous study, β-lactam antibiotics were chosen as a comparator group due to their similar clinical indications for usage, but without concern for the same mechanism of action on collagen which is suggested to increase the risk of RDs.2 To meet inclusion criteria, patients had to be registered with their general practitioner for at least 365 continuous days prior to the index date, which was defined as the date that the prescription of interest was written. Index dates for prescriptions with a previous prescription of either class of antibiotics within 365 days were excluded from the analysis. Patients were excluded from the cohort if they had any retinal tear or detachment (RB) diagnosis or procedure code on or before the prescription date. Also, patients who had both classes of antibiotic prescribed on the same index date were excluded. Lastly, any prescriptions written within the 90-day period following an intraocular surgery or a diagnosis of endophthalmitis were excluded because these conditions are known to increase the risk of retinal detachment. Patients were allowed to re-enter the cohort or even switch cohorts after 365 days assuming the second episode met the above eligibility criteria.
Outcomes and Covariates of Interest
Outcome events were defined by having a procedure code for an RB repair entered into the THIN database during the observation period of interest. RBs that did not have an associated procedure for a repair were not included in the analysis due to the possibility of an untreated RB being chronic or treated prior to entry into THIN. Also, a strict definition of codes was created to lessen the possibility that a procedure was performed for a RB not associated with a primary rhegmatogenous mechanism (i.e. exudative or tractional retinal detachments.) Procedure and diagnosis code lists can be found in the online supplemental Table 1.
In addition to the primary analysis evaluating repair of all retinal breaks in aggregate, secondary analyses were conducted examining the incidence of procedures for retinal tears and detachments separately during each of the observation periods, as well as an additional analysis focusing on a “high-risk” age cohort consisting only of those 50-70 years old. The high-risk age cohort corresponds to the average age for a posterior vitreous detachment (PVD) to occur,19,20 which would be a common precursor lesion for retinal breaks and, therefore, most retinal breaks would expect to be found in this age group in a large cohort. Patients with codes for a reparative procedure and/or for diagnoses for both a retinal tear and detachment had the earliest date taken as the censoring date and were considered to only have a retinal detachment in tabulation of totals and for all secondary analyses. Because the THIN database is coded by general practitioners and not ophthalmologists, a sensitivity analysis was performed on those RBs with an associated diagnostic (retinal tear or detachment) medcode 30 days before or after the procedure code, with the assumption that any patient with both a procedure code and a known corresponding diagnosis is more likely to truly have had the procedure performed. Possible covariates of interest that were included in the study were age, gender, diabetes, and calendar year of index date.
Statistical Analysis
Baseline and demographic characteristics were summarized using descriptive statistics (e.g. means and ranges for continuous variables such as age; percentages for categorical variables). Cox proportional hazard models were used to analyze the time to undergo a procedure to treat a RB in association with oral fluoroquinolone use from the prescription index date. The censoring date of eligible patients was defined as the earliest date among the following: occurrence of the event of interest, a code for intraocular surgery (other than for a RB), a prescription for the alternative class of oral antibiotic written after the index date, patient transferred out of the general practice (i.e., no longer followed in THIN), 365 days of follow-up was reached, the latest date THIN collected data from the practice or death of the patient. If a patient had a corresponding diagnosis code (retinal tear or detachment) within 30 days prior to the procedure, the date of the diagnosis code was used as the censor date instead of the procedure date. Hazard ratios were estimated for four observation periods: days 1-7, 1-30, 1-90 and 1-365 after the index date. Since the unit of observation was one prescription, patients who met entry criteria could be entered into the study more than once. To account for possible non-independence of multiple observations and also clustering of observations from one patient, robust variance estimates were used in all Cox Regression analyses.21 STATA® 12 (College Station, Texas) software was used for all statistical analysis. Results of the analyses were considered statistically significant for p<0.05 (two-tailed).
Results
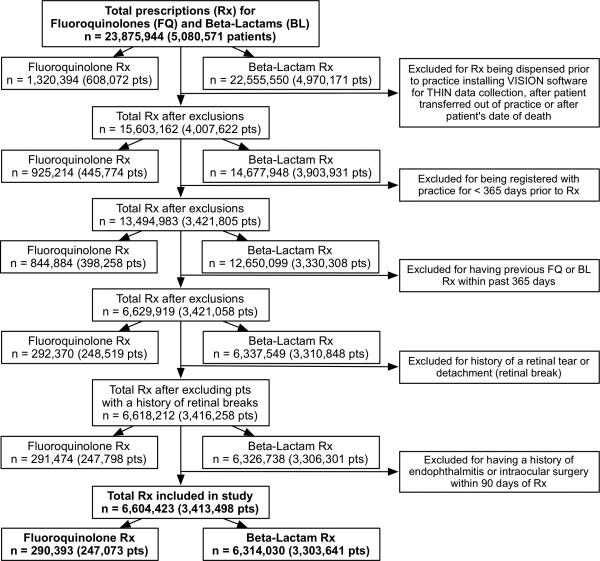
Included prescriptions were collected from June of 1994 though January of 2012. After exclusions, 6,604,423 prescriptions (290,393 FQ, 6,314,030 BL) from 3,413,498 patients (247,073 FQ, 3,303,641 BL) were eligible for analysis (Figure 1). Over 88% of all fluoroquinolone prescriptions studied were for ciprofloxacin (Table 2). The 290,393 fluoroquinolone prescriptions represent 3,978 to 5,569 person-years of fluoroquinolone use (depending on whether a 5- or 7-day prescription duration is assumed). The fluoroquinolone group consisted of fewer females than the β-lactam group (54.0% FQ vs. 55.8% BL, p<0.0001), and the fluoroquinolone cohort was statistically significantly older than the β-lactam cohort (55.1 years FQ vs 40.0 years BL, p<0.0001). There were 2,685 (661 retinal tears/ 2,024 retinal detachments) retinal breaks between both cohorts that occurred after an eligible prescription (Table 3). Of these, zero occurred within 7 days of a fluoroquinolone prescription and seven occurred within 7 days of a β-lactam prescription. After 30 days, the fluoroquinolone cohort had one RB and the β-lactam cohort had 28 RB. At 90 days after index date, the fluoroquinolone cohort had five RB and the β-lactam cohort had 87 RB. At 365 days from the index date, the fluoroquinolone cohort had 23 RB and the -lactam cohort had 373 RB (Table 4).
Figure 1.
Flow chart depicting numbers of prescriptions and patients after specific exclusion criteria and for final analysis.
Table 2.
Numbers of individual fluoroquinolone prescriptions
| Fluoroquinolone | Number of Prescriptions | Percent of Total |
|---|---|---|
| ciprofloxacin | 256,055 | 88.18 |
| ofloxacin | 13,488 | 4.64 |
| norfloxacin | 12,532 | 4.32 |
| levofloxacin | 5,812 | 2.00 |
| all others | 2506 | 0.86 |
| Totals | 290,393 | 100.00 |
Table 3.
Baseline characteristics of participants
| Characteristic | Fluoroquinolone Recipient | Beta-Lactam Recipient |
|---|---|---|
| Number of patients | 247,073 | 3,303,641 |
| Number of prescriptions (Rx) | 290,393 | 6,314,030 |
| Age, mean years (range) | 55.1 (1-109) | 40.0 (1-111)* |
| Female gender, percentage | 54.0% | 55.8%* |
| Diabetic (%patients/%Rx) | 10.2/10.2 | 6.0*/6.5* |
| Average year of cohort entry | 2005 | 2005 |
| Total eligible retinal breaks (RT/RD**) | 183 (49/134) | 2502 (612/1890) |
p<0.001
RT = retinal tear, RD = retinal detachment
Table 4.
Retinal Break (RB) Procedures by Antibiotic Prescription Class (RX)
| Fluoroquinolone Recipient | Beta-Lactam Recipient | |
|---|---|---|
| Total person years studied (after Rx) | 266,360 | 5,845,607 |
| RB incidence rate at 365 days+ | 8.63 | 6.4 |
| Number of RB Procedures | ||
| Within 7 days of Rx (RT/RD*) | 0 | 7 (3 RT/4 RD) |
| Incidence rate ratio (FQ/Beta) | 0 (95% CI: 0, 15.2) | |
| Within 30 days of Rx | 1 (0 RT/1 RD) | 28 (4 RT/24 RD) |
| Incidence rate ratio | 0.78 (95% CI: 0.02, 4.74) | |
| Within 90 days of Rx | 5 (2 RT/3 RD) | 87 (19 RT/68 RD) |
| Incidence rate ratio | 1.26 (95% CI: 0.40, 3.06) | |
| Within 365 days of Rx | 23 (7 RT/16 RD) | 373 (85 RT/288 RD)** |
| Incidence rate ratio | 1.35 (95% CI: 0.85, 2.06) | |
Per 100,000 person years
RT = retinal tear, RD = retinal detachment
Those with both a retinal tear and a retinal detachment were only included in the retinal detachment group
Cox univariate analysis showed that gender was not significantly associated with retinal breaks during the 7-day (HR=0.32, p=0.17, 95% CI: 0.06, 1.63), 30-day (HR=0.85, p=0.66, 95% CI: 0 .41, 1.76) or 90-day (HR=0.76, p=0.19, 95% CI: 0 .50, 1.14) observation periods, but female gender was associated with a protective HR of 0.79 (p=0.02, 95%CI: 0.65, 0.97) at the 365-day period. Older age was not associated with a RB during the 7-day period (HR=1.01, p=0.71, 95% CI: 0.98, 1.03), but there was an increased hazard ratio of 1.03 (p<0.001, 95% CI: 1.02, 1.04), 1.03 (p<0.001, 95% CI: 1.03, 1.04) and 1.04 (p<0.001, 95% CI: 1.04, 1.05) for every 1 year increase in age within the 30-day, 90-day and 365-day observation periods, respectively. Univariate analysis of calendar year of index date showed no association with RBs at the 7- or 30-day periods (HR=1.13, p=0.30; 95% CI: 0.90,1.43; HR=1.10, p=0.06, 95%CI: 0.99, 1.22, respectively), but more recent index year was associated with an 8% (HR=1.08, p<0.01, 95%CI: 1.02, 1.15) and a 10% (HR=1.10, p<0.01, 95%CI: 1.07, 1.13) increased hazard for RB in the 90 and 365-day observation windows, respectively. Having a diagnosis of diabetes significantly increased the univariate hazard ratio for a retinal break at each time period (7-day HR=11.3, p<0.01, 95% CI: 2.53, 50.53; 30-day HR=5.77, p<0.001, 95% CI:2.56, 13.02; or 90-day HR=6.68, p<0.001, 95% CI: 4.28, 10.41; 365-day HR=6.36, p<0.001, 95%CI: 5.12, 7.91). A hazard ratio (and subsequent p-value or confidence intervals) was unable to be calculated for the univariate analysis of the antibiotic cohorts at the 7-day observation period due to zero events occurring during that time in the fluoroquinolone cohort. Fluoroquinolones did not have a significant association with a RB in the 30-, 90- or 365-day observation periods (30-day HR=0.78, p=0.80, 95% CI: 0 .11, 5.71; 90-day HR=1.25, p=0.63, 95% CI: 0.51, 3.08; 365-day HR= 1.35, p=0.16, 95% CI: 0.89 2.06).
Due to the low number of events within the first seven days after antibiotic prescription, only age was included in the final reported multiple regression analyses. There was no effect modification or confounding observed on the HR between antibiotics and RB for any observation period for diabetes, calendar year of index or by either age or gender with inclusion of both variables (data not shown). An interaction term between age and antibiotics also was explored in the multivariable model but did not show relevant association or influence; hence it was removed from the final models (data not shown). The 7-day period in the multivariable analysis had zero events in the fluoroquinolone cohort, and therefore a hazard ratio was unable to be calculated. In the 30-, 90- and 365-day analysis, fluoroquinolone prescriptions were not associated with increased hazard of RB repair (HR's of 0.56 (p=0.57, 95% CI: 0.08, 4.14), 0.86 (p=0.75, 95% CI: 0.35, 2.12) and 0.89 (p=0.60, 95% CI: 0.58, 1.36), respectively; see Table 5). Increasing age was associated with a significant increase in RB—HR's of 1.03 (p<0.001; 95% CI: 1.02, 1.04), 1.03 (p<0.001, 95% CI: 1.03, 1.04) and 1.04 (p<0.001; 95% CI: 1.04, 1.05) per year—in the analyses through 30, 90 and 365 days, respectively. However, age was not significantly associated with RB during the 7-day period following antibiotic prescription (HR=1.01, p=0.65, 95%CI: 0 .98, 1.03).
Table 5.
Results of Cox proportional hazard analysis of fluoroquinolone versus β-Lactam antibiotic prescription*+
| Adjusted Hazard ratio | p-value | 95% CI | ||
|---|---|---|---|---|
| Lower | Upper | |||
| 7 Days after prescription | ** | ** | ** | ** |
| 30 Days after prescription | 0.56 | 0.57 | 0.08 | 4.14 |
| 90 Days after prescription | 0.87 | 0.75 | 0.35 | 2.12 |
| 365 Days after prescription | 0.89 | 0.60 | 0.58 | 1.36 |
Controlled for age
Other known associated systemic diseases, Marfan's and Stickler's Syndrome, were assessed, but found to occur in such small numbers as to be inconsequential to the results of the study and were not included in the final analysis
Not able to calculate due to 0 events in fluoroquinolone group
We performed a subset analysis on those aged 50-70 years to assess whether an association with fluoroquinolone therapy would be observed in a “high-risk” age cohort similar to that studied by Etminan and colleagues.2 This subset included 1,510,257 total prescriptions (790,452 FQ, 1,412,977 BL) from 831,978 patients (82,666 FQ, 97,280 BL). In this subset, through the 7-, 30-, 90- and 365-day observation periods, 3 (0 FQ, 3 BL), 19 (1 FQ, 18 BL), 48 (1 FQ, 47 BL) and 204 (9 FQ, 195 BL) retinal break events were observed, respectively. Again, none of the analyses suggested a higher risk in the fluoroquinolone group (unable to calculate HR for 7-day; HRs of 0.80 (p= 0.83, 95% CI: 0.11, 5.99), 0.30 (p=0.23, 95% CI: 0.04, 2.18) and 0.65 (p=0.20, 95%CI: 0.33, 1.27) through 30, 90 and 365 days follow-up respectively). Another secondary analysis performed within the full cohort for associations between fluoroquinolones and retinal tears or detachments individually were not significant in all four observation periods (HRs: 0.65-1.21, p>0.37 for all analyses).
A sensitivity analysis examining only the retinal break repairs with an associated diagnosis code within 30 days of the procedure code had no events for either cohort in the first 7 days, 3 RB (0 FQ, 3 BL) within 30 and 90 days and 54 RB (3 FQ, 51 BL) within 365 days. Once again due to no events occurring during the observation period HRs were unable to be calculated for the 7-, 30- and 90-day periods. The 365-day period had a HR of 0.88 (p=0.83), agreeing with the main analysis in finding no increased hazard of retinal break events following exposure to fluoroquinolones.
Discussion
In 2002, fluoroquinolones became the most commonly prescribed antibiotic in the United States,1 which has been attributed to their ability to treat community-acquired pneumonia and resistant infections. In our cohort study of patients from a United Kingdom database using β -lactams as a comparison group, we did not find an increased hazard of having a procedure to treat a retinal tear or detachment at any time point studied after patients were prescribed an oral fluoroquinolone.
The root “rhegma” is Greek and means “rent or fissure.”22 By definition then, a rhegmatogenous retinal detachment occurs after a break in the retina. Based on this definition and because previous reports suggested that oral fluoroquinolones may increase the risk of retinal detachments through their effect on collagen turnover,2,3 we included retinal tears in our study as part of the continuum of retinal detachments. Of the treatments that occurred for retinal breaks in our study, zero occurred within 7 days of the 290,393 index prescriptions for an oral fluoroquinolone, representing 5569 person years of fluoroquinolone use. Although direct comparison is difficult due to differences in study design, if the increase in incidence of 1 additional retinal detachment per 2500 person-years of use is taken as a benchmark, then there is only a 13% likelihood that our 0/5569 person-years estimate occurred by random chance..2
Confounding and the steps taken for its removal are of extreme importance for any observational study. One of the main differences between our study and previous published reports is our inclusion of all forms of intraocular surgery as a possible confounder in addition to cataract surgery. In addition, other studies did not account for the immediacy of the risk of retinal detachment after surgery which is typically highest in the first 90 days.2,3 We performed an additional analysis to determine the effect of removing our controls for intraocular surgery, and although our results did not reach significance, the point estimates all moved towards finding an association (univariate estimates of 90- and 365-day without IO HR= 1.45 for both vs. previous 90- and 365-day univariate estimates of 1.25 and 1.35 respectively; multivariate 90- and 365-day without IO HR=0.99 and 0.96 vs. previous 90-and 365-day with IO included HR of 0.87 and 0.89, respectively).
Additionally, a possible issue exists with the model used to create the propensity scores described by Kuo.3 One of the components used to create this score was “underlying ophthalmic conditions” thought to be associated with retinal detachments. Included under this heading were retinal vein occlusions, proliferative diabetic retinopathy and vitreous hemorrhages, which are not commonly associated with retinal detachments. Typically propensity scores even out the variables used to create the score. However, their definition of “underlying ophthalmic conditions” was treated as a binary variable and was not separated by individual ophthalmic conditions. Therefore there is a possibility for imbalance between conditions that are not known to be associated with retinal detachment and the established risk factors for RD.
Pasternak and colleagues4 recently reported a study where they found no association similar to our study. Despite the comparable findings, our study also included retinal tears . Given the mechanism, if there was an association between detachments and fluoroquinolones, the association should be seen in retinal tears as well. We wanted to be certain we were only examining procedures to repair RB thought to happen by the proposed mechanism of action of fluoroquinolones. Therefore, we were stricter in defining what constituted a rhegmatogeno et al. us retinal detachment when compared to Pasternak who included exudative and tractional detachments, which arise from mechanisms other than vitreous dissolution and a break in the retina.4
As is typical for analyses relying on an existing database, there are several limitations of this study. First, prescriptions and the indication for which they were written are not linked within the THIN database, meaning we are unable to identify the specific diagnosis for which each antibiotic prescription was written. We attempted to control for this by comparing the risk for retinal breaks between antibiotic classes with similar indications for use. While we cannot refute with certainty the possibility that the diseases treated by the antibiotic prescription conferred different degrees of risk for retinal breaks, thus obscuring an association with fluoroquinolones, it is unlikely differences of this nature existed. Second, the THIN database does not capture inpatient antibiotic use or hospitalizations, which therefore cannot be studied. Third, THIN relies on the GP to report 100% of the codes and does not occur directly from the specialist, nor is it required for payment. Either of these issues may have resulted in underreporting or erroneous recording of codes, but would be unlikely to be differential between groups. While non-differential misclassification tends to blunt associations, large negative effects still likely would have been identified; there was no suggestion of any tendency toward higher risk in the fluoroquinolone group in this analysis. Despite the decrease in “verified” procedures seen in the sensitivity analysis, the 365-day observation period HR was nearly identical for both the full cohort and the “verified” cohort with both a procedure and diagnosis code, suggesting that the GP's diligence in coding was not related to whether a patient received an antibiotic prescription for one of the two classes of interest. Also, we are not able to state with certainty that RBs do not occur more often in patients who take oral fluoroquinolones since our unit of observation was the RB repair, not the diagnosis. However it is unlikely that many clinically significant RBs would go untreated given the standard of care is to repair these lesions. Lastly, we cannot rule out the possibility of unmeasured confounding affecting our results because lattice degeneration and myopia—the two main ocular conditions associated with RB—are typically poorly coded for in administrative databases like THIN, but it's unlikely that systemic antibiotic prescription practices would be altered by these non-infectious ocular factors.
In summary, we did not find a higher risk of undergoing a procedure to treat a retinal tear or detachment in association with oral fluoroquinolone therapy in a large population-based database. If fluoroquinolones in fact increase the risk of retinal tears or detachments, it would be unlikely that our results would have been observed, raising doubts as to whether such an association exists. Thus, our findings fail to replicate the positive associated observations, reducing the level of confidence that oral fluoroquinolone use is associated with a higher risk of retinal detachment.
Acknowledgments
Financial Support: National Institutes of Health K12 Award (Dr. Brian VanderBeek), K12-EY015398, The project described was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1TR000003. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Additional funding was provided by Research to Prevent Blindness and the Paul and Evanina Mackall Foundation.
Footnotes
Conflicts of Interest: No conflicting relationship exists for any author
Portions of this data has been previously presented at the International Conference on Pharmacoepidemiology and Therapeutic Risk Management, August 2013 and the American Academy of Ophthalmology Annual Meeting, November 2013, New Orleans, LA
References
- 1.Linder JA, Huang ES, Steinman MA, Gonzales R, Stafford RS. Fluoroquinolone prescribing in the United States: 1995 to 2002. Am J Med. 2005;118:259–68. doi: 10.1016/j.amjmed.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 2.Etminan M, Forooghian F, Brophy JM, Bird ST, Maberley D. Oral fluoroquinolones and the risk of retinal detachment. JAMA. 2012;307(13):1414–19. doi: 10.1001/jama.2012.383. [DOI] [PubMed] [Google Scholar]
- 3.Kuo S, Chen Y, Lee Y. Association between recent use of fluoroquinolones and rhegmatogenous retinal detachment: a population-based cohort study. Clin Infect Dis. 2013 doi: 10.1093/cid/cit708. ePub ahead of print. [DOI] [PubMed] [Google Scholar]
- 4.Pasternak B, Svanström H, Melbye M, Hviid A. Association between fluoroquinolone use and retinal detachment. JAMA. 2013;310(20):2184–2190. doi: 10.1001/jama.2013.280500. [DOI] [PubMed] [Google Scholar]
- 5.Nowroozzadeh MH. Retinal detachment and fluoroquinolones [letter]. JAMA. 2012;308(3):233. doi: 10.1001/jama.2012.6630. [DOI] [PubMed] [Google Scholar]
- 6.Rao RC, Dlouhy BJ. Retinal detachment and fluoroquinolones [letter]. JAMA. 2012;308(3):233–4. doi: 10.1001/jama.2012.6628. [DOI] [PubMed] [Google Scholar]
- 7.Aristodemou P, Stylianides AC. Retinal detachment and fluoroquinolones [letter]. JAMA. 2012;308(3):234. doi: 10.1001/jama.2012.6618. [DOI] [PubMed] [Google Scholar]
- 8.Molloy AC, Mitry D. Retinal detachment and fluoroquinolones [letter]. JAMA. 2012;308(3):234–5. doi: 10.1001/jama.2012.6620. [DOI] [PubMed] [Google Scholar]
- 9.Etminan M, Brophy JM, Maberley D. Retinal detachment and fluoroquinolones [letter]. JAMA. 2012;308(3):235. doi: 10.1001/jama.2012.383. [DOI] [PubMed] [Google Scholar]
- 10.Albini TA, Karakousis PC, Abbey AM, et al. Association between oral fluoroquinolones and retinal detachment [editorial]. Am J Ophthalmol. 2012;154(6):919–21. doi: 10.1016/j.ajo.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 11.Han DP, Szabo A. Flashes, floaters, and oral fluoroquinolones: is retinal detachment a worry? JAMA Ophthalmol. 2013;131(1):91–3. doi: 10.1001/jamaophthalmol.2013.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwartz SG, Flynn HW, Jr, Mieler WF. Update on retinal detachment surgery. Curr Opin Ophthalmol. 2013;24:255–61. doi: 10.1097/ICU.0b013e32835f8e6b. [DOI] [PubMed] [Google Scholar]
- 13.Brett A. Oral Fluoroquinolone Use and Retinal Detachment Reconciling Conflicting Findings in Observational Research. JAMA. 2013;310(20):2151–2. doi: 10.1001/jama.2013.280501. [DOI] [PubMed] [Google Scholar]
- 14.Chang DF, Braga-Mele R, Mamalis N, et al. Prophylaxis of postoperative endophthalmitis after cataract surgery: results of the 2007 ASCRS member survey. J Cataract Refract Surg. 2007;33(10):1801–5. doi: 10.1016/j.jcrs.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 15.Al-Amri AM. Corneal perforation associated with topically applied gatifloxacin. Cornea. 2008;27(3):370–1. doi: 10.1097/ICO.0b013e31815dcfc4. [DOI] [PubMed] [Google Scholar]
- 16.Samarakoon N, Harrisberg B, Ell J. Ciprofloxacin-induced toxic optic neuropathy. Clin Experiment Ophthalmol. 2007;35(1):102–4. doi: 10.1111/j.1442-9071.2007.01427.x. [DOI] [PubMed] [Google Scholar]
- 17.Rampal S, Kaur R, Sethi R, et al. Ofloxacin-associated retinopathy in rabbits: role of oxidative stress. Hum Exp Toxicol. 2008;27(5):409–15. doi: 10.1177/0960327108092295. [DOI] [PubMed] [Google Scholar]
- 18.Blak BT, Thompson M, Dattani H, et al. Generalisability of The Health Improvement Network (THIN) database: demographics, chronic disease prevalence and mortality rates. Inform Prim Care. 2011;19(4):251–5. doi: 10.14236/jhi.v19i4.820. [DOI] [PubMed] [Google Scholar]
- 19.Yonemoto J, Ideta H, Sasaki K, et al. The age of onset of posterior vitreous detachment. Graefes Arch Clin Exp Ophthalmol. 1994;232:67–70. doi: 10.1007/BF00171665. [DOI] [PubMed] [Google Scholar]
- 20.Johnson MW. Posterior vitreous detachment: evolution and complications of its early stages. Am J Ophthalmol. 2010;149:371–82. doi: 10.1016/j.ajo.2009.11.022. [DOI] [PubMed] [Google Scholar]
- 21.Lin DY, Wei LJ. The robust inference for the Cox proportional hazards model. J Amer Statist Assoc. 1989;84(408):1074–8. [Google Scholar]
- 22. http://dictionary.reference.com/browse/rhegma accessed July 2013.