Abstract
Background
Somatically acquired genomic alterations with MYCN amplification (MNA) are key features of neuroblastoma (NB), the most common extra-cranial malignant tumour of childhood. Little is known about the frequency, clinical characteristics and outcome of NBs harbouring genomic amplification(s) distinct from MYCN.
Methods
Genomic profiles of 1100 NBs from French centres studied by array-CGH were re-examined specifically to identify regional amplifications. Patients were included if amplifications distinct from the MYCN locus were seen. A subset of NBs treated at Institut Curie and harbouring MNA as determined by array-CGH without other amplification was also studied. Clinical and histology data were retrospectively collected.
Results
In total, 56 patients were included and categorised into 3 groups. Group 1 (n = 8) presented regional amplification(s) without MNA. Locus 12q13-14 was a recurrent amplified region (4/8 cases). This group was heterogeneous in terms of INSS stages, primary localisations and histology, with atypical clinical features. Group 2 (n = 26) had MNA as well as other regional amplifications. These patients shared clinical features of those of a group of NBs MYCN amplified (Group 3, n = 22). Overall survival for group 1 was better than that of groups 2 and 3 (5 year OS: 87.5%±11% vs 34.9%±7%, log-rank p<0.05).
Conclusion
NBs harbouring regional amplification(s) without MNA are rare and seem to show atypical features in clinical presentation and genomic profile. Further high resolution genetic explorations are justified in this heterogeneous group, especially when considering these alterations as predictive markers for targeted therapy.
Introduction
Neuroblastoma (NB) is the most common extra-cranial malignant tumour of childhood, [1] and is characterised by its wide heterogeneity in clinical presentation and evolution [1]–[3]. Recent advances in genetic analysis of this heterogeneous tumour, using a wide panel of techniques including array Comparative Genomic Hybridization (aCGH), have revealed different recurrent genomic aberrations, most of which consist of copy number alterations. Indeed, it is now well established that the overall genomic pattern is an important prognostic marker which might be taken into account for treatment stratification [4]–[13]. Numerical chromosome alterations (whole chromosome gains or losses) are observed in NBs with good prognosis when exclusive. Typical segmental copy number alterations (deletions of chromosome arms 1p, 3p, 4p, 11q and gains of chromosome arms 1q, 2p, 17q) are associated with poor outcome [7].
Amplification of the proto-oncogene MYCN (MNA), found in 25 to 30% of NBs, is the most important genomic feature, in terms of prognosis and impact on treatment decisions [2], [3]. Other genomic aberrations defined by regional amplifications targeting various sites, non syntenic with the MYCN locus, have been previously described [5], [6], [14]–[19]. These amplicons seem to have a low recurrence and most often occur concomitantly with MNA [16]. In a previous study, the precise genetic mapping of such amplicons has been described, and a poor survival for patients with NBs harbouring loci co-amplified or not with MYCN has been suggested [16].
Nevertheless, to date, clinical features of NB harbouring amplicons different from MYCN, and particularly without concurrent MNA, have not yet been reported in detail. The role of these amplicons and their possible contribution to the oncogenic process are unclear and there is a need to better characterise clinically these tumours. The aim of this study is to describe occurrence, detailed clinical characteristics, histology and outcome of NBs harbouring amplicons at loci distinct from MYCN, without and with MNA.
Patients and Methods
Ethics statement
This study was authorized and approved by the ethics committee “Comité de Protection des Personnes Sud-Est IV”, reference L07-95 and L12–171 and the ethical committee Ile de France, reference 0811728. Written informed consent was obtained from parents according to national law and the ethics committees listed above approved this consent procedure.
Patients and samples
Between 1996 and 2011, tumour samples from a total of 1100 patients were sent to the laboratory from French centres for genetic analysis and were studied by aCGH.
The 1100 aCGH profiles were re-examined specifically for high level amplification, regardless of their overall genomic pattern, using the VAMP graphical interface and visual inspection [20]. aCGH profiles were taken into account if tumour cell content was known to be >50%, or in the absence of known tumour cell content, if the copy number profile showed a clear dynamic profile. All patients for whom amplifications distinct from the MYCN locus were observed were then selected. As a control group, patients treated at Institut Curie from 1999 to 2011, for whom aCGH was performed on the tumour and revealed a MNA without any other amplification were also studied. The aCGH platform and analysis steps were identical for all patients.
A total of 56 patients were included in this study. For all cases MYCN status was confirmed by Fluorescent in situ hybridization (FISH) [21] and no discordance between aCGH and FISH has been observed. Clinical data (sex, date of birth, date at diagnosis, INSS tumour stage, localisation, MIBG uptake, sequence of treatment, relapse or progression, date and status of last follow up), biological data (urinary catecholamine at diagnosis) and histology (tumours were classified according to INPC, with focus on the differentiation of the tumour cells) were retrospectively collected. Patients were treated in French centres from the Société Française des Cancers de l'Enfant (SFCE) according to national or international treatment protocols.
Comparative Genomic Hybridization and definition of genomic amplification
Tumour samples sent to the laboratory for somatic pangenomic analysis were studied by aCGH as previously described [16]. The resolution was determined by the genomic spacing of the array elements. Two types of arrays have been used: until 2009 an in-house designed array containing between 2855 and 3799 BAC-PAC clones covering the whole genome with a median probe spacing of 1 Mb [16], then a commercial array (NimbleGen) was used with an average resolution of 40 kb (72 000 probes).
Amplification was defined by at least two BAC clones (for the in-house array) or at least 3 adjacent oligonucleotide probes (for the NimbleGen array taking into account its higher resolution) with a fluorescent tumour/normal ratio ≥3 corresponding to a log2 ratio ≥1, 5 [16]. Boundaries of an amplicon were described according to the genomic position of the markers located outside the amplified region (coordinates of the non amplified markers closest to the observed amplicon, according to UCSC genome draft, hg19 (http://genome.ucsc.edu/)). On chromosome band 2p24, amplicons harbouring MYCN with or without directly adjacent co-amplified genes were considered as MNA. In case of amplifications of loci distant from MYCN but still within the cytogenetic 2p24 band, we defined arbitrarily an amplicon distinct from MYCN, when the amplicon was separated from MYCN locus by at least five BAC/PAC clones with a normal fluorescence tumour/normal ratio on the in-house array, or the corresponding number of probes on the NimbleGen array.
Analysis of somatic genetic alterations with definition of losses, gains and high level amplifications was performed as previously described [16]. Precise genetic analysis of 31 of the NBs in this study has been reported previously [16] but the precise clinical data had not been analysed for these patients.
Statistical analysis
Contingency tables were analysed by the Fisher exact test. Mean values were compared by the non parametric Kruskal Wallis Test. Median follow up was calculated according to the inversed Kaplan-Meier method. Progression free survival (PFS) was defined as the time between diagnosis and the first event: relapse, progression, and death from any cause or last follow-up. Overall survival (OS) was defined as the time between diagnosis and death of any cause or last follow-up. Survival curves were analyzed according to the Kaplan-Meier method and compared using the log-rank test with a P-value of less than 0.05 considered to be significant.
Results
Genomic amplifications
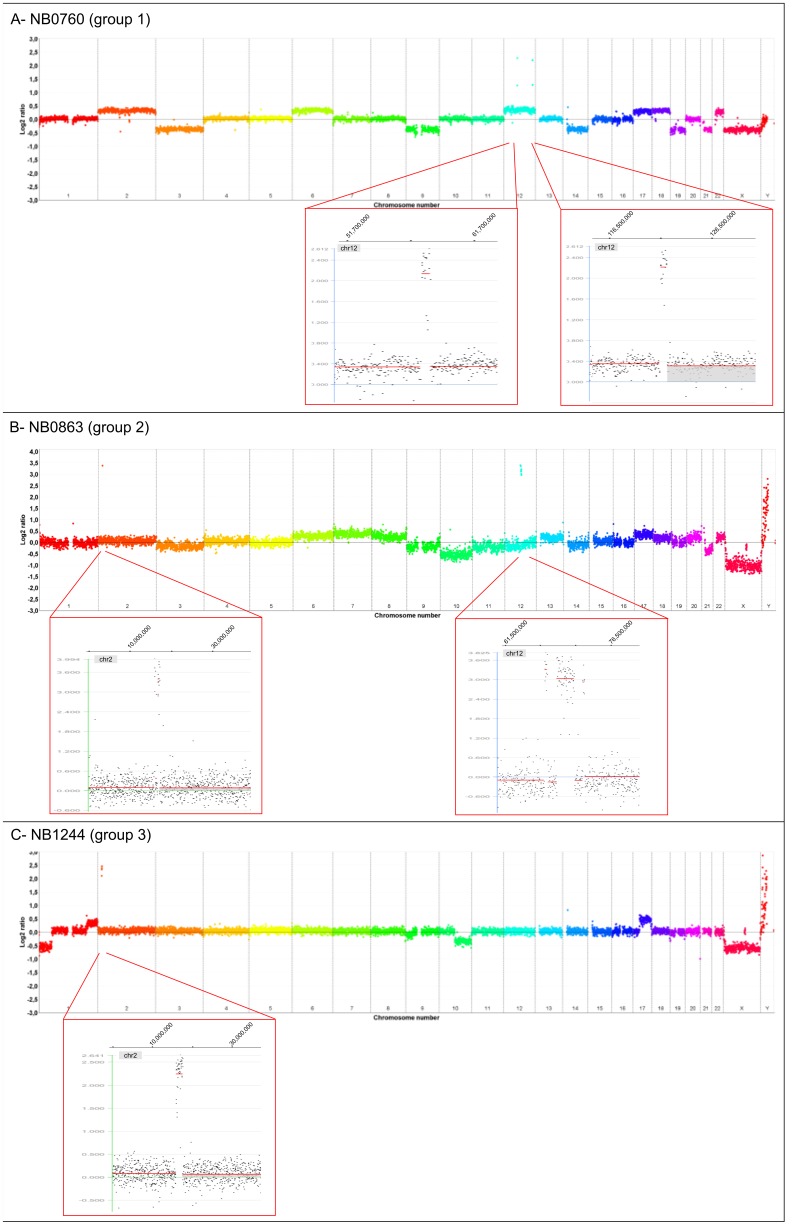
Among 1100 aCGH profiles, we found a total of 12 tumours showing amplification of one or several loci distinct from MYCN without any evidence of MNA (1%). We did not get access to clinical information for two of them. For another two, the histological report was non conclusive and a definitive diagnosis of NB could not be retained. Indeed, diagnosis of malignant pheochromocytoma was suggested. These four patients were not included. Therefore eight confirmed NBs presenting regional amplification(s), without MNA, were included as group 1 (n = 8). A further 26 patients were found with NB exhibiting MNA associated with one or several amplification(s) at other loci (group 2, n = 26). Finally, 22 patients treated for NB in our institution between 1999 and 2011, for whom aCGH have been performed on tumour, were identified with amplification only located at the MYCN locus and were considered as a control group (group 3, n = 22). Examples of genomic profile for each of the 3 groups are shown in Figure 1 with zoom on the amplified regions. Altogether, the most frequent amplified regions distinct from MNA were located at chromosome band 19p12, 2p25, 2p23, 21q21, 22q11 and 12q13–14, with amplification in other chromosome regions being much rarer. Genomic findings for groups 1 and 2 cases are summarised in Table 1 and Table 2 respectively. Precise amplification boundaries are available in Table S1 and in a.BED file (File S1) enabling to export all genes possibly included in the amplicons, according to UCSC genome draft, hg19 (http://genome.ucsc.edu/).
Figure 1. Examples of different genomic profiles with genomic amplifications obtained in neuroblastoma by array comparative genomic hybridization for each group at diagnosis.
For each panel, the genome wide aCGH profile is shown with zoom on the amplified regions. Genomic profiles were obtained using the NimbleGen R platform, and images were generated using the SignalMap R software. Log2 ratio = 0 corresponds to a balanced tumour/normal DNA ratio. Amplification is indicated by plots with a log2 ratio ≥1, 5 (corresponding to a tumour/normal DNA ratio ≥3). (A) Example of group 1 profile (NB0760): NB without MYCN amplification but harbouring amplifications at loci 12q13-14 and 12q24. (B) Example of group 2 profile (NB0863): NB with MYCN amplification (2p24) and harbouring amplification at locus 12q14. (C) Example of group 3 profile (NB1244): NB with MYCN amplification and no other amplicon.
Table 1. Clinical characteristics, genomic findings and histology data for group 1.
| Patient | Clinical characteristics | Genomic findings | Histology | ||||||||||
| Sex | Age at diagnosis (months) | INSS stage | Localisation | Metastasis at diagnosis | MIBG uptake | Urinary catechol | Initial treatment | Relapse (months) | Outcome (FU months) | Amplicons (cytogenetic band) | Segmental alterations | Grade of differentiation | |
| NB0384 | M | 23 | 4 | Abd | B, M | Y | H | IM | No | CR(121) | 11q13 | −1p, −3p, −11q, +17q | P. diff NB |
| NB0040 | M | 54 | 4 | Adr | B, M, DLN | Y | H | IM | Ms(25) | DOD(75,5) | 11q13, 17q25 | −11q, −16p, −16q, +17q | P. diff NB |
| NB0791 | M | 18 | 3 | Cervical | LLN | No | Nl | CT-S | No | CR(44) | 16q22 | numerical | Undiff NB |
| NB0760 | F | 17 | 4 | Abd | DLN | Y | H | IM | No | CR(44) | 12q13_14, 12q24 | numerical | P. diff NB |
| NB0830 | F | 22 | 2b | Abd median | none | No | Nl | S | No | CR(27) | 12q13_14 | −22q | Diff NB |
| NB0037 | M | 55 | 3 | Abd lumbar | LLN | Y | H | S-CT | L(7) | CR(129) | 12q13_15, 21q22 | +1p, +13q, +17q | P. diff NB |
| NB0072 | F | 51 | 4 | Adr | B, M, DLN | Y | na | CT-S | No | Al(31) | 7q21 | −3p, +18 pq | Undiff NB |
| NB0039 | M | 67 | 4 | Adr | Lung | No | Nl | IM | Ms+L(14,5) | DOD(19) | 12q12, 12q13_15 | +1p, +4q | P.diff NB |
M, male; F, female; Adr, adrenal; Abd, abdominal; B, bone; M: bone marrow; DLN: distant lymph nodes; LLN: local lymph nodes; Ms, Metastatic relapse; L, Local relapse; MIBG, metaiodobenzylguanidine uptake at primary tumour site; Y, yes; H, high secretion of urinary catecholamines; Nl, normal secretion of urinary catecholamines; IM, intensive multimodality; S: surgery; CT, chemotherapy; DOD, dead of disease; Al, alive status unknown; CR, complete remission; NB, neuroblastoma; Undiff., undifferentiated; P.diff., poorly differentiated; Diff, differentiating; na, not available.
Table 2. Clinical characteristics, genomic findings and histology data for group 2.
| Patient | Clinical characteristics | Genomic findings | Histology | ||||||||
| Sex | Age at dg (months) | INSS stage | Location | MIBG uptake | Urinary catechol | Relapse (months) | Outcome (FU months) | Amplicons (cytogenetic band) | Segmental alterations | ||
| NB0187 | M | 25 | 3 | Adr | Y | na | No | CR (107) | 19p12, 21q21 | −1p, −15q, +17q | NB NOS |
| NB1085 | M | 27 | 4 | Adr | Y | H | No | CR (18) | 1p31, 2p23 (ALK), 4q13 | −1p, +17q | Undiff NB |
| NB0240 | F | 26 | 1 | Adr | Y | H | L(23) | DOD (25) | 1p36.3 | −1p, +2p, +17q | P. diff NB |
| NB0038 | F | 25 | 4 | Pelvic | Y | H | L(12) | DOD (15) | 2p23 (ALK), 8q12, 17q23, 19p12, 21q21, 21q22, 22q11 | −1p | Undiff NB |
| NB0284 | M | 43 | 3 | Adr | Y | H | L(5,5) | DOD (6) | 1p34.2, 1q32 | +2p, −5q | NB NOS |
| NB0194 | F | 39 | 4 | Abd +mediastinum | Y | H | Ms+L(7,5) | DOD (10) | 2q35, 6p21 | −1p, +12q, −10p, +17q | NB NOS |
| NB0186 | M | 9 | 4 | Adr | Y | H | No | D tox (6) | 22q11 | −1p, +1q, −2p, +17q | P. diff NB |
| NB0196 | M | 24 | 4 | Adr | Y | H | Ms+L(3,5) | DOD (4) | 17q22, 17q25 | +11q13 int, −17p, +17q | GGNB |
| NB0234 | F | 9 | 2b | Adr | Y | H | No | RC (156) | 16q22_23 | none | NB NOS |
| NB0185 | F | 15 | 3 | Adr | Y | H | L(15,5) | DOD (19) | 21q21, 22q11 | −1p, +1q, +4q, −5q, −10p, −10q, +12q, +15q, +17q, +18q, −19q | Undiff NB |
| NB0232 | M | 17 | 4 | Adr | Y | H | No | CR (103) | 7q22,7q33_34, 7q36 | −1p, +2q, −10q, +17q | P. diff NB |
| NB0260 | M | 19 | 4 | Adr | Y | H | Ms+L(23) | DOD (25) | 19p12 | −1p, +3p, −5q, +7q, −16q, −17p, +17q, −19q | NB NOS |
| NB0236 | M | 21 | 4 | Thoraco-abd-pelvic | Y | H | Ms(7) | DOD (9) | 1p13, 6p23–24, 19p12, 21q21, 22q11 | −1p, +17q | Undiff NB |
| NB0015 | M | 25 | 4 | Adr | Y | H | No | CR (104) | 19p12 | −1p, +7pq, +17q | P. diff NB |
| NB0862 | F | 51 | 3 | Adr | Y | H | No | CR (43) | 5p15, 5q11 | +17q | P. diff NB |
| NB1015 | M | 29 | 4 | Adr | Y | na | Ms(8,5) | DOD (12) | 2p25 (ODC1) | none | P. diff NB |
| NB0863 | M | 19 | 4 | Abd | Y | H | Ms+L(14) | DOD (15) | 12q14 | numerical | P. diff NB |
| NB0230 | M | 44 | 4 | Adr | Y | H | Ms(14) | DOD (19,5) | 1p13, 2p23 (ALK), 2p25,19p12 | −1p, +6p, −6q, +11q, +17q | P. diff NB |
| NB0256 | M | 16 | 4 | Adr | Y | na | Ms(58) | DOD (65,4) | 19p12, 21q21 | −1p, +9q, −17p, +17q | P. diff NB |
| NB0173 | M | 6 | 4S | Adr | na | na | Ms+L(42) | DOD (49) | 19q13.4 | −1p, +17q | P. diff NB |
| NB0248 | F | 14 | 3 | Adr | Y | Nl | No | CR (96) | 17q23, 19p12 | −1p, −7q, −21q, +17q | P. diff NB |
| NB1173 | M | 27 | 4 | Adr | Y | na | Ms+L(11) | DOD (13) | 12q13–14, 12q14_15 | −1p, −12q, +17q | NB NOS |
| NB0013 | F | 13 | 4 | Adr | Y | na | Ms(10) | DOD (10) | 2p24_25 (ODC1) | −1p, −6q,+2p, +3q, +4q, +13q, +17q | NB NOS |
| NB1250 | F | 56 | 4 | Adr | Y | H | Ms(6) | DOD(10) | 2p25.2 | −1p, −6q,+11q, +17q | P. diff NB |
| NB1257 | F | 149 | 4 | Adr | Y | H | Ms+L(6,5) | DOD (17) | 2p23 (ALK), 2q22 | −1p, −5q, +6p, +7p, +7q, −10q, −12p, −14q, −15p, +17q, −18q | P. diff NB |
| NB0838 | M | 8 | 4 | Adr | Y | H | Ms(4) | DOD (5,5) | 2p25.1 (ODC1), 2p23 (ALK) | −1p | P. diff NB |
M, male; F, female; dg, diagnosis; Adr, adrenal; Abd, abdominal;; MIBG, metaiodobenzylguanidine uptake at primary tumour site; Y, yes; H, high secretion of urinary catecholamines; Nl, normal secretion of urinary catecholamines; Ms, Metastatic relapse; L, Local relapse; DOD, dead of disease; D tox, dead of toxicity; CR, complete remission; NB, neuroblastoma; GGNB, ganglioneuroblastoma; Undiff., undifferentiated; P.diff., poorly differentiated; Diff, differentiating; NOS, not otherwise specified.
In group 1, the amplified region 12q13–14 was recurrent, observed in 4/8 cases (NB0760, NB0830, NB0037, NB0039). For two of them, the amplification was larger and comprises chromosome bands 12q13 to 12q15. Amplification at 11q13 was observed in two cases (NB0384, NB0040). Four NBs had a single amplification and the other four (NB0037, NB0039, NB0040, NB0760) had two distinct amplicons. These amplifications arise in an overall genomic pattern of segmental aberrations ( Table 1 ). However for 4/8 cases, aCGH showed overall atypical genomic profiles for a NB, and for two others the genomic profile was numerical.
In group 2, more than 50% of cases had at least two regions co-amplified with MNA. Among these, amplification at chromosome band 19p12 was found in 8/26 cases, amplification of ALK at band 2p23 in 5/26 cases, and ODC1 at band 2p25 in 3/26 cases ( Table 2 and Table S1). The majority of tumours in group 2 had a genomic profile typical of NB, with segmental chromosome alterations including losses of 1p, 11q and gain of 17q. One had only numerical chromosome alterations and two other cases neither numerical nor segmental chromosome alterations. In this group, aCGH profiles globally showed a higher number of copy number alterations ( Table 2 ).
In group 3, aCGH profiles showed a single amplification at the MYCN locus associated with segmental chromosomal alterations typical of NB in most cases.
Clinical characteristics
All patients from the 3 groups presented non familial and non syndromic NB. Detailed clinical characteristics and histology data for patients of groups 1 and 2 are summarised in Tables 1 and 2 respectively.
For group 1, patients were of all INSS stages, the primary site occurred in different localisations, clinical features and histology were heterogeneous ( Table 1 ). Interestingly, three patients (NB0791, NB0830, NB0039) in this group had normal urinary catecholamines and no uptake of MIBG at scintigraphy at diagnosis. For NB0039, lung metastasis was observed at diagnosis. Of note, NB0037 had an atypical presentation with a lumbar primary site with metastatic relapse located at the spermatic cord.
Patients in groups 2 ( Table 2 ) and 3 (data not shown) shared clinical features with NB of advanced stage. All patients in group 2, except one (data not available), had positive MIBG uptake in their primary tumour. All except one (and data were not available for six patients) presented with high level urinary catecholamines. The primary tumour was localised mostly at the adrenal gland and histology was in general poorly differentiated or undifferentiated.
Concerning the general distribution of clinical parameters for the three groups ( Table 3 ), no statistically significant difference of median age at diagnosis was found between the three groups, with an overall median age of 25 months. No difference was found between the three groups concerning distribution of INSS stage at diagnosis, with a high percentage of advanced stages observed in all three groups (Fisher exact test, P = 0.35). Interestingly, distribution of primary tumour localisation was different between group 1 and the two other groups (Fisher exact test, P<0.001). Indeed, localisation was mainly abdominal for the three groups, but an adrenal site was found for 37.5% of primary tumours in group 1 versus 85% in group 2 and 100% in group 3 ( Table 3 ).
Table 3. Distribution of clinical parameters for the three groups.
| Parameters | Group 1 | Group 2 | Group 3 | ||||||
| n = 8 | % | n = 26 | % | n = 22 | % | Total | P | ||
| Tumour INSS Stage | 4 | 5 | 62,5 | 18 | 69 | 19 | 86 | 42 | NS |
| 3 | 2 | 25 | 5 | 19 | 3 | 14 | 10 | ||
| 1, 2, 4S | 1 | 12,5 | 3 | 12 | 0 | 0 | 4 | ||
| Median age at dg (months)[range] | 37 [17–67] | 24,5 [6–149] | 29 [8–73] | NS | |||||
| Age at dg | ≤18 months | 2 | 25 | 9 | 35 | 9 | 41 | 20 | NS |
| >18 months | 6 | 75 | 17 | 65 | 13 | 59 | 36 | ||
| Tumour localisation | Adrenal | 3 | 37,5 | 22 | 85 | 22 | 100 | 47 | <0.001 |
| Other abdominal | 4 | 50 | 3 | 11 | 0 | 0 | 7 | ||
| Non abdominal | 1 | 12,5 | 1 | 4 | 0 | 0 | 2 | ||
| Relapse | 3 | 37,5 | 18 | 69 | 9 | 41 | 30 | NS | |
| Metastatic +local | 1 | 7 | 6 | 14 | |||||
| Metastatic only | 1 | 7 | 3 | 11 | |||||
| Local only | 1 | 4 | 0 | 5 | |||||
INSS, international neuroblastoma staging system; dg, diagnosis; P, Fisher's exact test p-value; NS, not significant.
Survival analysis
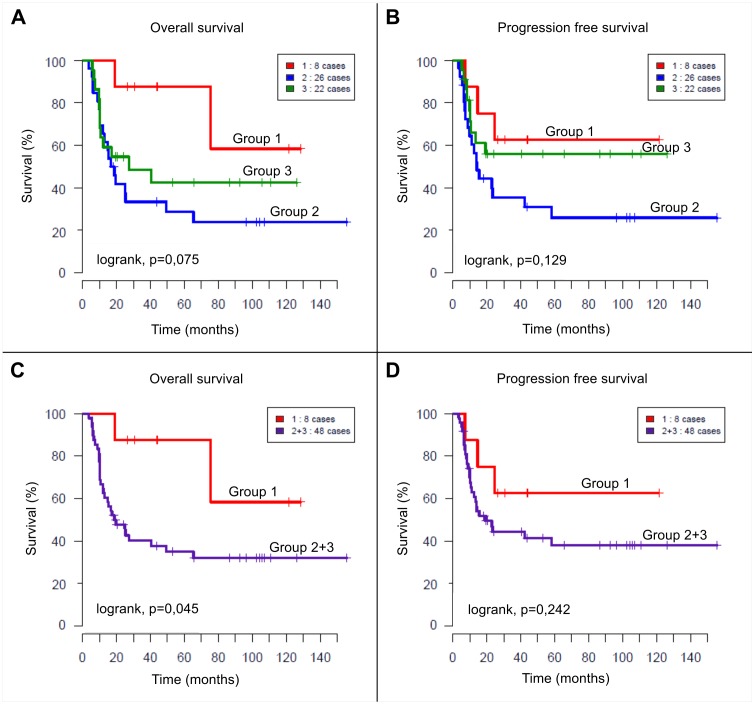
Overall median follow up was 88 months (range from 3.7 to 155 months). No significant difference in outcome was found between the three groups ( Figure 2A and 2B ).
Figure 2. Kaplan Meier survival curves.
(A, B) Overall survival and progression free survival curves of patients according to the 3 groups: group 1 (amplicon other than MYCN, not MYCN amplified, n = 8), group 2 (MYCN and other amplicons, n = 26), group 3 (only MYCN amplification, n = 22). Five-year OS rate was 87.5%±11.7%, 28.6%±9.2% and 42.4%±11.2% for groups 1, 2 and 3, respectively (P = 0.075). Five-year PFS rate was 62.5%±17%, 25.8%±9.2%, 55.9%±11% for groups 1, 2 and 3 respectively (P = 0.129). (C, D) Overall survival and progression free survival curves respectively for patients presenting NBs with amplification other than MYCN, without MYCN (group 1, n = 8) and patients with at least amplification of MYCN (group 2 and 3 pooled together, n = 48). Five-year OS rate was 87.5%±11.7% for group 1 and 34.9%±7% for group 2+3 (P = 0.045). Five-year PFS rate was 62.5%±17% for group 1 and 37.9%±7.7% for group 2+3 (P = 0.242).
However when comparing patients of group 1 to all patients with NB harbouring MYCN amplification, i.e. groups 2 and 3 pooled together, we found a significantly better OS for group 1 ( Figure 2C, P = 0, 045). There was no difference in PFS ( Figure 2D ).
Concerning groups 2 and 3, no statistically significant difference in outcome was found between patients with exclusively MYCN amplified NB and patients with MNA associated with other amplicons. Nevertheless a trend towards a poorer outcome in OS and particularly in PFS was observed for group 2 compared to group 3.
Discussion
Somatic DNA amplification plays an important role in the development of many solid tumours possibly by providing a means of overexpression of oncogenes [22], [23]. Identification of high level amplifications has clinical impact due to the role of such genetic alterations as both prognostic and predictive molecular markers. MYCN, first identified in NB, was the first amplified proto-oncogene with significant clinical relevance, and its status is routinely used to stratify treatment [2], [3], [24], [25]. In other cancer types, such as medulloblastoma, amplification of MYC family genes is associated with clinical high risk disease and predicts an extremely poor prognosis [26]. Other specific gene amplifications, for instance in breast cancer such as ERBB2 or MDM2 are associated with high grade cancer and have strong prognostic significance [23], [27].
In NB, in previous studies, regional amplifications other than MYCN have been occasionally described with low recurrence and most often concomitantly with MNA [5], [6], [14], [17]–[19]. The objective of this study was now to report in detail the clinical features of patients with NB harbouring amplification(s) other than MYCN.
In this more extensive series, we confirm the rarity of regional amplifications occurring either without MNA or together with MNA (1% and 3% of all cases, respectively) as detected by aCGH. Given the resolution of the arrays used in this study, it cannot be excluded that amplified regions smaller than the interval between the probes of the arrays might have gone undetected by our techniques. However only few amplified regions distinct from MYCN have been observed in recent high resolution sequencing studies based on whole exome/genome sequencing [28]–[30], confirming that this is a rare phenomenon. Thus our lower resolution approaches give a good overview of the majority of amplicons in the genome. In a next step, it will be interesting to determine with accuracy genes implicated in the amplicons using next generation sequencing.
Interestingly, patients with NBs harbouring amplifications other than MYCN, without concomitant MNA, constitute a heterogeneous group of patients with NBs arising from non adrenal sites observed more frequently, as well as occurrence of atypical metastatic sites (lung, spermatic cord). Furthermore an increased frequency of absence of MIBG avidity and absence of urinary catecholamine secretion was noted, when normally positive in 90–95% of NB cases [1]. In addition to atypical clinical features, the overall genomic pattern of these NBs revealed atypical segmental patterns. Although histological analysis confirmed the diagnosis of NB, novel histology characterisation using PHOX2B immuno-staining might be useful in this context of atypical NB to help in the diagnosis of undifferentiated types [31]. Indeed PHOX2B immunolabelling has been shown to improve the diagnosis of undifferentiated NB among childhood small round blue-cell tumours with high specificity and sensitivity. Considering recent publication, it would be also interesting for this atypical group of NB without MNA to further study expression of MYC protein in the tumour as it has been suggested that MYC protein expression could be a new prognostic factor indicating more aggressive clinical behaviour than MNA [32].
On the other hand, clinical features of patients whose tumours harbour regional amplifications other than MYCN together with MNA are comparable to those with MNA only.
Although limited by the small number of patients, analysis suggests that OS of patients with amplification(s) other than MYCN without MNA might be better than that of patients with MNA, whereas those harbouring both MYCN and other amplifications might have an even worse prognosis. Indeed tumours harbouring regional amplicons in addition to MNA showed a higher genomic instability as documented by the observation of more segmental chromosomal alterations with a tendency towards a poorer outcome, as suggested previously [16]. Furthermore when comparing OS to a group of 170 NBs with segmental chromosomal alterations but without MYCN or other amplification (corresponding to genomic type B and D from a previous study [7]), the OS for group 1 was comparable to these NBs (type B and D) with 5 year OS of 87, 5%±11, 7 SE for group 1 vs 73%±3,9 SE and this result was significantly better than OS for patients in groups 2 and 3.
The genes targeted by regional amplifications in NB have been analysed in detail in previous study [5], [6], [9], [14], [16]–[19]. The most frequent amplifications concern ALK amplification at band 2p23, frequently co-amplified with MYCN, accounting for 4% of NBs studied in a meta-analysis [33]–[35], found in five cases in our study (group 2) and ODC1 amplification at band 2p25 always found co-amplified with MYCN (20% of cases analysed in 2 studies) [9], [30], found in three cases in our study (group 2). Somatic amplification at 12q13–15 locus has also been described [6], [9], [12], [14]–[16], [19], [36]. This amplified region contains two potential target genes: CDK4 (12q13_14) involved in cell cycle progression and MDM2 (12q15), a target gene of the transcription factor tumour protein p53 and the encoded protein can target p53 for proteasomal degradation. In our study the amplicons at 12q13–14 and 12q13–15 were the most commonly amplified region in the absence of MNA with the CDK4 gene amplified constantly but MDM2 found amplified only in half of the cases. Amplifications at 12q13–14 and 12q13–15 have been reported in many other solid tumours such as malignant glioma, bladder cancer and sarcomas most often resulting in overexpression of genes in this region, with the implication of a worse prognosis in amplified cases [37]–[41]. CDK6 gene at 7q21 was also amplified in the absence of MNA in one case (NB0072) and CCND1 gene at 11q13 in two cases (NB0040 and NB0384). These observations are noteworthy considering that CCND1, CDK4 and CDK6 are G1 phase-regulating genes, part of the Cyclin D/CDK4/CDK6/RB pathway found hyperactive in NB, and considering the efficacy of new small molecule inhibitor targeting CDK4/CDK6 leading to G1 arrest and cellular senescence [42]. In group 1, without MNA, seven cases among eight presented amplification containing one of these genes.
Characterisation of amplicons using aCGH data combined with gene expression profiling analysis has shown that up to 25% of the genes targeted by genomic amplification are overexpressed in tumour cells, with a potential oncogenetic role, an observation of clinical importance when considering targeted therapies [16], [42].
Taken together, NB harbouring distinct amplification other than MYCN might have atypical clinical and genetic features and will warrant further studies including high resolution genomic analysis and expression data to more precisely characterise their genetic features and impact in oncogenic process. As more targeted therapies become available, such as molecules inhibiting specifically CDK4-CDK6 [42] or ALK for instance, it will be crucial to obtain precise information about genomic amplification status at diagnosis. As higher resolution genomic profiles are obtained, smaller genomically amplified regions might be detected more frequently. The prognostic impact of the amplified regions will have to be studied prospectively and their use as predictive markers for targeted therapy will be of importance.
Supporting Information
Boundaries for amplifications found in group 1 and in group 2. Boundaries of one amplified region are given according to the genomic position of the markers (BAC or oligonucleotide probe) located outside the amplified region (coordinates of the non amplified markers closest to the observed amplicon) and according to UCSC genome draft, hg19 (http://genome.ucsc.edu/).
(XLS)
A.BED file corresponding to the genomic positions of the markers enables to export all genes possibly included in the amplified regions, according to UCSC genome draft, hg19 ( http://genome.ucsc.edu/ ).
(BED)
Acknowledgments
The authors wish to thank the following associations: APAESIC (Association des Parents et des Amis des Enfants Soignés à l'Institut Curie), Association Hubert Gouin, “Les Bagouz à Manon” and “Enfants et Santé”, and “Les amis de Claire”. The authors thank Virginie Bernard for her help in the creation of a.BED file.
Funding Statement
This study was partly supported by the Annenberg foundation. This work was also supported by grants from the Institut National de la Santé et de la Recherche Médicale, the Ligue Nationale contre le Cancer (Equipe labellisée) and the PHRC AOM 02014 and PHRC IC2007-09. The construction of the BAC/PAC array was supported by grants from the Carte d'Identité des Tumeurs program of the Ligue Nationale Contre le Cancer. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Maris JM, Hogarty MD, Bagatell R, Cohn SL (2007) Neuroblastoma. Lancet 369: 2106–2120. [DOI] [PubMed] [Google Scholar]
- 2. Brodeur GM (2003) Neuroblastoma: biological insights into a clinical enigma. Nat Rev Cancer 3: 203–216. [DOI] [PubMed] [Google Scholar]
- 3. Maris JM (2010) Recent advances in neuroblastoma. N Engl J Med 362: 2202–2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Janoueix-Lerosey I, Schleiermacher G, Michels E, Mosseri V, Ribeiro A, et al. (2009) Overall genomic pattern is a predictor of outcome in neuroblastoma. J Clin Oncol 27: 1026–1033. [DOI] [PubMed] [Google Scholar]
- 5. Mosse YP, Diskin SJ, Wasserman N, Rinaldi K, Attiyeh EF, et al. (2007) Neuroblastomas have distinct genomic DNA profiles that predict clinical phenotype and regional gene expression. Genes Chromosomes Cancer 46: 936–949. [DOI] [PubMed] [Google Scholar]
- 6. Mosse YP, Greshock J, Margolin A, Naylor T, Cole K, et al. (2005) High-resolution detection and mapping of genomic DNA alterations in neuroblastoma. Genes Chromosomes Cancer 43: 390–403. [DOI] [PubMed] [Google Scholar]
- 7. Schleiermacher G, Janoueix-Lerosey I, Ribeiro A, Klijanienko J, Couturier J, et al. (2010) Accumulation of segmental alterations determines progression in neuroblastoma. J Clin Oncol 28: 3122–3130. [DOI] [PubMed] [Google Scholar]
- 8. Schleiermacher G, Mosseri V, London WB, Maris JM, Brodeur GM, et al. (2012) Segmental chromosomal alterations have prognostic impact in neuroblastoma: a report from the INRG project. Br J Cancer 107: 1418–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Spitz R, Oberthuer A, Zapatka M, Brors B, Hero B, et al. (2006) Oligonucleotide array-based comparative genomic hybridization (aCGH) of 90 neuroblastomas reveals aberration patterns closely associated with relapse pattern and outcome. Genes Chromosomes Cancer 45: 1130–1142. [DOI] [PubMed] [Google Scholar]
- 10. Vandesompele J, Baudis M, De Preter K, Van Roy N, Ambros P, et al. (2005) Unequivocal delineation of clinicogenetic subgroups and development of a new model for improved outcome prediction in neuroblastoma. J Clin Oncol 23: 2280–2299. [DOI] [PubMed] [Google Scholar]
- 11. Wang Q, Diskin S, Rappaport E, Attiyeh E, Mosse Y, et al. (2006) Integrative genomics identifies distinct molecular classes of neuroblastoma and shows that multiple genes are targeted by regional alterations in DNA copy number. Cancer Res 66: 6050–6062. [DOI] [PubMed] [Google Scholar]
- 12. Chen QR, Bilke S, Wei JS, Whiteford CC, Cenacchi N, et al. (2004) cDNA array-CGH profiling identifies genomic alterations specific to stage and MYCN-amplification in neuroblastoma. BMC Genomics 5: 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tomioka N, Oba S, Ohira M, Misra A, Fridlyand J, et al. (2008) Novel risk stratification of patients with neuroblastoma by genomic signature, which is independent of molecular signature. Oncogene 27: 441–449. [DOI] [PubMed] [Google Scholar]
- 14. Carr J, Bown NP, Case MC, Hall AG, Lunec J, et al. (2007) High-resolution analysis of allelic imbalance in neuroblastoma cell lines by single nucleotide polymorphism arrays. Cancer Genet Cytogenet 172: 127–138. [DOI] [PubMed] [Google Scholar]
- 15. Corvi R, Savelyeva L, Breit S, Wenzel A, Handgretinger R, et al. (1995) Non-syntenic amplification of MDM2 and MYCN in human neuroblastoma. Oncogene 10: 1081–1086. [PubMed] [Google Scholar]
- 16. Fix A, Lucchesi C, Ribeiro A, Lequin D, Pierron G, et al. (2008) Characterization of amplicons in neuroblastoma: high-resolution mapping using DNA microarrays, relationship with outcome, and identification of overexpressed genes. Genes Chromosomes Cancer 47: 819–834. [DOI] [PubMed] [Google Scholar]
- 17. Fix A, Peter M, Pierron G, Aurias A, Delattre O, et al. (2004) High-resolution mapping of amplicons of the short arm of chromosome 1 in two neuroblastoma tumors by microarray-based comparative genomic hybridization. Genes Chromosomes Cancer 40: 266–270. [DOI] [PubMed] [Google Scholar]
- 18. Molenaar JJ, van Sluis P, Boon K, Versteeg R, Caron HN (2003) Rearrangements and increased expression of cyclin D1 (CCND1) in neuroblastoma. Genes Chromosomes Cancer 36: 242–249. [DOI] [PubMed] [Google Scholar]
- 19. Su WT, Alaminos M, Mora J, Cheung NK, La Quaglia MP, et al. (2004) Positional gene expression analysis identifies 12q overexpression and amplification in a subset of neuroblastomas. Cancer Genet Cytogenet 154: 131–137. [DOI] [PubMed] [Google Scholar]
- 20. La Rosa P, Viara E, Hupe P, Pierron G, Liva S, et al. (2006) VAMP: visualization and analysis of array-CGH, transcriptome and other molecular profiles. Bioinformatics 22: 2066–2073. [DOI] [PubMed] [Google Scholar]
- 21. Ambros PF, Ambros IM, Brodeur GM, Haber M, Khan J, et al. (2009) International consensus for neuroblastoma molecular diagnostics: report from the International Neuroblastoma Risk Group (INRG) Biology Committee. Br J Cancer 100: 1471–1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Albertson DG (2006) Gene amplification in cancer. Trends Genet 22: 447–455. [DOI] [PubMed] [Google Scholar]
- 23. Albertson DG, Collins C, McCormick F, Gray JW (2003) Chromosome aberrations in solid tumors. Nat Genet 34: 369–376. [DOI] [PubMed] [Google Scholar]
- 24. Schwab M (1999) Oncogene amplification in solid tumors. Semin Cancer Biol 9: 319–325. [DOI] [PubMed] [Google Scholar]
- 25. Rubie H, Hartmann O, Michon J, Frappaz D, Coze C, et al. (1997) N-Myc gene amplification is a major prognostic factor in localized neuroblastoma: results of the French NBL 90 study. Neuroblastoma Study Group of the Societe Francaise d'Oncologie Pediatrique. J Clin Oncol 15: 1171–1182. [DOI] [PubMed] [Google Scholar]
- 26. Ryan SL, Schwalbe EC, Cole M, Lu Y, Lusher ME, et al. (2012) MYC family amplification and clinical risk-factors interact to predict an extremely poor prognosis in childhood medulloblastoma. Acta Neuropathol 123: 501–513. [DOI] [PubMed] [Google Scholar]
- 27. Al-Kuraya K, Schraml P, Torhorst J, Tapia C, Zaharieva B, et al. (2004) Prognostic relevance of gene amplifications and coamplifications in breast cancer. Cancer Res 64: 8534–8540. [DOI] [PubMed] [Google Scholar]
- 28. Molenaar JJ, Koster J, Zwijnenburg DA, van Sluis P, Valentijn LJ, et al. (2012) Sequencing of neuroblastoma identifies chromothripsis and defects in neuritogenesis genes. Nature 483: 589–593. [DOI] [PubMed] [Google Scholar]
- 29. Pugh TJ, Morozova O, Attiyeh EF, Asgharzadeh S, Wei JS, et al. (2013) The genetic landscape of high-risk neuroblastoma. Nat Genet 45: 279–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sausen M, Leary RJ, Jones S, Wu J, Reynolds CP, et al. (2013) Integrated genomic analyses identify ARID1A and ARID1B alterations in the childhood cancer neuroblastoma. Nat Genet 45: 12–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bielle F, Freneaux P, Jeanne-Pasquier C, Maran-Gonzalez A, Rousseau A, et al. (2012) PHOX2B immunolabeling: a novel tool for the diagnosis of undifferentiated neuroblastomas among childhood small round blue-cell tumors. Am J Surg Pathol 36: 1141–1149. [DOI] [PubMed] [Google Scholar]
- 32. Wang LL, Suganuma R, Ikegaki N, Tang X, Naranjo A, et al. (2013) Neuroblastoma of undifferentiated subtype, prognostic significance of prominent nucleolar formation, and MYC/MYCN protein expression: a report from the Children's Oncology Group. Cancer 119: 3718–3726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Chen Y, Takita J, Choi YL, Kato M, Ohira M, et al. (2008) Oncogenic mutations of ALK kinase in neuroblastoma. Nature 455: 971–974. [DOI] [PubMed] [Google Scholar]
- 34. George RE, Sanda T, Hanna M, Frohling S, Luther W 2nd, et al. (2008) Activating mutations in ALK provide a therapeutic target in neuroblastoma. Nature 455: 975–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Janoueix-Lerosey I, Lequin D, Brugieres L, Ribeiro A, de Pontual L, et al. (2008) Somatic and germline activating mutations of the ALK kinase receptor in neuroblastoma. Nature 455: 967–970. [DOI] [PubMed] [Google Scholar]
- 36. Slack A, Lozano G, Shohet JM (2005) MDM2 as MYCN transcriptional target: implications for neuroblastoma pathogenesis. Cancer Lett 228: 21–27. [DOI] [PubMed] [Google Scholar]
- 37. Reifenberger G, Ichimura K, Reifenberger J, Elkahloun AG, Meltzer PS, et al. (1996) Refined mapping of 12q13–q15 amplicons in human malignant gliomas suggests CDK4/SAS and MDM2 as independent amplification targets. Cancer Res 56: 5141–5145. [PubMed] [Google Scholar]
- 38. Simon R, Struckmann K, Schraml P, Wagner U, Forster T, et al. (2002) Amplification pattern of 12q13–q15 genes (MDM2, CDK4, GLI) in urinary bladder cancer. Oncogene 21: 2476–2483. [DOI] [PubMed] [Google Scholar]
- 39. Mejia-Guerrero S, Quejada M, Gokgoz N, Gill M, Parkes RK, et al. (2010) Characterization of the 12q15 MDM2 and 12q13–14 CDK4 amplicons and clinical correlations in osteosarcoma. Genes Chromosomes Cancer 49: 518–525. [DOI] [PubMed] [Google Scholar]
- 40. Xia SJ, Pressey JG, Barr FG (2002) Molecular pathogenesis of rhabdomyosarcoma. Cancer Biol Ther 1: 97–104. [DOI] [PubMed] [Google Scholar]
- 41. Berner JM, Forus A, Elkahloun A, Meltzer PS, Fodstad O, et al. (1996) Separate amplified regions encompassing CDK4 and MDM2 in human sarcomas. Genes Chromosomes Cancer 17: 254–259. [DOI] [PubMed] [Google Scholar]
- 42. Rader J, Russell MR, Hart LS, Nakazawa MS, Belcastro LT, et al. (2013) Dual CDK4/CDK6 inhibition induces cell-cycle arrest and senescence in neuroblastoma. Clin Cancer Res 19: 6173–6182. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Boundaries for amplifications found in group 1 and in group 2. Boundaries of one amplified region are given according to the genomic position of the markers (BAC or oligonucleotide probe) located outside the amplified region (coordinates of the non amplified markers closest to the observed amplicon) and according to UCSC genome draft, hg19 (http://genome.ucsc.edu/).
(XLS)
A.BED file corresponding to the genomic positions of the markers enables to export all genes possibly included in the amplified regions, according to UCSC genome draft, hg19 ( http://genome.ucsc.edu/ ).
(BED)