Abstract
Background
The economic burden of chronic noncancer pain (CNCP) remains insufficiently documented in primary care.
Purpose
To evaluate the annual direct health care costs and productivity costs associated with moderate to severe CNCP in primary care patients taking into account their pain disability.
Materials and methods
Patients reporting noncancer pain for at least 6 months, at a pain intensity of 4 or more on a 0 (no pain) to 10 (worst possible pain) intensity scale, and at a frequency of at least 2 days a week, were recruited from community pharmacies. Patients’ characteristics, health care utilization, and productivity losses (absenteeism and presenteeism) were documented using administrative databases, pharmacies’ renewal charts, telephone, and self-administered questionnaires. Patients were stratified by tertile of pain disability measured by the Brief Pain Inventory questionnaire.
Results
Patients (number =483) were, on average, 59 years old, mainly women (67.5%), and suffered from CNCP for a mean of 12 years at an average pain intensity of 6.5±1.9. The annual direct health care costs and productivity costs averaged CAD $9,565 (±$13,993) and CAD $7,072 (±$11,716), respectively. The use of complementary health care services accounted for almost 50% of the direct health care costs. The mean adjusted total direct health care costs (considering pain-related hospitalizations only) and productivity costs increased with more pain disability: low disability, CAD $12,118; moderate, CAD $18,278; and severe, CAD $19,216; P=0.001.
Conclusion
The economic burden of CNCP is substantial and increases with the level of pain disability, which suggests the need for and potential benefits of improving CNCP management through specific and adapted treatment plans targeting the impact of pain on daily functioning.
Keywords: noncancer chronic pain, primary care, cohort study, direct health care costs, productivity costs, Brief Pain Inventory
Introduction
Chronic noncancer pain (CNCP) is defined by the International Association for the Study of Pain as a pain persisting beyond the normal healing time for a specific illness or injury.1 It is estimated that more than 25% of the Canadian population is affected by CNCP,2,3 a prevalence that tends to increase in our aging society.4 Based on four European studies published between 1991 and 2002, Ospina and Harstall5 estimated the prevalence of chronic pain to be 35.5%. Affected individuals report lower quality of life,6 experience interferences in their daily activities4,7,8 and are at higher risk of suffering from depression and anxiety disorders,4,8 sleep problems,7 and additional comorbid conditions.9
CNCP is associated with substantial direct health care costs. In Quebec (Canada), the annual direct health care costs associated with rheumatoid arthritis, fibromyalgia, and painful neuropathic disorders are estimated to average CAD $10,287 (±$12,728 [2002 values]; $12,257 [2011 values]),10 CAD $4,065 (±$6,798 [2007 values]; $4,339 [2011 values]),11 and CAD $4,163 (±$7,536 [2002 values]; $4,960 [2011 values])12 per patient, respectively. Individuals with CNCP make more physician visits (mean of 12.9 visits per year versus 3.8 visits per year) and have longer hospital stays (mean of 3.9 days versus 0.7 days) than individuals without it.13
Chronic pain also causes substantial productivity losses arising from work absences (absenteeism) and reduced productivity at work (presenteeism).8 A Canadian survey revealed that individuals with CNCP missed an average of 9.3 (95% confidence interval [CI]: 4.7–13.7) workdays annually due to their pain, a number rising to 16.0 (95% CI: 5.1–26.9) among individuals with severe pain.2 In Australia, the productivity costs associated with CNCP are estimated to amount to AU $5.1 billion annually.14
Pain-related direct health care costs and productivity costs yield considerable global societal costs. Total CNCP expenditures represent more than 3% of Finland’s gross national product15 and US $2.1 million per employer annually (1998 values) in the United States.16 More severe pain disability seems to be associated with higher societal costs. Patients with arthritis and rheumatism reporting more disability incurred higher direct health care17,18 and productivity costs.19,20 In the United States, when these costs are considered, the total annual cost of pain was greater than the annual costs of treating heart disease, cancer, and diabetes respectively.21
Although the vast majority of CNCP patients are followed-up in primary care,8 most studies have evaluated the economic burden of CNCP in patients recruited in specialized clinics.18,22–24 The objective of this project was, therefore, to describe the direct health care and productivity costs associated with CNCP among primary care patients. Patients with various diagnoses were considered and the costs were described as a function of their pain disability.
Materials and methods
Study design
As part of the ACCORD Program (Application Concertée des COnnaissances et Ressources en Douleur), a knowledge translation research program in the field of CNCP, a cohort study was conducted (one submitted paper is accepted for publication).25,26 In this cohort study, individuals with CNCP having an active analgesic prescription from a primary care physician were recruited from May 2009–January 2010 in community pharmacies. Patients completed a structured telephone interview and a self-administered questionnaire. Governmental administrative databases, the Régie de l’assurance maladie du Québec (RAMQ; Quebec health insurance board; QC, Canada) and the Maintenance et exploitation des données pour l’étude de la clientèle hospitalière (MED-ÉCHO – a hospitalization database), as well as community pharmacies’ renewal charts were used to document health care use and costs in the year preceding the recruitment. Ethical approvals were obtained from the Comité scientifique et d’éthique de la recherche of the Centre de santé et de services sociaux de Laval (Laval, QC, Canada) and from the Commission d’accès à l’information (QC, Canada). Each patient signed an informed consent form and received a financial compensation of $25 for completing the questionnaires. Pharmacists received a financial compensation of $50 for every consenting patient.
Study population
The study was conducted in the Réseau universitaire intégré de santé de l’Université de Montréal (Montreal, QC, Canada), which encompasses six areas in the province of Quebec (Canada): Mauricie et Centre du Québec; Laval; Montréal; Laurentides; Lanaudière; and Montérégie, representing more than 40% of the population in this province. Based on the Quebec Health Ministry’s atlas, 513 community pharmacies were identified in this territory.27 Among those, a random sampling stratified by region and weighted by the number of pharmacies located within each region was done. To recruit 60 pharmacies, selected pharmacies were sequentially contacted until the target numbers of pharmacies were reached in each region. To recruit 600 patients, each pharmacy had to identify between 10 and 15 consecutive and potentially eligible patients. During the course of the study, additional pharmacies were invited to participate, so as to compensate for those that did not recruit the expected number of patients.
To be eligible, patients had to: 1) be ≥18 years of age; 2) report suffering from noncancer pain for at least 6 months and for a minimum of 2 days per week; 3) rate their average pain in the past 7 days as ≥4 on a 0–10 intensity scale (0= no pain; 10= worst possible pain);28 4) have an active analgesic prescription from a primary care physician; and 5) speak and read French or English. Patients reporting migraine as the only source of pain and those unable to provide informed consent were not eligible. The Canadian Pain Society and the World Health Organization define chronic pain as a pain lasting 6 months or more.29,30 This definition is currently used in research.31 In order to ensure that patients’ pain had some impact on various aspects of their daily functioning, only those who reported pain at least 2 days a week were selected.
Direct health care and productivity costs
Direct health care costs
Direct health care costs, expressed in Canadian dollars, were estimated for each participant based on the health care resources used in the year preceding the recruitment.
All outpatient physician visits, as well as tests and interventions (related and unrelated to CNCP), were documented from the RAMQ database. In this database, a service code is assigned to each of these components, along with the specialty of the professional consulted, the date, the site, and the amount reimbursed by the RAMQ, which was used to estimate the cost of the services. A pain specialist (DL) reviewed all tests and interventions provided to cohort patients in order to identify those related to CNCP.
All visits to emergency rooms (ER) were considered. Costs of these visits were documented from the RAMQ database and they included the costs of the visit, tests and interventions, and physician consultations. For each ER visit, a unitary cost of CAD $270.54 (2011 values) was considered. This cost corresponds to the average provincial cost per ER according the Quebec Health Ministry (Direction de l’allocation des ressources, unpublished data) and accounts for expenses incurred by the health care institution itself, including overheads and consumables. The costs of physician consultation(s), test(s), and intervention(s) provided during the ER stay were those paid by the RAMQ during the year preceding the recruitment (May 2008–January 2009).
All hospitalizations and those related, or possibly related, to CNCP were considered. Hospitalizations were documented from the MED-ÉCHO database, where information regarding the admission date, the primary and secondary diagnoses, the length of stay, and the site are recorded. The hospitalization costs included those of the hospital stay, physician visits, tests, and interventions. The cost of hospital stay represents a per diem cost of CAD $948.73 (2011 values) according the Quebec Health Ministry (Direction de l’allocation des ressources, unpublished data), including overheads and consumables. This cost is the mean provincial cost per day of hospitalization, and it accounts for expenses related to the costs of nursing care, laboratory tests, medications, laundry, food, administration, and maintenance. Physician visit and test/intervention costs provided during hospitalizations were documented from the RAMQ database and corresponded to those reimbursed by the RAMQ from 2008–2009. The primary and secondary diagnostic codes associated with the hospitalizations were reviewed by a pain specialist (DL) (see Table S1) to identify those related or possibly related to CNCP.
The use of nonpharmacological health care services was documented during the telephone interview by asking patients, “Now, I will read a list of different types of therapy that can be used to relieve pain. Please stop me each time I name a therapy you have used in the past.” Overall, 23 therapies were enumerated: relaxation/breathing techniques; meditation; hypnosis; visualization; individual distraction; individual psychotherapy; group psychotherapy; self-help support group; physiotherapy; occupational therapy; hydrotherapy/hot bath/aqua therapy; electrostimulation; intramuscular stimulation; ultrasounds; biofeedback; acupuncture; massotherapy; chiropractic; osteopathy; therapeutic touch; reflexology; Reiki; and magnet therapy. When patients identified a therapy that they had employed, the interviewer then asked them, “Have you used it in the past 6 months?” and if yes, “How frequently did you use it in the past 6 months? Every day, a few times every week, a few times every month, or a few times every year?” Those frequencies were translated into actual numbers of annual visits; every day =260 (annual number of weekdays); a few times every week =104; a few times every month =24; and a few times every year =2. The costs of each visit corresponded to the mean cost per visit in the Montreal area (QC, Canada) as a function of the type of professional consulted, and it varied between CAD $45 and CAD $90 (2007 values).32
Prescribed analgesics dispensed 1 year prior to the recruitment were documented from the RAMQ database or from pharmacies’ dispensing charts; the latter allowed for the documentation of pharmacologic treatments of individuals not insured by the RAMQ for their medications. For each analgesic prescription (new and renewals), the following information was recorded: date of dispensation; common drug denomination; form; dosage; and quantity. Analgesics included acetaminophen, nonsteroidal antiinflammatory drugs, antidepressants, anticonvulsants, muscle relaxants, opioids, antiretroviral therapy, disease-modifying antirheumatic drugs, and antirheumatic biologic agents. Only antidepressants and anticonvulsants recommended for pain treatment were taken into account (see Table S2),33,34 and they were documented for patients not reporting depression or epilepsy. Antiretrovirals were those recommended to treat zona-related pain35 (valacyclovir, famciclovir, acyclovir). Prescribed medications to prevent or control the gastrointestinal adverse effects that are frequently reported with analgesics were also documented (laxatives, antacids, gastroprotectants, and antiemetics). The costs of each medication corresponded to those reimbursed by the RAMQ (List of Medications 2011)36 based on the form and the dosage of each product. The pharmacist’s fee for each medication dispensed was also considered. For patients insured by the RAMQ, we used the actual dispensing fee paid by the RAMQ. For patients not insured by the RAMQ, a fee of CAD $7.87, which corresponds to the mean dispensing fee paid by the RAMQ in 2011, was assumed.
To document over-the-counter medications used to treat pain and adverse effects associated with analgesics, patients were asked during the telephone interview: “In the past 6 months, have you taken over-the-counter medications or natural products for pain and for drug-related side effects such as constipation, heartburn, and nausea or vomiting?” The frequency of use was described in terms of every day, a few times every week, a few times every month, and a few times every year, and was later translated into annual numbers of daily recommended doses: every day =365; a few times every week =104; a few times every month =24; and a few times every year =2. Unitary costs were estimated using the McKesson database37 (McKesson distributes medications to more than 6,000 community pharmacies in Canada). Daily dosages represented the minimum recommended daily doses of each specific product in the Vigilance Santé Program38 – a computerized program that is frequently used in community pharmacies.
Productivity costs
Productivity costs, described in terms of absenteeism and presenteeism, were solely considered for individuals who were currently employed at the time of the interview (full-or part-time job), and for those who were on temporary or permanent disability; they were not considered for unemployed individuals, nor for those who were retired. This information was assessed during the telephone interview, as participants had to choose one of the enumerated choices, which included full- and part-time work and permanent and temporary disabilities.
Absenteeism was documented during the telephone interview using the following question: “In the past 6 months, how many days of work did you miss because of your pain or medical appointment, or treatment for you pain?” To evaluate the annual costs of absenteeism, the reported number of days absent from work due to pain in the past 6 months was multiplied by 2. For individuals with a full- or part-time job, productivity costs were calculated by multiplying the annual number of workdays missed by the mean Canadian hourly wage (CAD $23.06 [2011 values])39 and the mean number of hours worked daily (7.24 hours).40 For individuals on temporary or permanent disability, productivity costs were calculated by multiplying the annual number of workdays missed by the minimum wage as estimated in 2011:41 CAD $9.65/hour; 8 hours/day. For individuals on temporary disability, the annual number of workdays missed represented the reported number of days absent from work due to pain in the past 6 months, multiplied by 2, and for individuals on permanent disability, it corresponded to 260 (annual number of weekdays absent).
As for absenteeism, presenteeism was only estimated for individuals with a full- or part-time job and for those on permanent or temporary disability. Based on the method described by Hu et al,42 presenteeism was evaluated during the telephone interview using the following question: “In the past 6 months, what percentage of your productivity at work did you lose, on average, because of your pain? Please answer using a scale from 0% to 100% where 0% means ‘no loss in productivity’ and 100% means the ‘loss of all productivity’.” Presenteeism was estimated by multiplying the time lost due to pain (the number of workdays with pain by the percent of productivity lost on those days), by the number of hours worked per day (7.24 hours)40 and by the hourly wage (CAD $23.06 [2011 values]).39
Pain disability
The impact of pain on daily functioning was assessed in the telephone interview using the interference items of the modified Brief Pain Inventory (BPI). The BPI is a widely used instrument in pain research and its psychometric qualities are well documented.43,44 It includes ten interference items. For each one, patients are asked to rate, on a 0–10 scale (0= does not interfere, 10= interferes completely), the extent to which pain interferes with various aspects of their daily living including general activity, walking ability, mood, normal work, relations with other people, sleep, enjoyment of life, self-care, recreational activities, and social activities. A global BPI score is derived by taking the average rating on the ten items.43
Patients’ characteristics
Sociodemographic and pain characteristics were documented with the self-administered questionnaire and telephone interview. The characteristics of pain included its duration (time since onset) and frequency in the past week. The circumstances surrounding the onset of the pain and its location(s) were also recorded. Pain diagnoses were based on patients’ self-reports using the following question during the telephone interview: “I will read a list of diagnoses that can be at the origin of your pain. Please stop me each time I read a diagnosis corresponding to your condition.” The list included ten diagnoses, and patients had the opportunity to report diagnoses not included in the list. Diagnoses were then grouped into eight main categories: 1) back pain; 2) neck pain; 3) fibromyalgia; 4) neuropathic pain; 5) visceral pain; 6) inflammatory arthritic pain (for example, rheumatoid arthritis); 7) degenerative arthritic pain (for example, osteoarthritis); and 8) tendinitis, bursitis, capsulitis, and epicondylitis. The impact of pain on sleep was investigated using the Chronic Pain Sleep Inventory,45 while depression and anxiety levels were measured using the Hospital Anxiety and Depression Scale.46 Depression and anxiety scores were rated as “absent” (scores ≤7), “uncertain” (scores between 8–10), or “probable” (scores ≥11). The presence of comorbid conditions was assessed through the Charlson Comorbidity Index, an instrument that takes into account the number and seriousness of comorbid diseases.47
Data analyses
Annual costs were described on the basis of a societal perspective, in terms of direct health care and productivity costs. They were adjusted to 2011 Canadian dollar values based on the consumer price index (Statistics Canada, Ottawa, ON, Canada).48 Taking into account the resources used in the year preceding the recruitment, the costs of hospitalizations, the ER visits, the outpatient physician, and other health care professional visits, pharmacotherapy (prescribed and over-the-counter medications that were used to treat pain and adverse effects associated with analgesic medications), as well as the costs associated with productivity loss due to absenteeism and presenteeism, were computed for each patient. Thereafter, the total direct health care costs and the costs associated with productivity loss were computed. The mean (± standard deviation) of these costs was computed for the entire cohort, as well as by three subcohorts defined by the tertile of the global BPI scores labeled as mild, moderate, and severe disability. The statistical significance of the between subcohort differences was estimated using a univariate linear regression model and chi-square statistics for continuous (for example, annual health care resource use and health care costs) and categorical variables, respectively.
Multivariate linear regression models were also developed to predict the costs as a function of the BPI tertile after adjusting for the following confounders: age;12,17 sex;12 duration of pain;17,49 and the Charlson comorbidity score.22,23,50,51 All variables associated with at least a 10% change in the cost estimate in the univariate analyses were included in the final multivariate model. Given the lack of precision in the identification of hospitalizations related to CNCP, all-cause hospitalizations were considered in this analysis. In a secondary analysis, only pain-related hospitalizations were reported. For each BPI tertile, the mean cost and its 95% CI were calculated. Gamma transformations of costs were employed in all cases.52 Statistical analyses were carried out using SPSS Statistics Base 19.0 for Windows® (IBM Corporation, Armonk, NY, USA) and SAS® Software (version 9.1; SAS Institute Inc., Cary, NC, USA).
Results
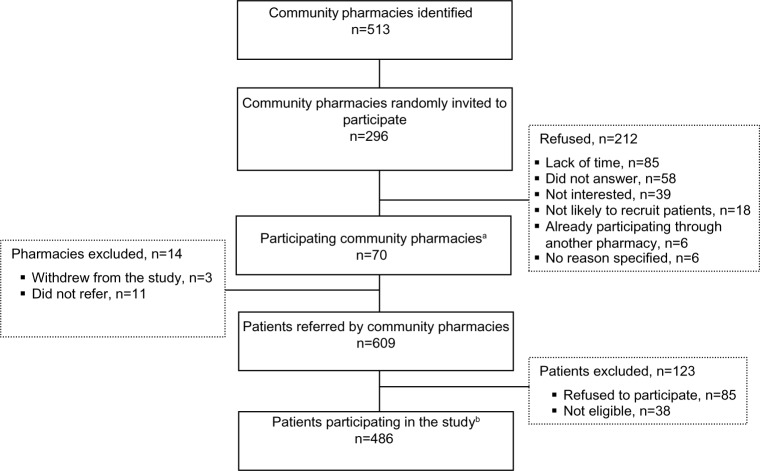
Between May and October 2009, a total of 296 community pharmacies were invited to participate; 84 pharmacies were recruited and 70 completed the study and recruited patients (Figure 1). Between May 2009 and January 2010, pharmacists referred 609 potentially eligible patients, of whom 38 were ineligible and 85 refused to participate. Data from the community pharmacies’ renewal charts and from the RAMQ and the MED-ÉCHO databases were available for all participants (number [n] =486). Telephone interviews and self-administered questionnaires were completed by 485 and 483 individuals, respectively. Based on the BPI tertile scores, three subcohorts were created and included 483 individuals: mild disability, BPI scores between 0.0–4.30 (n=165); moderate disability, scores between 4.31–6.40 (n=160); and severe disability, scores between 6.41–10.0 (n=158).
Figure 1.
Recruitment of pharmacies and patients.
Notes: aPharmacy distribution per region (n of recruited pharmacies/total n per region): Mauricie et Centre du Québec, 6/60 (10.0%); Montréal, 18/134 (13.4%); Laval, 13/70 (18.6%); Lanaudière, 8/77 (10.4%); Laurentides, 14/95 (14.7%); Montérégie, 11/77 (14.3%); bpatient distribution per region (n of recruited patients per region/total n of patients): Mauricie et Centre du Québec, 44/486 (9.1%); Montréal, 92/486 (18.9%); Laval, 67/486 (13.8%); Lanaudière, 91/486 (18.7%); Laurentides, 117/486 (24.1%); Montérégie, 75/186 (15.4%).
Abbreviation: n, number.
As reported in Table 1, participants were middle aged (mean age: 59±13 years), mainly women (67.5%), Caucasian (96.3%), and French-speaking (90.5%). The majority reported having an elementary school diploma or less (27.3%) or a high-school diploma (35.2%) as their highest level of education. Differences were observed between the subcohorts of patients defined by BPI tertile scores; those reporting more severe pain disability were younger, reported lower familial income, and were more likely to be on permanent or temporary disability.
Table 1.
Sociodemographic characteristics
| All patients (n=483) | Patients stratified by level of pain disability
|
P-values | |||
|---|---|---|---|---|---|
| Mild disabilitya (n=165) | Moderate disabilityb (n=160) | Severe disabilityc (n=158) | |||
| Age (years), mean (SD) | 59 (13) | 61 (13) | 58 (12) | 57 (11) | 0.002 |
| Women, n (%) | 326 (67.5) | 110 (66.7) | 106 (66.3) | 110 (69.6) | 0.783 |
| Type of insurances, n (%) | 0.321 | ||||
| Public (RAMQ) | 295 (61.1) | 96 (58.2) | 95 (59.4) | 104 (65.8) | |
| Private | 188 (38.9) | 69 (41.8) | 65 (40.6) | 54 (34.2) | |
| Ethnicity (Caucasian),d n (%) | 465 (96.3) | 161 (97.6) | 154 (96.3) | 150 (94.9)e | 0.457 |
| First language (French),f n (%) | 437 (90.5) | 151 (91.5) | 146 (91.3) | 140 (88.6) | 0.931 |
| Highest level of education completed,g n (%) | 0.664 | ||||
| None or elementary school | 132 (27.3) | 48 (29.1) | 41 (25.6) | 43 (27.2) | |
| High-school | 170 (35.2) | 54 (32.7) | 61 (38.1) | 55 (34.8) | |
| College-technical school or CEGEP | 90 (18.6) | 26 (15.8) | 30 (18.8) | 34 (21.5) | |
| University | 87 (18.0) | 36 (21.8) | 28 (17.5) | 23 (14.6) | |
| Civil status,h n (%) | 0.034 | ||||
| Married or common law | 263 (54.5) | 98 (59.4) | 91 (56.9) | 74 (46.8) | |
| Single | 64 (13.3) | 15 (9.1) | 19 (11.9) | 30 (19.0) | |
| Separated/divorced | 98 (20.3) | 27 (16.4) | 33 (20.6) | 38 (24.1) | |
| Widowed | 57 (11.8) | 25 (15.2) | 16 (10.0) | 16 (10.1) | |
| Annual family income,i n (%) | 0.011 | ||||
| <$20,000 | 128 (26.5) | 33 (20.0) | 36 (22.5) | 59 (37.3) | |
| $20,000–$50,000 | 188 (38.9) | 66 (40.0) | 66 (41.3) | 56 (35.4) | |
| >$50,000 | 117 (24.2) | 44 (26.7) | 42 (26.3) | 31 (19.6) | |
| Current work status,j,k n (%) | <0.0001 | ||||
| Full-time job | 93 (19.3) | 43 (26.1) | 33 (20.6) | 17 (10.8) | |
| Part-time job | 22 (4.6) | 9 (5.5) | 9 (5.6) | 4 (2.5) | |
| Temporary disability | 19 (3.9) | 2 (1.2) | 7 (4.4) | 10 (6.3) | |
| Permanent disability | 86 (17.8) | 16 (9.7) | 24 (15.0) | 46 (29.1) | |
Notes:
Patients in the first BPI tertile (scores ranging from 0–4.3)
patients in the second BPI tertile (scores ranging from 4.31–6.4)
patients in the third BPI tertile (scores ranging from 6.41–10.0)
additional categories were reported: Black; Native American; Hispanic; Asian; and other
one patient refused to answer
additional categories were reported: English; Spanish; Italian; Portuguese; German; Arabic; Chinese; Japanese; and Vietnamese
one and three patients refused to answer in the mild and severe disability groups, respectively
one patient refused to answer in the moderate disability group
twenty-two, 16, and 12 patients refused to answer in the mild, moderate, and severe disability groups, respectively
additional categories were reported: homemaker; student; unemployed; laid off; and volunteer
two, seven, and four patients refused to answer in the mild, moderate, and severe disability groups, respectively.
Abbreviations: n, number; SD, standard deviation; RAMQ, Régie de l’assurance maladie du Québec; CEGEP, Collège d’enseignement général et professionnel; BPI, Brief Pain Inventory.
Clinical and psychological characteristics
As reported in Table 2, on average, individuals suffered from pain for 12 years (±11 years). The proportion of patients reporting a pain duration of 4 years or more tended to be higher among those with more severe pain disability. In terms of pain frequency, the majority (75.2%) were suffering continuously. Patients reported a mean pain intensity score of 6.5 (±1.9) in the past week. Based on the Hospital Anxiety and Depression Scale46, 24.0% and 40.0% of participants probably suffered from depression and anxiety, respectively. The mean number of reported pain diagnoses per individual was 2.5 (±1.3), the most frequent being chronic back pain (64.0%) and degenerative osteopathies such as osteoarthritis and arthrosis (60.7%). Patients classified in the severe disability category reported more frequent and more intense pain than those in the mild and moderate categories. They were also more likely to feel depressed and anxious, experience more pain-related sleep problems, and suffer from multiple pain syndromes.
Table 2.
Clinical and psychosocial characteristics
| All patients (n=483) | Patients stratified by level of pain disability
|
P-values | |||
|---|---|---|---|---|---|
| Mild disabilitya (n=165) | Moderate disabilityb (n=160) | Severe disabilityc (n=158) | |||
| Duration of pain (years), mean (SD) | 12 (11) | 11 (11) | 11 (11)d | 13 (12) | 0.186 |
| Duration of pain, n (%)d | 0.003 | ||||
| 6–12 months | 37 (7.7) | 17 (10.3) | 12 (7.5) | 8 (5.1) | |
| 13–14 months | 1 (0.2) | 1 (0.6) | 0 (0.0) | 0 (0.0) | |
| 15–36 months | 74 (15.3) | 35 (21.2) | 23 (14.4) | 16 (10.1) | |
| 37–48 months | 32 (6.6) | 6 (3.6) | 12 (7.5) | 14 (8.9) | |
| 49 months or more | 338 (70.0) | 106 (64.2) | 112 (70.0) | 120 (75.9) | |
| Frequency of pain in the past 7 days, n (%) | 0.000 | ||||
| Always | 363 (75.2) | 99 (60.0) | 125 (78.1) | 139 (88.0) | |
| Occasionally | 116 (24.0) | 62 (37.6) | 35 (21.9) | 19 (12.0) | |
| Never | 4 (0.8) | 4 (2.4) | 0 (0.0) | 0 (0.0) | |
| Average pain intensity in the past 7 days, mean (SD) | 6.5 (1.9) | 5.5 (1.9)e | 6.7 (1.6) | 7.3 (1.6) | 0.000 |
| Pain functional impact score,f mean (SD) | 5.3 (2.2) | 2.8 (1.2) | 5.5 (0.6) | 7.7 (0.8) | 0.000 |
| Depression,g n (%) | 116 (24.0) | 5 (3.0) | 38 (23.8) | 73 (46.2)d | 0.000 |
| Anxiety,g n (%) | 193 (40.0) | 34 (20.6) | 70 (43.8) | 89 (56.3)d | 0.000 |
| Pain sleep impact score,h mean (SD) | 5.1 (2.9) | 3.3 (2.6) | 5.4 (2.7) | 6.6 (2.4) | 0.000 |
| Comorbidity index,i mean (SD) | 2.5 (1.9) | 2.6 (2.0) | 2.3 (1.7) | 2.5 (1.9) | 0.303 |
| Number of self-reported pain diagnoses per patient, mean (SD) | 2.5 (1.3) | 2.3 (1.2) | 2.4 (1.3) | 2.9 (1.5) | 0.000 |
| Self-reported pain diagnoses, n (%)j | |||||
| Chronic back pain | 309 (64.0) | 90 (54.5) | 104 (65.0) | 115 (72.8) | 0.003 |
| Chronic neck pain | 186 (38.5) | 52 (31.5) | 60 (37.5) | 74 (46.8) | 0.017 |
| Fibromyalgia | 114 (23.6) | 33 (20.0) | 33 (20.6) | 48 (30.4) | 0.050 |
| Osteoarthritis, arthrosis, and other degenerative osteopathies | 293 (60.7) | 102 (61.8) | 88 (55.0) | 103 (65.2) | 0.165 |
| Rheumatoid arthritis and other inflammatory osteopathies | 55 (11.4) | 17 (10.3) | 17 (10.6) | 21 (13.3) | 0.653 |
| Tendinitis, bursitis, capsulitis, and epicondylitis | 101 (20.9) | 28 (17.0) | 35 (21.9) | 38 (24.1) | 0.275 |
| Visceral pain | 74 (15.3) | 16 (9.7) | 22 (13.8) | 36 (22.8) | 0.004 |
| Neuropathic pain | 88 (18.2) | 38 (23.0) | 26 (16.3) | 24 (15.2) | 0.139 |
Notes:
Patients in the first BPI tertile (scores ranging from 0–4.3)
patients in the second BPI tertile (scores ranging from 4.31–6.4)
patients in the third BPI tertile (scores ranging from 6.41–10.0)
one missing value
two missing values
BPI questionnaire
Hospital Anxiety and Depression Scale; presence of depression and anxiety disorder is probable when score ≥11
Chronic Pain Sleep Inventory questionnaire
Charlson Comorbidity Index
individuals could report more than one diagnosis.
Abbreviations: n, number; SD, standard deviation; BPI, Brief Pain Inventory.
Health care resource utilization and productivity losses
Individuals were hospitalized for an average of 1.9 (9.9) days annually, where 1.1 (8.3) days were possibly related to CNCP (Table 3). Overall, 19.7% of the cohort of patients were hospitalized (all causes considered) and 8.9% of the cohort of patients were hospitalized for a cause that was possibly related to pain (data not reported in table). During this 1-year period, participants visited the ER 0.9 times (±1.6) on average and saw primary care physicians and specialists for an average of 4.8 (±4.9) times and 2.1 (±3.1) times, respectively. Patients reporting more pain disability were more likely to have visited the ER or be seen by primary care physicians and specialists. The majority of participants (56.1%) reported at least one visit to a health care professional other than a physician (data not reported in table), with an annual number of visits per patient averaging 74.6 (±135.5). Physiotherapists and massage therapists were the most frequently seen with an average of 40.3 (±90.1) visits per patient and 13.5 (±48.8) visits per patient, respectively. In terms of pain medication, individuals took an average of 3.9 (±2.0) and 1.5 (±1.6) different prescribed and over-the-counter medications to treat pain and/or the adverse effects of pain treatments, respectively. The number of prescribed medications was the highest among patients classified in the severe pain disability subgroup. Patients with more pain disability were more likely to have opioid analgesics dispensed in the year prior to recruitment: mild, 49%; moderate, 68%; and severe, 80%; P=0.0001. Among those on opioids, 19 patients were dispensed a high oral morphine-equivalent dose (>200 mg per day). These patients were equally distributed across the pain disability subgroups (data not reported in table).
Table 3.
Annual health care resource utilization and productivity losses per patient
| Mean (SD) | All patients (n=483) | Patients stratified by level of pain disability
|
P-value | ||
|---|---|---|---|---|---|
| Mild disabilitya (n=165) | Moderate disabilityb (n=160) | Severe disabilityc (n=158) | |||
| Health care resources utilization per patient | |||||
| Number of hospitalization days | |||||
| All causes | 1.9 (9.9) | 1.1 (5.8) | 3.2 (15.1) | 1.5 (5.5) | 0.146 |
| Pain-related as possible cause | 1.1 (8.3) | 0.7 (5.6) | 1.8 (12.6) | 0.8 (4.2) | 0.468 |
| Number of physician visits | |||||
| Primary care | 0.4 (2.7) | 0.2 (1.3) | 0.4 (2.3) | 0.6 (3.9) | 0.423 |
| Specialists | 1.1 (4.4) | 0.8 (3.8) | 1.4 (5.5) | 1.1 (3.7) | 0.449 |
| Number of emergency room visits | 0.9 (1.6) | 0.6 (1.3) | 0.9 (1.8) | 1.1 (1.7) | 0.046 |
| Number of physician visits at emergency | |||||
| Primary care | 0.2 (1.3) | 0.2 (1.3) | 0.2 (1.3) | 0.3 (1.2) | 0.645 |
| Specialists | 0.9 (3.3) | 0.4 (1.9) | 1.2 (4.0) | 1.1 (3.7) | 0.085 |
| Number of outpatient physician visits | |||||
| Primary care | 4.8 (4.9) | 4.4 (3.9) | 4.1 (4.1) | 6.0 (6.3) | 0.001 |
| Specialists | 2.1 (3.1) | 1.9 (2.7) | 1.8 (2.7) | 2.8 (3.8) | 0.008 |
| Number of outpatient tests and interventions | |||||
| All | 10.7 (7.5) | 10.0 (6.9) | 10.6 (8.1) | 11.6 (7.3) | 0.136 |
| Pain-related | 1.4 (1.8) | 1.2 (1.6) | 1.5 (1.9) | 1.4 (1.8) | 0.322 |
| Number of complementary health care provider visits | |||||
| Psychotherapists | 2.7 (13.4) | 1.7 (9.5) | 2.9 (14.7) | 3.5 (15.4) | 0.451 |
| Physiotherapists | 40.3 (90.1) | 31.3 (75.5) | 45.3 (98.0) | 44.6 (95.6) | 0.291 |
| Massage therapists | 13.5 (48.8) | 9.0 (34.3) | 15.1 (49.6) | 16.5 (59.6) | 0.336 |
| Occupational therapists | 5.4 (30.7) | 4.4 (30.6) | 6.4 (29.4) | 5.4 (32.3) | 0.848 |
| Acupuncturists | 4.3 (21.3) | 4.7 (19.9) | 4.2 (18.6) | 4.0 (25.1) | 0.946 |
| Osteopaths | 4.2 (18.0) | 6.4 (22.8) | 3.6 (16.8) | 2.7 (12.8) | 0.159 |
| Chiropractors | 4.2 (18.9) | 6.3 (23.8) | 2.3 (12.4) | 3.9 (18.5) | 0.157 |
| Total | 74.6 (135.5) | 63.9 (110.8) | 79.7 (142.7) | 80.7 (150.8) | 0.454 |
| Number of prescribed pain-related medicationsd | 3.9 (2.0) | 3.4 (1.9) | 4.1 (2.0) | 4.2 (2.0) | 0.000 |
| Number of over-the-counter pain-related medicationsd | 1.5 (1.6) | 1.5 (1.6) | 1.5 (1.7) | 1.5 (1.6) | 0.897 |
| Annual productivity losses per patient | |||||
| Number of absenteeism dayse | 57.3 (106.3) | 32.9 (83.4) | 54.9 (104.7) | 85.3 (122.0) | 0.000 |
| Number of presenteeism daysf | 12.1 (36.0) | 8.7 (24.1) | 19.0 (46.7) | 8.7 (33.0) | 0.012 |
| Total number of workdays lost | 69.4 (111.3) | 41.6 (86.3) | 73.9 (114.5) | 94.0 (124.7) | 0.000 |
Notes:
Patients in the first BPI tertile (scores ranging from 0–4.3)
patients in the second BPI tertile (scores ranging from 4.31–6.4)
patients in the third BPI tertile (scores ranging from 6.41–10.0)
including analgesic and medication to treat side effects of analgesics
individuals with full- or part-time jobs, as well as those on temporary or permanent disability were included. A null value was computed for all other individuals
only individuals answering yes to the question “Do you currently have a paid job?” and those having a full- or part-time job were included. A null value was computed for all other individuals.
Abbreviations: SD, standard deviation; n, number; BPI, Brief Pain Inventory.
Work productivity data revealed that individuals lost an equivalent of 69.4 (±111.3) workdays annually due to pain or its treatment; the number of days lost due to absenteeism and presenteeism averaged 57.3 (±106.3) days and 12.1 (±36.0) days, respectively. Annual workdays lost were higher in individuals with more severe pain disability.
Unadjusted direct health care and productivity costs
The mean annual total direct health care costs per patient averaged CAD $7,334 (±$9,276), CAD $11,128 (±$19,131), and CAD $10,311 (±$11,501) for patients with mild, moderate, and severe pain disability, respectively (Table 4). Major cost components included nonpharmacologic health care services, which accounted for 47.1% (CAD $4,505/CAD $9,565) of the total direct health care costs, hospitalizations and ER visits (24.6%), prescribed medications (20.5%), and outpatient medical visits (6.3%). For patients with mild, moderate, and severe pain disability, productivity costs per patient averaged CAD $4,523 (±$8,951), CAD $8,254 (±$13,386), and CAD $8,536 (±$12,077), respectively. Absenteeism and presenteeism costs accounted for 71.4% and 28.6% of those costs, respectively. When combining the direct health care costs and productivity costs, the mean annual costs per patient were equal to CAD $11,857 (±$13,685), CAD $19,382 (±$23,228), and CAD $18,847 (±$18,734) for patients with mild, moderate, and severe pain disability, respectively. The costs of hospitalizations, outpatient visits, prescribed medications, and total costs were found to be significantly and positively related to the level of pain disability.
Table 4.
Crude annual direct health care costs and productivity costs (CAD dollars) per patient
| Mean (SD) | All patients (n=483) | Patients stratified by level of pain disability
|
P-values | ||
|---|---|---|---|---|---|
| Mild disabilitya (n=165) | Moderate disabilityb (n=160) | Severe disabilityc (n=158) | |||
| Direct health care costs | |||||
| Hospitalizations | |||||
| All hospitalization costs, except physician visits | 1,908 (9,877) | 1,148 (5,849) | 3,117 (15,080) | 1,480 (5,583) | 0.021 |
| Pain-related hospitalization costs | 1,102 (8,304) | 739 (5,555) | 1,763 (12,610) | 810 (4,213) | 0.043 |
| General practitioner visits | 14 (98) | 9 (47) | 13 (91) | 22 (137) | 0.004 |
| Specialist visits | 114 (321) | 106 (307) | 138 (380) | 99 (267) | 0.508 |
| Total costs | 2,036 (10,137) | 1,262 (6,053) | 3,266 (15,404) | 1,600 (5,878) | 0.030 |
| Emergency room visits | |||||
| Emergency room costs | 250 (481) | 179 (369) | 267 (553) | 308 (498) | 0.150 |
| General practitioner visits | 8 (44) | 5 (33) | 6 (42) | 13 (55) | 0.001 |
| Specialist visits | 62 (289) | 43 (260) | 65 (262) | 78 (341) | 0.455 |
| Total costs | 320 (686) | 227 (528) | 338 (753) | 399 (752) | 0.148 |
| Outpatient medical consultations | |||||
| Primary care visits | 231 (247) | 211 (205) | 204 (233) | 278 (291) | 0.129 |
| Specialist visits | 163 (240) | 137 (195) | 144 (222) | 209 (290) | 0.094 |
| All outpatient tests and interventions | 145 (170) | 132 (163) | 149 (186) | 152 (161) | 0.699 |
| Pain-related tests and interventions | 66 (102) | 50 (80) | 75 (116) | 72 (105) | 0.115 |
| Total costs | 604 (541) | 531 (437) | 573 (561) | 712 (602) | 0.048 |
| Complementary health care provider visits | |||||
| Psychotherapists | 257 (1,276) | 160 (902) | 279 (1,400) | 335 (1,466) | 0.103 |
| Physiotherapists | 2,337 (5,231) | 1,818 (4,382) | 2,626 (5,688) | 2,586 (5,546) | 0.528 |
| Massage therapists | 781 (2,830) | 521 (1,992) | 873 (2,876) | 959 (3,457) | 0.181 |
| Occupational therapists | 343 (1,944) | 281 (1,937) | 405 (1,861) | 345 (2,043) | 0.607 |
| Acupuncturists | 249 (1,235) | 274 (1,153) | 243 (1,077) | 230 (1,455) | 0.875 |
| Osteopaths | 339 (1,426) | 507 (1,801) | 288 (1,326) | 216 (1,011) | 0.043 |
| Chiropractors | 198 (899) | 299 (1,131) | 108 (587) | 185 (880) | 0.013 |
| Total costs | 4,505 (8,115) | 3,860 (6,706) | 4,822 (8,599) | 4,856 (8,924) | 0.640 |
| Prescribed analgesics and medication to treat side effects of medication | 1,963 (2,978) | 1,304 (1,728) | 1,979 (3,029) | 2,635 (3,728) | <0.001 |
| Over-the-counter analgesics and medication to treat side effects | 136 (601) | 150 (709) | 150 (708) | 108 (275) | 0.341 |
| Total direct health care costs | 9,565 (13,993) | 7,334 (9,276) | 11,128 (19,131) | 10,311 (11,501) | 0.008 |
| Productivity costs | |||||
| Absenteeism | 5,052 (9,429) | 3,068 (7,677) | 5,084 (9,743) | 7,091 (10,339) | 0.082 |
| Presenteeism | 2,020 (6,013) | 1,455 (4,027) | 3,171 (7,804) | 1,445 (5,511) | 0.057 |
| Total productivity costs | 7,072 (11,716) | 4,523 (8,951) | 8,254 (13,386) | 8,536 (12,077) | 0.158 |
| Total overall costs | 16,636 (19,182) | 11,857 (13,685) | 19,382 (23,228) | 18,847 (18,734) | <0.001 |
Notes:
Patients in the first BPI tertile (scores ranging from 0–4.3)
patients in the second BPI tertile (scores ranging from 4.31–6.4)
patients in the third BPI tertile (scores ranging from 6.41–10.0).
Abbreviations: CAD, Canadian; SD, standard deviation; n, number; BPI, Brief Pain Inventory.
Adjusted direct health care costs and productivity costs
Once they were adjusted for age, sex, pain duration, and Charlson comorbidity scores, the mean annual direct costs per patient averaged CAD $7,374 (95% CI: $5,819–$8,930), CAD $10,524 (95% CI: $8,383–$12,665), and CAD $9,546 (95% CI: $7,502–$11,590) for patients with mild, moderate, and severe pain disability, respectively (Table 5). Productivity costs were CAD $3,005 (95% CI: $1,587–$4,422), CAD $5,083 (95% CI: $2,647–$7,519), and CAD $5,385 (95% CI: $2,789–$7,981) for each group, with total costs adding up to CAD $12,913 (95% CI: $10,534–$15,292), CAD $17,970 (95% CI: $14,782–$21,159), and CAD $17,292 (95% CI: $14,075–$20,510). A significant positive association was observed between the level of pain disability, as well as the total adjusted direct health care costs (considering pain-related hospitalizations only) and productivity costs: mild disability, CAD $12,118; moderate disability, CAD $18,278; and severe disability, CAD $19,216; P=0.001.
Table 5.
Adjusted annual direct health care costs and productivity costs (CAD dollars) per patient
| Mean (95% CI) | Mild disabilitya (n=165) | Moderate disabilityb (n=160) | Severe disabilityc (n=158) | P-values |
|---|---|---|---|---|
| Direct health care costs | ||||
| Hospitalization | ||||
| All-cause hospitalizations | 897 (415; 1,380) | 2,857 (1,348; 4,365) | 2,021 (849; 3,193) | 0.012 |
| Pain-related hospitalizations | 326 (146; 507) | 1,700 (707; 2,693) | 883 (224; 1,542) | 0.001 |
| Emergency room visits | 228 (137; 319) | 339 (202; 476) | 400 (238; 563) | 0.149 |
| Outpatient consultation visits | 532 (441; 622) | 574 (475; 673) | 713 (589; 837) | 0.048 |
| Complementary health care provider visits | 4,165 (2,553; 5,776) | 4,279 (2,638; 5,921) | 4,345 (2,665; 6,024) | 0.989 |
| Prescribed analgesics | 1,428 (1,143; 1,713) | 1,976 (1,589; 2,363) | 2,330 (1,848; 2,812) | 0.004 |
| Over-the-counter analgesics | 112 (74; 150) | 138 (91; 185) | 116 (76; 155) | 0.646 |
| Total | 7,374 (5,819; 8,930) | 10,524 (8,383; 12,665) | 9,546 (7,502; 11,590) | 0.051 |
| Productivity costs | ||||
| Absenteeism | 2,320 (1,179; 3,460) | 3,175 (1,587; 4,763) | 4,922 (2,449; 7,395) | 0.108 |
| Presenteeism | 826 (368; 1,284) | 1,761 (841; 2,681) | 300 (130; 469) | 0.000 |
| Total | 3,005 (1,587; 4,422) | 5,083 (2,647; 7,519) | 5,385 (2,789; 7,981) | 0.194 |
| Total direct health care and productivity costs | ||||
| Including all cause hospitalizations | 12,913 (10,534; 15,292) | 17,970 (14,782; 21,159) | 17,292 (14,075; 20,510) | 0.024 |
| Including pain-related hospitalizations | 12,118 (9,844; 14,393) | 18,278 (14,909; 21,648) | 19,216 (15,538; 22,894) | 0.001 |
Notes:
Patients in the first BPI tertile (scores ranging from 0–4.3)
patients in the second BPI tertile (scores ranging from 4.31–6.4)
patients in the third BPI tertile (scores ranging from 6.41–10.0).
Abbreviations: CAD, Canadian; CI, confidence interval; n, number; BPI, Brief Pain Inventory.
Discussion
This is one of the rare studies providing a comprehensive evaluation of the economic burden of CNCP in a large cohort of patients followed up in primary care. The direct health care costs of CNCP in this cohort of patients represented nearly 60% of the total direct health care and productivity costs. The use of complementary health care services accounted for almost 50% of the direct costs. The total direct health care and productivity costs averaged CAD $16,636 per patient per year and varied according to the level of pain disability – the more disabled the patients were, the higher the costs were. Although high, these numbers represent only a portion of the true costs since they do not include other indirect costs such as patients’ travel expenses, paid household help, expenses incurred by family members, and so on.
Complementary health care services (for example, physiotherapy, massage therapy, occupational therapy) are known to be extensively used by individuals with CNCP,7,53 including those with chronic low back pain.54 Not considering these costs may, therefore, lead to an important underestimation of the direct health care costs of CNCP and may explain discrepancies among studies. For example, Lachaine et al12 estimated that the annual direct health care costs associated with neuropathic painful disorders in Quebec (Canada) averaged CAD $4,065 per patient (±$6,798 [2007 values]; $4,339 [2011 values]). In another study on the costs associated with fibromyalgia in Quebec,11 the direct health care costs added up to CAD $4,163 (±$7,536 [2002 values]; $4,960 [2011 values]). Differences with our results might be explained by the fact that complementary health care services were not considered in these studies.
In patients with chronic pain, higher than normal absenteeism rates,2 as well as significant interference with work performance,8 have been reported. In our study, the mean annual cost associated with productivity losses represented about 40% of the total direct health care and productivity costs. This proportion is consistent with earlier observations made in individuals suffering from fibromyalgia syndrome55 and chronic low back pain54 where the proportion of costs associated with productivity losses accounted for more than half of the total costs. Similar observations were also made by Guerriere et al24 in a population of chronic pain patients waiting for treatment in tertiary care pain clinics. Although they remain insufficiently documented, presenteeism costs should be systematically taken into consideration, as illustrated by an Australian and an American study where these costs accounted for the majority of the CNCP costs.14,21
When combined, the direct health care costs and productivity costs led to mean annual total costs of CAD $16,636 per patient, which compares with previous estimates in fibromyalgia (US $15,000 [2009 values]; CAD $15,489 [2011 values]),56 chronic low back pain (US $19,473 [2002 values]; CAD $23,566 [2011 values]),54 and osteoarthritis (US $16,146 [2005 values]; CAD $18,189 [2011 values]).57 Other studies have also reported that economic burden increases with the severity of pain disability. For example, among individuals with rheumatoid arthritis, increases in self-report disability status, as measured by the Health Assessment Questionnaire, were associated with higher costs.17,18,58,59 Costs incurred by chronic low back pain and by neuropathic pain were also found to vary as a function of the degree of disability levels.54,60 However, the present study is the first to demonstrate this association for a variety of chronic pain diagnoses in a primary care setting.
Strengths and limitations
Like any other study, the present one has some limitations that must be taken into consideration. Patients were recruited only if they had an active analgesic prescription from a primary care physician in their pharmacy chart. Our results cannot be extrapolated to those having no active analgesic prescriptions or only prescriptions from a specialist. Furthermore, some of our results are based on patient self-reports and may be influenced by social desirability (tendency to answer questions in a manner that will be viewed favorably by others) and memory biases. However, the research assistants who conducted the telephone interviews were well trained and used a structured interview protocol. Self-administered questionnaires were used to document more sensitive information such as levels of depression and anxiety. Some assumptions were also made to estimate the annual costs. Annual productivity costs, as well as annual use of over-the-counter medication and complementary health care services, were estimated using data covering a 6-month period. This may have resulted in an overestimation or underestimation of costs, as resource utilization rates may have changed over time. Furthermore, the frequency of use was not precisely documented. Finally, we took into account the direct costs to patients associated with different self-management techniques (eg cost of physiotherapy). However, we did not consider the impact this may have on caregiver time (eg time absent from work for the patient’s wife).
Despite those limitations, this study offers a comprehensive description of the direct health care costs and productivity costs associated with CNCP. The use of administrative databases and pharmacy charts enabled the precise documentation of prescribed pharmacological treatments of participants, as well as their use of health care resources. Furthermore, we also assessed the use of over-the-counter medication and complementary health care services, both documented through telephone interviews with the patients. The structured interview protocol also allowed for the documentation of productivity losses due to pain or its treatment, which were further translated into productivity costs based on the method previously described by Hu et al.42
Conclusion
CNCP among primary care patients is associated with substantial economic burden not only for the health care system and the workforce, but also for patients themselves. These costs tend to increase as pain causes more limitations in a patient’s daily activities. Further research is clearly needed to improve the management of CNCP in primary care. Finding efficient strategies to reduce further chronicity of pain problems is certainly an avenue that needs to be explored, as it could alleviate not only the burden of illness, but also its associated costs.
Supplementary materials
Table S1.
Hospitalization codes related or possibly related to chronic pain
| • Adhesive capsulitis of shoulder |
| • Algoneurodystrophy, unspecified |
| • Arthritis, unspecified |
| • Articular ankylosis |
| • Articular ankylosis – knee joint |
| • Carpal tunnel syndrome |
| • Cervicalgia |
| • Chronic intractable pain |
| • Chronic salpingitis and oophoritis |
| • Coxarthrosis, unspecified |
| • Endometriosis of uterus |
| • Endometriosis, unspecified |
| • Fibromyalgia |
| • Gonarthrosis, unspecified |
| • Gout, unspecified |
| • Idiopathic gout – elbow joint |
| • Idiopathic gout – hand joints |
| • Irritable bowel syndrome with diarrhea |
| • Irritable bowel syndrome without diarrhea |
| • Lateral epicondylitis |
| • Low back pain |
| • Osteoarthritis, unspecified |
| • Other cervical disc displacement |
| • Other dorsalgia |
| • Other specified arthrosis |
| • Other specified disorders of bone – leg |
| • Other specified intervertebral disc displacement |
| • Other specified spondylopathies – cervical region |
| • Pain in limb – scapular region |
| • Radiculopathy – dorsal region |
| • Rheumatoid arthritis, unspecified |
| • Rotator cuff syndrome |
| • Spinal instabilities – lumbar region |
| • Spinal stenosis – cervical region |
| • Spinal stenosis – lumbar region |
| • Spondylosis, unspecified – lumbar region |
Table S2.
Documented analgesics
| Therapeutic class | International common denomination |
|---|---|
| Anticonvulsants | |
| Carboxylic acid derivatives | Valproic acid |
| Gamma-aminobutyric acid analogs | Gabapentin, Pregabalin |
| Iminostilbene | Carbamazepine, Oxcarbazepine |
| Other anticonvulsants | Divalproex, Lamotrigine, Topiramate |
| Antidepressants | |
| Selective serotonin reuptake inhibitors | Citalopram, Escitalopram, Fluoxetine, Fluvoxamine, Paroxetine, Sertraline, Trazodone |
| Serotonin and noradrenaline reuptake inhibitors | Duloxetine, Venlafaxine |
| Tricyclic and tetracyclic antidepressants | Amitriptyline, Clomipramine, Desipramine, Doxepin, Imipramine, Maprotiline, Mirtazapine, Nortriptyline, Trimipramine |
| Other antidepressants | Bupropion |
| Antiretroviral | Acyclovir, Famciclovir, Valacyclovir |
| Disease-modifying antirheumatic drugs | Auranofin, Aurothioglucose, Aurothiomalate, Azathioprine, Chloroquine, Cyclosporine, D-penicillamine, Hydroxychloroquine, Leflunomide, Methotrexate, Sulfasalazine |
| Muscle relaxants | |
| Benzodiazepine | Diazepam, Tetrazepam |
| Carbamic acid derivatives | Methocarbamol |
| Centrally acting myorelaxants | Cyclobenzaprine, Tizanidine |
| Gamma-aminobutyric acid derivatives | Baclofen |
| Other muscle relaxants | Thiocolchicoside |
| Nonsteroidal antiinflammatory | |
| Acetic acids | Diclofenac, Etodolac, Indomethacin, Ketorolac, Nabumetone |
| Acetylsalicylic acid | |
| Coxibs | Celecoxib |
| Fenamates | Meclofenamate, Mefenamic acid |
| Oxicams | Meloxicam, Piroxicam |
| Propionic acids | Fenoprofen, Flurbiprofen, Ibuprofen, Ketoprofen, Naproxen, Oxaprozin |
| Opioids | |
| Agonist–antagonist derivatives | Buprenorphine, Butorphanol, Nalbuphine, Pentazocine |
| Antagonists | Naloxone |
| Benzomorphan derivatives | Pentazocine |
| Centrally acting analgesics | Tramadol |
| Meperidine-like agonists | Fentanyl, Meperidine |
| Methadone-like agonists | Methadone, Propoxyphene |
| Morphine-like agonists | Codeine, Hydrocodone, Hydromorphone, Levorphanol, Morphine, Oxycodone, Oxymorphone |
| Natural cannabinoids | Tetrahydrocannabinol, Cannabidiol |
| Synthetic cannabinoids | Dronabinol, Nabilone |
Acknowledgments
We are grateful for the excellent collaboration of community pharmacists and patients who took part in this project. This work was conducted as part of the master research project of Alexandra Beaulieu-Boivin. We acknowledge her time and effort in the conduct of this analysis. Special thanks to Chantal Legris for the preparation and submission of this article. Lyne Lalonde and Sylvie Perreault are scientists supported by the Fonds de recherche du Québec – Santé.
Footnotes
Disclosure
This study was funded by a team grant – Community Alliances for Health Research and Knowledge Exchange in Pain of the Canadian Institutes of Health Research (CIHR) in partnership with AstraZeneca Canada Inc. (Grant # 86787), and by Pfizer Canada Inc. The authors report no other conflicts of interest in this work.
References
- 1.Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl. 1986;3:S1–S226. [PubMed] [Google Scholar]
- 2.Moulin DE, Clark AJ, Speechley M, Morley-Forster PK. Chronic pain in Canada – prevalence, treatment, impact and the role of opioid analgesia. Pain Res Manag. 2002;7(4):179–184. doi: 10.1155/2002/323085. [DOI] [PubMed] [Google Scholar]
- 3.Boulanger A, Clark AJ, Squire P, Cui E, Horbay GL. Chronic pain in Canada: have we improved our management of chronic noncancer pain? Pain Res Manag. 2007;12(1):39–47. doi: 10.1155/2007/762180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Millar WJ. Chronic pain. Health Rep. 1996;7(4):47–53. [PubMed] [Google Scholar]
- 5.Ospina M, Harstall C. Prevalence of Chronic Pain: An Overview. Edmonton, AB: Alberta Heritage Foundation for Medical Research; 2002. [Accessed April 6, 2011]. Available from: http://ihe.ca/documents/prevalence_chronic_pain_0.pdf. [Google Scholar]
- 6.Kerr S, Fairbrother G, Crawford M, Hogg M, Fairbrother D, Khor KE. Patient characteristics and quality of life among a sample of Australian chronic pain clinic attendees. Intern Med J. 2004;34(7):403–409. doi: 10.1111/j.1444-0903.2004.00627.x. [DOI] [PubMed] [Google Scholar]
- 7.Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10(4):287–333. doi: 10.1016/j.ejpain.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 8.Gureje O, Von Korff M, Simon GE, Gater R. Persistent pain and well-being: a World Health Organization Study in Primary Care. JAMA. 1998;280(2):147–151. doi: 10.1001/jama.280.2.147. [DOI] [PubMed] [Google Scholar]
- 9.McWilliams LA, Cox BJ, Enns MW. Mood and anxiety disorders associated with chronic pain: an examination in a nationally representative sample. Pain. 2003;106(1–2):127–133. doi: 10.1016/s0304-3959(03)00301-4. [DOI] [PubMed] [Google Scholar]
- 10.Fautrel B, Clarke AE, Guillemin F, et al. Costs of rheumatoid arthritis: new estimates from the human capital method and comparison to the willingness-to-pay method. Med Decis Making. 2007;27(2):138–150. doi: 10.1177/0272989X06297389. [DOI] [PubMed] [Google Scholar]
- 11.Lachaine J, Beauchemin C, Landry PA. Clinical and economic characteristics of patients with fibromyalgia syndrome. Clin J Pain. 2010;26(4):284–290. doi: 10.1097/AJP.0b013e3181cf599f. [DOI] [PubMed] [Google Scholar]
- 12.Lachaine J, Gordon A, Choinière M, Collet JP, Dion D, Tarride JE. Painful neuropathic disorders: an analysis of the Régie de l’Assurance Maladie du Québec database. Pain Res Manag. 2007;12(1):31–37. doi: 10.1155/2007/713835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agence d’évaluation des technologies et des modes d’intervention en santé . Management of Chronic (Non-Cancer) Pain: Organization of Health Services. Montreal, QC: Agence d’évaluation des technologies et des modes d’intervention en santé; 2006. [Google Scholar]
- 14.van Leeuwen MT, Blyth FM, March LM, Nicholas MK, Cousins MJ. Chronic pain and reduced work effectiveness: the hidden cost to Australian employers. Eur J Pain. 2006;10(2):161–166. doi: 10.1016/j.ejpain.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 15.Kumpusalo E, Mäntyselkä P, Takala J. Chronic pain in primary care. Fam Pract. 2000;17(4):352. doi: 10.1093/fampra/17.4.352. [DOI] [PubMed] [Google Scholar]
- 16.Pizzi LT, Carter CT, Howell JB, Vallow SM, Crawford AG, Frank ED. Work loss, healthcare utilization, and costs among US employees with chronic pain. Disease Management and Health Outcomes. 2005;13(3):201–208. [Google Scholar]
- 17.Michaud K, Messer J, Choi HK, Wolfe F. Direct medical costs and their predictors in patients with rheumatoid arthritis: a three-year study of 7,527 patients. Arthritis Rheum. 2003;48(10):2750–2762. doi: 10.1002/art.11439. [DOI] [PubMed] [Google Scholar]
- 18.Yelin E, Wanke LA. An assessment of the annual and long-term direct costs of rheumatoid arthritis: the impact of poor function and functional decline. Arthritis Rheum. 1999;42(6):1209–1218. doi: 10.1002/1529-0131(199906)42:6<1209::AID-ANR18>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 19.Clarke AE, Zowall H, Levinton C, et al. Direct and indirect medical costs incurred by Canadian patients with rheumatoid arthritis: a 12 year study. J Rheumatol. 1997;24(6):1051–1060. [PubMed] [Google Scholar]
- 20.Burton W, Morrison A, Maclean R, Ruderman E. Systematic review of studies of productivity loss due to rheumatoid arthritis. Occup Med (Lond) 2006;56(1):18–27. doi: 10.1093/occmed/kqi171. [DOI] [PubMed] [Google Scholar]
- 21.Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13(8):715–724. doi: 10.1016/j.jpain.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 22.Maetzel A, Li LC, Pencharz J, Tomlinson G, Bombardier C, Community Hypertension and Arthritis Project Study Team The economic burden associated with osteoarthritis, rheumatoid arthritis, and hypertension: a comparative study. Ann Rheum Dis. 2004;63(4):395–401. doi: 10.1136/ard.2003.006031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Penrod JR, Bernatsky S, Adam V, Baron M, Dayan N, Dobkin PL. Health services costs and their determinants in women with fibromyalgia. J Rheumatol. 2004;31(7):1391–1398. [PubMed] [Google Scholar]
- 24.Guerriere DN, Choinière M, Dion D, et al. The Canadian STOP-PAIN project – Part 2: What is the cost of pain for patients on waitlists of multidisciplinary pain treatment facilities? Can J Anaesth. 2010;57(6):549–558. doi: 10.1007/s12630-010-9306-4. [DOI] [PubMed] [Google Scholar]
- 25.Lalonde L [webpage on the Internet] Optimisation de la gestion de la douleur chronique en soins de première ligne [Optimizing the management of chronic pain in ambulatory primary care] ACCORD Regroupment des forces pour gérer la douleur chronique; Montreal,QC: 2009. [Accessed April 22, 2013]. Available from: http://www.programmeaccord.org/volets/premiereligne. [Google Scholar]
- 26.Jouini G, Choiniere M, Martin E, Perreault S, Berbiche D, Lussier D, et al. Pharmacotherapeutic management of chronic noncancer pain in primary care: lessons for pharmacists. J Pain Res. 2014;7:163–173. doi: 10.2147/JPR.S56884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Atlas de la santé et des services sociaux du Québec! [webpage on the Internet] Québec: Santé et Services sociaux Québec; 2014. [Accessed May 12, 2014]. Available from: http://www.msss.gouv.qc.ca/statistiques/atlas/atlas/index.php. [Google Scholar]
- 28.Hoffman DL, Sadosky A, Dukes EM, Alvir J. How do changes in pain severity levels correspond to changes in health status and function in patients with painful diabetic peripheral neuropathy? Pain. 2010;149(2):194–201. doi: 10.1016/j.pain.2009.09.017. [DOI] [PubMed] [Google Scholar]
- 29.World Health Organization . A new understanding of chronic pain. In: Kaplun A, editor. Health Promotion and Chronic Illness Discovering a New Quality of Health. Copenhagen, Denmark: WHO Regional Publications; 1992. pp. 141–226. [Google Scholar]
- 30.Jovey RD, Ennis J, Gardner-Nix J, et al. Canadian Pain Society Use of opioid analgesics for the treatment of chronic noncancer pain – a consensus statement and guidelines from the Canadian Pain Society, 2002. Pain Res Manag. 2003;8(Suppl A):3A–28A. doi: 10.1155/2003/436716. [DOI] [PubMed] [Google Scholar]
- 31.Merskey H, Bogduk N, editors. Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definition of Pain Terms. Seattle, WA: IASP Press; 2011. [Google Scholar]
- 32.Beaudry N [webpage on the Internet] Les tarifs des spécialistes de la santé en 2007 [The rates of health care professionals in 2007] Montreal, QC: Normandin Beaudry; [Accessed November 4, 2013]. Communiqué. 2007;10(12). Available from: http://www.normandin-beaudry.ca/publications/communiques/archives/2007/vol10-n12.fr.html. [Google Scholar]
- 33.Moulin DE, Clark AJ, Gilron I, et al. Canadian Pain Society Pharmacological management of chronic neuropathic pain – consensus statement and guidelines from the Canadian Pain Society. Pain Res Manag. 2007;12(1):13–21. doi: 10.1155/2007/730785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O’Connor AB, Dworkin RH. Treatment of neuropathic pain: an overview of recent guidelines. Am J Med. 2009;122(Suppl 10):S22–S32. doi: 10.1016/j.amjmed.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 35.Harpaz R, Ortega-Sanchez IR, Seward JF, Advisory Committee on Immunization Practices (ACIP) Centers for Disease Control and Prevention (CDC) Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2008;57(RR-5):1–30. quiz CE2–CE4. [PubMed] [Google Scholar]
- 36.Régie de l’assurance maladie du Québec . List of Medications. Gatineau, QC: Service des relations avec la clientele; 2011. [Accessed April 22, 2013]. Available from: https://www.prod.ramq.gouv.qc.ca/DPI/PO/Commun/PDF/Liste_Med/Liste_Med/liste_med_mod1_2011_12_16_en.pdf. [Google Scholar]
- 37.McKesson Canada [homepage on the Internet] McKesson Canada. San Francisco, CA: McKesson Corporation; 2013. [Accessed September 9, 2013]. Available from: https://www.mckesson.ca. [Google Scholar]
- 38.Vigilance Santé [homepage on the Internet] Vigilance Santé. Repentigny, QC: Vigilance Santé; 2013. [Accessed September 9, 2013]. Available from: http://www.vigilance.ca. [Google Scholar]
- 39.Statistics Canada [webpage on the Internet] Salaires horaires moyens des employés selon certaines caractéristiques et occupations, données non désaisonnalisées, par province (mensuel) (Canada) Ottawa, ON: Government of Canada; 2005. [Accessed September 9, 2013]. Available from: http://www.statcan.gc.ca/tables-tableaux/sum-som/l02/cst02/labr69a-fra.htm. [Google Scholar]
- 40.Statistics Canada [webpage on the Internet] Labour force survey estimates (LFS), by sex and detailed age group annual (persons x 1,000) Ottawa, ON: Government of Canada; 2014. [Accessed September 9, 2013]. Available from: http://www5.statcan.gc.ca/cansim/a05?lang=eng&id=2820002. [Google Scholar]
- 41.Commission des normes du travail du Québec [webpage on the Internet] History of the minimum wage. Québec, QC: Commission des norms du travail Québec; [Accessed August 26, 2013]. Available from: http://www.cnt.gouv.qc.ca/en/wages-pay-and-work/wages/history-of-the-minimum-wage/index.html. [Google Scholar]
- 42.Hu XH, Markson LE, Lipton RB, Stewart WF, Berger ML. Burden of migraine in the United States: disability and economic costs. Arch Intern Med. 1999;159(8):813–818. doi: 10.1001/archinte.159.8.813. [DOI] [PubMed] [Google Scholar]
- 43.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23(2):129–138. [PubMed] [Google Scholar]
- 44.Tyler EJ, Jensen MP, Engel JM, Schwartz L. The reliability and validity of pain interference measures in persons with cerebral palsy. Arch Phys Med Rehabil. 2002;83(2):236–239. doi: 10.1053/apmr.2002.27466. [DOI] [PubMed] [Google Scholar]
- 45.Kosinski M, Janagap CC, Gajria K, Schein J. Psychometric testing and validation of the Chronic Pain Sleep Inventory. Clin Ther. 2007;29(Suppl):2562–2577. doi: 10.1016/j.clinthera.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 46.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 47.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 48.Consumer Price Index, historical summary (1994 to 2013) [webpage on the Internet] Ottawa: Statistics Canada, Government of Canada; [Accessed May 12, 2014]. [updated January 24, 2014]. Available from: http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/econ46a-eng.htm. [Google Scholar]
- 49.Verstappen SM, Verkleij H, Bijlsma JW, et al. Determinants of direct costs in Dutch rheumatoid arthritis patients. Ann Rheum Dis. 2004;63(7):817–824. doi: 10.1136/ard.2003.014340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Walen HR, Cronan PA, Bigatti SM. Factors associated with healthcare costs in women with fibromyalgia. Am J Manag Care. 2001;7(Spec No):SP39–SP47. [PubMed] [Google Scholar]
- 51.Wolfe F, Ross K, Anderson J, Russell IJ, Hebert L. The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum. 1995;38(1):19–28. doi: 10.1002/art.1780380104. [DOI] [PubMed] [Google Scholar]
- 52.Manning WG. The logged dependent variable, heteroscedasticity, and the retransformation problem. J Health Econ. 1998;17(3):283–295. doi: 10.1016/s0167-6296(98)00025-3. [DOI] [PubMed] [Google Scholar]
- 53.Fleming S, Rabago DP, Mundt MP, Fleming MF. CAM therapies among primary care patients using opioid therapy for chronic pain. BMC Complement Altern Med. 2007;7:15. doi: 10.1186/1472-6882-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ekman M, Jönhagen S, Hunsche E, Jönsson L. Burden of illness of chronic low back pain in Sweden: a cross-sectional, retrospective study in primary care setting. Spine (Phila Pa 1976) 2005;30(15):1777–1785. doi: 10.1097/01.brs.0000171911.99348.90. [DOI] [PubMed] [Google Scholar]
- 55.Robinson RL, Birnbaum HG, Morley MA, Sisitsky T, Greenberg PE, Claxton AJ. Economic cost and epidemiological characteristics of patients with fibromyalgia claims. J Rheumatol. 2003;30(6):1318–1325. [PubMed] [Google Scholar]
- 56.Silverman S, Dukes EM, Johnston SS, Brandenburg NA, Sadosky A, Huse DM. The economic burden of fibromyalgia: comparative analysis with rheumatoid arthritis. Curr Med Res Opin. 2009;25(4):829–840. doi: 10.1185/03007990902728456. [DOI] [PubMed] [Google Scholar]
- 57.White AG, Birnbaum HG, Janagap C, Buteau S, Schein J. Direct and indirect costs of pain therapy for osteoarthritis in an insured population in the United States. J Occup Environ Med. 2008;50(9):998–1005. doi: 10.1097/JOM.0b013e3181715111. [DOI] [PubMed] [Google Scholar]
- 58.Jacobsson LT, Lindroth Y, Marsal L, Juran E, Bergström U, Kobelt G. Rheumatoid arthritis: what does it cost and what factors are driving those costs? Results of a survey in a community-derived population in Malmö, Sweden. Scand J Rheumatol. 2007;36(3):179–183. doi: 10.1080/03009740601089580. [DOI] [PubMed] [Google Scholar]
- 59.Pugner KM, Scott DI, Holmes JW, Hieke K. The costs of rheumatoid arthritis: an international long-term view. Semin Arthritis Rheum. 2000;29(5):305–320. doi: 10.1016/s0049-0172(00)80017-7. [DOI] [PubMed] [Google Scholar]
- 60.Tarride JE, Collet JP, Choinière M, Rousseau C, Gordon A. The economic burden of neuropathic pain in Canada. J Med Econ. 2006;9(1–4):55–68. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Hospitalization codes related or possibly related to chronic pain
| • Adhesive capsulitis of shoulder |
| • Algoneurodystrophy, unspecified |
| • Arthritis, unspecified |
| • Articular ankylosis |
| • Articular ankylosis – knee joint |
| • Carpal tunnel syndrome |
| • Cervicalgia |
| • Chronic intractable pain |
| • Chronic salpingitis and oophoritis |
| • Coxarthrosis, unspecified |
| • Endometriosis of uterus |
| • Endometriosis, unspecified |
| • Fibromyalgia |
| • Gonarthrosis, unspecified |
| • Gout, unspecified |
| • Idiopathic gout – elbow joint |
| • Idiopathic gout – hand joints |
| • Irritable bowel syndrome with diarrhea |
| • Irritable bowel syndrome without diarrhea |
| • Lateral epicondylitis |
| • Low back pain |
| • Osteoarthritis, unspecified |
| • Other cervical disc displacement |
| • Other dorsalgia |
| • Other specified arthrosis |
| • Other specified disorders of bone – leg |
| • Other specified intervertebral disc displacement |
| • Other specified spondylopathies – cervical region |
| • Pain in limb – scapular region |
| • Radiculopathy – dorsal region |
| • Rheumatoid arthritis, unspecified |
| • Rotator cuff syndrome |
| • Spinal instabilities – lumbar region |
| • Spinal stenosis – cervical region |
| • Spinal stenosis – lumbar region |
| • Spondylosis, unspecified – lumbar region |
Table S2.
Documented analgesics
| Therapeutic class | International common denomination |
|---|---|
| Anticonvulsants | |
| Carboxylic acid derivatives | Valproic acid |
| Gamma-aminobutyric acid analogs | Gabapentin, Pregabalin |
| Iminostilbene | Carbamazepine, Oxcarbazepine |
| Other anticonvulsants | Divalproex, Lamotrigine, Topiramate |
| Antidepressants | |
| Selective serotonin reuptake inhibitors | Citalopram, Escitalopram, Fluoxetine, Fluvoxamine, Paroxetine, Sertraline, Trazodone |
| Serotonin and noradrenaline reuptake inhibitors | Duloxetine, Venlafaxine |
| Tricyclic and tetracyclic antidepressants | Amitriptyline, Clomipramine, Desipramine, Doxepin, Imipramine, Maprotiline, Mirtazapine, Nortriptyline, Trimipramine |
| Other antidepressants | Bupropion |
| Antiretroviral | Acyclovir, Famciclovir, Valacyclovir |
| Disease-modifying antirheumatic drugs | Auranofin, Aurothioglucose, Aurothiomalate, Azathioprine, Chloroquine, Cyclosporine, D-penicillamine, Hydroxychloroquine, Leflunomide, Methotrexate, Sulfasalazine |
| Muscle relaxants | |
| Benzodiazepine | Diazepam, Tetrazepam |
| Carbamic acid derivatives | Methocarbamol |
| Centrally acting myorelaxants | Cyclobenzaprine, Tizanidine |
| Gamma-aminobutyric acid derivatives | Baclofen |
| Other muscle relaxants | Thiocolchicoside |
| Nonsteroidal antiinflammatory | |
| Acetic acids | Diclofenac, Etodolac, Indomethacin, Ketorolac, Nabumetone |
| Acetylsalicylic acid | |
| Coxibs | Celecoxib |
| Fenamates | Meclofenamate, Mefenamic acid |
| Oxicams | Meloxicam, Piroxicam |
| Propionic acids | Fenoprofen, Flurbiprofen, Ibuprofen, Ketoprofen, Naproxen, Oxaprozin |
| Opioids | |
| Agonist–antagonist derivatives | Buprenorphine, Butorphanol, Nalbuphine, Pentazocine |
| Antagonists | Naloxone |
| Benzomorphan derivatives | Pentazocine |
| Centrally acting analgesics | Tramadol |
| Meperidine-like agonists | Fentanyl, Meperidine |
| Methadone-like agonists | Methadone, Propoxyphene |
| Morphine-like agonists | Codeine, Hydrocodone, Hydromorphone, Levorphanol, Morphine, Oxycodone, Oxymorphone |
| Natural cannabinoids | Tetrahydrocannabinol, Cannabidiol |
| Synthetic cannabinoids | Dronabinol, Nabilone |