Abstract
Background
Pustular psoriasis of the digits (acrodermatitis continua of Hallopeau) may be localized to one or more digits for over an extended period of time. Characteristic presentation is that of tender, diffusely eroded, and fissured pustular plaques on one or more digits. Transition to other forms of psoriasis and to generalized pustular psoriasis is known to occur. These patients have an increased risk of acute generalized exanthematous pustulosis (AGEP) compared to the general population. Pustular psoriasis is often therapy resistant.
Main observations
We report the case of a 54-year-old Caucasian woman who presented with a pustular psoriasis flare complicated by AGEP. Treatment course included hospital admission, cyclosporine, acitretin, and discontinuation of cephalexin.
Conclusion
The precipitating factor in the course of treatment is thought to be cephalexin. When treating patients with pustular psoriasis the occurrence of druginduced complications should be carefully examined. Our case suggests that avoidance of β-lactam antibiotics in these patients is warranted unless absolutely indicated.
Keywords: acrodermatitis of Hallopeau, acute generalized exanthematous pustulosis (AGEP), pustular psoriasis
Introduction
Acrodermatitis continua of Hallopeau is a rare form of pustular psoriasis characterized by tender pustules on erythematous and erosive skin affecting one or more digits.[1] Treatment proves challenging since conventional treatment often fails.[2] Acute generalized exanthematous pustulosis (AGEP) as a consequence of antibiotic use during disease flare has been reported.[3-7]
The mechanism behind pustular psoriasis involves certain T cells such as Th 17 cells, and inflammatory cytokines.[8] Autoimmune diseases, family history, and lifestyle factors are thought to be implicated in the development of psoriasis.[9,10] Recent studies also suggest a genetic component; it has been suggested that psoriatic flares leading to generalized pustular psoriasis may be linked to mutations in IL36 receptor.[11,12]
We report the case of a 54-year-old Caucasian woman with a four-year history of acrodermatitis continua of Hallopeau who developed a severe flare of pustular psoriasis. The pustular psoriasis responded to oral cyclosporine (150 mg po bid) and increasing dosages of oral acitretin (25-50 mg po daily). Treatment was complicated by AGEP, most likely secondary to cephalexin which had been used to treat possible secondary skin infection.
Case Report
A 54-year-old Caucasian woman was seen in consultation for treatment of severe progressive pustular psoriasis. She had a four year history of recalcitrant acrodermatitis which had been previously managed with numerous treatments including: steroid ointments & injections, calcipotriol/betamethasone ointment, acitretin, immunosuppressants (methotrexate and azathioprine), and PUVA hand soaks. Present treatment included acitretin 10 mg po once daily. She had previously been unable to tolerate higher doses of acitretin due to "sticky skin".
Physical examination revealed pustular psoriasis on five fingers with associated loss of fingernails, and psoriatic plaques on right elbow and left breast. She also had tender, pruritic, erythematous patches and plaques studded with tiny pustules on her trunk and limbs. In addition she also complained of arthritic knee and mild finger joint pain. Associated symptoms included fever and chills. She was admitted to the hospital for management of her pustular psoriasis flare.
At time of admission her daily medications included rosuvastatin (10 mg once daily), hormone replacement therapy (HRT) (conjugated estrogens 0.625 mg once daily & medroxyprogesterone acetate 7.5 mg once daily), hydroxyzine (20 mg qid), and 10 mg acitretin once daily. She was admitted to the internal medicine service and started on the following medications orally: cephalexin 500 mg four times per day, cyclosporine 150 mg twice a day, hydroxyzine 25 mg four times per day as needed, dimenhydrinate 25-50 mg every four to six hours as needed, zopiclone 7.5 mg at night time, and acetominophen 325-650 mg every four to six hours as needed. Betamethasone n 0.1% cream BID was applied to affected areas and 1% hydrocortisone cream BID to flexural psoriasis. Rosuvastatin was held due to drug interactions with cyclosporine. Investigations revealed an elevated white count of (24.8 X 109/L, reference value of 4-10 X 109/L) with a neutrophil predominance. The oral acitretin dose was increased to 25 mg once daily the following day.
Two days later, because of the spreading pustular eruption, the oral acitretin dose was increased to 50 mg daily. On the third day of admission she had developed widespread blistering and peeling of skin with extensive denudation and weeping [Fig. 1]. Patient was admitted to a burn unit after consultation with plastic surgery. She was felt to have AGEP or TEN (toxic epidermal necrolysis) secondary to cephalexin, and cephalexin was discontinued. Laboratory results showed elevated WBC (24.0 X 109/L), neutrophils (19.9 X 109/L), platelets (407 X 109/L), and eosinophils (0.5 X 109/L), low CO2 (17 mmol/L), calcium (2.02 mmol/L), magnesium (0.65 mmol/L), and albumin (22.0 g/L).
Figure 1.
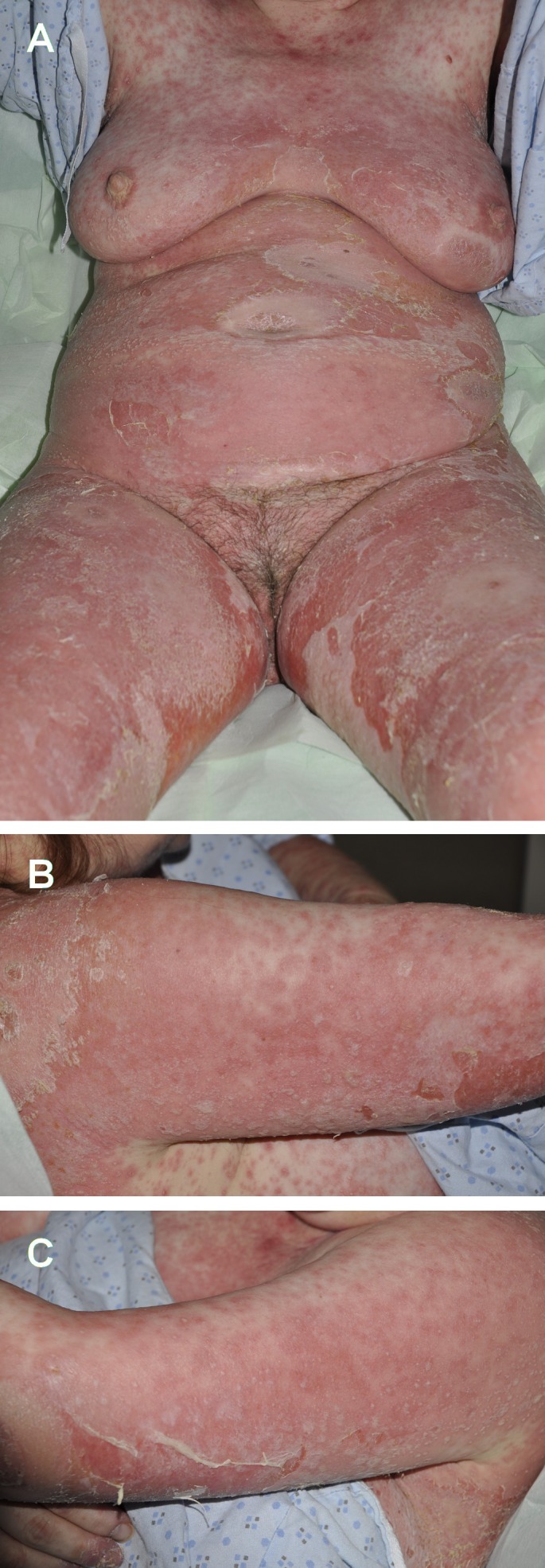
Acute Generalized Exanthematous Pustulosis (AGEP) during psoriatic flareup in hospital. (A) Frontal body involvement; (B) Right forearm; (C) Left arm.
Because of the clinical possibility of TEN she was treated with intravenous immunoglobulin (IVIG). A skin biopsy was also performed to help ascertain the nature of skin changes. Our patients' pathology report demonstrated neutrophilic spongiosis, neutrophils in both the superficial and deeper epidermal layers and the presence of a subcorneal pustule [Fig. 2A,B]. PAS stain was negative. Given the histopathology and clinical correlation the diagnosis was suggestive of AGEP. In AGEP histopathology is described with foci of neutrophilic spongiosis and subcorneal pustules.[13] It is associated with papillary dermal edema and perivascular infiltrates usually containing eosinophils.[13] It is differentiated from pustular psoriasis based on the presence of eosinophils and/or clinical correlation that suggests the commencement of a new medication.[14] Our patients' condition slowly improved over the next week with the combination treatment of acitretin and cyclosporine and discontinuation of antibiotics. She received topical wound care to open blistered areas.
Figure 2.
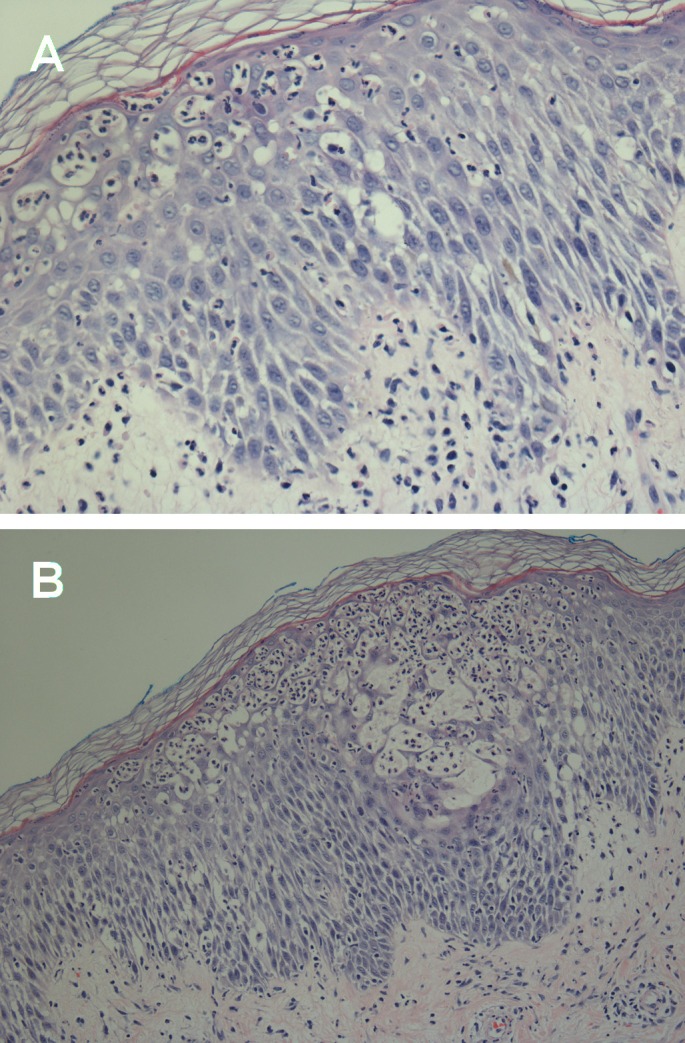
Dermatopathology. (A) Neutrophilic spongiosis; (B) Subcorneal pustule.
Following discharge, she was started on adalimumab (humira) [1st dose was 80 mg subcutaneous (SC) & 2nd dose was 40 mg SC]. She discontinued this medication on her own after two months due to development of a sore throat. She was able to tolerate acitretin 25 mg once daily [Fig. 3]. Her lipid profile indicates elevated triglycerides 2.72 mmol/L [reference value: 0.35-1.70 mmol/L] and cholesterol 7.46 mmol/L [reference value: 3.80-5.20 mmol/L]. She was switched to Ustekinumab once insurance coverage was obtained. Ustekinumab has shown some efficacy for recalcitrant pustular psoriasis that has failed conventional and biologic treatments.[15] She has noted marked improvement since the start of Ustekinumab and has been able to return to work. Since her psoriasis has not completed cleared we are planning to increase her dose from the current subcutaneous dose of 45 mg every 12 weeks to 90 mg every 12 weeks.
Figure 3.
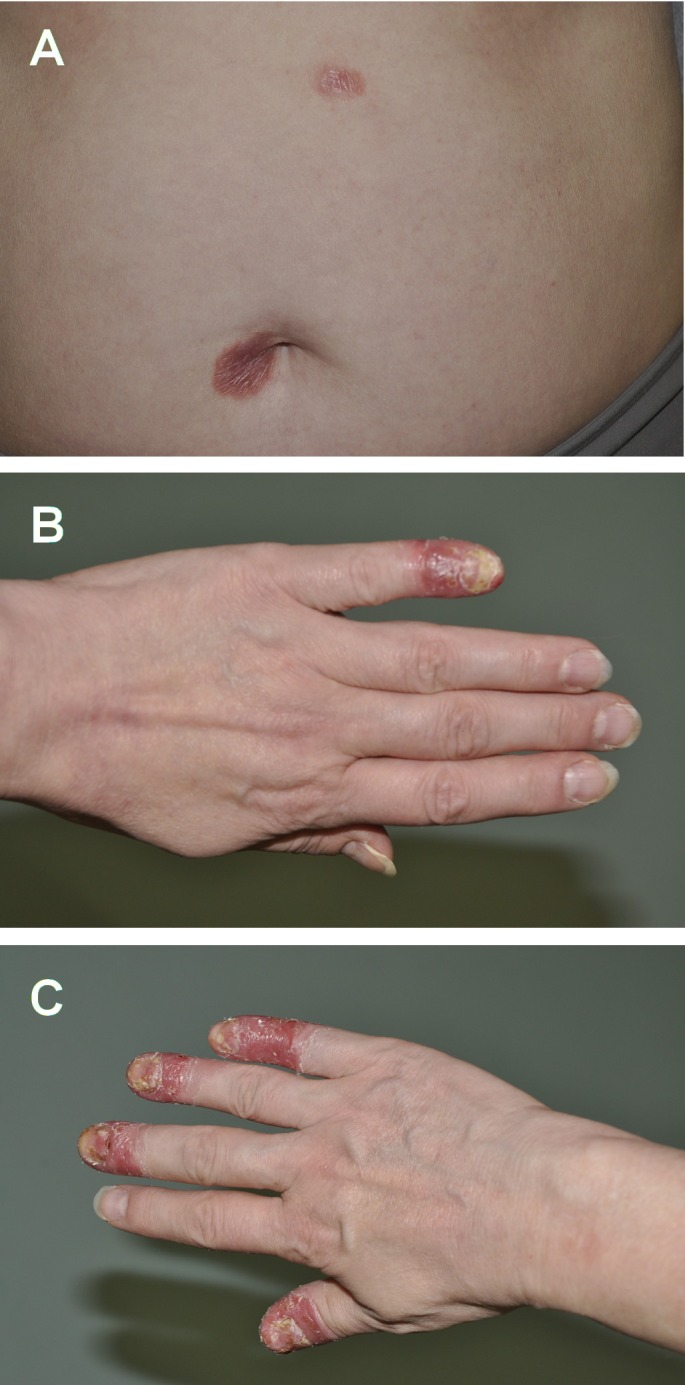
Psoriasis post-hospitalization. (A) Discrete plaques around Umbilicus & torso; (B) Left dorsal involvement; (C) Right dorsal involvement.
Discussion
During hospital admission the patients’ psoriasis was most likely aggravated by cephalexin. Cephalexin has previously been shown to cause generalized pustular eruptions.[4] In fact, in France, β-lactams were the cause of AGEP in 44% of cases.[16] Discontinuation of this medication and treatment with acitretin and cyclosporine resolved the psoriatic flare-up.
The inability of the initial hospital treatment regime to control the psoriatic flare-up and improvement once cephalexin was stopped supports the diagnoses of AGEP. 17% of patients with AGEP have a prior history of psoriasis and it is felt that patients with psoriasis are at increased risk for this form of drug reaction.[16] Patch testing with the suspect agent can reproduce a pustular eruption at 48 hours in approximately 50% of cases.[16] As systemic reactions to patch testing for evaluation of AGEP have been reported we were reluctant to patch test this patient.[16]
Our patient presented with acrodermatitis, pustular, and plaque psoriasis that has been refractory to conventional treatment. Antibiotic treatment during hospitalization likely contributed to the development of AGEP. When treating patients with pustular psoriasis the occurrence of drug-induced complications should be considered. As pustular psoriasis patients are at increased risk for AGEP, clinicians should avoid the usage of β-lactam antibiotics in these patients unless absolutely indicated.
Conclusion
AGEP is more likely to develop in patients with pustular psoriasis or who use β-latctam antibiotics. Hence our case in particular seems to exemplify this corollary. Clinical correlation with histopathology suggests that the use of cephalexin caused severe AGEP and prolonged our patients’ treatment course in hospital.
References
- Habif TP. Clinical Dermatology. 5th ed. St. Louis, MO: Mosby Elsevier; 2009. pp. 269–273. [Google Scholar]
- Benoit S, Toksoy A, Bröcker EB, Gillitzer R, Goebeler M. Treatment of recalcitrant pustular psoriasis with infliximab: effective reduction of chemokine expression. Br J Dermatol. 2004;150:1009–1012. doi: 10.1111/j.1365-2133.2004.05960.x. [DOI] [PubMed] [Google Scholar]
- Serra D, Gonçalo M, Mariano A, Figueiredo A. Pustular psoriasis and drug-induced pustulosis. G Ital Dermatol Venereol. 2011;146:155–158. [PubMed] [Google Scholar]
- Jackson H, Vion B, Levy PM. Generalized eruptive pustular drug rash due to cephalexin. Dermatologica. 1988;177:292–294. doi: 10.1159/000248581. [DOI] [PubMed] [Google Scholar]
- Whittam LR, Wakelin SH, Barker JN. Generalized pustular psoriasis or drug-induced toxic pustuloderma? The use of patch testing. Clin Exp Dermatol. 2000;25:122–124. doi: 10.1046/j.1365-2230.2000.00592.x. [DOI] [PubMed] [Google Scholar]
- Sidoroff A, Halevy S, Bavinck JN, Vaillant L, Roujeau JC. Acute generalized exanthematous pustulosis (AGEP) – A clinical reaction pattern. J Cutan Pathol. 2001;28:113–119. doi: 10.1034/j.1600-0560.2001.028003113.x. [DOI] [PubMed] [Google Scholar]
- Momin SB, Del Rosso JQ, Michaels B, Mobini N. Acute generalized exanthematous pustulosis: an enigmatic drug-induced reaction. Cutis. 2009;83:291–298. [PubMed] [Google Scholar]
- Teraki Y, Tanaka S, Hitomi K, Izaki S. A case of generalized psoriasiform and pustular eruption induced by infliximab: evidence for skin-homing Th17 in the pathogenesis. Br J Dermatol. 2010;163:1347–1351. doi: 10.1111/j.1365-2133.2010.10002.x. [DOI] [PubMed] [Google Scholar]
- Naldi L, Chatenoud L, Linder D, Belloni Fortina A, Peserico A, Virgili AR, Bruni PL, Ingordo V, Lo Scocco G, Solaroli C, Schena D, Barba A, Di Landro A, Pezzarossa E, Arcangeli F, Gianni C, Betti R, Carli P, Farris A, Barabino GF, La Vecchia C. Cigarette smoking, body mass index, and stressful life events as risk factors for psoriasis: Results from an Italian case-control study. J Invest Dermatol. 2005;125:61–67. doi: 10.1111/j.0022-202X.2005.23681.x. [DOI] [PubMed] [Google Scholar]
- Christophers E. Psoriasis − epidemiology and clinical spectrum. Clin Exp Dermatol. 2001;26:314–320. doi: 10.1046/j.1365-2230.2001.00832.x. [DOI] [PubMed] [Google Scholar]
- Onoufriadis A, Simpson MA, Pink AE, Di Meglio P, Smith CH, Pullabhatla V, Knight J, Spain SL, Nestle FO, Burden AD, Capon F, Trembath RC, Barker JN. Mutations in IL36RN/IL1F5 are associated with the severe episodic inflammatory skin disease known as generalized pustular psoriasis. Am J Hum Genet. 2011;89:432–437. doi: 10.1016/j.ajhg.2011.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marrakchi S, Guigue P, Renshaw BR, Puel A, Pei XY, Fraitag S, Zribi J, Bal E, Cluzeau C, Chrabieh M, Towne JE, Douangpanya J, Pons C, Mansour S, Serre V, Makni H, Mahfoudh N, Fakhfakh F, Bodemer C, Feingold J, Hadj-Rabia S, Favre M, Genin E, Sahbatou M, Munnich A, Casanova JL, Sims JE, Turki H, Bachelez H, Smahi A. Interleukin-36-receptor antagonist deficiency and generalized pustular psoriasis. N Engl J Med. 2011;365:620–628. doi: 10.1056/NEJMoa1013068. [DOI] [PubMed] [Google Scholar]
- Barnhill RL. Dermatopathology. New York: McGraw-Hill Medical; 2010. pp. 20–60. [Google Scholar]
- Billings SD, Cotton J. Inflammatory Dermatopathology: A Pathologist's Survival Guide. New York: Springer; 2011. pp. 21–36. [Google Scholar]
- Daudén E, Santiago-et-Sánchez-Mateos D, Sotomayor-López E, García-Díez A. Ustekinumab: effective in a patient with severe recalcitrant generalized pustular psoriasis. Br J Dermatol. 2010;163:1346–1347. doi: 10.1111/j.1365-2133.2010.09995.x. [DOI] [PubMed] [Google Scholar]
- James WD, Berger DM, Elston DM, Odom RB. Contact Dermatitis and Drug Eruptions. Andrews' Diseases of the Skin: Clinical Dermatology. Philadelphia: Saunders Elsevier; 2006. pp. 124–125. [Google Scholar]


